Abstract
Schwartz-Jampel syndrome (SJS) is a rare autosomal recessive disorder characterized by typical facial dysmorphism, generalized muscle stiffness, joint contracture, and skeletal abnormalities. This condition is caused by mutations in the heparan sulfate proteoglycan 2 (HSPG2) gene, which encodes perlecan, a component of the basement membrane. The management of patients with SJS primarily aims to alleviate symptoms related to muscle stiffness. In this report, we describe a male patient with SJS type 1A. Trio whole-exome sequencing identified a pathogenic mutation (NM_001291860.1: c.10897C>T; p.Arg3633Ter) and variants of unknown significance (NM_001291860.2: c.413+10G>T). The patient experienced difficulty in opening his eyes and mouth, which significantly limited his daily activities. Botulinum toxin A injection was administered and demonstrated significant clinical improvement after the treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Schwartz-Jampel syndrome (SJS) is a rare autosomal recessive disorder characterized by typical facial dysmorphism, generalized muscle stiffness, joint contracture, and skeletal abnormalities. |
The ultimate goal of treatment is to minimize abnormal muscle activity, which causes stiffness and cramping. |
Pharmacologic treatment, including mexiletine, carbamazepine, lamotrigine, and flecainide, is commonly used to reduce myotonic symptoms. Botulinum toxin A (BTX-A) injection can also be used and demonstrated significant clinical improvement after the treatment to relieve facial blepharospasm. However, the optimal doses and intervals must be individually tailored to optimize symptom control. |
When treating pediatric patients, the use of an injector should minimize the dosage of BTX-A administered during each treatment session to prevent the side effects. |
Introduction
Schwartz-Jampel syndrome (SJS, OMIM #255800) was first documented in 1962 and is characterized by congenital blepharophimosis, distinctive facies, muscle stiffness, and joint deformities, also known as myotonic chondrodystrophy [1]. SJS is an uncommon autosomal recessive disorder caused by mutations in the heparan sulfate proteoglycan 2 (HSPG2) gene, situated on chromosome 1p34-36 [2]. These mutations lead to defects in the perlecan protein, encoded by the HSPG2 gene, resulting in abnormal cartilage development and anomalous neuromuscular activity.
The primary objective of SJS treatment is symptomatic management, focusing on specific symptoms and potential complications of the disease. The ultimate goal is to minimize abnormal muscle activity, which causes stiffness and cramping. Pharmacologic treatment, including mexiletine, carbamazepine, lamotrigine, and flecainide, is commonly used to reduce myotonic symptoms [3]. Non-pharmacologic modalities, such as warming, massage, pre-exercise warm-up, and gradual stretching combined with medications, have also been reported [1]. Surgical techniques, such as myectomy, levator resection, and lateral canthopexy, offer excellent and long-lasting relief for blepharospasm and eyelid anomalies [4]. However, the presence of jaw muscle tightness, bony deformities, and the risk of malignant hyperthermia may increase surgical complications [5]. Botulinum toxin A (BTX-A) is widely accepted as the principal therapy for blepharospasm and other facial dystonias [6, 7]. Additionally, BTX-A has been reported as a therapeutic option for patients with SJS, although appropriate dosing may vary [8]. In this report, we describe the comprehensive clinical presentation of a patient with genetically confirmed SJS who achieved successful treatment with BTX-A.
Case Presentation
A 20-month-old Thai boy presented with a history of difficulty walking, abnormal gait, and muscle stiffening since the age of 1 year. He was born full-term to non-consanguineous parents without any complications and began walking at approximately 1 year old. Physical examination revealed several notable findings, including short stature (height < 3rd percentile), low weight (< 3rd percentile), and a normal head circumference (10th–25th percentiles). Distinctive facial features were observed, characterized by a fixed facial expression, narrow palpebral fissure, pursed lips, small mandible, pucker chin, and a high-pitched voice. Generalized muscle stiffening, hypertonia, and depressed reflexes were also noted. At that time, electromyography (EMG) was not performed because of its unavailability.
Written informed consent has been obtained from the patient’s parents for publication.
Skeletal radiographs taken at the age of 9 years displayed specific abnormalities, including sclerotic sacroiliac joints, retroposition of the femoral neck, and mild widening of the metaphysis of the humerus (Fig. 1). On the basis of the clinical presentation and findings, the patient was diagnosed with Schwartz-Jampel Syndrome (SJS) type 1A. At the age of 11, he underwent orthopedic surgery as a result of severe femoral retrotorsion.
