Abstract
Background
People living with human immunodeficiency virus (PLHIV) have a similar prevalence of psoriasis as the general population, though incidence and severity correlate with HIV viral load. Adequately treating HIV early renders the infection a chronic medical condition and allows PLHIV with a suppressed viral load (PLHIV-s) to live normal lives. Despite this, safety concerns and a lack of high-level data have hindered the use of systemic psoriasis therapies in PLHIV-s.
Objectives
We aim to provide a structured framework that supports healthcare professionals and patients discussing the risks and benefits of systemic psoriasis therapy in PLHIV-s. Our goal was to address the primary question, are responses to systemic therapies for the treatment of psoriasis in PLHIV-s similar to those in the non-HIV population?
Methods
We implemented an inference-based approach relying on indirect evidence when direct clinical trial data were absent. In this instance, we reviewed indirect evidence supporting inferences on the status of immune function in PLHIV. Recommendations on systemic treatment for psoriasis in PLHIV were derived using an inferential heuristic.
Results
We identified seven indirect indicators of immune function informed by largely independent bodies of evidence: (1) functional assays, (2) vaccine response, (3) life expectancy, (4) psoriasis manifestations, (5) rate of infections, (6) rate of malignancies, and (7) organ transplant outcomes.
Conclusions
Drug-related benefits and risks when treating a patient with systemic psoriasis therapies are similar for non-HIV patients and PLHIV with a suppressed viral load and normalized CD4 counts. Prior to initiating psoriasis treatment in PLHIV, HIV replication should be addressed by an HIV specialist. Exercise additional caution for patients with a suppressed viral load and discordant CD4 responses on antiretroviral therapy.
Plain Language Summary
People living with human immunodeficiency virus (PLHIV) develop psoriasis as often as everyone else. We asked: what are effective and safe treatments when PLHIV need systemic therapy (pills or injections) for their psoriasis?
HIV infection attacks the immune system. When HIV is not treated, the immune system declines. A less effective immune system makes it harder for the body to fight infections and certain cancers. Psoriasis is a skin condition caused by overactive immune cells. Effective psoriasis treatments reduce immune-cell activity. There are some concerns that treatments for psoriasis may not work and could worsen infections or cancers.
To answer the question, we gathered 11 dermatologists and 4 HIV specialists. We reviewed the international scientific literature on PLHIV and psoriasis. The absence of direct evidence and volume of information to review made the process challenging. The end results were worthwhile.
We concluded that people who are diagnosed early and take antiretroviral therapy to control their HIV infection (PLHIV-c) can live long, healthy lives. Accordingly, we determined that PLHIV-c can likely expect the same safety and efficacy for systemic psoriasis treatments as the general population. Treatment decisions should be made on a case-by-case basis through consultation with the patient and treating physician(s).
Pillars of modern medicine are evidence-based care and collaborative decision-making. Too often, neither care provider nor patient are adequately informed. We have tried to fill one information gap for PLHIV and psoriasis. This process may help answer questions in other disease populations where direct evidence is scarce or absent.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
People living with human immunodeficiency virus (PLHIV) have similar psoriasis prevalence as the general population and may benefit from systemic psoriasis therapy. |
Use of systemic psoriasis therapies in these patients is hindered by concerns about the alteration of immune function, with its potential increased risks of infection and malignancy. |
PLHIV receiving early antiretroviral therapy can achieve viral load suppression and lead normal lives with a chronic medical condition. |
The present guidance document uses an inference-based approach to explore the risks and benefits imposed on PLHIV when their psoriasis is treated with systemic psoriasis agents. |
Relying on indirect evidence when direct clinical trial data are absent, we provide a structured framework that supports a discussion between healthcare professionals and their patients about the risks and benefits of systemic psoriasis therapy in PLHIV. |
Introduction
As psoriasis is an immune-mediated disease, treatments must alter immunological pathways to be effective. Altered immune function may increase the risks of infection and malignancy. Concerns over these risks heighten when individuals with underlying immune disorders, specifically the human immunodeficiency virus (HIV) infection, seek psoriasis treatment. Psoriasis onset and severity appear to be related to the level of HIV viral control [1]. The prevalence of psoriasis in people living with HIV (PLHIV) is similar to that of the general population when HIV is controlled with antiretroviral therapy (ART) [2, 3]. In the absence of effective ART strategies, infection with HIV can progress to acquired immunodeficiency syndrome (AIDS) with early mortality consequent to specific opportunistic infections (OIs) and infection-associated malignancies [4]. HIV guidelines now recommend starting ART as soon as possible following a confirmed diagnosis of HIV infection, regardless of CD4 count [5]. Successful HIV treatment results in suppressed or undetectable viral load, typically within 6 months of initiation, and globally the goal is to achieve undetectable viral loads in 90% of PLHIV [6]. This may not be achieved in settings of inadequate access or poor adherence resulting from mental health or other social or economic challenges. Treating HIV early renders the infection a chronic medical condition allowing PLHIV with a suppressed viral load on antiretroviral therapy (PLHIV-s) to live normal lives [7].
