Abstract
Introduction
This study aimed to understand treatment response dynamics, including factors associated with favorable response, among patients with moderate-to-severe psoriasis who received guselkumab, adalimumab, or secukinumab.
Methods
These post hoc analyses used data from the phase III clinical trials ECLIPSE and VOYAGE 1, which were conducted between September 2021 and November 2022. On the basis of absolute Psoriasis Area and Severity Index (aPASI) scores, patients were divided into short-term response types (SRT1–6, based on week 20–48 response) and long-term response types (LRT1–4, based on week 52–252 response). Response types (RTs) were based on aPASI cutoffs deemed clinically relevant by the investigators; SRT1/LRT1 were the most favorable response types. Baseline characteristics were compared across RTs, and logistic regression analyses established factors associated with SRT1/LRT1.
Results
Overall, 1045, 662, and 272 patients were included in the ECLIPSE short-term, VOYAGE 1 short-term, and VOYAGE 1 long-term analyses, respectively. Mean age, body mass index (BMI), baseline aPASI score, and body surface area were lower in SRT1 than SRT6. In VOYAGE 1, adalimumab treatment, high BMI, and current/former smoking status resulted in less favorable responses. In the VOYAGE 1 long-term analysis, patients in LRT4 had the highest baseline aPASI score, were older, and were more often obese compared with other LRT groups. Regression analyses showed that SRT1 (both treatments) in VOYAGE 1 and ECLIPSE, and LRT1 (guselkumab group) in the VOYAGE 1 long-term analysis, were associated with week 16 aPASI response. In VOYAGE 1, SRT1 was associated with psoriasis duration and smoking status.
Conclusions
Early treatment response and baseline characteristics, including smoking, psoriasis duration, and obesity, may be associated with longer-term response to biologics.
Trial Registration Numbers
ECLIPSE: NCT03090100, VOYAGE 1: NCT02207231.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The aim of this study was to assess which characteristics are associated with favorable response to biologics in patients with psoriasis. |
In these analyses of the ECLIPSE and VOYAGE 1 trials, favorable response to treatment through week 48 and 252 was associated with absolute Psoriasis Area and Severity Index response at week 16; psoriasis duration and smoking status were also associated with favorable response in VOYAGE 1 through week 48. Certain baseline characteristics, such as high body mass index, were more common in patients with less favorable response types than other groups. |
Early response to treatment and certain baseline characteristics (smoking, psoriasis duration, and obesity) may be associated with longer-term response. |
Introduction
Psoriasis is a chronic inflammatory skin disease that can significantly affect patients’ quality of life [1, 2]. In recent years, as the pathogenesis of the disease has become better understood, a variety of novel targeted treatments have become available [1, 3]. Multiple biologic classes have demonstrated efficacy for the treatment of moderate-to-severe plaque psoriasis at set time points, including tumor necrosis factor (TNF) inhibitors, interleukin (IL)-17 inhibitors, an IL-12/23 inhibitor, and IL-23 inhibitors [3, 4]. There is also evidence that these treatments can improve patients’ quality of life [5, 6]. However, data on predictors and dynamics of response to biologic treatment are limited and primarily drawn from registry and retrospective studies [7,8,9,10]. Therefore, generating association models from randomized controlled trial data may help with efforts to personalize healthcare in psoriasis, to maximize positive efficacy outcomes and minimize negative safety outcomes [11].
Guselkumab, an IL-23p19 inhibitor administered by subcutaneous injection, has been extensively investigated in studies of patients with moderate-to-severe plaque psoriasis, such as the phase III clinical trials VOYAGE 1 (which included an open-label extension [OLE]) and ECLIPSE [12,13,14]. In VOYAGE 1, higher proportions of patients achieved Investigator’s Global Assessment (IGA) 0 or 1 and Psoriasis Area and Severity Index (PASI) 90 responses at week 16 with guselkumab versus placebo (co-primary endpoint) or adalimumab [12]. In ECLIPSE, guselkumab was superior to secukinumab on the basis of the PASI 90 primary endpoint at week 48 [13].
In clinical practice, patient responses to biologics can be categorized into a variety of response types (RTs), such as “maintenance of clear response” and “non-acceptable response.” We hypothesize that a patient’s RT is likely to vary over time. When biologic treatment is initiated, there is usually an induction period during which initial response occurs and continues to improve (weeks 0–12/16), followed by a stabilization period when maximal efficacy is achieved and begins to level off (weeks 20–48). Beyond this point (week 52 onwards, “long term”), patients are in a maintenance phase.
The objective of these post hoc analyses of data from ECLIPSE and VOYAGE 1 was to understand the treatment response dynamics of different subgroups of patients with short-term RTs (SRTs) receiving guselkumab, adalimumab, or secukinumab in phase III trials and long-term RTs (LRTs) for those who continued guselkumab in the VOYAGE 1 OLE. We then evaluated factors associated with the most favorable treatment RT.