Further evaluation was initiated to address his short stature, which led to an endocrinology evaluation at the age of 4 years. The evaluation revealed a low level of free thyroxine (free T4 = 0.915 ng/dl) and a normal thyroid-stimulating hormone level (TSH = 2.43 mIU/ml). Consequently, the patient was placed on Eltroxin for central hypothyroidism. Later, at the age of 7, he was diagnosed with obstructive sleep apnea on the basis of polysomnography findings (apnea–hypopnea index = 29). Continuous positive airway pressure was introduced to manage the condition.
The patient’s cognitive function was assessed using the Wechsler Intelligence Scale of Children-Third edition (WISC-III), which yielded a full-scale intelligence quotient (IQ) of 93, verbal IQ score of 90, and performance IQ score of 98. Since the age of 3, he had been prescribed carbamazepine and phenytoin, which effectively alleviated his myotonic symptoms. However, over time, his myotonia worsened, leading to difficulty in opening his mouth and eyes, significantly impacting his daily activities, including eating and attending school.
To elucidate the underlying cause of the myotonia, trio whole exome sequencing was performed. This involved capturing all exon regions of human genes using the xGen Exome Research Panel v2 (Integrated DNA Technologies, Coralville, Iowa, USA) and sequencing the captured regions with Novaseq 6000 (Illumina, San Diego, CA, USA). The raw genome sequencing data analysis, including alignment to the GRCh37/hg19 human reference genome, variant calling, and annotation, was conducted using open-source bioinformatics tools and in-house software (3billion Inc., Korea). The results revealed a heterozygous pathogenic variant in HSPG2 (NM_001291860.1; c.10897C>T; p.Arg3633Ter) inherited from his mother. Additionally, an in-trans heterozygous novel variant of uncertain significance was identified in the intronic region (c.413+10G>T) of the same gene, inherited from the father. On the basis of all clinical and genomic information, the patient was conclusively diagnosed with SJS type 1 due to compound heterozygosity of HSPG2 mutations, inherited in an autosomal recessive manner.
The patient was subsequently referred for evaluation of severe blepharophimosis at the Department of Dermatology at Siriraj Hospital. During the dermatology clinical examination at the age of 9 years, a narrow palpebral fissure with imitations of elbow flexion and shoulder extension was noted. The response to carbamazepine was modest and limited to treating generalized hypertonia. Therefore, BTX-A (abobotulinumtoxinA, ABO, Dysport®, Ipsen Biopharm Ltd., UK) injections were administered.
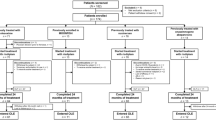
After topical anesthetic cream was removed, the patient was injected with ABO at 1:2 ml dilution (a vial of 500 U of ABO was reconstituted with 2 ml of sterile, preservative-free normal saline solution to yield a solution of 25 units per 0.1 ml). The patient was treated by a well-trained injector using an intramuscular injection technique with a 1-ml syringe and 31-gauge needle. The patient was asked to perform facial rubbing or massage for 2 weeks after injection to avoid unwanted diffusion of toxin. The details of dosage used at each visit are shown in Table 1 and Fig. 2.
Notably, functional improvement was reported, with improved ability to open his eyes and mouth during daily activities. The last treatment was performed in July 2020. The condition of severe blepharophimosis significantly improved for at least 6 months following the last treatment. Although symptoms worsened after that period, they have not regressed to their previous severity for 3 years after the last treatment (Figs. 3 and 4). Surgical management has not been performed or considered in this patient because he responded well to botulinum toxin.
Discussion
We present the clinical characteristics of a patient diagnosed with SJS type 1A based on the Giedion classification [9]. While electromyography (EMG) signs of myotonia and X-ray abnormalities are commonly used in diagnosing SJS, we opted for genetic confirmation instead of EMG [10]. To the best of our knowledge, this is the first genetically confirmed case of SJS in a Southeast Asian individual. Additionally, we describe the progressive nature of myotonia symptoms in this patient, who showed successful treatment with ABO.
SJS is characterized by prominent myotonia and skeletal abnormalities. In the case of SJS type 1A, myotonia is typically observed in early childhood, followed by bone dysplasia during childhood. Our patient presented with a distinct mask-like facial appearance, blepharospasm, short stature, and muscle stiffness at the age of 1 year, followed by bone abnormalities that required orthopedic surgery later. The exact pathogenesis of perlecan mutations, which contribute to SJS, remains partially understood. However, it is hypothesized that perlecan deficiency leads to decreased acetylcholinesterase levels at the neuromuscular junction, resulting in higher acetylcholine concentrations and possibly generating myotonic discharges. Alternatively, ion channel dysfunction could be a consequence of perlecan abnormalities.
