Abstract
Introduction
Patients with moderate-to-severe plaque psoriasis who experience poor clinical outcomes, including patients with obesity or prior treatment, need improved treatment options. Risankizumab specifically inhibits interleukin 23 and has demonstrated superior efficacy in active-comparator studies in patients with moderate-to-severe plaque psoriasis. We compared the efficacy of risankizumab with that of secukinumab across patient subgroups.
Methods
Subgroup analyses using data from the phase 3 IMMerge study (NCT03478787) were performed. Efficacy in adults with moderate-to-severe psoriasis treated with risankizumab 150 mg and secukinumab 300 mg was assessed as the proportion of patients who achieved ≥ 90% improvement in Psoriasis Area Severity Index (PASI 90) at week 52 across demographics and disease characteristics. Post hoc analyses evaluated the proportion of patients who achieved PASI 90 and the least-squares mean percent PASI improvement from baseline at week 52 by body weight and body mass index (BMI), PASI 90 by prior treatment, and clinical response [PASI 90, PASI 100, and/or static Physician’s Global Assessment (sPGA) score of clear (0) or almost clear (1)] at week 16 and maintained particular response at week 52. Logistic regression analyses examined the effect of covariates (age, sex, BMI, baseline PASI, treatment) and potential interactions on PASI 90 at week 52.
Results
More patients who received risankizumab (n = 164) compared with secukinumab (n = 163) achieved PASI 90 at week 52, regardless of demographics and disease characteristics (BMI, prior treatment, disease duration, and maintenance of clinical response at week 52). Improvements in PASI were greater in patients taking risankizumab than those taking secukinumab, regardless of weight or BMI. Results from logistic regression analysis showed treatment type had a significant impact on PASI 90 (risankizumab versus secukinumab, p < 0.0001).
Conclusion
Risankizumab showed consistently greater efficacy compared with secukinumab across different patient subgroups, and this was maintained through 52 weeks.
Trial Registration
ClinicalTrials.gov identifier; NCT03478787.
Plain Language Summary
Patients with moderate-to-severe plaque psoriasis are often unable to achieve treatment success with currently available biologic therapies when they have other conditions, such as obesity, or have previous biologic therapy exposure and/or failure. We studied patients in the IMMerge phase 3 clinical trial (NCT03478787) to assess the efficacy of risankizumab compared with secukinumab for the treatment of plaque psoriasis and to determine risankizumab’s ability to remain effective after 52 weeks of administration. In our analysis, we looked across patient subgroups including patient body weight, body mass index, previous use of biologic therapies, length of time patients had been living with their disease, and the durability of risankizumab efficacy at 52 weeks. Results from our analysis showed that patients had greater success with risankizumab compared with secukinumab in treating their plaque psoriasis, despite their age, sex, race, and disease characteristics, and that risankizumab remained effective in treating plaque psoriasis at week 52. Previously reported safety results from the IMMerge clinical trial showed that there were no new concerns regarding side effects for either risankizumab or secukinumab. Overall, these results support the use of risankizumab to treat patients, including those who have other conditions or may not have had success with other therapies in treating their plaque psoriasis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Patients with plaque psoriasis and comorbidities, such as obesity, or those who have received prior biologic treatment, often have difficulty achieving high levels of efficacy using many of the current biologic therapies for moderate-to-severe psoriasis. |
Efficacious therapies are needed to provide adequate clinical benefit across a variety of patients, regardless of patient demographics and disease characteristics, including obesity, treatment history, and disease duration. |
This subanalysis of the IMMerge phase 3 clinical trial assessed risankizumab efficacy compared with secukinumab at week 52 across patient subgroups. Analyses included body weight, body mass index, prior biologic history, disease duration, and the durability of risankizumab efficacy at week 52. |
What was learned from the study? |
Risankizumab showed greater efficacy compared with secukinumab, regardless of patient demographics and disease characteristics, and efficacy was maintained at week 52. |
Results from this subgroup analysis support risankizumab treatment for a variety of patients, including those who are difficult to treat. |
Introduction
Plaque psoriasis is a common, chronic, immune-mediated inflammatory skin disorder in which approximately 100 million people worldwide [1] are impacted by physical, psychological, social, and economic burdens collectively referred to as cumulative life course impairment [2]. Patients with plaque psoriasis often have comorbidities, including obesity [body mass index (BMI) ≥ 30 kg/m2], that negatively affect treatment response [3,4,5,6]. Current biologic therapies for psoriasis, such as tumor necrosis factor (TNF) or interleukin (IL) 12/23 inhibitors, are associated with less favorable clinical outcomes among patients with comorbid obesity [3, 4, 7,8,9], a prior biologic treatment failure [5, 6, 10], or a longer disease duration [11]. Despite the availability of current therapies to treat moderate-to-severe psoriasis, there remains a need for efficacious treatments that provide long-term clinical benefit in a variety of patients, including those who are difficult to treat, regardless of patient demographics and disease characteristics.
The IL-23/IL-17 immune axis plays a key role in the development and maintenance of psoriasis [12, 13]. IL-23 aids in driving psoriasis by inducing the proliferation, differentiation, and maintenance of T-helper-17 and innate immune cells that produce proinflammatory cytokines, including IL-17 and IL-22, where reductions in these cytokines are observed in psoriatic lesions when inhibiting IL-23 [12, 14].