Methods
Source of Data
Data were derived from the ECLIPSE (NCT03090100; April 2017 through September 2018 at 142 sites) and VOYAGE 1 (NCT02207231; December 2014 through June 2020, including the OLE, at 101 sites) phase III, global, multicenter trials. Study designs have been published previously and are briefly described here [12, 13]. Results of these post hoc analyses are presented. Data were analyzed between September 2021 and November 2022.
Participants
Eligible patients were ≥ 18 years of age and had moderate-to-severe plaque psoriasis (absolute PASI [aPASI] ≥ 12, IGA score ≥ 3, and body surface area [BSA] involvement ≥ 10%) for ≥ 6 months, and were candidates for phototherapy or systemic therapy [12, 13]. The protocols for ECLIPSE and VOYAGE 1 were approved by relevant ethics committees and review boards. Both studies were conducted in accordance with the Declaration of Helsinki and are consistent with Good Clinical Practice. Participating patients provided written informed consent.
Randomization, Treatment, and Masking
In ECLIPSE, patients were randomized 1:1 to receive either guselkumab (100 mg at weeks 0 and 4, then every 8 weeks) or secukinumab (300 mg at weeks 0, 1, 2, 3, and 4, then every 4 weeks) through week 44 [13]. In VOYAGE 1, patients were randomized 2:1:2 to receive either guselkumab 100 mg (weeks 0 and 4, then every 8 weeks), placebo/guselkumab (placebo at weeks 0, 4, and 12, then guselkumab at weeks 16 and 20, then every 8 weeks), or adalimumab (80 mg at week 0, 40 mg at week 1, then 40 mg every 2 weeks through week 47) [12]. Patients in the VOYAGE 1 OLE receiving guselkumab from baseline for ≥ 156 consecutive weeks were included [14].
Outcome Assessments
In ECLIPSE, aPASI scores were obtained weekly from baseline to week 4 and every 4 weeks thereafter until week 48; in VOYAGE 1 and the OLE, aPASI scores were obtained at baseline, week 2, every 4 weeks from week 4 to 52, then every 8 weeks to week 252.
SRTs and LRTs were author-defined at weeks 48 and 252, respectively, and were based on aPASI scores using cutoff values judged to be clinically relevant. Patients receiving treatment with guselkumab, secukinumab, or adalimumab between weeks 0 and 48 in ECLIPSE and VOYAGE 1 were categorized into six SRTs (Table 1). Patients receiving guselkumab from week 0 for ≥ 156 consecutive weeks through up to 5 years in the VOYAGE 1 OLE were categorized into four LRTs (Table 1). RTs were mutually exclusive, and each patient was assigned to the most favorable RT they achieved, based on as-observed aPASI scores reported at each time point through a defined period. Analyses were also conducted with four alternatively defined LRTs based on aPASI and Dermatology Life Quality Index (DLQI) scores reported at each time point through a defined period using clinically relevant cutoff values as determined by the authors (Table 1). DLQI scores were collected at weeks 0, 8, 16, 24, and 48 in VOYAGE 1 and weeks 76, 100, 124, 156, 172, 204, 228, and 252 in the VOYAGE 1 OLE, but were not collected in ECLIPSE.
Analyses
After classification of patients into RTs and development of heatmap visualizations, baseline characteristics were compared across RTs with descriptive statistics. A Sankey diagram was developed to depict the proportion of patients in VOYAGE 1 SRTs who were recategorized into each of the respective LRTs in the VOYAGE 1 OLE.
A multivariable logistic regression model was developed to establish factors associated with RT1. For ECLIPSE and VOYAGE 1, SRT1 was defined over weeks 20–48 for patients treated with guselkumab, adalimumab, or secukinumab, and for the VOYAGE 1 OLE, LRT1 was defined over weeks 52–252 for patients treated with guselkumab, with LRTs based on aPASI or aPASI and DLQI criteria. Variables included in the model were chosen on the basis of results of comparing characteristics across RTs; variables included baseline age, body mass index (BMI), sex, smoking status, presence of psoriatic arthritis, psoriasis duration, prior exposure to systemic treatment, aPASI score, C-reactive protein level, and aPASI score at week 16. Observed data were used with no imputation. Forward and backward elimination techniques, with alpha = 0.10, were used for covariate selection. Significance was not corrected. All statistical analyses were conducted using SAS version 9.4 (SAS Institute, Inc., Cary, NC, USA) or higher using the Windows operating system.
Results
Patient Disposition and RTs
Short-Term RTs
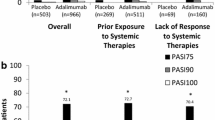
For ECLIPSE, 1045 patients were included in the SRT analysis (guselkumab, n = 534; secukinumab, n = 511); three patients were randomized but not treated and therefore were not included [13]. The largest numerical differences in between-group distribution of SRTs were between the proportion of patients in SRT6, the least favorable SRT (10.7% vs 18.4%, respectively), and SRT1, the most favorable SRT (34.1% vs 29.2%; Supplementary Fig. 1a).