The management of SJS primarily revolves around supportive measures. Medical treatments using carbamazepine, phenytoin, or procainamide aim to alleviate myotonia-related issues, although they do not offer a cure [11]. Continuous motor activity in the facial muscles poses challenges in terms of functional and cosmetic symptoms. Various surgical techniques have been employed to address blepharophimosis [4, 8], but the presence of tight jaw muscles and bony deformities may increase surgical complications [5]. In SJS, myotonia is most pronounced in the facial muscles, and it appears to be associated with structural and functional mutations of the perlecan gene (HSPG2) at the neuromuscular junction [12,13,14]. Consequently, BTX-A has been hypothesized to be beneficial in SJS cases. Several reports have indicated improvement in blepharophimosis after treatment with BTX-A injection. BTX-A is widely accepted as the principal therapy for blepharospasm and other facial dystonias [6, 7]. However, determining the appropriate dose and frequency of treatment remains challenging as a result of individual patient variations.
In this case, the author aimed to minimize the dosage of botulinum toxin administered during each treatment session. In the initial session, perioral muscles, including levator labii superioris alaeque nasi (LLSAN), depressor labii inferioris (DLI), and mentalis, were treated. Notably, the improvement in mouth movement was significant even without treating the depressor anguli oris (DAO). The necessity of LLSAN treatment arises from its role as a superficial elevator muscle of the nose and upper lip involved in orofacial expressions. LLSAN widens the nostrils and elevates the upper lip, contributing to facial expressions such as snarling. While LLSAN aids in elevating the upper lip, it can also lift the alar, resulting in a snarling appearance (refer to Fig. 3, pre-treatment). Partially inhibiting LLSAN function in this patient proved beneficial in relaxing the midface and upper lip.
When addressing abnormal muscle functions or movements around the mouth, it is not mandatory to treat all muscles related to mouth opening or closure. The primary goal of treatment in this case was to alleviate perioral spasm by relaxing the muscles around the mouth. Although the masseter, temporalis, and pterygoids play roles in mouth closure, their functions are primarily associated with mastication. Paralyzing these muscles may not effectively reduce mouth spasm.
Table 2 summarizes published reports on cases that received BTX-A injections, providing details on doses, frequency, brand, and target muscles of the injections. Out of the 13 published cases, five were unresponsive to botulinum toxin injection and required surgical interventions. In contrast, eight case reports showed favorable clinical outcomes with botulinum toxin injection for treating myotonic spasms. Comparing with our case, which also demonstrated positive results, we observed similarities in terms of multiple administered doses and long intervals between botulinum toxin injections (3–6 months). As there are no established guidelines for botulinum toxin injection doses, determining the appropriate dosage should be based on the severity and location of myotonia. Further clinical follow-up is necessary to assess the lasting effects of botulinum toxin injections.
Conclusion
A multidisciplinary team approach is essential for managing patients with SJS. BTX-A should be considered as a therapeutic option to relieve facial blepharospasm. However, the optimal doses and intervals must be individually tailored to optimize symptom control. Further research into the use of botulinum toxin A in managing Schwartz-Jampel syndrome is warranted.
References
Basiri K, Fatehi F, Katirji B. The Schwartz-Jampel syndrome: case report and review of literature. Adv Biomed Res. 2015;4:163.
Nicole S, Davoine C-S, Topaloglu H, et al. Perlecan, the major proteoglycan of basement membranes, is altered in patients with Schwartz-Jampel syndrome (chondrodystrophic myotonia). Nat Genet. 2000;26(4):480–3.
Jitpimolmard N, Matthews E, Fialho D. Treatment updates for neuromuscular channelopathies. Curr Treat Options Neurol. 2020;22(10):1–20.
Lucci LM, Yen MT, Anderson RL, Hwang IP, Black RE. Orbicularis myectomy with levator advancement in Schwartz-Jampel syndrome. Am J Ophthalmol. 2001;132(5):799–801.
Viljoen D, Beighton P. Schwartz-Jampel syndrome (chondrodystrophic myotonia). J Med Genet. 1992;29(1):58–62.
da Silveira EB, Rogers AI. Treatment of achalasia with botulinum A toxin. Am J Ther. 2002;9(2):157–61.
Glogau RG. Review of the use of botulinum toxin for hyperhidrosis and cosmetic purposes. Clin J Pain. 2002;18(6):S191–7.