Risankizumab is a humanized immunoglobulin G1 monoclonal antibody that specifically inhibits IL-23 by binding its p19 subunit [15,16,17]. In patients with moderate-to-severe plaque psoriasis, risankizumab demonstrated superior efficacy compared with placebo [18, 19] and several systemic therapies in active-comparator studies, including fumaric acid esters [20], adalimumab [21], and ustekinumab [18]. While there are currently no head-to-head studies comparing IL-23–targeted agents, recent real-world evidence demonstrates favorable efficacy and safety in patients who received long-term IL-23 treatment during routine clinical practice [22,23,24]. Secukinumab is a fully human monoclonal antibody that inhibits IL-17A, and has shown greater skin clearance than ustekinumab, an inhibitor of IL-12 and IL-23 [25].
IMMerge was a phase 3, global, multicenter, randomized, open-label, efficacy-assessor-blinded, active-comparator study (NCT03478787) in which the efficacy and safety of risankizumab compared with secukinumab were examined in treating moderate-to-severe plaque psoriasis [26]. Risankizumab was non-inferior to secukinumab at week 16, with an 8.2% difference in the proportion of patients who achieved ≥ 90% improvement in Psoriasis Area and Severity Index (PASI 90) (within the predefined non-inferiority margin of 12%; primary endpoint), and was superior to secukinumab with an 29.8% efficacy gain based on proportions of patients achieving PASI 90 at week 52 (primary endpoint). Additionally, risankizumab was superior to secukinumab at week 52 in PASI 100 (100% improvement in PASI), static Physician’s Global Assessment (sPGA) score of clear (0) or almost clear (1), and PASI 75 (≥ 75% improvement in PASI; secondary endpoints). Overall, the safety profiles of risankizumab and secukinumab were consistent with those identified in other phase 3 clinical trials, and no new target-specific safety signals were identified. The aim of this analysis was to evaluate the efficacy of risankizumab compared with secukinumab from the phase 3 IMMerge study in subgroups of patients with moderate-to-severe plaque psoriasis based on key patient baseline demographics and disease characteristics (weight, BMI, prior psoriasis treatment history, and disease duration), and determine the maintenance of clinical response at week 52.
Methods
Study Design and Treatment
Details on study design and treatment were previously described by Warren et al. [26]. Briefly, the study consisted of a 30-day screening period, a 52-week open-label treatment period, and a 16-week follow-up period. Adult patients enrolled in the study had chronic, moderate-to-severe plaque psoriasis for at least 6 months, were candidates for systemic therapy, and had psoriasis plaques that covered at least 10% of their body surface area, an sPGA score of ≥ 3, and a PASI ≥ 12 at screening and baseline. Patients were excluded if they previously had erythrodermic psoriasis, generalized or localized pustular psoriasis, medication-induced or exacerbated psoriasis, or new-onset guttate psoriasis (or other active skin diseases). Eligible adults were randomized 1:1 to receive risankizumab 150 mg at weeks 0, 4, and every 12 weeks thereafter until the last dose at week 40, or secukinumab 300 mg at weeks 0, 1, 2, 3, 4, and every 4 weeks thereafter until the last dose at week 48 via subcutaneous injection. Patients randomized to risankizumab in France received two additional treatments at weeks 52 and 64 to provide continuous treatment until risankizumab was commercially available [26]. Randomization was stratified by baseline weight (≤ 100 kg versus > 100 kg) and exposure to prior biologic treatment (0 versus ≥ 1). Information on patients’ history of psoriasis, psoriatic arthritis, and prior and concomitant therapy was obtained via patient interview at screening and baseline. Patients identified with psoriatic arthritis either had a diagnosis or psoriatic arthritis was suspected. Further details describing treatment were previously published [26].
This study was performed in accordance with the Good Clinical Practice Guideline as defined by the International Conference on Harmonisation, the Declaration of Helsinki, and/or all applicable federal and local regulations and institutional review board mandates. All patients provided written informed consent.
Assessments
Efficacy
Subgroup analyses were performed on the primary endpoints for the following demographic and baseline characteristics subgroups: (1) age (years < 40, ≥ 40), (2) sex (male, female), (3) race (White, Non-White), smoking (current, former or never), (4) BMI (normal, < 25 kg/m2; overweight, ≥ 25 to < 30 kg/m2; obese, ≥ 30 kg/m2), (5) baseline PASI (≤ median, > median), (6) baseline sPGA (score of 3, score of 4), (7) psoriatic arthritis (yes, no), and (8) prior biologic treatment (0, ≥ 1). All subgroups except for the duration of plaque psoriasis were prespecified in the statistical analysis plan. Post hoc analyses were performed to examine the proportion of patients who achieved (1) PASI 90 and the least-squares (LS) mean percent PASI improvement from baseline at week 52 across BMI categories, weight categories, and weight quartiles; (2) PASI 90 at week 52 by type of prior biologic (IL-17, TNF, or IL-12/23 inhibitor); prior biologic failure (yes, no); and (3) PASI 90 at week 16 with this clinical response maintained at week 52, as assessed using three clinical outcome parameters (PASI 90, PASI 100, sPGA 0/1).
Safety
Safety was assessed for the duration of the study in the safety population by reporting treatment-emergent adverse events (TEAEs) and serious adverse events. Further details on safety assessments were previously described [26].
