Abstract
Background
Patients with treated solid tumours (TSTs) are a highly heterogeneous population at an increased risk for malignancy compared with the general population. When treating psoriasis in patients with a history of TSTs, clinicians are concerned about the immunosuppressive nature of psoriasis therapies, the possibility of augmenting cancer recurrence/progression, and infectious complications. No direct, high-level evidence exists to address these concerns.
Objectives
We aim to provide a structured framework supporting healthcare professional and patient discussions on the risks and benefits of systemic psoriasis therapy in patients with previously TSTs. Our goal was to address the clinically important question, “In patients with TSTs, does therapy with systemic agents used for psoriasis increase the risk of malignancy or malignancy recurrence?”
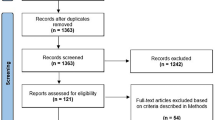
Methods
We implemented an inference-based approach relying on indirect evidence when direct clinical trial and real-world data were absent. We reviewed indirect evidence supporting inferences on the status of immune function in patients with TSTs. Recommendations on systemic psoriasis therapies in patients with TSTs were derived using an inferential heuristic.
Results
We identified five indirect indicators of iatrogenic immunosuppression informed by largely independent bodies of evidence: (1) overall survival, (2) rate of malignancies with psoriasis and systemic psoriasis therapies, (3) rate of infections with psoriasis and systemic psoriasis therapies, (4) common disease biochemical pathways for solid tumours and systemic psoriasis therapies, and (5) solid organ transplant outcomes. On the basis of review of the totality of this data, we provided inference-based conclusions and ascribed level of support for each statement.
Conclusions
Prior to considering new therapies for psoriasis, an understanding of cancer prognosis should be addressed. Patients with TSTs and a good cancer prognosis will have similar outcomes to non-TST patients when treated with systemic psoriasis therapies. For patients with TSTs and a poor cancer prognosis, the quality-of-life benefits of treating psoriasis may outweigh the theoretical risks.
Plain Language Summary
Patients with previously treated cancer have a higher chance of cancer recurrence compared with the general population. With cancer incidence rising worldwide, doctors across medical specialities will need to treat other medical conditions, including inflammatory diseases such as psoriasis, in these patients. Effective systemic therapies for psoriasis reduce immune cell activity. Accordingly, there are concerns that treatments for psoriasis could worsen cancer recurrence/progression and infectious complications. There is not enough quality evidence to make broad recommendations for treating other inflammatory conditions in patients with a history of cancer. To guide patient and doctor discussions, we asked: what are effective and safe treatments when patients with treated solid tumours need systemic therapy (pills or injections) for their psoriasis? We focused on patients with solid tumours and excluded blood and skin cancers. Our panel of experts, including 12 dermatologists and 3 medical oncologists, reviewed direct and indirect evidence to answer this question. Considering the totality of evidence reviewed, the expert panel drafted and rated their level of support for opinion statements on important considerations in treating patients with psoriasis who have a history of solid tumours. By making inferences on systemic psoriasis therapies in this heterogeneous population, we take the onus off individual physicians to review the indirect data. This process may help answer questions in other disease populations where direct evidence is scarce or absent. To support treatment decisions, doctors should have a guided conversation with the patient and their family on a case-by-case basis about the risks and benefits of treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Patients with treated solid tumours (TSTs) are a highly heterogeneous population that differ on the basis of cancer type, including stage and tissue of origin, mutational status of cancer, cancer prognosis and cancer treatment received. |
Use of systemic psoriasis therapies in these patients is hindered by concerns about the possibility of augmenting cancer recurrence/progression or infectious complications. |
Given the limited direct evidence to answer the clinical question, the present guidance document uses an inference-based approach to explore the risks and benefits imposed on patients with a history of TSTs when their psoriasis is treated with systemic psoriasis therapies to provide a structured framework that helps guide treatment decisions. |
This framework supports a discussion between healthcare professionals and their patients about the risks and benefits of systemic psoriasis therapy in patients with previously TSTs. |
The initiation of systemic psoriasis therapy after cancer treatment largely depends on immune reconstitution post-cancer treatment that depends primarily on the type of cancer treatment received rather than on the type of solid tumour or other factors (stage, mutational status, etc.). |
Introduction
While cancer incidence is rising steadily worldwide [1], mortality rates and age-adjusted incidence rates of many solid tumours (STs) are declining [2]. Declining rates result from public health measures, lifestyle modification (especially the avoidance and cessation of cigarette smoking), and better treatments for both cancer and causative infectious diseases [2]. Accordingly, clinicians across medical specialities more frequently encounter patients with a history of treated solid tumours (TSTs). Lifespans of patients with TSTs remain shortened due to delayed cancer treatment toxicities: radiation therapy and certain chemotherapy regimens; secondary cancers; and comorbidities related to common risk factors [3]. Challenges arise in providing recommendations for treating other medical conditions in patients with TSTs due to the heterogeneity of cancer outcomes across different types and stages of solid tumours. In addition, cancer outcome data are skewed by various factors including country, access to resources, and socioeconomic status [4]. Socioeconomically deprived patients with cancer experience a higher loss of life expectancy, primarily from lung and stomach cancers, compared with non-socioeconomically deprived patients [5]. Owing to the heterogeneity and complexity of the topic, there is a need to provide guidance for treating other diseases, such as psoriasis, in patients with TSTs.
In patients with psoriasis, clinicians are concerned about the immunosuppressive nature of systemic psoriasis therapies. Specific concerns include possible augmentation of cancer recurrence/progression and infectious complications in patients with past or active malignancy. Additionally, there is a concern that poor outcomes in cancer survivors might be ascribed to the systemic psoriasis therapy. Notably, cancer survivors have a 14% increased risk of new or recurrent malignancies compared with the general population [6]. In addition, these patients have inherent risk for cancer-related death regardless of psoriasis status and treatment choices [3]. Anticipating that immune processes, treatment paradigms, and risks may differ between broad tumour categories, we focused on patients with TSTs and excluded hematopoietic and cutaneous malignancies.
The objective of this work is to provide a structured framework exploring the risks and benefits for patients with TSTs when treating their psoriasis with systemic psoriasis therapies (which includes biologics and small molecules). A multidisciplinary panel of dermatologists and oncologists was convened to provide guidance on the main clinical question, “Are responses (including drug-related adverse effects and benefits) to systemic psoriasis therapies in patients with TSTs similar to the general psoriasis population?” Answering this question proved to be complex due to the limited direct evidence and heterogeneity of the TST patient population. Patients with TSTs are excluded from clinical trials of agents to treat psoriasis. Observational cohort studies in inflammatory disorders have too few patients with TST to provide meaningful results [7,8,9]. With very limited direct evidence available to answer the clinical question, the panel employed an inference-based approach reviewing indirect evidence relevant to the immune status of patients with TSTs. Levels of evidence and grading of evidence cannot, at this time, be ascribed to the recommendations herein. Rather than providing directive statements, the intended outcome is the development of statements supporting informed discussions between healthcare professionals and their patients regarding the risks and benefits of systemic psoriasis therapy in patients with TSTs. The expert panel defined solid tumours broadly and did not explore the complexities of specific types of solid tumours. Different cancer treatments were explored, with resultant recommendations dependent on the type of therapy received and cancer prognosis. The conclusions are agnostic to specific immune pathways and are therefore applicable to a larger audience of healthcare professionals who manage immune-mediated conditions.
Methods
A panel of 12 dermatologists and 3 medical oncologists (BM, SS, SH) convened following the framework of the New Psoriasis Guidelines group [10]. Through panel discussions directed towards identifying observable scenarios with addressable questions, the primary question was deconstructed in multiple revisions using a layered, inference-based approach (Table S1, Supplementary Material). Our original objective was to identify data assessing immune response in patients with previously and currently TSTs, thereby identifying the potential for altered risk or efficacy when treating psoriasis with a systemic psoriasis therapy. Structured systematic or scoping literature searches were conducted for each deconstructed question from December 2021 to January 2022. See Supplementary Material for literature search keywords. Working group authors summarised key evidence per topic and met in April and May of 2022 to discuss their summaries. Considering the totality of the evidence reviewed, the chairs (KAP, VP) reconstructed statements to address the overarching questions, where possible. Oncologists reviewed and revised the statements prior to all-author rating in September 2022. This study quantifies expert-elicited level of support for inference-based conclusions. A data summary of key evidence reviewed at the working group meetings was provided to all panel members (Supplementary Material), who then rated statements via online surveys, providing their level of support/confidence/agreement with upper and lower values to represent their range of uncertainty in the level of support. Experts provided their ratings on a scale of 0–100% based on approximate, verbal transformations of subjective probability for use in expert elicitation [11]. Here, rating 90% meant the statement was likely to be true, and 99% meant the statement was very likely to be true (Fig. S1, Supplementary Material). Ethics committee approval was not required per section 2.3b of the Tri-Council Policy Statement: Ethical Conduct for Research Involving Humans (TCPS2), as experts who participated in the surveys are published authors on this work and therefore had no expectation of privacy.