Though systemic psoriasis therapies may benefit PLHIV-s with psoriasis, safety concerns have hindered their use [1, 8,9,10,11]. Additionally, PLHIV are excluded from psoriasis clinical trials, largely reflective of generally held apprehensions regarding systemic treatments in this population. Systemic therapies for psoriasis block certain immune or metabolic pathways in an effort to normalize the aberrant immune actions manifesting as psoriasis. Immune blockade results in disease control but in parallel raises safety concerns. These concerns stem from our understanding of immune mechanisms relating to risk of infection, risk of malignancy, and possible off-target effects in PLHIV. We can anticipate that differences in immune responses in the PLHIV compared with the non-HIV population would reflect differences in the immunological status between the two populations. Normalization of immune response is sufficient to conclude that the benefits and risks of an intervention are highly similar to those experienced by the general, non-HIV population. Recognizing the paucity of high-level, direct evidence, we implemented a formalized inference-based approach to interrogate indirect evidence of immune response in PLHIV [12]. Inference-based conclusions were made to address the primary guideline question and generate resultant recommendations.
The objective of this paper is to explore the risks and benefits imparted on PLHIV when treating their psoriasis with systemic psoriasis agents, biologics, and small molecules. We provide a structured, inference-based framework that supports a discussion between healthcare professionals and their patients about the risks and benefits of systemic psoriasis therapy in PLHIV. The conclusions are agnostic to specific immune pathways and are therefore applicable to a larger audience of healthcare professionals who manage immune-mediated conditions.
Methods
A panel of 11 dermatologists, three HIV specialists (SLW, JR, AP), and one infectious disease specialist (CLC), convened following the framework of the New Psoriasis Guidelines group [12]. Through panel discussions directed toward identifying observable scenarios, the primary question was deconstructed in a layered, inference-based approach (Table 1). Our objective was to identify data assessing immune response in patients with controlled HIV, including residual immune alteration, and thereby identify the potential for altered risk or efficacy when treating psoriasis. Structured systematic or scoping literature searches were conducted for each deconstructed question. See Supplementary Material S1 for detailed methodology. Working group authors summarized key evidence per topic, which was then reconstructed to generate answers to overarching questions. Within working groups, four to five authors who reviewed and summarized the data for their section also rated their level of support for lower-level statements. A scale of 0–100% was used, based on verbal transformations of subjective probability for use in expert elicitation [13] where 90% meant the statement was likely to be true, and 99% meant the statement was very likely to be true (Supplementary Material S1, Figure S2). One panel member combined the average support levels through a heuristic, mathematical model for logical inference to estimate support for overarching questions (Supplementary Material S2). All panel members accepted or adjusted the resultant levels via online surveys. Following review of the evidence, all panel members drafted and refined the final three recommendation statements and rated their level of support and uncertainty via online surveys. The AGREE II checklist for reporting of clinical practice guidelines was used where applicable [14]. Ethics committee approval was not required as per section 2.3b of the TCPS2 since experts who participated in the surveys are published authors on this work and therefore have no expectation of privacy.