The SRT analysis for VOYAGE 1 included 662 patients. The largest numerical differences between guselkumab and adalimumab groups were between the proportion of patients in SRT6, the least favorable (15.2% vs 43.2%, respectively), and SRT1, the most favorable SRT (22.5% vs 10.8%; Supplementary Fig. 1b).
Long-Term RTs
In VOYAGE 1, 329 patients were enrolled to receive guselkumab; however, 57 (17.3%) discontinued treatment before week 156 and were not included in the LRT analysis. Therefore, 272 patients were included and categorized into four LRTs (Supplementary Fig. 1c).
Because the criteria between SRTs and LRTs differed, patient distributions across both were compared for VOYAGE 1 (short-term) and the OLE (long-term). A Sankey diagram depicted the proportion of patients in each SRT and their recategorization into an LRT is shown in Fig. 1. Most patients were recategorized from SRTs to similar/corresponding LRTs. Similar results were seen when patients were categorized into RTs based on observed aPASI and DLQI scores (Supplementary Fig. 2).
Sankey diagram depicting proportion of patients receiving guselkumab in VOYAGE 1 according to each SRT and their recategorization into an LRT in the VOYAGE 1 OLE. A large proportion of patients in VOYAGE 1 who achieved a specific SRT went on to achieve a similar LRT. Only patients who were in the study for ≥ 156 weeks, received guselkumab, and included in both the short- and long-term analyses are included. SRTs and LRTs were defined on the basis of aPASI only. aPASI absolute Psoriasis Area and Severity Index, LRT long-term RT, OLE open-label extension, RT response type, SRT short-term RT
Baseline Characteristics
Short-Term RTs
Across the overall study populations of ECLIPSE and VOYAGE 1 (Supplementary Tables 1–4), mean age, BMI, aPASI score, and BSA at baseline were lower for SRT1 versus SRT6. SRT1 and SRT2 included the highest proportions of younger patients (< 45 years of age); in VOYAGE 1, SRT4 had the lowest proportion of patients who never smoked; mean body weight was generally higher in less favorable RTs. In ECLIPSE, psoriasis duration was shortest in SRT1 for patients receiving secukinumab, and lowest in SRT2 and SRT4 for patients receiving guselkumab. In VOYAGE 1, psoriasis duration was shortest in SRT1 for patients treated with adalimumab or guselkumab.
Patients treated with adalimumab in VOYAGE 1 with a high BMI and/or who were current smokers were often categorized into less favorable SRTs, whereas a higher proportion of never-smokers were included in more favorable SRTs. However, BMI and smoking status appeared to have a less substantial effect on SRTs for guselkumab. Mean aPASI score at baseline was numerically lower in SRT1 versus SRT6 in the guselkumab group but similar between SRT1 and SRT6 in the adalimumab group.
Long-Term RTs
Baseline characteristics across LRTs in the VOYAGE 1 OLE are shown in Supplementary Table 5. Patients in LRT4 had higher mean age, BMI, and aPASI at baseline and more were obese versus all other LRTs. The proportion of patients without nail psoriasis was highest in LRT1 and LRT2. All other characteristics were generally similar across LRTs. Similarly, when using observed aPASI and DLQI scores to categorize patients into LRTs, patients in LRT4 had the highest baseline aPASI scores, and LRT4 included more patients with nail psoriasis at baseline than other LRTs (Supplementary Table 6).
Efficacy and Patient-Reported Outcomes Over Time
Mean aPASI scores over time are shown in Fig. 2a–c. Across all trials, in all SRTs and LRTs, aPASI score improved over time from baseline to the end of trial. Results were similar for the VOYAGE 1 OLE, with patients categorized into LRTs based on observed aPASI and DLQI scores (Supplementary Fig. 3). Heatmap visualizations of patient-level aPASI scores for each of the treatment groups in ECLIPSE, VOYAGE 1, and the VOYAGE 1 OLE are shown in Supplementary Figs. 4, 5, and 6. More patients were categorized into SRT1 or SRT2 with guselkumab versus secukinumab in ECLIPSE (Supplementary Figs. 1a and 4); this was also true for guselkumab versus adalimumab in VOYAGE 1 (Supplementary Figs. 1b and 5). In the VOYAGE 1 OLE, most patients were categorized into LRT2 based on aPASI score (Supplementary Figs. 1c and 6). In the VOYAGE 1 OLE, with LRT groups categorized on the basis of observed aPASI and DLQI scores, similar numbers of patients fell into LRT2 and LRT3 (Supplementary Fig. 6b).