Statistical Analysis
Statistical analyses were performed using the intent-to-treat population that included all patients randomized at baseline, and the safety population that included all patients who received at least one dose of study drug. Missing efficacy data were addressed using nonresponder imputation for categorical variables and last observation carried forward for continuous variables. Categorical variables were assessed using the Cochran–Mantel–Haenszel test and adjusted for stratification by baseline weight (≤ 100 kg versus > 100 kg), and prior systemic biologics to treat psoriasis (0 versus ≥ 1). Between-treatment comparisons for BMI categories, weight categories, and weight quartiles were examined using the Cochran–Mantel–Haenszel test that was adjusted for randomization strata for dichotomous endpoints and analysis of covariance with randomization stratum, baseline value, and treatment as factors for continuous variables. The median time at which patients achieved clinical response (PASI 90, PASI 100, sPGA 0/1) with a 95% confidence interval (CI) when treated with either risankizumab or secukinumab was estimated using the Kaplan–Meier method; survival distributions between risankizumab and secukinumab were compared using a log-rank test. Logistic regression modeling was performed to investigate the effect of the five following covariates on PASI 90 at week 52 (model without interactions): (1) age (< 40 years, 40 to < 65 years, ≥ 65 years), (2) sex (male, female), (3) BMI (< 25 kg/m2, 25 to < 30 kg/m2, ≥ 30 kg/m2), (4) baseline PASI (≤ median, > median), and (5) treatment (risankizumab, secukinumab), and the potential interactions between BMI and age, BMI and sex, BMI and baseline PASI, age and sex, age and baseline PASI, and sex and baseline PASI (model with interactions). Logistic regression with Bonferroni adjustment was performed to address multiplicity [27, 28]. Other subgroup analyses were univariate analyses without multiplicity adjustments [27]. Statistical analyses were performed using SAS version 9.4 (SAS Institute, Inc., Cary, NC, USA) using the UNIX operating system.
Results
Patients
Of 409 patients screened, 327 were randomized to receive risankizumab (n = 164) or secukinumab (n = 163) (Table 1). Demographics and baseline characteristics were similar between treatment groups (Table 1). Overall, most patients were male (65%), the mean [standard deviation (SD)] patient age was 47.1 (14.1) years, and the mean (SD) weight was 91.5 (24.7) kg. Patients had a mean (SD) baseline PASI of 19.9 (7.2), and the majority (84.7%) had a baseline sPGA score of 3. In total, 120 patients (36.7%) received prior biologic treatment for psoriasis, and 50 (15.3%) had a history of psoriatic arthritis. In total, 312 (95.4%) patients completed week 16 of the study, and 286 (87.5%) completed week 52 [risankizumab group, 151 (92.1%); secukinumab group, 135 (82.8%)].
Efficacy Assessments
In all patient subgroups, a numerically greater proportion of patients treated with risankizumab achieved PASI 90 at week 52 compared with patients treated with secukinumab (risankizumab, 74.1–92.3%; secukinumab, 46.8–65.0%; Fig. 1). When treated with secukinumab, numerically greater proportions of patients achieved PASI 90 who were aged < 40 years (< 40, 65.0% versus ≥ 40, 52.4%), male (male, 63.4% versus female, 46.8%), had a BMI < 25 kg/m2 or 25 kg/m2 to < 30 kg/m2 (< 25 kg/m2, 64.9%, or 25 kg/m2 to < 30 kg/m2, 63.8% versus ≥ 30 kg/m2, 49.4%), or who did not have prior biologic treatment (no prior biologic, 61.0% versus prior biologic, 50.0%). A greater proportion of patients who had more severe disease [PASI > median (18.0); sPGA of severe (score of 4)] or who had a shorter duration of plaque psoriasis [≤ median (15.6) years] compared with patients with less severe disease or who had longer disease duration at baseline achieved PASI 90 when treated with either risankizumab or secukinumab.
Proportion of patients who achieved PASI 90 at week 52 by baseline demographics and disease characteristic subgroups (intent-to-treat population). BMI body mass index, PASI Psoriasis Area and Severity Index; PASI 90 ≥ 90% improvement in PASI, sPGA static Physician’s Global Assessment, 95% CI 95% confidence interval. aDuration of plaque psoriasis was not prespecified in the statistical analysis plan
Adjusted by important patient characteristics, logistic regression modeling showed treatment type (risankizumab versus secukinumab) had a significant impact on the proportion of patients who achieved PASI 90 at week 52 (p < 0.0001). PASI 90 was not significantly impacted by the covariates age, sex, BMI, and baseline PASI (p > 0.05) (Table S1) or their interactions (p > 0.05 for all interaction values).
PASI 90 was achieved by more patients at week 52 who were treated with risankizumab compared with patients receiving secukinumab, regardless of BMI (risankizumab, 84.6–88.9%; secukinumab, 49.4–64.9%; p < 0.05), body weight (risankizumab, 85.7–88.5%; secukinumab, 44.4–63.3%; p < 0.001), or weight quartiles (risankizumab, 78.0–92.5%; secukinumab, 42.9–66.7%; p < 0.05; Fig. 2a). Patients receiving risankizumab had statistically greater improvement in PASI LS mean percent change from baseline at week 52 across BMI categories, weight categories, and weight quartiles compared with patients receiving secukinumab (risankizumab versus secukinumab; p < 0.05 for all; Fig. 2b).