Recommendations and Supporting Evidence
We reviewed indirect evidence to support inferences on the status of immune function in PLHIV-s considering systemic treatment for psoriasis. We identified seven indirect indicators of immune function informed by largely independent bodies of evidence: (1.1.1) functional assays, (1.1.2) vaccine response, (1.1.3) life expectancy, (1.1.4) psoriasis manifestations, (1.1.5) rate of infections, (1.1.6) rate of malignancies, and (1.1.7) organ transplant outcomes. The questions, inference-based concluding statements, and level of support for each statement are summarized below and in Table 1. See Supplementary Material S1 for literature search output and Supplementary Material S2 for summary tables of the evidence reviewed.
1. Are Responses* to Using Systemic Psoriasis Therapies for Treatment of Psoriasis in PLHIV-s Similar to Those in the Non-HIV Population?
*Responses include drug-related adverse events as well as drug-related benefits.
1.1 Are there Substantive Differences in Immune Function in PLHIV-s Compared with the Non-HIV Population?
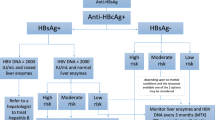
The accumulated weight of the evidence from the seven independent topics complements a similar conclusion: the degree to which an outcome normalizes is dependent upon the degree to which HIV infection is controlled, the period between HIV acquisition and initiation of ART, and adherence to treatment. In the majority of PHLIV-s, adequate CD4 counts indicate immune recovery, but a small number of patients will have discordant responses (persistently low CD4 counts despite viral control) [15]. Owing to the complexity of discordant responses in PLHIV-s, collaboration with HIV specialists is advised when making treatment decisions for systemic psoriasis therapy. Although the literature suggests that 10–40% of HIV‐1‐infected individuals have discordant responses [15], the proportion is likely much lower in countries with early ART established as the standard of care. Conclusion statements were only possible for PHLIV-c because of the limited evidence in patients with discordant responses. On the basis of the indirect evidence, we infer that PLHIV-c will respond to systemic psoriasis treatment similarly to the general population in terms of drug-related benefits and risks (Tables 1, 2). For patients with uncontrolled HIV (i.e., not on treatment or nonsuppressed viral load) presenting with psoriasis, the priority is to start ART, maximize adherence, and achieve HIV viral load suppression prior to considering any new medication for psoriasis.
1.1.1. Do Functional Immune Assays Show Reconstitution of Immune Response in PLHIV-s Compared with the Non-HIV Population?
CD4 + T-cell functional assays trend to normal with control of HIV.
Effective ART normalizes clinically used immune function assays. The degree of normalization is dependent on several factors, predominantly the CD4 counts at initiation of therapy. Plasma HIV RNA is the most reliable indicator of response to ART and is predictive of clinical progression [16, 17]. The goal of ART is viral load suppression below the limits of detection (< 20–50 copies/mL depending on the assay) [18]. Immune recovery in PLHIV is primarily measured by CD4 counts. Absolute CD4 counts above 500 cells/μL are considered functionally normal, whereas counts of 200–500 cells/μL pose concern. At levels < 200 cells/μL, OIs and malignancies may occur [5]. The degree to which immune reconstitution occurs depends largely on the degree of immune impairment prior to initiating ART [15, 19, 20]. CD4 counts prior to ART, the time interval between acquiring HIV and initiating ART, age, lifestyle, comorbidities, and coinfection play contributing roles in immune reconstitution.
1.1.2. Do PLHIV-s Have Similar Response to Vaccines Compared with the Non-HIV Population?
Vaccine response in patients with controlled HIV is similar to that in the non-HIV population.
Vaccine response in a population provides an indirect measure of immune function. HIV-infected patients were shown to have a decreased response to vaccinations such as hepatitis B virus (HBV) vaccine, relative to HIV-negative patients [21,22,23,24]. Many of these studies were conducted prior to the current ART era. More recent studies suggest that HIV control (undetectable viral load and CD4 counts in the normal range) on ART is associated with normalized vaccine effectiveness [25,26,27]. For example, patients with HIV with controlled viral load and CD4 counts > 350 cells/μL had normal responses to the COVID vaccine [28]. Vaccine recommendations vary according to CD4 counts [29], but generally, vaccinations are considered safe and effective in PLHIV with suppressed viral load.
1.1.3. What are the Differences in Mortality Between PLHIV-s and the Non-HIV Population?
The average life expectancy for PLHIV-c approaches that of the non-HIV population.