Morrison DA, Mellington FB, Hamada S, Moore AT. Schwartz-Jampel syndrome: surgical management of the myotonia-induced blepharospasm and acquired ptosis after failure with botulinum toxin A injections. Ophthalmic Plast Reconstr Surg. 2006;22(1):57–9.
Giedion A, Boltshauser E, Briner J, et al. Heterogeneity in Schwartz-Jampel chondrodystrophic myotonia. Eur J Pediatr. 1997;156:214–23.
Nicole S, Topaloglu H, Fontaine B. 102nd ENMC International Workshop on Schwartz-Jampel Syndrome, 14–16 December, 2001, Naarden, the Netherlands. Neuromusc Disorders. 2003;13(4):347–51.
Aburahma SK, Al-Khateeb T, Alrefai A, Amarin Z. Botulinum toxin A injections for the treatment of Schwartz-Jampel syndrome: a case series. J Child Neurol. 2009;24(1):5–8.
Carruthers J, Stubbs HA. Botulinum toxin for benign essential blepharospasm, hemifacial spasm and age-related lower eyelid entropion. Can J Neurol Sci. 1987;14(1):42–5.
Koman LA, Smith BP, Balkrishnan R. Spasticity associated with cerebral palsy in children. Pediatr Drugs. 2003;5(1):11–23.
Scott AB. Botulinum toxin injection into extraocular muscles as an alternative to strabismus surgery. J Pediatr Ophthalmol Strabismus. 1980;17(1):21–5.
Vargel I, Canter HI, Topaloglu H, Erk Y. Results of botulinum toxin: an application to blepharospasm Schwartz- Jampel syndrome. J Craniofac Surg. 2006;17(4):656–60. https://doi.org/10.1097/00001665-200607000-00008.
Kashkouli MB, Shahrzad S, Jazayeri AA, Abtahi MB. Treatment of Blepharospasm in Schwartz-Jampel Syndrome: Botulinum Toxin A Injection or Surgery. Ophthalmic Plast Reconstr Surg. 2017;33(3S Suppl 1):S47–9. https://doi.org/10.1097/IOP.0000000000000503.
Bandeira ID, Jagersbacher JG, Barretto TL, Santos CV, Lucena R. Botulinum toxin type A in the treatment of facial myotonia in Schwartz-Jampel syndrome. Muscle Nerve. 2017;56(2):E10–1. https://doi.org/10.1002/mus.25610.
Eshraghi B, Shadravan M, Aalami E, Pour EK. Orbicularis Oculi Myectomy as a Treatment for Blepharospasm in a Case of Schwartz Jampel Syndrome. J Ophthalmic Vis Res. 2016;11(3):329–32. https://doi.org/10.4103/2008-322X.188401.
Ding J, Xu Y, Yuan B, Li D. Management of blepharospasm and blepharophimosis associated with Schwartz- Jampel syndrome. J AAPOS. 2021;25(1):54–6. https://doi.org/10.1016/j.jaapos.2020.10.009.
Acknowledgements
We are grateful to 3billion, Inc., Korea for their effective genetic testing laboratory.
Medical Writing and Editorial Assistance
The authors did not use any medical writing or editorial assistance for this paper.
Funding
The Rapid Service Fee was funded by the Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand.
Author information
Authors and Affiliations
Contributions
Panittra Suphatsathienkul and Rungsima Wanitphakdeedecha had full access to all data in this case report and takes responsibility for the integrity of data and the accuracy of the data presentation. Laboratory investigations: Kullasate Sakpichaisakul, Thanin Wechapinan, Objoon Trachoo, and Sorawit Virawan. Acquisition of data: All authors. Analysis and interpretation of data: Kullasate Sakpichaisakul, Thanin Wechapinan, Objoon Trachoo, and Sorawit Virawan. Drafting of the manuscript: Panittra Suphatsathienkul, Kullasate Sakpichaisakul, and Rungsima Wanitphakdeedecha. Critical revision of the manuscript for important intellectual content: Rungsima Wanitphakdeedecha.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflicts of interests with this case report.
Ethical Approval
Written informed consent has been obtained from the patient’s parents for publication.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Suphatsathienkul, P., Sakpichaisakul, K., Wechapinan, T. et al. Successful Treatment of Schwartz-Jampel Syndrome with Botulinum Toxin Type A. Dermatol Ther (Heidelb) 14, 545–556 (2024). https://doi.org/10.1007/s13555-023-01088-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-023-01088-7