Proportion of patients who achieved PASI 90 at week 52 by BMI categories, weight categories, and weight quartiles (NRI) (a), and with improvement in PASI 90 as LS mean percent change from baseline at week 52 (LOCF) (b). *p < 0.05, **p < 0.01,***p < 0.001 versus secukinumab. BMI body mass index, LS least squares, LOCF last observation carried forward, NRI nonresponder imputation, PASI 90 ≥ 90% improvement in Psoriasis Area and Severity Index, 95% CI 95% confidence interval
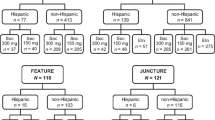
A greater proportion of patients treated with risankizumab achieved PASI 90 at week 52 than did patients treated with secukinumab, regardless of prior use of biologics (risankizumab, 85.5–87.3% versus secukinumab, 50.0–61.0%; Fig. 3a). Among patients treated with risankizumab, a numerically similar proportion of patients achieved PASI 90 despite having received prior treatment or not (prior treatment, 85.5% versus no prior treatment, 87.3%). Fewer patients receiving secukinumab achieved PASI 90 among those who had used biologic treatment in the past compared with those who had not (50.0% versus 61.0%). More patients treated with risankizumab achieved PASI 90, regardless of prior biologic treatment class (IL-17, TNF, or IL-12/23 inhibitors) compared with patients treated with secukinumab (risankizumab, 78.9–93.3% versus secukinumab, 42.1–50.0%; Fig. 3b). More patients who had experienced prior treatment failure and received risankizumab achieved PASI 90 compared with those who had experienced prior treatment failure and had received secukinumab (72.7% versus 27.3%; Fig. 3c). Similar results were observed for patients without treatment failure (risankizumab, 88.2% versus secukinumab, 55.3%). For both treatment groups, smaller proportions of patients achieved PASI 90 who experienced prior treatment failure compared with those who did not (prior failure: risankizumab, 72.7%; secukinumab, 27.3% versus no prior failure: risankizumab, 88.2%; secukinumab, 55.3%).
More patients treated with risankizumab who achieved a clinical response (PASI 90, PASI 100, and/or sPGA 0/1) at week 16 maintained a clinical response at week 52 than did patients receiving secukinumab (risankizumab, 81.9–90.9% versus secukinumab, 67.9–81.3%; Fig. 4). The times to reach PASI 90 and sPGA 0/1 were not statistically different between treatment groups [PASI 90: risankizumab, 12.0 weeks (median), secukinumab, 8.6 weeks (median), p = 0.151; sPGA 0/1: risankizumab, 8.1 weeks (median); secukinumab, 4.4 weeks (median), p = 0.911]; however, patients treated with risankizumab who achieved PASI 100 did so in a significantly shorter time compared with patients treated with secukinumab (median: risankizumab, 20.0 weeks; secukinumab, 28.1 weeks; p < 0.001; Fig. S1a). Between weeks 16 and 52, patients treated with risankizumab maintained clinical response (PASI 90, PASI 100, and/or sPGA 0/1) at more visits than did patients treated with risankizumab compared with patients treated with secukinumab (Fig. S1b).
Clinical response maintenance at week 52 for patients who achieved PASI 90 at week 16 and maintained their clinical response at week 52 (NRI). NRI nonresponder imputation, PASI 90/100 ≥ 90%/100% improvement in Psoriasis Area and Severity Index, sPGA 0/1 static Physician’s Global Assessment of clear (0) or almost clear (1)
Safety
Results from the safety analysis were previously reported by Warren et al. [26]. Overall, the proportions of patients reporting any TEAEs were similar between the risankizumab (71.3%) and secukinumab (71.2%) treatment groups. The most frequently reported TEAEs were nasopharyngitis (risankizumab, 21.3%; secukinumab, 16.6%), and upper respiratory tract infection (risankizumab, 12.8%; secukinumab, 8.6%). Oral or vulvovaginal candida infections were reported by three patients in the risankizumab group and by four patients in the secukinumab group. As described previously, one patient in the secukinumab group reported a new case of inflammatory bowel disease (ulcerative colitis) that was serious and considered related to the treatment, which led to discontinuation of treatment [26]. AEs leading to treatment discontinuation were less frequent in patients treated with risankizumab (1.2%) compared with patients treated with secukinumab (4.9%).
Discussion
In this subgroup analysis of data from the phase 3 IMMerge study, risankizumab showed greater efficacy numerically compared with secukinumab, regardless of baseline demographics and disease characteristics. The clinical response to risankizumab remained consistent across all patient subgroups evaluated, including age, sex, and baseline disease severity, and was similar to that observed in the general study population [26] and to an integrated analysis conducted in subgroups comparing risankizumab and ustekinumab published previously [27]. Among patients treated with secukinumab, clinical response varied most prominently by age, BMI, and prior treatment subgroups. Numerically more patients achieved PASI 90 who were aged < 40 years, male, had lower BMI (< 30 kg/m2), or did not have prior biologic treatment, though there were no statistical differences between subgroups. Results from logistic regression analysis showed that age, sex, BMI, and baseline PASI did not significantly influence clinical outcome; however, treatment (risankizumab versus secukinumab) significantly impacted the proportion of patients achieving PASI 90 at week 52. As shown previously, the efficacy of risankizumab was non-inferior to that of secukinumab at week 16 and was superior to secukinumab at week 52. Regarding safety, both risankizumab and secukinumab were well tolerated over the 52 weeks of treatment [26].