Data Analysis
Individual levels of support were fitted to beta-distributions assuming the lower, likely, and upper estimates were 2.5th, 50th, and 97.5th percentiles, respectively. The estimated beta-distributions were combined using averaging and Bayesian analyses to arrive at the estimated prevalence of psoriasis in the adult population. All analyses were performed using R statistics software [12]. Best fit beta-distribution using the quantile estimates provided by each expert was analysed using the betaparms function of the rriskDistributions package (v2.1.2; Belgorodski 2017; https://github.com/cran/rriskDistributions). Bayesian estimates were derived using one of the determined beta-distributions as the prior probability distribution. The averaged distribution parameters were determined by averaging the means and standard deviations of the panel member beta-distributions.
Recommendations and Supporting Evidence
We reviewed indirect evidence to support inferences on the status of immune function in patients with previously TSTs considering a systemic psoriasis therapy. Five indirect indicators of immune function were explored, informed by largely independent bodies of evidence: (1) overall survival (populations included general patients with TSTs and patients with TSTs and psoriasis), (2) rate of malignancies with psoriasis and systemic psoriasis therapies, (3) rate of infections with psoriasis and systemic psoriasis therapies, (4) common disease biochemical pathways for STs and systemic psoriasis therapies, and (5) solid organ transplant outcomes (including patients with TSTs pre-transplant and patients with post-transplant malignancy). The inference-based concluding statements made on the basis of review of the totality of these data and level of support for each statement are summarised below and in Table 1 and Fig. S2 (Supplementary Material), with resultant recommendations summarised in Table 2 (and Fig. S3, Supplementary Material). See Supplementary Material for literature search output and data summaries. Of note, one respondent was an outlier with their assessments, as seen in the individual responses.
Framing the Conclusions
Patients with TSTs are a highly heterogeneous population that differ on the basis of cancer type, including stage and tissue of origin, mutational status of cancer, cancer prognosis, and cancer treatment received. The initiation of systemic psoriasis therapy after cancer treatment will depend largely on immune reconstitution post-cancer treatment. Cancer treatment is increasingly focused on specific oncogenic mutations rather than the tissue of origin, and consequently similar types of treatments are increasingly being received across cancer types [13]. Upon reviewing the evidence, the oncologists unanimously agreed that immune reconstitution following cancer treatment for patients with TSTs depends more on the type of treatment received than on the type of ST or any other factor (stage, mutational status, etc.). Accordingly, this document is relevant for a broad range of treated solid tumours and is not limited to certain types of solid tumours. Physicians should consider the concepts herein as a guide in addition to considering any differences for specific types of solid tumours, which is beyond the scope of the present review. Clinically, immune reconstitution during or after cancer treatment is primarily assessed by normalisation of cell counts. The time frame of normalisation differs depending on the class of cancer treatment received (Table 3). Many types of chemotherapy may induce psoriasis remission [14], with possible recurrence of psoriasis post-completion of chemotherapy. There is a trend in cancer treatment paradigms towards less chemotherapy, less exposure to or more focused radiation therapy, and greater reliance on immune-checkpoint inhibitors (ICIs). ICI therapy has immunostimulatory effects that increase the risk of immune-mediated adverse effects, including skin conditions such as psoriasis [15]. Due to the complexities of this topic, treating de novo psoriasis or psoriasis exacerbated by ICI therapy is not considered here. For patients on active or maintenance treatment for solid tumours, confounding from drug–drug interactions, paucity of direct data, and the complexity and multi-factorial nature of this population prevents generalisable recommendations which are beyond the scope of the present investigation.
An understanding of the patient’s cancer prognosis and immune competence provides some context for discussing risk and benefit of treatment for inflammatory disorders in patients with a history of TSTs. A summary of common STs and survival by stage at diagnosis based on the Surveillance, Epidemiology, and End Results (SEER) Program in the USA provides some guidance to dermatologists (Table 4). This table is included as a guide, and the present guideline is a broad exploration of concepts related to solid tumours, beyond these common STs. Clinical trials and databases in oncology use different staging systems that update frequently, making the interpretation of longitudinal data difficult. Real-world cancer databases lack encoded staging and longer-term follow-up beyond 10–20 years. As a result of the heterogeneity of outcomes from phase 3 oncology clinical trials, disease-free survival for patients with TSTs was not summarised here.
An informed risk–benefit conversation with patients with TST should support all treatment decisions on a case-by-case basis, considering cancer prognosis, the type and intensity of cancer treatment received, and patient preferences. For patients with a poor prognosis (i.e. high risk of recurrence/metastasis), quality-of-life benefits of treating psoriasis with a systemic psoriasis therapy may outweigh the theoretical risks. These patients have inherent risk for cancer-related death regardless of psoriasis status and treatment choices. The present review focused on patients with a good cancer prognosis, that is, those treated with a curative intent. These patients comprise a significant and growing population of patients seeking treatment for psoriasis who require guidance when considering systemic treatments for psoriasis.
General Concepts of Immunosuppression, Immunomodulation, Immune Surveillance, and Senescence in the Development of Malignancies
Cancer formation is a complex of processes involving genetics, immune surveillance, comorbidities, environmental, dietary and lifestyle factors [16, 17]. Age is by far the greatest risk factor [18, 19], with minor contributions to overall cancer risk from environmental [excluding ultraviolet (UV) light exposure] and lifestyle factors [17, 20] as well as occupational exposure [21]. Chronic infections [16] and chronic inflammation [22, 23] contribute to various types of cancer including prostate [24,25,26], breast [27,28,29,30], lung [31,32,33,34,35], colorectal [36,37,38,39,40], and pancreatic [41] cancers. Chronic inflammation results in T-cell exhaustion, thus providing a permissive environment for tumour development, growth and metastasis [42]. T-cell exhaustion resulting from immunosenescence, chronic infection or chronic inflammation provides an opportunity for tumour development, growth and metastasis [43]. Although we reviewed the literature on mechanisms of action of systemic psoriasis therapies to identify any associations with cancer pathways, the evidence was unclear and the effect sizes are likely small; thus, meaningful conclusions could not be made on the basis of this evidence. Depending on the tumour microenvironment, the pathways and cytokines blocked by systemic psoriasis therapies may inhibit, promote or have no effect on tumourigenesis. Interleukin (IL)-17 and T helper 17 (Th17) cells are often associated with chronic inflammatory processes, including those associated with malignancies [42]. Inflammation, while an inducer of malignancy, is also necessary to eliminate malignancy, whereas chronic inflammation is immunosuppressive [44, 45].
Generally, systemic psoriasis therapies are neither inducers nor promoters of cancer pathways and may provide very small benefit by reducing the local inflammatory burden. The exceptions are cyclosporine A (CsA), which may promote the development of cutaneous squamous cell carcinoma (SCC), and UVB light, which is both an inducer and promoter of cutaneous SCC and basal cell carcinoma [46]. Conversely, the benefit of reducing local or systemic inflammatory burden in inflammation-associated malignancies is uncertain, and increasingly so at a later stage. The risk of effect is cumulative; therefore, intervening at a late stage cannot result in a significant benefit [47]. The reported reduction in lung cancer associated with IL-1 inhibition in the CANTOS study is, almost certainly, an incidental finding given the short observation period [47].
Indirect Evidence from Transplant Patients with Immunosuppression
We considered indirect evidence from patients with solid organ transplant (SOT), with and without a history of cancer, who were treated post-transplant with broadly immunosuppressive therapies. In general, SOT recipients have a higher risk of developing certain types of cancer, including Kaposi sarcoma, non-melanoma skin cancer, non-Hodgkin lymphoma, and cancers of the liver, anus, vulva, and lip [48,49,50,51,52,53,54,55,56]. Cancer risk and cancer-related mortality are increased in patients with SOT possibly due to the effects of broad immunosuppression. The nature of tumours developing in patients with SOT suggests the elevated risk is related to a decrease in immunologic control over oncogenic infections or reactivation of latent infections [48, 52]. In general, pre-transplant malignancy is associated with an increased risk of all-cause mortality in transplant patients with SOT, and possibly cancer-specific mortality [50, 54, 57,58,59,60,61,62]. This is likely due to end-stage organ disease and transplant-related complications, but is highly influenced by type of malignancy, grade/stage, tumour-specific characteristics, projected overall survival, time to transplant, and age [50, 54, 57,58,59,60,61,62]. It is unclear if modified immunosuppressive regimens lead to increased all-cause mortality in transplant patients with SOT. However, some studies suggest there is no increase in all-cause mortality for cancers with a good prognosis [59].