Plots of mean aPASI scores for patients in each numbered RT group across the three clinical trials. Patients with more favorable SRTs achieved better skin responses than patients with less favorable SRTs. a ECLIPSE, b VOYAGE 1, and c VOYAGE 1 OLE. Patients with more favorable SRTs achieved better skin responses than patients with less favorable SRTs. Data shown are for the overall population for each trial, and, therefore, a and b include patients that were treated with guselkumab or secukinumab and guselkumab or adalimumab, respectively. Patients in the OLE of VOYAGE 1 were treated with guselkumab (c). SRTs and LRTs were defined on the basis of aPASI only. aPASI absolute Psoriasis Area and Severity Index, LRT long-term RT, OLE open-label extension, RT response type, SRT short-term RT
Among patients receiving guselkumab in VOYAGE 1, DLQI scores were largely aligned with aPASI scores, although DLQI scores were more variable over time. In general, DLQI responses were achieved by week 24 and maintained thereafter in SRT1–6, and DLQI score was consistently lower in SRT1 and SRT2 versus other SRTs (Fig. 3a). DLQI patterns over 252 weeks in patients receiving guselkumab in the VOYAGE 1 OLE were similar to those seen for aPASI scores, particularly for LRT1–3 (Fig. 3b). At week 24, mean DLQI scores were 0.69–5.70 and 0.88–3.14 across SRTs in VOYAGE 1 and LRTs in the VOYAGE 1 OLE, respectively. As with mean aPASI scores over time for the VOYAGE 1 OLE, when RTs were based on observed aPASI and DLQI scores, the DLQI results were similar compared with RTs based on observed aPASI score alone (Supplementary Fig. 7). At week 24, mean DLQI scores ranged from 0.59 to 3.61 across RTs in the VOYAGE 1 OLE when RTs were based on observed aPASI and DLQI scores. Heatmap visualizations of patient-level DLQI scores for each treatment group in the VOYAGE 1 and VOYAGE 1 OLE are shown in Supplementary Fig. 8.
Plots of mean DLQI scores over time for patients from VOYAGE 1 and the VOYAGE 1 OLE stratified by RT. Patients with more favorable short-term and long-term RTs achieved greater improvements in DLQI scores than patients in less favorable RTs. a Data shown are for the overall VOYAGE 1 population and, therefore, the graph includes patients that received guselkumab or adalimumab. b Patients in the OLE of VOYAGE 1 were treated with guselkumab. SRTs and LRTs were defined on the basis of aPASI only. aPASI absolute Psoriasis Area and Severity Index, DLQI Dermatology Life Quality Index, LRT long-term RT, OLE open-label extension, RT, response type, SRT short-term RT
Logistic Regression Model: Factors Associated with Classification in RT1 When Receiving Biologic Treatment
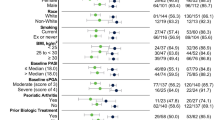
Results of the multivariable logistic regression for factors associated with SRT1 (patients from ECLIPSE and VOYAGE 1 treated with guselkumab, adalimumab, or secukinumab) and LRT1 (patients from the VOYAGE 1 OLE treated with guselkumab), using the backward elimination model are presented in Fig. 4, with odds ratios shown for selected covariates. Results using the full model are presented in Supplementary Fig. 9.
Association of factors with SRT1 (ECLIPSE and VOYAGE 1) and LRT1 (VOYAGE 1 OLE); backward elimination model. Forest plot shows that, in ECLIPSE, achievement of SRT1 was associated with aPASI score at week 16. In VOYAGE 1, aPASI score at week 16 and smoking status (former smoker vs never smoker) at baseline were associated with achievement of SRT1. In the VOYAGE 1 OLE, aPASI score at week 16 was associated with achievement of LRT1. The model for the SRT is based on patients receiving guselkumab or secukinumab in ECLIPSE and guselkumab or adalimumab in VOYAGE 1; the model for the LRT is based on patients receiving guselkumab in the VOYAGE 1 OLE. aPASI absolute Psoriasis Area and Severity Index, BMI body mass index, CI confidence interval, DLQI Dermatology Life Quality Index, LRT long-term response type, OLE open-label extension, SRT short-term response type, W week
In the backward elimination model, achieving SRT1 in ECLIPSE, SRT1 in VOYAGE 1, and LRT1 in the VOYAGE 1 OLE were associated with aPASI scores at week 16 (Fig. 4). In ECLIPSE, this was the only variable associated with achievement of SRT1, and in the VOYAGE 1 OLE it was the only variable associated with achievement of LRT1 (irrespective of how LRTs were defined). Of note, when looking at baseline demographics, there was not a statistically significant association between lower BMI at baseline and achievement of LRT1. However, in VOYAGE 1, SRT1 was associated with psoriasis duration and smoking status at baseline.