In general, obesity is negatively associated with treatment response for plaque psoriasis [3, 4, 7, 8], in which achievement of lower treatment response (e.g., PASI 75) is often reported for patients with greater body weights (e.g., ≥ 90 kg) compared with patients who weighed less when treated with fixed-dose biologics [29,30,31,32,33,34]. As a result, adjustments to dose or dosing frequency for patients with greater body weight to optimize efficacy for some drugs, including secukinumab, have been evaluated [9, 35, 36].
Obtaining insurance approval for higher doses of biologics or more frequent dosing for patients with higher body weight is often difficult due to the fixed doses approved by regulatory agencies. Regardless of weight or BMI, greater proportions of patients treated with risankizumab achieved clinical improvement at week 52 compared with patients treated with secukinumab. Additionally, clinical response was more consistent across body weights in patients treated with risankizumab compared with patients in the secukinumab group. These results highlight that risankizumab was efficacious in patients with greater body weights or BMI, and dosing adjustments were not required.
Medication adjustments, including switching therapies, may be required to maintain adequate control of plaque psoriasis for patients who discontinue their first biologic because of treatment failure caused from unsatisfactory treatment responses, or loss of treatment efficacy over time [37,38,39]. It is imperative that these second- or third-line biologics are not impacted by the patient’s prior treatment history, show durability over time, and have an adequate time to treatment response. However, lower efficacy was reported for patients who have had prior treatment history including previous treatment failure [5, 6], and many biologics have been discontinued over time [39]. Additionally, longer disease duration was shown to be a negative predictor of clinical outcomes with other biologics [11]. We showed that, regardless of prior biologic use, including type and prior failure, more patients achieve PASI 90 at week 52 when treated with risankizumab compared with those patients treated with secukinumab. This was true even for patients previously treated with an IL-12/23 inhibitor. Similarly, preliminary results from a 16-week retrospective study showed patients with moderate-to-severe plaque psoriasis who previously failed IL-17, IL-12/23, and/or IL-23 inhibitors benefited from risankizumab treatment during routine clinical practice, regardless of previous biologic use [40]. A larger phase 3b study evaluating risankizumab in patients who have had a suboptimal response to secukinumab or ixekizumab is ongoing [41]. Additionally, we showed that more patients with a long duration of disease [> 15.6 (median) years] achieved a clinical response with risankizumab than with secukinumab. More patients who achieved clinical response with risankizumab at week 16 maintained this benefit at week 52 compared with patients treated with secukinumab, showing the durability of risankizumab efficacy. Lastly, we showed that the times to achieve PASI 90 or sPGA 0/1 were not different between treatment groups, and patients treated with risankizumab reached PASI 100 significantly faster compared with patients treated with secukinumab.
Some of the potential limitations of this study include the single-blind (assessor) design and differences in the timing of the last dose, which were discussed in the primary report [26]. Additionally, this is a post hoc analysis of the primary clinical trial data; duration of plaque psoriasis was the only subgroup analysis that was not prespecified in the statistical analysis plan. This study did utilize logistic regression analyses to better mimic routine clinical practice. The logistic regression analysis was used to determine which variables, including age, sex, BMI, and baseline PASI, and their possible interactions were predictive of treatment response; however, clinical variables, such as prior treatment or duration of plaque psoriasis, were not included, and the small sample size of PASI 90 may limit the power to identify a clinical predictive factor. Future analyses can evaluate effectiveness, durability, and safety of risankizumab versus secukinumab for various patient subgroups in the real-world setting.
Conclusions
Overall, risankizumab showed greater efficacy compared with secukinumab consistently across different patient groups, regardless of baseline demographics and disease characteristics, including BMI, treatment history, and disease duration, which was maintained at 52 weeks. These data showed risankizumab is a durable treatment for plaque psoriasis across many patients, including those with greater body weight and those who have had less than adequate response to other biologics.
References
World Health Organization. Global report on psoriasis. Geneva, Switzerland: World Health Organization; 2016. Accessed May 6, 2020. https://www.who.int/publications/i/item/global-report-on-psoriasis.
Warren RB, Kleyn CE, Gulliver WP. Cumulative life course impairment in psoriasis: patient perception of disease-related impairment throughout the life course. Br J Dermatol. 2011;164(suppl 1):1–14.
Bremmer S, Van Voorhees AS, Hsu S, Korman NJ, Lebwohl MG, Young M, et al. Obesity and psoriasis: from the Medical Board of the National Psoriasis Foundation. J Am Acad Dermatol. 2010;63(6):1058–69.
Armstrong AW, Harskamp CT, Armstrong EJ. The association between psoriasis and obesity: a systematic review and meta-analysis of observational studies. Nutr Diabetes. 2012;2:e54. https://doi.org/10.1038/nutd.2012.26.
Mazzotta A, Esposito M, Costanzo A, Chimenti S. Efficacy and safety of etanercept in psoriasis after switching from other treatments: an observational study. Am J Clin Dermatol. 2009;10(5):319–24.