Recent guidelines indicate that patients with previously TST with a good prognosis can receive a transplant (and subsequent broad immunosuppressive therapy) with minimal-to-no wait time and similar outcomes as the general SOT population [63]. Similar conclusions can be inferred for patients with psoriasis. Patients at high risk for metastasis, including stage IV and some high-risk stage II–III, are not considered candidates for transplantation until at least 3–5 years post-cancer; therefore, no inference could be drawn from this subpopulation [63].
Considerations for Virus-Associated Cancers
Certain viral infections, including hepatitis B virus (HBV) and hepatitis C virus (HCV), alter cellular signalling and can lead to malignancy [64,65,66,67]. Associated chronic inflammation resulting from immunological responses endeavoring to constrain the persistent infection results in fibrosis and T-cell exhaustion, both of which result in a more permissive environment for the development, growth, and metastasis of malignancy [43]. Chronic inflammation may result in chromatin breaks. Human papillomavirus (HPV) increases the risk of carcinogenesis by mechanisms similar to HBV and HCV [68,69,70]. In general, we found no evidence from our review that oncogenic infections are increased with systemic psoriasis therapy. Other types of infections may be increased with certain systemic psoriasis therapies, which has implications for actively TSTs.
In SOT populations, additional caution is warranted for viral transformative cancers such as HPV or Epstein–Barr virus (EBV), where immune suppression may increase the risk of disease progression and recurrence [48, 51, 71]. This may be relevant for systemic psoriatic therapies with broad T-cell immunosuppression (e.g. CsA), but not the case for systemic psoriasis therapies that immunomodulate by inhibiting Th17 pathway [e.g. IL-17 inhibitors (IL-17i), IL-23 inhibitors (IL-23i) and tumour necrosis factor-alpha inhibitors (TNFi)] [72]. For treatment of psoriasis with TNFi, there is a small theoretical risk of causing active infection with HBV but an anticipated benefit in treating patients infected with HCV. Special consideration should be given to cancers secondary to oncogenic viruses such as cervical cancer and hepatocellular carcinoma, as limited mechanistic data suggest possible negative effect of TNF inhibition [73]. Clinical data in patients with psoriasis that show no significant increase in STs is reassuring.
Baseline Risk of Cancer in Patients with Psoriasis and Its Treatments
Psoriasis and its treatments are not causally associated with an increased risk of STs. Patients with psoriasis may have an increased incidence of lymphomas and non-melanoma skin cancer [74,75,76,77,78,79]. Cutaneous SCC risk, possibly increased in the psoriasis population, is primarily from UVB light exposure [80]. Some studies have suggested that risk of dying from cancer may be increased in patients with more severe psoriasis [74, 81]. However, modifiable risk factors strongly confound the association between psoriasis and cancer death, thus highlighting the importance of patient counselling on weight control, smoking cessation, and moderating alcohol consumption [74, 81].
For each category of systemic psoriasis therapy, we reviewed the limited direct evidence of systemic psoriasis therapy in patients with solid tumours and indirect evidence from the general psoriasis population, and other indications, where available. Direct evidence from cases of psoriasis treatments in patients with a history of malignancy are reassuring, with no worsening or recurrence of cancers noted for any of the treatments studied (Table S2, Supplementary Material) [7]; however, these data should be considered with caution due to reporting bias, with small patient numbers and short follow-up times. The most data exist for risk of cancer recurrence in patients with a history of cancer treated with TNFi for other immune-mediated conditions, including rheumatoid arthritis and inflammatory bowel disease (Table S3, Supplementary Material). These data include meta-analyses of up to 13,598 patients and 32,473 patient-years of follow-up, with no increased risk of cancer recurrence observed [82,83,84]. Although clinical trials exclude patients with a history of TSTs, long-term extensions and meta-analyses estimate baseline cancer risk with systemic treatments. Biologics targeting IL-17, IL-12/23, and IL-23 do not show an increased risk of malignancy or serious infection in the general psoriasis population with up to 5 years of follow-up [85,86,87,88,89,90,91,92,93,94,95,96]. Likewise, biologics targeting TNF-α have up to 8.2 years of long-term extension, real-world and randomised controlled trial data, suggesting that the development of new solid tumours in patients with psoriasis is similar to the SEER database population [85, 97,98,99,100,101,102]. Although preliminary studies have suggested little-to-no increased risk of cancer incidence in patients with psoriasis treated with biologics, longer follow-up periods and increased power are required to properly examine the potential cancer risk, particularly for site-specific cancers [103]. Of note, patients with psoriasis on TNFi are at an increased risk of infection, including serious infection, although real-world evidence suggests that rates are lower than those seen in clinical trials [97, 104]. Clinicians should be cautious about adding TNFi to patients with actively TST on immunosuppressive chemotherapies.
In addition to biologics, systemic psoriasis therapies include traditional systemics and newer emerging small molecules. There are insufficient numbers of patients with psoriasis treated with these specific psoriasis therapies to suggest altered risk for the development of solid tumours. Methotrexate (MTX) is not an inducer or promoter of malignancy [105, 106]. At higher doses, oncologists use MTX to treat solid tumours. Compared with biologics, studies have not shown an increased risk of malignancy associated with the use of low-dose MTX [85, 107,108,109,110], however, there may be a small risk of skin cancer associated with its use [111]. CsA is not known to be an inducer nor a promoter of solid tumours [106], with the possible exception of keratinocyte malignancies [112]. There are several reports suggesting an increased risk of cutaneous SCC in patients receiving CsA [113, 114]. CsA is also associated with a higher risk of infections [115, 116], which has implications for actively TSTs. One study followed 17 patients with psoriasis who were treated with CsA and MTX for 9.5 weeks and reported no occurrences of cancer after a median of 76 months of follow-up [117]. Acitretin is not known to be an inducer or promoter of malignancy [113]. Interestingly, it may be used to prevent or minimise keratinocyte carcinoma in high-risk patients post-transplant [118], though the effect size is uncertain. Neither apremilast [a phosphodiesterase-4 inhibitor (PDE4i)] nor deucravacitinib [an emerging tyrosine kinase 2 inhibitor (TYK2i) with limited long-term data] are known to promote or induce malignancy [119].
Timing of Systemic Psoriasis Therapy Initiation Post-cancer Treatment
There are theoretical concerns about the increased risk of recurrence for patients with TSTs treated with immunosuppressive therapies following chemotherapy. On the basis of our analysis of the literature, a 5-year interval post-cancer treatment [120, 121] is overly cautious and generally unwarranted. The present recommendations (Table 1) are based on anticipated time to immune reconstitution post-cancer treatment, with a 1-month period post-chemotherapy, and no wait time warranted for radiation or endocrine and targeted therapies [i.e. kinase or vascular endothelial growth factor (VEGF)-targeting angiogenesis inhibitors] for STs with a good prognosis. A risk–benefit discussion with patients should always guide treatment decisions. In general, the highest risk of recurrence occurs in the first year post-cancer, with future life expectancy for survivors improving further out from diagnosis and slowly approaching general population life expectancy over time [122]. On the basis of the survival curves for solid tumours, the later the onset of cancer, the closer to a normal life expectancy one can expect [122]. It is unlikely that any of the systemic psoriasis therapies will alter the risk of recurrence or alter the shape or slope of the curves for solid tumours. There is no evidence suggesting that intervening earlier than 5 years with systemic psoriasis therapies will change overall survival or cancer recurrence. One random effects meta-analysis pooling 16 studies of patients with inflammatory bowel disease, rheumatoid arthritis, and psoriasis found similar pooled incidence values for new or primary cancers when immunosuppression was initiated within 6 years versus more than 6 years after the index cancer [83]. In addition, recall that patients with SOT with a history of TST and a good prognosis can receive transplantation and subsequent broad immunosuppression without a wait time or with minimal wait time [63]. A more cautious approach may be warranted for cancers with a poor prognosis or with viral transformative cancers such as HPV and EBV.