Discussion
In these post hoc analyses of data from two multicenter randomized controlled clinical trials, patients in favorable SRTs and LRTs tended to be younger, have lower baseline BMI and aPASI scores, and have shorter duration of psoriasis than those in less favorable RTs. In multivariable logistic regression analyses, lower week 16 aPASI scores were consistently associated with a higher chance of achieving the most favorable RTs (SRT1 in ECLIPSE and VOYAGE 1, and LRT1 in the VOYAGE 1 OLE). In VOYAGE 1, but not ECLIPSE, shorter disease duration and never having smoked (versus being a former smoker) were also associated with a higher probability of achieving SRT1; no baseline demographics were associated with achieving LRT1.
As expected, on the basis of the efficacy results from the ECLIPSE and VOYAGE 1 studies, more patients receiving guselkumab were classified into favorable SRTs versus secukinumab or adalimumab. At the end of the VOYAGE 1 OLE, most patients treated with guselkumab had low disease activity (LRT2). These analyses identified differences in characteristics that help to explain these results. For example, short-term treatment with adalimumab resulted in categorization into less favorable SRTs among current smokers versus patients who had never smoked, whereas smoking status did not appear to impact SRT classification for patients receiving secukinumab or guselkumab. Higher baseline BMI appeared to result in categorization into less favorable SRTs among patients receiving secukinumab or adalimumab, but no clear pattern was observed with guselkumab. Validation studies are required to confirm the association between variables identified and the RTs defined here and to support use of these RTs for the guidance of treatment in clinical practice.
These results contribute to the ongoing effort to personalize treatment of psoriasis, which requires an understanding of the factors that may affect response to different treatments [11, 15]. The RTs used were author-defined and based on clinical experience, but generally appear consistent with wider interpretation of aPASI scores. For example, in an analysis of data from the British Association of Dermatologists Biologics and Immunomodulators Register (BADBIR), including more than 13,000 patients with psoriasis, achieving aPASI score ≤ 4 was concordant with PASI 75 response in 88% of cases [16]. Additionally, in a population-based cohort study including 2034 patients with moderate-to-severe psoriasis and 3 years’ sustained treatment with adalimumab, etanercept, infliximab, certolizumab pegol, ustekinumab, secukinumab, ixekizumab, or brodalumab, predictive prognostic models were used to identify optimal biologic treatment [17]. Modeling predicted which cytokine targets were associated with a successful treatment outcome with 59.2–63.6% accuracy overall and 93.9–95.9% accuracy for the two most successful treatments. Therefore, predicted response to treatment could potentially be used to guide a holistic approach for managing patients with psoriasis, which may allow physicians to optimize the balance of treatment benefit and the risk of side effects on an individual basis [11, 15].
The association of smoking with the onset of psoriasis and disease severity is well established [18,19,20]. Data from real-world registries [7,8,9], retrospective analyses [10], and a recent meta-analysis [21] have shown that smokers have a worse response to biologic therapy than non-smokers. However, biologics have more commonly been studied either by mechanism of action or as an overall class, but differences between individual biologics have not been established. In a recent pooled analysis evaluating the effect of baseline factors on outcomes with secukinumab, there were more non-smokers in groups with better responses to treatment; a similar, but weaker, trend was also seen in patients treated with etanercept [22]. The value of smoking cessation for reducing psoriasis severity remains unclear, and its impact on treatment outcomes in patients with psoriasis has yet to be explored [21]. Nonetheless, smoking cessation programs should be considered for patients with psoriasis [20].
The less favorable outcomes observed in this study in patients with a high BMI treated with secukinumab and adalimumab are also consistent with observations in real-world and retrospective analyses [7,8,9,10]. Additionally, in an analysis of pooled phase III data from patients with psoriasis (FIXTURE, ERASURE, and CLEAR trials), lower BMI was associated with a better response to treatment with secukinumab [22]. In the prospective GUIDE study, which analyzed factors leading to complete skin clearance following guselkumab treatment, each kg/m2 increase in BMI negatively affected the likelihood of achieving clearance [23]. However, consistent with real-world studies [24, 25], our analyses found that the effect of BMI on efficacy may be less with guselkumab treatment compared with other treatments. Weight loss has been shown to improve treatment outcomes in patients with psoriasis [26, 27], and weight loss interventions should also be considered when treating patients.
Finally, prior biologic therapy may be associated with a poor short-term response to guselkumab and secukinumab. This is consistent with other studies showing that prior systemic or biologic therapy can negatively affect the efficacy of TNF inhibitors [28, 29], ustekinumab [28, 30], secukinumab [22], and guselkumab [25].