Papp KA, Gordon KB, Langley RG, Lebwohl MG, Gottlieb AB, Rastogi S, et al. Impact of previous biologic use on the efficacy and safety of brodalumab and ustekinumab in patients with moderate-to-severe plaque psoriasis: integrated analysis of the randomized controlled trials AMAGINE-2 and AMAGINE-3. Br J Dermatol. 2018;179(2):320–8.
Chiricozzi A, Gisondi P, Girolomoni G. The pharmacological management of patients with comorbid psoriasis and obesity. Expert Opin Pharmacother. 2019;20(7):863–72.
Takeshita J, Grewal S, Langan SM, Mehta NN, Ogdie A, Van Voorhees AS, et al. Psoriasis and comorbid diseases: epidemiology. J Am Acad Dermatol. 2017;76(3):377–90.
Lebwohl M, Yeilding N, Szapary P, Wang Y, Li S, Zhu Y, et al. Impact of weight on the efficacy and safety of ustekinumab in patients with moderate to severe psoriasis: rationale for dosing recommendations. J Am Acad Dermatol. 2010;63(4):571–9.
Menter A, Papp KA, Gooderham M, Pariser DM, Augustin M, Kerdel FA, et al. Drug survival of biologic therapy in a large, disease-based registry of patients with psoriasis: results from the Psoriasis Longitudinal Assessment and Registry (PSOLAR). J Eur Acad Dermatol Venereol. 2016;30(7):1148–58.
Papp KA, Langley RG, Lebwohl M, Krueger GG, Szapary P, Yeilding N, et al. Efficacy and safety of ustekinumab, a human interleukin-12/23 monoclonal antibody, in patients with psoriasis: 52-week results from a randomised, double-blind, placebo-controlled trial (PHOENIX 2). Lancet. 2008;371(9625):1675–84.
Puig L. The role of IL 23 in the treatment of psoriasis. Expert Rev Clin Immunol. 2017;13(6):525–34.
Gooderham MJ, Papp KA, Lynde CW. Shifting the focus—the primary role of IL-23 in psoriasis and other inflammatory disorders. J Eur Acad Dermatol Venereol. 2018;32(7):1111–9.
Gaffen SL, Jain R, Garg AV, Cua DJ. The IL-23-IL-17 immune axis: from mechanisms to therapeutic testing. Nat Rev Immunol. 2014;14(9):585–600.
Krueger JG, Ferris LK, Menter A, Wagner F, White A, Visvanathan S, et al. Anti-IL-23A mAb BI 655066 for treatment of moderate-to-severe psoriasis: safety, efficacy, pharmacokinetics, and biomarker results of a single-rising-dose, randomized, double-blind, placebo-controlled trial. J Allergy Clin Immunol. 2015;136(1):116-24.e7.
Singh S, Kroe-Barrett RR, Canada KA, Zhu X, Sepulveda E, Wu H, et al. Selective targeting of the IL23 pathway: generation and characterization of a novel high-affinity humanized anti-IL23A antibody. MAbs. 2015;7(4):778–91.
SKYRIZI. Prescribing information. AbbVie Inc.; 2021. https://www.rxabbvie.com/pdf/skyrizi_pi.pdf. Accessed July1, 2021.
Gordon KB, Strober B, Lebwohl M, Augustin M, Blauvelt A, Poulin Y, et al. Efficacy and safety of risankizumab in moderate-to-severe plaque psoriasis (UltIMMa-1 and UltIMMa-2): results from two double-blind, randomised, placebo-controlled and ustekinumab-controlled phase 3 trials. Lancet. 2018;392(10148):650–61.
Ohtsuki M, Fujita H, Watanabe M, Suzaki K, Flack M, Huang X, et al. Efficacy and safety of risankizumab in Japanese patients with moderate to severe plaque psoriasis: results from the SustaIMM phase 2/3 trial. J Dermatol. 2019;46(8):686–94.
Thaçi D, Eyerich K, Pinter A, Sebastian M, Unnebrink K, Rubant S, et al. Direct comparison of risankizumab and fumaric acid esters in systemic-therapy-naive patients with moderate to severe plaque psoriasis: a randomized controlled trial. Br J Dermatol. 2021. https://doi.org/10.1111/bjd.20481 (Published online May 15, 2021).
Reich K, Gooderham M, Thaçi D, Crowley JJ, Ryan C, Krueger JG, et al. Risankizumab compared with adalimumab in patients with moderate-to-severe plaque psoriasis (IMMvent): a randomised, double-blind, active-comparator-controlled phase 3 trial. Lancet. 2019;394(10198):576–86.
Ruggiero A, Fabbrocini G, Cinelli E, Megna M. Guselkumab and risankizumab for psoriasis: a 44-week indirect real-life comparison. J Am Acad Dermatol. 2021;85(4):1028–30.
Gkalpakiotis S, Cetkovska P, Arenberger P, Dolezal T, Arenbergerova M, Velackova B, et al. Risankizumab for the treatment of moderate-to-severe psoriasis: real-life multicenter experience from the Czech Republic. Dermatol Ther (Heidelb). 2021;11(4):1345–55.
Hansel K, Zangrilli A, Bianchi L, Peris K, Chiricozzi A, Offidani A et al. A 52-week update of a multicentre real-life experience on effectiveness and safety of risankizumab in psoriasis. J Eur Acad Dermatol Venereol. 2021.