Discussion/Limitations
The present guidance document demonstrates a formal inference-based process, novel to clinical medicine, guiding practice where high-level evidence is lacking [10, 123]. In addition to recommendation statements, we provide inference-based conclusions supporting healthcare professional discussions and shared decision making. This approach is useful when guidance is needed but direct evidence is lacking. Clinical trials require small, well-defined populations. Real-world data, while reporting on larger populations, are confounded by inclusion and observation biases. An inference-based approach provides guidance on clinical scenarios for populations in which clinical trial and real-world studies are unlikely to be conducted [124, 125]. Practical clinical decisions are often made in the face of limited evidence. The process of considering indirect evidence provides reflective, critical and structured support for care providers. Implementing a formalised methodology reduces the burden on individual physicians to review and assess available data while encouraging clinicians to engage patients in an informed manner [10]. Deconstructing the main question into components and addressing the sub-components permits restructuring of evidence supporting, or refuting, a conclusion. The result is a statement of confidence in the recommendations based on the totality of evidence. The responses of expert dermatologists and oncologists indicated significant support with high levels of confidence regarding the risks of treating psoriasis with systemic psoriasis therapies in patients with TSTs. One participant was an outlier in their assessments. Regardless of whether their evaluations reflect personal beliefs, their considered assessment of the evidence, or their comfort with the process, the summary stands apparent and transparent.
It is impractical and ill-considered to provide comprehensive or directive statements. The uniqueness of each clinical situation and each patient requires a holistic approach based on a reasonable understanding of the facts. Significant clinical heterogeneity and knowledge gaps characterise malignancy. The authors have attempted to provide informed guidance based on limited data. Our observations do not address patients with TSTs on active or maintenance cancer treatment. The present framework notes that the type of cancer treatment received will impact immune reconstitution more than other cancer-related factors, suggesting there are few differences across ST types. Optimal patient care demands dermatologists consult with treating oncologists regarding cancer prognosis, concerns related to cancer type and stage, and systemic psoriasis therapy should it be necessary.
Generalisations made here may not be relevant for all tumour types. Previously published guidance on systemic psoriasis therapy use in patients with TSTs were based on weak evidence that was subject to reporting and observer bias: case reports or case series [78]. Previous guidance suggests a 5-year interval post-remission before introducing systemic psoriasis therapy for psoriasis in patients with TSTs [120, 121]. Previous guidelines may reflect an unwarranted, overly cautious approach. Immune reconstitution is realised soon after stopping cancer treatment in most patients with a good cancer prognosis (see Table 3). Inferring from indirect data, our multidisciplinary group, consisting of dermatologists and oncologists, concurred that patients with a good cancer prognosis will likely experience similar responses to systemic therapies as those in the general population. Additional caution should be taken for those who have a poor prognosis.
Conclusions
We reviewed indirect evidence supporting inferences on additional risks and benefits imposed on patients with TSTs requiring systemic therapies for the treatment of psoriasis. On the basis of our review, we expect that patients with TSTs and a good prognosis will have similar drug-related adverse effects and benefits to non-TST patients when treated with systemic psoriasis therapies. Prior to considering new therapies for psoriasis, an understanding of cancer prognosis should be addressed with the treating oncologist and patient. All treatment decisions should be made on a case-by-case basis after an informed discussion with the treating physician and patient.
Change history
06 July 2023
A Correction to this paper has been published: https://doi.org/10.1007/s13555-023-00949-5
References
Global Burden of Disease Cancer Collaboration, Fitzmaurice C, Akinyemiju TF, Al Lami FH, Alam T, Alizadeh-Navaei R, et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 29 cancer groups, 1990 to 2016: a systematic analysis for the global burden of disease study. JAMA Oncol. 2018;4:1553–68.
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2021. CA Cancer J Clin. 2021;71:7–33.
National Comprehensive Cancer Network. Survivorship (Version 1.2022) https://www.nccn.org/professionals/physician_gls/pdf/survivorship.pdf. Accessed 9 Sep 2022
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49.
Syriopoulou E, Bower H, Andersson TM-L, Lambert PC, Rutherford MJ. Estimating the impact of a cancer diagnosis on life expectancy by socio-economic group for a range of cancer types in England. Br J Cancer. 2017;117:1419–26.
Curtis RE, Freedman DM, Ron E, Ries LAG, Hacker DG, Edwards BK, Tucker MA, Fraumeni JF Jr. (eds). New malignancies among cancer survivors: SEER Cancer Registries, 1973–2000. National Cancer Institute, NIH Publ. No. 05-5302. Bethesda, MD, 2006.
Mastorino L, Dapavo P, Avallone G, Merli M, Cariti C, Rubatto M, et al. Biologic treatment for psoriasis in cancer patients: should they still be considered forbidden? J Dermatol Treat. 2021;1–8.
Valenti M, Pavia G, Gargiulo L, Facheris P, Sanna F, Borroni RG, et al. Biologic therapies for plaque type psoriasis in patients with previous malignant cancer: long-term safety in a single- center real-life population. J Dermatol Treat. 2021;1–5.
Bellinato F, Gisondi P, Maurelli M, Girolomoni G. IL-17A inhibitors in patients with chronic plaque psoriasis and history of malignancy: a case series with systematic literature review. Dermatol Ther. 2021;34: e14889.
Papp K, Gooderham M, Lynde C, Poulin Y, Beecker J, Dutz J, et al. Practical and relevant guidelines for the management of psoriasis: an inference-based methodology. Dermatol Ther (Heidelb). 2022;12:253–65.
Vick SG. Degrees of belief: subjective probability and engineering judgment. Reston: American Society of Civil Engineers; 2002.
R Core Team. A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2014.
Schneider G, Schmidt-Supprian M, Rad R, Saur D. Tissue-specific tumorigenesis: context matters. Nat Rev Cancer. 2017;17:239–53.
Jeffes EW, Weinstein GD. Methotrexate and other chemotherapeutic agents used to treat psoriasis. Dermatol Clin. 1995;13:875–90.
Sibaud V. Dermatologic reactions to immune checkpoint inhibitors: skin toxicities and immunotherapy. Am J Clin Dermatol. 2018;19:345–61.
Blackadar CB. Historical review of the causes of cancer. WJCO. 2016;7:54.
Ames BN, Gold LS, Willett WC. The causes and prevention of cancer. Proc Natl Acad Sci USA. 1995;92:5258–65.
DePinho RA. The age of cancer. Nature. 2000;408:248–54.
White MC, Holman DM, Boehm JE, Peipins LA, Grossman M, Jane HS. Age and cancer risk. Am J Prev Med. 2014;46:S7-15.
Danaei G, Vander Hoorn S, Lopez AD, Murray CJ, Ezzati M. Causes of cancer in the world: comparative risk assessment of nine behavioural and environmental risk factors. The Lancet. 2005;366:1784–93.
Doll R, Peto R. The causes of cancer: quantitative estimates of avoidable risks of cancer in the United States today. 1981;66:117
Gonzalez H, Hagerling C, Werb Z. Roles of the immune system in cancer: from tumor initiation to metastatic progression. Genes Dev. 2018;32:1267–84.
Greten FR, Grivennikov SI. Inflammation and cancer: triggers, mechanisms, and consequences. Immunity. 2019;51:27–41.
De Marzo AM, Platz EA, Sutcliffe S, Xu J, Grönberg H, Drake CG, et al. Inflammation in prostate carcinogenesis. Nat Rev Cancer. 2007;7:256–69.
Sfanos KS, De Marzo AM. Prostate cancer and inflammation: the evidence: prostate cancer and inflammation. Histopathology. 2012;60:199–215.
de Bono JS, Guo C, Gurel B, De Marzo AM, Sfanos KS, Mani RS, et al. Prostate carcinogenesis: inflammatory storms. Nat Rev Cancer. 2020;20:455–69.
Picon-Ruiz M, Morata-Tarifa C, Valle-Goffin JJ, Friedman ER, Slingerland JM. Obesity and adverse breast cancer risk and outcome: Mechanistic insights and strategies for intervention: breast cancer, inflammation, and obesity. CA Cancer J Clin. 2017;67:378–97.
Howe LR. Inflammation and breast cancer. Cyclooxygenase/prostaglandin signaling and breast cancer. Breast Cancer Res. 2007;9:210.
De Nardo DG, Coussens LM. Inflammation and breast cancer. Balancing immune response: crosstalk between adaptive and innate immune cells during breast cancer progression. Breast Cancer Res. 2007;9:212.