The primary strength of this analysis is that it is based on robust datasets from two randomized clinical trials that included a total of almost 2000 participants. Our analysis therefore includes comparison of three different treatments. In addition, these datasets included long-term follow-up, to a maximum of 252 weeks, allowing differentiation of short-term and long-term response. It is also a strength that the RT definitions were based on thresholds deemed clinically relevant by psoriasis experts. In contrast, a limitation of the analysis is that the RT definitions did not consider patient views. A recent consensus study, including patients with psoriasis, dermatologists, and nurses, described freedom from disease as multifaceted, with five domains identified as management of clinical symptoms, considerations beyond the skin, treatment burden, quality of care, and well-being [31]. Hence, this analysis may have missed certain patient-relevant considerations by focusing on clinical responses, evaluating aPASI ± DLQI alone. Other limitations include the post hoc nature of these analyses, use of descriptive statistics, and the lack of statistical analyses comparing adjustment for baseline characteristics across different RTs. Long-term data were only available for guselkumab, with no comparator. Additionally, with the exception of obesity, baseline cardiometabolic parameters were not evaluated; diabetes, metabolic syndrome, and hypertension have all been shown to be associated with response to biologics in other studies [22]. While similar results were found with RTs defined on the basis of aPASI score alone or aPASI and DLQI scores, patient-reported outcomes are important measures of treatment success [31]. Covariates using logistic regression were derived on the basis of a relatively small number of patients, and correlation/agreement within covariates was not evaluated. Further, aPASI score was used to define RTs and was also a covariate and therefore, as expected, was associated with SRT1/LRT1. Most covariates were measured at baseline with the response variable based on a time interval; it is possible that a given characteristic could have changed (e.g., smoking status) during the time interval used to define the RT. Lastly, the performance of the models was never compared.
Conclusion
Our analyses suggest associations between initial response and certain baseline characteristics (e.g., smoking, psoriasis duration, and obesity) with long-term response to treatment. Such associations may differ between biologics. Lifestyle and weight management appear to be important in management of psoriasis, given their impact on treatment outcomes. Further research is needed to confirm these findings and validate the clinical relevance of the RT definitions presented here: for instance, future prospective studies should collect data on a wider range of potential treatment response predictors. It could also be valuable to run a similar analysis including patient-identified disease outcomes as noted above. However, the present study suggests that tailored disease management based on patients’ baseline characteristics for more effective treatment appears to be a future possibility.
Data Availability
The data sharing policy of Janssen Pharmaceutical Companies of Johnson & Johnson is available at https://www.janssen.com/clinical-trials/transparency. Requests for access to the study data can be submitted through the Yale Open Data Access (YODA) Project site.
References
Rendon A, Schakel K. Psoriasis pathogenesis and treatment. Int J Mol Sci. 2019;20(6):1475. https://doi.org/10.3390/ijms20061475.
Nabieva K, Vender R. Quality of life and body region affected by psoriasis: a systematic review. Actas Dermosifiliogr. 2023;114(1):T33–8. https://doi.org/10.1016/j.ad.2022.07.025.
Sbidian E, Chaimani A, Guelimi R, et al. Systemic pharmacological treatments for chronic plaque psoriasis: a network meta-analysis. Cochrane Database Syst Rev. 2023;7(7):Cd011535. https://doi.org/10.1002/14651858.CD011535.pub6.
Thatiparthi A, Martin A, Liu J, Egeberg A, Wu JJ. Biologic treatment algorithms for moderate-to-severe psoriasis with comorbid conditions and special populations: a review. Am J Clin Dermatol. 2021;22(4):425–42. https://doi.org/10.1007/s40257-021-00603-w.
Karpinska-Mirecka A, Bartosinska J, Krasowska D. The effects of selected biologics and a small molecule on health-related quality of life in adult plaque psoriasis patients: a systematic review and meta-analysis. PLoS ONE. 2020;15(12):e0241604. https://doi.org/10.1371/journal.pone.0241604.
de Ruiter CC, Rustemeyer T. Biologics can significantly improve Dermatology Life Quality Index (DLQI) in psoriatic patients: a systematic review. Psoriasis (Auckl). 2022;12:99–112. https://doi.org/10.2147/PTT.S356568.
Schwarz CW, Loft N, Rasmussen MK, et al. Predictors of response to biologics in patients with moderate-to-severe psoriasis: a Danish nationwide cohort study. Acta Derm Venereol. 2021;101(10):adv00579. https://doi.org/10.2340/actadv.v101.351.
Warren RB, Marsden A, Tomenson B, et al. Identifying demographic, social and clinical predictors of biologic therapy effectiveness in psoriasis: a multicentre longitudinal cohort study. Br J Dermatol. 2019;180(5):1069–76. https://doi.org/10.1111/bjd.16776.
Warren RB, Smith CH, Yiu ZZN, et al. Differential drug survival of biologic therapies for the treatment of psoriasis: a prospective observational cohort study from the British Association of Dermatologists Biologic Interventions Register (BADBIR). J Invest Dermatol. 2015;135(11):2632–40. https://doi.org/10.1038/jid.2015.208.