Blauvelt A, Reich K, Tsai T-F, Tyring S, Vanaclocha F, Kingo K, et al. Secukinumab is superior to ustekinumab in clearing skin of subjects with moderate-to-severe plaque psoriasis up to 1 year: results from the CLEAR study. J Am Acad Dermatol. 2017;76(1):60-9.e9.
Warren RB, Blauvelt A, Poulin Y, Beeck S, Kelly M, Wu T, et al. Efficacy and safety of risankizumab vs secukinumab in patients with moderate-to-severe plaque psoriasis (IMMerge): results from a phase III, randomized, open-label, efficacy-assessor-blinded clinical trial. Br J Dermatol. 2021;184(1):50–9.
Strober B, Menter A, Leonardi C, Gordon K, Lambert J, Puig L, et al. Efficacy of risankizumab in patients with moderate-to-severe plaque psoriasis by baseline demographics, disease characteristics and prior biologic therapy: an integrated analysis of the phase III UltIMMa-1 and UltIMMa-2 studies. J Eur Acad Dermatol Venereol. 2020;34(12):2830–8.
Dmitrienko A, D’Agostino RB Sr. Multiplicity considerations in clinical trials. N Engl J Med. 2018;378(22):2115–22.
Gordon K, Korman N, Frankel E, Wang H, Jahreis A, Zitnik R, et al. Efficacy of etanercept in an integrated multistudy database of patients with psoriasis. J Am Acad Dermatol. 2006;54(3 Suppl 2):S101–11.
Naldi L, Addis A, Chimenti S, Giannetti A, Picardo M, Tomino C, et al. Impact of body mass index and obesity on clinical response to systemic treatment for psoriasis. Evidence from the Psocare project. Dermatology. 2008;217(4):365–73.
Clark L, Lebwohl M. The effect of weight on the efficacy of biologic therapy in patients with psoriasis. J Am Acad Dermatol. 2008;58(3):443–6.
Papp KA, Langley RG, Sigurgeirsson B, Abe M, Baker DR, Konno P, et al. Efficacy and safety of secukinumab in the treatment of moderate-to-severe plaque psoriasis: a randomized, double-blind, placebo-controlled phase II dose-ranging study. Br J Dermatol. 2013;168(2):412–21.
Singh S, Facciorusso A, Singh AG, Vande Casteele N, Zarrinpar A, Prokop LJ, et al. Obesity and response to anti-tumor necrosis factor-alpha agents in patients with select immune-mediated inflammatory diseases: a systematic review and meta-analysis. PLoS ONE. 2018;13(5): e0195123. https://doi.org/10.1371/journal.pone.
Papp KA, Reich K, Blauvelt A, Kimball AB, Gooderham M, Tyring SK, et al. Efficacy of tildrakizumab for moderate-to-severe plaque psoriasis: pooled analysis of three randomized controlled trials at weeks 12 and 28. J Eur Acad Dermatol Venereol. 2019;33(6):1098–106.
Lee JE, Wang J, Florian J, Wang YM, Kettl D, Marcus K, et al. Effect of body weight on risk-benefit and dosing regimen recommendation of secukinumab for the treatment of moderate to severe plaque psoriasis. Clin Pharmacol Ther. 2019;106(1):78–80.
Reich K, Puig L, Szepietowski JC, Paul C, Lacour JP, Tsianakas A, et al. Secukinumab dosing optimization in patients with moderate-to-severe plaque psoriasis: results from the randomized, open-label OPTIMISE study. Br J Dermatol. 2020;182(2):304–15.
Feldman SR, Zhao Y, Navaratnam P, Friedman HS, Lu J, Tran MH. Patterns of medication utilization and costs associated with the use of etanercept, adalimumab, and ustekinumab in the management of moderate-to-severe psoriasis. J Manag Care Spec Pharm. 2015;21(3):201–9.
Menter A, Strober BE, Kaplan DH, Kivelevitch D, Prater EF, Stoff B, et al. Joint AAD–NPF guidelines of care for the management and treatment of psoriasis with biologics. J Am Acad Dermatol. 2019;80(4):1029–72.
Warren RB, Smith CH, Yiu ZZN, Ashcroft DM, Barker J, Burden AD, et al. Differential drug survival of biologic therapies for the treatment of psoriasis: a prospective observational cohort study from the British Association of Dermatologists Biologic Interventions Register (BADBIR). J Invest Dermatol. 2015;135(11):2632–40.
Megna M, Fabbrocini G, Ruggiero A, Cinelli E. Efficacy and safety of risankizumab in psoriasis patients who failed anti-IL-17, anti-12/23 and/or anti IL-23: preliminary data of a real-life 16-week retrospective study. Dermatol Ther. 2020;33(6):e14144.
A study of the safety and efficacy of risankizumab in adult participants with plaque psoriasis who have had a suboptimal response to secukinumab or ixekizumab. ClinicalTrials.gov identifier: NCT04102007 [Internet]. Available from: https://ClinicalTrials.gov/show/NCT04102007. Cited 10 Dec 2021.
Acknowledgements
AbbVie and the authors thank the patients who participated in this clinical trial and all the study investigators for their contributions
Funding
AbbVie Inc. participated in the study design; study research; collection, analysis, and interpretation of data; and writing, reviewing, and approving this manuscript for publication. AbbVie funded the research for this study, paid for Rapid Service Fees to Dermatology and Therapy, and provided writing support for this manuscript.