We reviewed life expectancy as a holistic marker of immune function in the HIV population. Although chronological age is not a direct indicator of immune function and individual life span does not indicate normal immune response, at a population level, improved life expectancy adds to the body of evidence supporting immune recovery in PLHIV-c. Life expectancy for PLHIV has been increasing toward normal as mortality rates decreased with the introduction of ART and earlier adoption of therapy at higher CD4 counts [7, 30,31,32,33,34,35]. According to a 2016 US study, there remains a gap of 6.8 years in life expectancy for PLHIV who start ART with CD4 counts ≥ 500 cells/μL compared with the non-HIV population [30]. It is thought that this life expectancy gap is continuing to narrow, and the persistent gap is largely a consequence of poor adherence to ART, hepatitis C virus (HCV) coinfection, injection drug use, and low socioeconomic status [30, 33, 36, 37]. As life expectancy normalizes, PLHIV are demonstrating increased rates of comorbidities (chronic liver, kidney, cardiovascular, and lung disease, diabetes, and cancer) relative to those without HIV [7, 30, 36, 38]. These comorbidities are considered part of normal aging with HIV for patients on ART but may also be related to lifestyle risks such as smoking, toxicity of older ART agents, and residual inflammation despite control of viral replication. Further, accelerated immunosenescence is associated with chronic HIV; hence, earlier treatment reduces the life expectancy gap by abbreviating the immune burn rate [39]. Similar to the non-HIV population, cardiovascular disease and cancer are major causes of death among PLHIV [36].
1.1.4. Are there Differences in Psoriasis Manifestations in PLHIV-s and the Non-HIV Population?
Manifestations of psoriasis in PLHIV-c are the same as those of the non-HIV population.
PLHIV-s develop psoriasis at about the same rate as the non-HIV population and present with approximately the same spectrum of disease burden as the non-HIV population [40,41,42]. Worse or different forms of psoriasis may be related to the level of HIV control and immune reconstitution [2]. Uncontrolled HIV replication may induce or exacerbate psoriasis [2, 42, 43], whereas HIV-associated psoriasis may improve or resolve upon ART initiation [44,45,46]. Paradoxical worsening of psoriasis through immune reconstitution inflammatory syndrome is rare but possible upon initiating ART [47]. While all clinical subtypes of psoriasis can occur in patients with HIV, erythrodermic, guttate-like, and inverse psoriasis are more common and often concurrent in the same patient [2, 45, 48]. Recognizing that a segment of PLHIV are unaware of their HIV-positive status, dermatologists should consider universal screening and offer HIV testing to all patients with de novo onset of unusual forms of psoriasis or unusual worsening of psoriasis, and in all patients with risk factors for HIV. The normalized presentation and prevalence of psoriasis in patients treated early in infection with ART indirectly supports normalized immune response in PLHIV-c.
1.1.5.1. Are There Differences in the Rate of Infection in PLHIV-s Compared with the Non-HIV Population?
The overall risk of infections, including OIs, is the same in PLHIV-c as in the non-HIV population.
A significant contributor to increased life expectancy in HIV is reduction in infection risk for patients with improved CD4 counts on ART. During infectious processes, common inflammatory pathways and distinct pathogen-dependent immunological mechanisms are activated. In HIV, the major concern has been the reactivation of latent infections that are controlled by T-cell immunity. For bacterial pathogens, the rate of infection in PLHIV-c is extremely low and comparable to rates for non-HIV populations [49]. Patients with discordant CD4/viral load responses have lower bacterial infection rates than patients with uncontrolled HIV but higher rates than PLHIV-c [49, 50]. The occurrence of OIs such as deep fungal infections and toxoplasmosis has decreased in high-income countries with readily available ART. In the developing world where ART is not as accessible, OIs are more frequent and more severe [51, 52]. Suppressed viral load and CD4 counts above 200 cells/μL allow discontinuation of prophylaxis for primary and secondary Pneumocystis jirovecii pneumonia and toxoplasmosis in PLHIV as the risk for these OIs normalizes [53, 54]. Although the incidence of herpes zoster (HZ) in PLHIV remains higher than in the general population [55,56,57,58,59], risk factors include markers of poor immune function, which in turn suggests that appropriate ART reduces HZ risk in this population [55, 56].