Di Lernia V, Ricci C, Lallas A, Ficarelli E. Clinical predictors of non-response to any tumor necrosis factor (TNF) blockers: a retrospective study. J Dermatolog Treat. 2014;25(1):73–4. https://doi.org/10.3109/09546634.2013.800184.
Camela E, Potestio L, Ruggiero A, Ocampo-Garza SS, Fabbrocini G, Megna M. Towards personalized medicine in psoriasis: current progress. Psoriasis (Auckl). 2022;12:231–50. https://doi.org/10.2147/ptt.s328460.
Blauvelt A, Papp KA, Griffiths CE, et al. Efficacy and safety of guselkumab, an anti-interleukin-23 monoclonal antibody, compared with adalimumab for the continuous treatment of patients with moderate to severe psoriasis: results from the phase III, double-blinded, placebo- and active comparator-controlled VOYAGE 1 trial. J Am Acad Dermatol. 2017;76(3):405–17. https://doi.org/10.1016/j.jaad.2016.11.041.
Reich K, Armstrong AW, Langley RG, et al. Guselkumab versus secukinumab for the treatment of moderate-to-severe psoriasis (ECLIPSE): results from a phase 3, randomised controlled trial. Lancet. 2019;394(10201):831–9. https://doi.org/10.1016/s0140-6736(19)31773-8.
Griffiths CEM, Papp KA, Song M, et al. Continuous treatment with guselkumab maintains clinical responses through 4 years in patients with moderate-to-severe psoriasis: results from VOYAGE 1. J Dermatolog Treat. 2022;33(2):848–56. https://doi.org/10.1080/09546634.2020.1782817.
Camela E, Potestio L, Fabbrocini G, Pallotta S, Megna M. The holistic approach to psoriasis patients with comorbidities: the role of investigational drugs. Expert Opin Investig Drugs. 2023;32(6):537–52. https://doi.org/10.1080/13543784.2023.2219387.
Mahil SK, Wilson N, Dand N, et al. Psoriasis treat to target: defining outcomes in psoriasis using data from a real-world, population-based cohort study (the British Association of Dermatologists Biologics and Immunomodulators Register, BADBIR). Br J Dermatol. 2020;182(5):1158–66. https://doi.org/10.1111/bjd.18333.
Nielsen ML, Petersen TC, Maul JT, et al. Multivariable predictive models to identify the optimal biologic therapy for treatment of patients with psoriasis at the individual level. JAMA Dermatol. 2022;158(10):1149–56. https://doi.org/10.1001/jamadermatol.2022.3171.
Gerdes S, Zahl VA, Weichenthal M, Mrowietz U. Smoking and alcohol intake in severely affected patients with psoriasis in Germany. Dermatology. 2010;220(1):38–43. https://doi.org/10.1159/000265557.
Li W, Han J, Choi HK, Qureshi AA. Smoking and risk of incident psoriasis among women and men in the United States: a combined analysis. Am J Epidemiol. 2012;175(5):402–13. https://doi.org/10.1093/aje/kwr325.
Pezzolo E, Naldi L. The relationship between smoking, psoriasis and psoriatic arthritis. Expert Rev Clin Immunol. 2019;15(1):41–8. https://doi.org/10.1080/1744666x.2019.1543591.
Zhou H, Wu R, Kong Y, Zhao M, Su Y. Impact of smoking on psoriasis risk and treatment efficacy: a meta-analysis. J Int Med Res. 2020;48(11):1–20. https://doi.org/10.1177/0300060520964024.
Pinter A, Gerdes S, Papavassilis C, Reinhardt M. Characterization of responder groups to secukinumab treatment in moderate to severe plaque psoriasis. J Dermatolog Treat. 2020;31(8):769–75. https://doi.org/10.1080/09546634.2019.1626973.
Schakel K, Reich K, Asadullah K, et al. Early disease intervention with guselkumab in psoriasis leads to a higher rate of stable complete skin clearance ('clinical super response’): week 28 results from the ongoing phase IIIb randomized, double-blind, parallel-group, GUIDE study. J Eur Acad Dermatol Venereol. 2023;37(10):2016–27. https://doi.org/10.1111/jdv.19236.
Galluzzo M, Tofani L, Lombardo P, et al. Use of guselkumab for the treatment of moderate-to-severe plaque psoriasis: a 1 year real-life study. J Clin Med. 2020;9(7):2170. https://doi.org/10.3390/jcm9072170.
Hung YT, Lin YJ, Chiu HY, Huang YH. Impact of previous biologic use and body weight on the effectiveness of guselkumab in moderate-to-severe plaque psoriasis: a real-world practice. Ther Adv Chronic Dis. 2021;12:1–12. https://doi.org/10.1177/20406223211046685.
Al-Mutairi N, Nour T. The effect of weight reduction on treatment outcomes in obese patients with psoriasis on biologic therapy: a randomized controlled prospective trial. Expert Opin Biol Ther. 2014;14(6):749–56. https://doi.org/10.1517/14712598.2014.900541.