Cole SW. Chronic inflammation and breast cancer recurrence. JCO. 2009;27:3418–9.
Engels EA. Inflammation in the development of lung cancer: epidemiological evidence. Expert Rev Anticancer Ther. 2008;8:605–15.
Walser T, Cui X, Yanagawa J, Lee JM, Heinrich E, Lee G, et al. Smoking and lung cancer: the role of inflammation. Proc Am Thorac Soc. 2008;5:811–5.
Brenner DR, McLaughlin JR, Hung RJ. Previous lung diseases and lung cancer risk: a systematic review and meta-analysis. Myer L, editor. PLoS ONE. 2011;6: e17479.
Conway EM, Pikor LA, Kung SHY, Hamilton MJ, Lam S, Lam WL, et al. Macrophages, inflammation, and lung cancer. Am J Respir Crit Care Med. 2016;193:116–30.
Engels EA, Wu X, Gu J, Dong Q, Liu J, Spitz MR. Systematic evaluation of genetic variants in the inflammation pathway and risk of lung cancer. Cancer Res. 2007;67:6520–7.
Grivennikov SI. Inflammation and colorectal cancer: colitis-associated neoplasia. Semin Immunopathol. 2013;35:229–44.
Wang S, Liu Z, Wang L, Zhang X. NF-kappaB signaling pathway, inflammation and colorectal cancer. Mol Immunol. 2009;6:8.
Rhodes JM, Campbell BJ. Inflammation and colorectal cancer: IBD-associated and sporadic cancer compared. Trends Mol Med. 2002;8:10–6.
Kraus S, Arber N. Inflammation and colorectal cancer. Curr Opin Pharmacol. 2009;9:405–10.
Canavan C, Abrams KR, Mayberry J. Meta-analysis: colorectal and small bowel cancer risk in patients with Crohn’s disease. Aliment Pharmacol Ther. 2006;23:1097–104.
Dai J, Jiang M, Wang X-P, Tian L. Inflammation-related pancreatic carcinogenesis: mechanisms and clinical potentials in advances. Pancreas. 2017;46:973–85.
Liu Y, Cao X. Immunosuppressive cells in tumor immune escape and metastasis. J Mol Med. 2016;94:509–22.
Zheng L, Qin S, Si W, Wang A, Xing B, Gao R, et al. Pan-cancer single-cell landscape of tumor-infiltrating T cells. Science. 2021;374:abe6474.
Shalapour S, Karin M. Immunity, inflammation, and cancer: an eternal fight between good and evil. J Clin Invest. 2015;125:3347–55.
Sacdalan DB, Lucero JA. The association between inflammation and immunosuppression: implications for ICI biomarker development. Onco Targets Ther. 2021;14:2053–64.
Waldman A, Schmults C. Cutaneous squamous cell carcinoma. Hematol Oncol Clin N Am. 2019;33:1–12.
Ridker PM, MacFadyen JG, Thuren T, Everett BM, Libby P, Glynn RJ, et al. Effect of interleukin-1β inhibition with canakinumab on incident lung cancer in patients with atherosclerosis: exploratory results from a randomised, double-blind, placebo-controlled trial. Lancet. 2017;390:1833–42.
Gogna S, Ramakrishna K, John S. Post transplantation cancer. StatPearls. Treasure Island: StatPearls Publishing; 2021.
Hall EC, Pfeiffer RM, Segev DL, Engels EA. Cumulative incidence of cancer after solid organ transplantation: cancer incidence after transplantation. Cancer. 2013;119:2300–8.
Sprangers B, Nair V, Launay-Vacher V, Riella LV, Jhaveri KD. Risk factors associated with post–kidney transplant malignancies: an article from the Cancer-Kidney International Network. Clin Kidney J. 2018;11:315–29.
Rossi AP, Klein CL. Posttransplant malignancy. Surg Clin N Am. 2019;99:49–64.
Manickavasagar R, Thuraisingham R. Post renal-transplant malignancy surveillance. Clin Med. 2020;20:142–5.
Shtraichman O, Ahya VN. Malignancy after lung transplantation. Ann Transl Med. 2020;8:416–416.
Farrugia D, Mahboob S, Cheshire J, Begaj I, Khosla S, Ray D, et al. Malignancy-related mortality following kidney transplantation is common. Kidney Int. 2014;85:1395–403.
Stallone G, Infante B, Grandaliano G. Management and prevention of post-transplant malignancies in kidney transplant recipients: Table 1. Clin Kidney J. 2015;8:637–44.
Gibson JAG, Cordaro A, Dobbs TD, Griffiths R, Akbari A, Whitaker S, et al. The association between immunosuppression and skin cancer in solid organ transplant recipients: a control-matched cohort study of 2,852 patients. Eur J Dermatol. 2021;31:712–21.
Wong G, Chapman JR, Craig JC. Death from cancer: a sobering truth for patients with kidney transplants. Kidney Int. 2014;85:1262–4.
Engels EA, Haber G, Hart A, Lynch CF, Li J, Pawlish KS, et al. Predicted cure and survival among transplant recipients with a previous cancer diagnosis. J Clin Oncol. 2021;39:4039–48.
Engels EA, Haber G, Hart A, Lynch CF, Li J, Pawlish KS, et al. Solid organ transplantation and survival among individuals with a history of cancer. Cancer Epidemiol Biomark Prev. 2021;30:1312–9.
Acuna SA, Lam W, Daly C, Kim SJ, Baxter NN. Cancer evaluation in the assessment of solid organ transplant candidates: a systematic review of clinical practice guidelines. Transplant Rev (Orlando). 2018;32:29–35.
Livingston-Rosanoff D, Foley DP, Leverson G, Wilke LG. Impact of pre-transplant malignancy on outcomes after kidney transplantation: united network for organ sharing database analysis. J Am Coll Surg. 2019;229:568–79.
Liauw SL, Ham SA, Das LC, Rudra S, Packiam VT, Koshy M, et al. Prostate cancer outcomes following solid-organ transplantation: a SEER-Medicare analysis. J Natl Cancer Inst. 2020;112:847–54.
Al-Adra DP, Hammel L, Roberts J, Woodle ES, Levine D, Mandelbrot D, et al. Pretransplant solid organ malignancy and organ transplant candidacy: a consensus expert opinion statement. Am J Transplant. 2021;21:460–74.
Tsai W-L, Chung RT. Viral hepatocarcinogenesis. Oncogene. 2010;29:2309–24.
Lemon SM, McGivern DR. Is hepatitis C virus carcinogenic? Gastroenterology. 2012;142:1274–8.
Levrero M, Zucman-Rossi J. Mechanisms of HBV-induced hepatocellular carcinoma. J Hepatol. 2016;64:S84-101.
Fung J, Lai C-L, Yuen M-F. Hepatitis B and C virus-related carcinogenesis. Clin Microbiol Infect. 2009;15:964–70.
Williams VM, Filippova M, Soto U, Duerksen-Hughes PJ. HPV-DNA integration and carcinogenesis: putative roles for inflammation and oxidative stress. Futur Virol. 2011;6:45–57.
Chan CK, Aimagambetova G, Ukybassova T, Kongrtay K, Azizan A. Human papillomavirus infection and cervical cancer: epidemiology, screening, and vaccination—review of current perspectives. J Oncol. 2019;2019:1–11.
Wang X, Huang X, Zhang Y. Involvement of human papillomaviruses in cervical cancer. Front Microbiol. 2018;9:2896.
Martinez OM, de Gruijl FR. Molecular and immunologic mechanisms of cancer pathogenesis in solid organ transplant recipients. Am J Transplant. 2008;8:2205–11.
Raaschou P, Söderling J, Turesson C, Askling J. Tumor necrosis factor inhibitors and cancer recurrence in Swedish patients with rheumatoid arthritis. Ann Intern Med. 2018;169:291–9.
Bessaleli E, Scheinfeld N, Kroumpouzos G. Squamous cell carcinoma of the cervix arising in a patient on adalimumab—a need for cervical screenings in patients on tumor necrosis factor inhibitors. Dermatology Online Journal [Internet]. 2018;24. https://escholarship.org/uc/item/3fs049h2. Accessed 2022 Jul 15.
Chiesa Fuxench ZC, Shin DB, Ogdie Beatty A, Gelfand JM. The risk of cancer in patients with psoriasis: a population-based cohort study in the health improvement network. JAMA Dermatol. 2016;152:282.
Vaengebjerg S, Skov L, Egeberg A, Loft ND. Prevalence, incidence, and risk of cancer in patients with psoriasis and psoriatic arthritis: a systematic review and meta-analysis. JAMA Dermatol. 2020;156:421.