Medical Writing Assistance
Medical writing assistance, funded by AbbVie, was provided by Marion France, PhD, of JB Ashtin.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published. No honoraria or payments were made for authorship.
Author Contributions
JJC, RL, KBG, AP, LF, and RBW contributed to data acquisition. ZX, TW, and TZ contributed to statistical analysis. All authors contributed to the study design and data interpretation, critically reviewed this manuscript, and provided final approval for publication.
Prior Presentation
The results presented here were previously presented virtually at the 29th European Academy of Dermatology and Venereology Congress, October 29 to 31, 2020, and virtually at the Fall Clinical Dermatology Conference, October 29 to November 1, 2020.
Disclosures
Jeffrey J. Crowley has received research/grant support from AbbVie, Amgen, Arcutis, Boehringer Ingelheim, Janssen, Lilly, MC2 Therapeutics, Merck, Novartis, Pfizer, Regeneron, Sandoz, Sanofi, Sun Pharma, UCB, and Verrica. He has served as a consultant for AbbVie, Amgen, Arcutis, Arena Pharmaceuticals, Boehringer Ingelheim, Bristol Myers Squibb, Celgene, Dermira, Lilly, Novartis, Sun Pharma, and UCB, and has worked on speakers’ bureaus for AbbVie, Janssen, Lilly, Novartis, Regeneron, Sanofi, and UCB. Richard G. Langley has served as principal investigator for and is a paid member of scientific advisory boards or served as a speaker for AbbVie, Amgen, Boehringer Ingelheim, Celgene, Janssen, LEO Pharma, Lilly, Merck, Novartis, Pfizer, and UCB. Kenneth B. Gordon has received research/grant support from AbbVie, Bristol Myers Squibb, Celgene, Janssen, Lilly, and Novartis. He has served as a consultant for or received honoraria from AbbVie, Almirall, Amgen, Bristol Myers Squibb, Celgene, Dermavant, Dermira, Janssen, Kyowa Kirin, LEO Pharma, Lilly, Novartis, Pfizer, Ortho Dermatologics, Sun Pharma, and UCB. Andreas Pinter has worked as an investigator and/or speaker and/or advisor for AbbVie, Amgen, Biogen, BioNTec, Boehringer Ingelheim, Celgene, GlaxoSmithKline, Galderma, Hexal, Janssen, LEO Pharma, Lilly, MC2 Therapeutics, Medac, Merck, Mitsubishi Tanabe Pharma, Novartis, Pascoe, Pfizer, Tigercat Pharma, Regeneron, Roche, Sandoz, Sanofi Genzyme, Schering-Plough, and UCB. Laura K. Ferris has received consulting fees from AbbVie, Arcutis, Bristol Myers Squibb, Dermavant, Lilly, Janssen, and Pfizer, and has been an investigator for AbbVie, Arcutis, Bristol Myers Squibb, Celgene/Amgen, Dermavant, Galderma, Janssen, LEO Pharma, Novartis, and Regeneron. Simone Rubant, Huzefa Photowala, Zhenyi Xue, Tianshuang Wu, Tianyu Zhan, Stefan Beeck, and Megha Shah are full-time employees of AbbVie, Inc. and may hold AbbVie stock and/or stock options. Richard B. Warren has received research grants from and leads clinical trials for AbbVie, Almirall, Amgen, Bristol Myers Squibb, Celgene, Lilly, Janssen, LEO Pharma, Novartis, Pfizer, and UCB. He has received consulting fees from AbbVie, Almirall, Amgen, Arena Pharmaceuticals, Avillion, Boehringer Ingelheim, Bristol Myers Squibb, Celgene, Janssen, LEO Pharma, Lilly, Novartis, Pfizer, Sanofi, and UCB, and is supported by the Manchester NIHR Biomedical Research Centre.
Compliance with Ethics Guidelines
This study was performed in accordance with the Good Clinical Practice Guideline as defined by the International Conference on Harmonisation, the Declaration of Helsinki, and/or all applicable federal and local regulation and institutional review board mandates. All patients provided written informed consent.
Data Availability
AbbVie is committed to responsible data sharing regarding the clinical trials we sponsor. This includes access to anonymized, individual, and trial-level data (analysis data sets), as well as other information (eg, protocols and clinical study reports), as long as the trials are not part of an ongoing or planned regulatory submission. This includes requests for clinical trial data for unlicensed products and indications. This clinical trial data can be requested by any qualified researchers who engage in rigorous, independent scientific research, and will be provided following review and approval of a research proposal and statistical analysis plan and execution of a data sharing agreement. Data requests can be submitted at any time and the data will be accessible for 12 months, with possible extensions considered. For more information on the process, or to submit a request, visit the following link: https://www.abbvie.com/our-science/clinical-trials/clinical-trials-data-and-information-sharing/data-and-information-sharing-with-qualified-researchers.html.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Crowley, J.J., Langley, R.G., Gordon, K.B. et al. Efficacy of Risankizumab versus Secukinumab in Patients with Moderate-to-Severe Psoriasis: Subgroup Analysis from the IMMerge Study. Dermatol Ther (Heidelb) 12, 561–575 (2022). https://doi.org/10.1007/s13555-021-00679-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-021-00679-6