Jensen P, Zachariae C, Christensen R, et al. Effect of weight loss on the severity of psoriasis: a randomized clinical study. JAMA Dermatol. 2013;149(7):795–801. https://doi.org/10.1001/jamadermatol.2013.722.
Garcia-Doval I, Perez-Zafrilla B, Ferrandiz C, et al. Development of clinical prediction models for good or bad response to classic systemic drugs, anti-TNFs, and ustekinumab in psoriasis, based on the BIOBADADERM cohort. J Dermatolog Treat. 2016;27(3):203–9. https://doi.org/10.3109/09546634.2015.1088130.
Hoffmann JH, Knoop C, Enk AH, Hadaschik EN. Baseline anti-dsDNA concentrations and previous treatments predict response to adalimumab and etanercept: a retrospective investigation of 146 psoriasis patients. J Dermatol Sci. 2014;76(3):180–5. https://doi.org/10.1016/j.jdermsci.2014.09.003.
Umezawa Y, Saeki H, Nakagawa H. Some clinical factors affecting quality of the response to ustekinumab for psoriasis. J Dermatol. 2014;41(8):690–6. https://doi.org/10.1111/1346-8138.12538.
van Ee I, Deprez E, Egeberg A, et al. Freedom from disease in psoriasis: a Delphi consensus definition by patients, nurses and physicians. J Eur Acad Dermatol Venereol. 2022;36(3):403–12. https://doi.org/10.1111/jdv.17829.
Acknowledgements
We thank the participants of the study.
Medical Writing/Editorial Assistance
Medical writing and editorial support were provided by Madeleine Nowak, MSci, Lois Skellon, BSc, and Adam Lister, PhD, of Leonardo, an OPEN Health team, OPEN Health Communications, and funded by Janssen-Cilag in accordance with Good Publication Practice guidelines (www.ismpp.org/gpp-2022).
Funding
The ECLIPSE and VOYAGE 1 clinical trials were funded by Janssen-Cilag. For this manuscript, Janssen-Cilag funded medical writing and editorial support and the Open Access fee.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by JB and LA. The first draft of the manuscript was written by Madeleine Nowak, MSci, and all authors commented on all versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Alexander Egeberg has received research funding from AbbVie, Boehringer Ingelheim, Bristol Myers Squibb, the Danish National Psoriasis Foundation, Eli Lilly, Janssen Pharmaceuticals, the Kgl Hofbundtmager Aage Bang Foundation, Novartis, Pfizer, and the Simon Spies Foundation, and honoraria as consultant or speaker from AbbVie, Almirall, Boehringer Ingelheim, Bristol Myers Squibb, Dermavant, Eli Lilly, Galapagos NV, Galderma, Horizon Therapeutics, Janssen, LEO Pharma, Mylan, Novartis, Pfizer, Samsung Bioepis Co., Ltd., Sun Pharmaceuticals, UCB, Union Therapeutics, and Zuellig Pharma Ltd. Since the completion of this work, Alexander Egeberg has changed affiliation. His new affiliation is LEO Pharma A/S, Industriparken 55, DK-2750 Ballerup, Denmark. Curdin Conrad received research grants or served as a scientific adviser or clinical study investigator for AbbVie, Actelion, Almirall, Amgen, Boehringer Ingelheim, Bristol Myers Squibb, Celgene, Eli Lilly, Galderma, Incyte, Janssen, LEO Pharma, MSD, Novartis, Pfizer, Samsung, Sanofi, and UCB. Jozefien Buyze, Patricia Gorecki, and Sven Wegner are employees of Janssen; Sven Wegner holds stocks in Johnson & Johnson; Lorenzo Acciarri is an employee of Valos Srl, a Johnson & Johnson partner company. Diamant Thaçi has been a consultant, investigator, and speaker and participated in advisory boards for AbbVie, Almirall, Amgen, Biogen Idec, Bristol Myers Squibb, Janssen-Cilag, LEO Pharma, Lilly, Novartis, Pfizer, Regeneron, Sanofi, and UCB, and has received research/educational grants from AbbVie, LEO Pharma, Novartis, and Sanofi.
Ethical Approval
The ECLIPSE and VOYAGE 1 trials were sponsored by Janssen and conducted in accordance with the ethical principles derived from international guidelines, including the Declaration of Helsinki. An institutional review board or ethics committee approved the study protocol at participating sites.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Egeberg, A., Conrad, C., Gorecki, P. et al. Response Types and Factors Associated with Response Types to Biologic Therapies in Patients with Moderate-to-Severe Plaque Psoriasis from Two Randomized Clinical Trials. Dermatol Ther (Heidelb) 14, 745–758 (2024). https://doi.org/10.1007/s13555-024-01123-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-024-01123-1