Kimball AB, Schenfeld J, Accortt NA, Anthony MS, Rothman KJ, Pariser D. Incidence rates of malignancies and hospitalized infectious events in patients with psoriasis with or without treatment and a general population in the U.S.A.: 2005–09. Br J Dermatol. 2014;170:366–73.
Kimball AB, Schenfeld J, Accortt NA, Anthony MS, Rothman KJ, Pariser D. Cohort study of malignancies and hospitalized infectious events in treated and untreated patients with psoriasis and a general population in the United States. Br J Dermatol. 2015;173:1183–90.
Geller S, Xu H, Lebwohl M, Nardone B, Lacouture ME, Kheterpal M. Malignancy risk and recurrence with psoriasis and its treatments: a concise update. Am J Clin Dermatol. 2018;19:363–75.
Loft ND, Vaengebjerg S, Skov L. Cancer risk in patients with psoriasis: should we be paying more attention? Expert Rev Clin Immunol. 2020;16:479–92.
Gandhi SA, Kampp J. Skin cancer epidemiology, detection, and management. Med Clin N Am. 2015;99:1323–35.
Voelker R. Study clarifies cancer risk among people with psoriasis. JAMA. 2019;322:2273.
Xie W, Yang X, Huang H, Gao D, Ji L, Zhang Z. Risk of malignancy with non-TNFi biologic or tofacitinib therapy in rheumatoid arthritis: a meta-analysis of observational studies. Semin Arthritis Rheum. 2020;50:930–7.
Shelton E, Laharie D, Scott FI, Mamtani R, Lewis JD, Colombel J-F, et al. Cancer recurrence following immune-suppressive therapies in patients with immune-mediated diseases: a systematic review and meta-analysis. Gastroenterology. 2016;151:97-109.e4.
Micic D, Komaki Y, Alavanja A, Rubin DT, Sakuraba A. Risk of cancer recurrence among individuals exposed to antitumor necrosis factor therapy: a systematic review and meta-analysis of observational studies. J Clin Gastroenterol. 2019;53:e1-11.
Fiorentino D, Ho V, Lebwohl MG, Leite L, Hopkins L, Galindo C, et al. Risk of malignancy with systemic psoriasis treatment in the Psoriasis Longitudinal Assessment Registry. J Am Acad Dermatol. 2017;77:845-854.e5.
Blauvelt A, Tsai T-F, Langley RG, Miller M, Shen Y-K, You Y, et al. Consistent safety profile with up to 5 years of continuous treatment with guselkumab: pooled analyses from the phase 3 VOYAGE 1 and VOYAGE 2 trials of patients with moderate-to-severe psoriasis. J Am Acad Dermatol. 2022;86:827–34.
Gordon KB, Lebwohl M, Papp KA, Bachelez H, Wu JJ, Langley RG, et al. Long-term safety of risankizumab from 17 clinical trials in patients with moderate-to-severe plaque psoriasis*. Br J Dermatol. 2022;186:466–75.
Rahman P, Ritchlin CT, Helliwell PS, Boehncke W-H, Mease PJ, Gottlieb AB, et al. Pooled safety results through 1 year of 2 phase III trials of guselkumab in patients with psoriatic arthritis. J Rheumatol. 2021;48:1815–23.
van de Kerkhof PCM, Griffiths CEM, Reich K, Leonardi CL, Blauvelt A, Tsai T-F, et al. Secukinumab long-term safety experience: a pooled analysis of 10 phase II and III clinical studies in patients with moderate to severe plaque psoriasis. J Am Acad Dermatol. 2016;75:83-98.e4.
Armstrong A, Paul C, Puig L, Boehncke WH, Freeman M, Torii H, et al. Safety of ixekizumab treatment for up to 5 years in adult patients with moderate-to-severe psoriasis: results from greater than 17,000 patient-years of exposure. Dermatol Ther (Heidelb). 2020;10:133–50.
Lebwohl M, Deodhar A, Griffiths CEM, Menter MA, Poddubnyy D, Bao W, et al. The risk of malignancy in patients with secukinumab-treated psoriasis, psoriatic arthritis and ankylosing spondylitis: analysis of clinical trial and postmarketing surveillance data with up to five years of follow-up. Br J Dermatol. 2021;185:935–44.
Mease P, Roussou E, Burmester G-R, Goupille P, Gottlieb A, Moriarty SR, et al. Safety of ixekizumab in patients with psoriatic arthritis: results from a pooled analysis of three clinical trials. Arthritis Care Res. 2019;71:367–78.
Gottlieb A, Lebwohl M, Liu C, Israel RJ, Jacobson A. Malignancy rates in brodalumab clinical studies for psoriasis. Am J Clin Dermatol. 2020;21:421–30.
Megna M, Fabbrocini G, Cinelli E, Camela E, Ruggiero A. Guselkumab in moderate to severe psoriasis in routine clinical care: an Italian 44-week real-life experience. J Dermatolog Treat. 2020;1–5.
Papp KA, Griffiths CEM, Gordon K, Lebwohl M, Szapary PO, Wasfi Y, et al. Long-term safety of ustekinumab in patients with moderate-to-severe psoriasis: final results from 5 years of follow-up. Br J Dermatol. 2013;168:844–54.
Reich K, Papp KA, Griffiths CEM, Szapary PO, Yeilding N, Wasfi Y, et al. An update on the long-term safety experience of ustekinumab: results from the psoriasis clinical development program with up to four years of follow-up. J Drugs Dermatol. 2012;11:300–12.
Strober B, Crowley J, Langley RG, Gordon K, Menter A, Leonardi C, et al. Systematic review of the real-world evidence of adalimumab safety in psoriasis registries. J Eur Acad Dermatol Venereol. 2018;32:2126–33.
Burmester GR, Panaccione R, Gordon KB, McIlraith MJ, Lacerda APM. Adalimumab: long-term safety in 23 458 patients from global clinical trials in rheumatoid arthritis, juvenile idiopathic arthritis, ankylosing spondylitis, psoriatic arthritis, psoriasis and Crohn’s disease. Ann Rheum Dis. 2013;72:517–24.
Chen Y, Friedman M, Liu G, Deodhar A, Chu C-Q. Do tumor necrosis factor inhibitors increase cancer risk in patients with chronic immune-mediated inflammatory disorders? Cytokine. 2018;101:78–88.
Saliba L, Moulis G, Abou Taam M, Rousseau V, Chebane L, Petitpain N, et al. Tumor necrosis factor inhibitors added to nonbiological immunosuppressants vs. nonbiological immunosuppressants alone: a different signal of cancer risk according to the condition. A disproportionality analysis in a nationwide pharmacovigilance database. Fundam Clin Pharmacol. 2016;30:162–71.
Leonardi C, Papp K, Strober B, Thaçi D, Warren RB, Tyring S, et al. Comprehensive long-term safety of adalimumab from 18 clinical trials in adult patients with moderate-to-severe plaque psoriasis. Br J Dermatol. 2019;180:76–85.
Asgari MM, Ray GT, Geier JL, Quesenberry CP. Malignancy rates in a large cohort of patients with systemically treated psoriasis in a managed care population. J Am Acad Dermatol. 2017;76:632–8.
Trafford AM, Parisi R, Kontopantelis E, Griffiths CEM, Ashcroft DM. Association of psoriasis with the risk of developing or dying of cancer: a systematic review and meta-analysis. JAMA Dermatol. 2019;155:1390.
Garcia-Doval I, Cohen AD, Cazzaniga S, Feldhamer I, Addis A, Carretero G, et al. Risk of serious infections, cutaneous bacterial infections, and granulomatous infections in patients with psoriasis treated with anti–tumor necrosis factor agents versus classic therapies: prospective meta-analysis of Psonet registries. J Am Acad Dermatol. 2017;76:299-308.e16.
Ruderman EM. Overview of safety of non-biologic and biologic DMARDs. Rheumatology. 2012;51:vi37-43.
Weaver JL. Establishing the carcinogenic risk of immunomodulatory drugs. Toxicol Pathol. 2012;40:267–71.
Solomon DH, Kremer JM, Fisher M, Curtis JR, Furer V, Harrold LR, et al. Comparative cancer risk associated with methotrexate, other non-biologic and biologic disease-modifying anti-rheumatic drugs. Semin Arthritis Rheum. 2014;43:489–97.
Rudzki JD. Risk of cancer after long-term therapy of autoimmune disorders with glucocorticoids or DMARDs—a controversial issue. memo. 2019;12:225–9.
Mazaud C, Fardet L. Relative risk of and determinants for adverse events of methotrexate prescribed at a low dose: a systematic review and meta-analysis of randomized placebo-controlled trials. Br J Dermatol. 2017;177:978–86.
Pouplard C, Brenaut E, Horreau C, Barnetche T, Misery L, Richard M-A, et al. Risk of cancer in psoriasis: a systematic review and meta-analysis of epidemiological studies. J Eur Acad Dermatol Venereol. 2013;27:36–46.
Solomon DH, Glynn RJ, Karlson EW, Lu F, Corrigan C, Colls J, et al. Adverse effects of low-dose methotrexate: a randomized trial. Ann Intern Med. 2020;172:369–80.
Han W, Ming M, He T-C, He Y-Y. Immunosuppressive cyclosporin A activates AKT in keratinocytes through PTEN suppression: implications in skin carcinogenesis. J Biol Chem. 2010;285:11369–77.
Balak DMW, Gerdes S, Parodi A, Salgado-Boquete L. Long-term safety of oral systemic therapies for psoriasis: a comprehensive review of the literature. Dermatol Ther (Heidelb). 2020;10:589–613.
Naldi L, Griffiths CEM. Traditional therapies in the management of moderate to severe chronic plaque psoriasis: an assessment of the benefits and risks. Br J Dermatol. 2005;152:597–615.
Kaushik SB, Lebwohl MG. Review of safety and efficacy of approved systemic psoriasis therapies. Int J Dermatol. 2019;58:649–58.
Dávila-Seijo P, Dauden E, Descalzo MA, Carretero G, Carrascosa J-M, Vanaclocha F, et al. Infections in moderate to severe psoriasis patients treated with biological drugs compared to classic systemic drugs: findings from the BIOBADADERM registry. J Invest Dermatol. 2017;137:313–21.
Aydin F, Yuksel EP, Senturk N, Canturk T, Turanli AY. Cancer-free survival of psoriasis patients treated with methotrexate and cyclosporine combination. Cutan Ocul Toxicol. 2014;33:181–3.
Solomon-Cohen E, Reiss-Huss S, Hodak E, Davidovici B. Low-dose acitretin for secondary prevention of keratinocyte carcinomas in solid-organ transplant recipients. Dermatology. 2022;238:161–6.
Balato A, Campione E, Cirillo T, Malara G, Trifirò C, Bianchi L, et al. Long-term efficacy and safety of apremilast in psoriatic arthritis: focus on skin manifestations and special populations. Dermatol Ther. 2020;33: e13440.
Lambert JLW, Segaert S, Ghislain PD, Hillary T, Nikkels A, Willaert F, et al. Practical recommendations for systemic treatment in psoriasis in case of coexisting inflammatory, neurologic, infectious or malignant disorders (BETA-PSO: Belgian Evidence-based Treatment Advice in Psoriasis; part 2). J Eur Acad Dermatol Venereol. 2020;34:1914–23.
Smith CH, Jabbar-Lopez ZK, Yiu ZZ, Bale T, Burden AD, Coates LC, et al. British Association of Dermatologists guidelines for biologic therapy for psoriasis 2017. Br J Dermatol. 2017;177:628–36.
Capocaccia R, Gatta G, Dal Maso L. Life expectancy of colon, breast, and testicular cancer patients: an analysis of US-SEER population-based data. Ann Oncol. 2015;26:1263–8.
Papp KA, Beecker J, Cooper C, Kirchhof MG, Pozniak AL, Rockstroh JK, et al. Use of systemic therapies for treatment of psoriasis in people living with controlled HIV: inference-based guidance from a multidisciplinary expert panel. Dermatol Ther (Heidelb). 2022;12:1073–89.
Dickey JM. Uncertain judgements: eliciting experts’ probabilities by O’Hagan, A, Buck, C. E., Daneshkhah, A., Eiser, J. R., Garthwaite, P. H., Jenkinson, D. J., Oakley, J. E., and Rakow, T. Biometrics. 2008;64:989–90.
O’Hagan A. Expert knowledge elicitation: subjective but scientific. Am Stat. 2019;73:69–81.
Lyman GH, Kuderer NM, Aapro M. Improving outcomes of chemotherapy: established and novel options for myeloprotection in the COVID-19 era. Front Oncol. 2021;11: 697908.
Barreto JN, McCullough KB, Ice LL, Smith JA. Antineoplastic agents and the associated myelosuppressive effects: a review. J Pharm Pract. 2014;27:440–6.
Brahmer JR, Abu-Sbeih H, Ascierto PA, Brufsky J, Cappelli LC, Cortazar FB, et al. Society for Immunotherapy of Cancer (SITC) clinical practice guideline on immune checkpoint inhibitor-related adverse events. J Immunother Cancer. 2021;9: e002435.
Maritaz C, Broutin S, Chaput N, Marabelle A, Paci A. Immune checkpoint-targeted antibodies: a room for dose and schedule optimization? J Hematol Oncol. 2022;15:6.
Kumari S, Mukherjee S, Sinha D, Abdisalaam S, Krishnan S, Asaithamby A. Immunomodulatory effects of radiotherapy. Int J Mol Sci. 2020;21:8151.
Jiang L, Liu J. Immunological effect of tyrosine kinase inhibitors on the tumor immune environment in non-small cell lung cancer (review). Oncol Lett. 2022;23:165.
Ren Z, Sun J, Sun X, Hou H, Li K, Ge Q. Efficacy and safety of different molecular targeted agents based on chemotherapy for gastric cancer patients treatment: a network meta-analysis. Oncotarget. 2017;8:48253–62.
Wang Y, Probin V, Zhou D. Cancer therapy-induced residual bone marrow injury: mechanisms of induction and implication for therapy. Curr Cancer Ther Rev. 2006;2:271–9.
Verma R, Foster RE, Horgan K, Mounsey K, Nixon H, Smalle N, et al. Lymphocyte depletion and repopulation after chemotherapy for primary breast cancer. Breast Cancer Res. 2016;18:10.
Lumniczky K, Candéias SM, Gaipl US, Frey B. Editorial: radiation and the immune system: current knowledge and future perspectives. Front Immunol. 2018;8:1933.
Lumniczky K, Impens N, Armengol G, Candéias S, Georgakilas AG, Hornhardt S, et al. Low dose ionizing radiation effects on the immune system. Environ Int. 2021;149: 106212.
de Carvalho HA, Villar RC. Radiotherapy and immune response: the systemic effects of a local treatment. Clinics (São Paulo). 2018;73: e557s.
Standish LJ, Torkelson C, Hamill FA, Yim D, Hill-Force A, Fitzpatrick A, et al. Immune defects in breast cancer patients after radiotherapy. J Soc Integr Oncol. 2008;6:110–21.
Acknowledgements
We thank the following professional and patient organizations for their support and endorsement of this guideline’s initiative: Alberta Society of Dermatologists, Atlantic Provinces Dermatology Association, Dermatology Association of Ontario, The Dermatologic Society of Manitoba, Saskatchewan Dermatology Association, Canadian Association of Psoriasis Patients, and Canadian Skin Patient Alliance.
Funding
This project was initiated and financially sponsored by the Dermatology Association of Ontario. Unrestricted educational grants have been provided by the following industry partners (listed alphabetically): AbbVie Inc., Amgen Inc., Janssen Inc., LEO Pharma Inc., Novartis Pharmaceuticals Inc., SUN Pharmaceuticals Ltd., and UCB Canada Inc. These grants were pooled and used to pay for the journal’s Rapid Service Fee as well as medical writing assistance as outlined below. Funders did not influence the content of the project.
Medical Writing, Editorial, and Other Assistance
Anna Czerwonka, H BSc, Marcia Bos, BScPhm, RPh, and Julia Jaramillo, MSc, of FUSE Health (Toronto, ON) provided professional medical writing services and organizational support for this manuscript as detailed in funding section above.
Author Contributions
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole and have given their approval for this version to be published. All authors contributed to the study conception, ratings, writing of the draft related to their section, review and editing of the manuscript. Methodology: Kim A. Papp, Jan P. Dutz, Mark G. Kirchhof, Robert Gniadecki. Data analysis, Resources and Supervision: Kim A. Papp. Funding acquisition: Kim A. Papp, Melinda J. Gooderham, Charles W. Lynde.
Disclosures
Outside the submitted work, the authors declare the following conflicts of interest: Dr. Kim A. Papp serves as the treasurer of the Dermatology Association of Ontario and has served as an investigator, speaker, advisor and/or consultant for, and/or received grants/honoraria from: AbbVie, Acelyrin, Akros, Amgen, Anacor, Aralez Pharmaceuticals, Arcutis, Avillion, Bausch Health (Valeant), Boehringer Ingelheim, Bristol Myers Squibb (BMS), CanFite Biopharma, Celgene, Celltrion, Coherus, Dermavant, Dermira, Dice Pharmaceuticals, Dow Pharma, Eli Lilly, Evelo, Forbion, Galderma, Gilead, GlaxoSmithKline (GSK), Incyte, Janssen, Kyowa Hakko Kirin, LEO Pharma, Meiji Seika Pharma, Merck (MSD), Mitsubishi Pharma, Novartis, Pfizer, Regeneron, Reistone, Sanofi Genzyme, Sandoz, Sun Pharma, Takeda, UCB, vTv Therapeutics, and Xencor. Dr. Barbara Melosky has served as an advisory board member for, and/or received honoraria from Roche, Pfizer, Jazz, Novartis, BMS, Merck, BI, Amgen, AZ, Ibsen, Aisai, Lilly, and Janssen. Dr. Sandeep Sehdev has served as an investigator, speaker, and/or advisory board member for, and/or received grants/honoraria from Abbvie, AstraZeneca, Novartis, Lilly, Roche, Bristol Myers Squibb, Merck, Pfizer, Gilead, Seagen, Janssen, Mylan, Apobiologix, Organon, Elvium, and Helsinn. Dr. Sebastien J Hotte has served as an investigator, speaker, and/or advisory board member for, and/or received grants/honoraria from AAA/Novartis, AbbVie, Astellas, AstraZeneca, Ayala, Bayer, BMS, Eisai, Exelixis, Ipsen, Janssen, Merck, Pfizer, Roche, Sanofi, SeaGen, SignalChem. Dr. Jennifer R. Beecker serves as a Counselor for the Dermatology Association of Ontario, CDA President, Director for the National Capital Skin Disease Foundation, and has served as an investigator, speaker, advisor and/or consultant for, and/or received grants/honoraria from: AbbVie, Amgen, Arcutis, Boehringer Ingelheim, Bristol Myers Squibb, Celgene, Concert, Galderma, Eli Lilly, Evelo Biosciences, Incyte, Janssen, Johnson and Johnson, LEO Pharma, L’Oréal Group, Novartis, Pfizer, Reistone, Sanofi Genzyme, Sun Pharma, and UCB. Dr. Mark Kirchhof has served as an advisor/consultant for AbbVie, Actelion, Amgen, Bausch Health, Celgene, Eli Lilly, Janssen, LEO Pharma, Novartis, UCB, Sanofi Genzyme, and served as a speaker for AbbVie, Janssen, LEO Pharma, Novartis, Pfizer, UCB, Sanofi Genzyme. Dr. Irina Turchin has served as an investigator, speaker, and/or advisory board member for, and/or received grants/honoraria from: Abbvie, Amgen, Arcutis, Aristea, Bausch Health, Bristol Myers Squibb (BMS), Boehringer Ingelheim, Celgene, Eli Lilly, Galderma, Incyte, Janssen, Kiniksa, Leo Pharma, Mallinckrodt, Novartis, Pfizer, Sanofi, Sun Pharma, and UCB. Dr. Jan Dutz has served as an advisor/consultant for AbbVie, Amgen, Bausch, Celgene, Janssen, LEO Pharma, Lilly, Novartis, Sanofi, has received grants and honoraria from AbbVie, Janssen, Corbis, Lilly, and has served as a speaker for Celgene, Janssen. JD is supported by a Senior Scientist Award of the BC Children’s Hospital Research Institute. Dr. Melinda J. Gooderham serves as the Vice President of the Dermatology Association of Ontario and has served as an investigator, speaker, advisor and/or consultant for, and/or received grants/honoraria from: AbbVie, Akros, Amgen, Arcutis, Aslan, Aristea, AnaptysBio, Bausch Health, Boehringer Ingelheim, Bristol Myers Squibb, Celgene, Coherus, Dermira, Dermavant, Eli Lilly, Galderma, GlaxoSmithKline (GSK), Incyte, Janssen, Kyowa Kirin, LEO Pharma, MedImmune, Meiji, Merck, Moonlake, Nimbus, Novartis, Pfizer, Regeneron, Reistone, Sanofi Genzyme, Sun Pharma, and UCB. Dr. Robert Gniadecki has served as an advisor/consultant for AbbVie, Bausch, Celgene, Janssen, LEO Pharma, Lilly, Novartis, Mallinckrodt Pharmaceuticals, Sanofi, and served as a speaker for Mallinckrodt Pharmaceuticals, Janssen, Sanofi. Dr. Chih-ho Hong has served as a consultant, advisory board member, and/or speaker for, and/or received grants/honoraria from: Abbvie, Amgen, Bausch Health, Celgene, Dermavant, Eli Lilly, Galderma, GlaxoSmithKline (GSK), Janssen, Leo Pharma, Novartis, Pfizer, Regeneron/Sanofi, Sun Pharma, and UCB. Received research grants for investigator services from Abbvie, Akros, Amgen, Arcutis, Boehringer-Ingelheim, Bristol-Meyers-Squibb, Celgene, Cutanea, Dermira, Dermavant, DS Biopharma, Eli Lilly, Evelo, Galderma, GlaxoSmithKline (GSK), Incyte, Janssen, Leo Pharma, Medimmune, Novartis, Pfizer, Regeneron/Sanofi, Roche, and UCB. Prof. Jo Lambert has received recent grant support from AbbVie, Amgen, Janssen, Novartis, and UCB, and has served as an advisor to/speaker for AbbVie, argenx, Almirall, Bristol-Meyers-Squibb (BMS), MS Pharma inc., Celltrion, Janssen, Novartis, and UCB. All fees are wired to an institutional scientific account, and not to personal benefit. Dr. Charles W. Lynde has served as an advisory board member, speaker, and/or consultant for, and/or received honoraria or grants from: AbbVie, Acelyrin, Akros, Amgen, Anacor, Aralez Pharmaceuticals, Arcutis, Avillion, Bausch Health (Valeant), Boehringer Ingelheim, Bristol Myers Squibb (BMS), Celgene, Celltrion, Coherus, Dermavant, Dermira, Eli Lilly, Evelo, Galderma, Gilead, GlaxoSmithKline (GSK), Incyte, Janssen, Kyowa Hakko Kirin, LEO Pharma, Meiji Seika Pharma, Merck (MSD), Novartis, Pfizer, Regeneron, Sanofi Genzyme, Sandoz, Sun Pharma, Takeda, and UCB. Dr. Vimal H. Prajapati has served as an advisor, consultant, investigator, and/or speaker for for, and/or received grants/honoraria from: AbbVie, Actelion, Amgen, Aralez, Arcutis, Arena, Asana, Aspen, Bausch Health (Valeant), Boehringer Ingelheim, Bristol Myers Squibb (BMS), Celgene, Cipher, Concert, Corrona/CorEvitas, Dermavant, Dermira, Eli Lilly, Galderma, GlaxoSmithKline (GSK), Homeocan, Incyte, Janssen, LEO Pharma, L’Oreal, Medexus, Nimbus Lakshmi, Novartis, Pediapharm, Pfizer, Regeneron, Reistone, Sanofi Genzyme, Sun Pharma, Tribute, and UCB. Dr. Ronald Vender has served as an advisor/consultant and speaker, and received grants/honoraria, from AbbVie, Amgen, Bausch-Health, Celgene, Janssen, Lilly, Merck, Novartis, Pfizer, and UCB.
Compliance with Ethics Guidelines
Ethics committee approval was not required per section 2.3b of the TCPS2 since experts who participated in the surveys are published authors on this work and therefore have no expectation of privacy.
Data Availability
Data summaries are available in article supplementary material. Springer Healthcare is not responsible for the validity of guidelines it publishes.
Author information
Authors and Affiliations
Corresponding author
Additional information
The original online version of this article was revised: Funding note “UCB Canada” added to the list of funders.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Papp, K.A., Melosky, B., Sehdev, S. et al. Use of Systemic Therapies for Treatment of Psoriasis in Patients with a History of Treated Solid Tumours: Inference-Based Guidance from a Multidisciplinary Expert Panel. Dermatol Ther (Heidelb) 13, 867–889 (2023). https://doi.org/10.1007/s13555-023-00905-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-023-00905-3