1.1.5.2. Are There Additional Risks of Infection in PLHIV-s Compared with the Non-HIV Population When Treated with Systemic Psoriasis Therapies?
There is no increased risk of infection with addition of systemic psoriasis therapy for PLHIV-c compared with the non-HIV population.
For PLHIV-c treated with systemic psoriasis therapies, no additional risks of infection were identified (see Supplementary Material S2 for summary and references) [9, 10, 60].
1.1.6.1 Are There Differences in Rate of Malignancy in PLHIV-s Compared with the Non-HIV Population?
The overall risk of HIV-related malignancies and nonviral malignancies is the same in PLHIV-c as in the non-HIV population.
AIDS-defining cancers (ADCs) such as Kaposi’s sarcoma (KS), aggressive non-Hodgkin lymphoma, and cervical cancer were common in the pre-ART era but are far less common in PLHIV-c [61]. ADCs can still be seen in PLHIV who present late, who do not maintain viral suppression, or those in whom the CD4/CD8 ratio remains low. The shared route of transmission may account for rates of viral-associated malignancies related to human papilloma virus, Epstein–Barr virus, KS-associated herpesvirus (human herpesvirus-8), HBV, and HCV [62]. Although non-ADCs are a leading cause of death in PLHIV-s, there is no evidence for an increase in non-AIDs-defining, nonviral malignancies in persons with HIV (e.g., lung, breast, colon, prostate) independent of identifiable confounders such as smoking [61,62,63,64]. We infer that similar malignancy rates in PLHIV-c and the non-HIV populations supports improved immune function in PLHIV-c. Baseline cancer risk in patients with psoriasis, not considering HIV status, is difficult to assess owing to possible confounding from phototherapy and immunosuppressive therapy, observer bias, and small population size [65]. A recent systemic review and meta-analysis of over 2 million patients showed that the overall risk of cancer was slightly increased in patients with psoriasis, particularly keratinocyte cancer and lymphomas (RR 1.21 CI 1.11–1.33) [66].
1.1.6.2. Are There Additional Risks of Malignancy in PLHIV-s Compared with the Non-HIV Population When Treated with Systemic Psoriasis Therapies?
There is no increased risk of malignancy with addition of systemic psoriasis therapy for PLHIV-c compared with the non-HIV population.
Data on PLHIV treated for psoriasis are limited to case studies without long-term follow-up [8, 67]. For PLHIV-c treated with systemic psoriasis therapies, no additional risks of malignancy were identified (see Supplementary Material S2 for references) [9, 10, 60]. On the basis of pooled data from clinical trials where patients with HIV are excluded, and post-marketing surveillance data, cancer risk in patients with psoriasis remains similar across systemic therapeutic classes, including biologics, small molecules, retinoids, and classic immunosuppressives [65, 66, 68,69,70,71,72]. These results, though weak, lend support to the inference-based conclusion. Acitretin has limited efficacy and is believed to be safe in patients with HIV and psoriasis [73], on the basis of limited to no data. Interestingly, cyclosporine inhibits HIV viral replication in vitro [74]. Conversely, cyclosporine is a potent inhibitor of some immunological processes and requires careful assessment because of known drug–drug interactions with certain ART agents. We briefly draw attention to TNF-alpha, which, like all cytokines, plays a complex role in immune response. Successful infections must bypass immune mechanisms that would otherwise be abortive. Some infections use inflammatory pathways to their benefit. HIV replication, for example, is enhanced by TNF and inhibited by TNF antagonism [75,76,77]. Janus kinase (JAK) inhibitors are a new drug class not currently approved for the treatment of psoriasis that has the potential to reset the immunologic milieu in PLHIV. Targeted inhibition of JAK provides a selective and potent mechanism to inhibit replication of drug-resistant HIV-1, reactivation of latent HIV-1, and HIV-1 replication in lymphocytes and macrophages [78, 79]. Apart from the potential for drug–drug interactions with certain ART agents, we would expect responses to treatment in PLHIV-c to be similar to those in the non-HIV population.
1.1.7. Do PLHIV-s Receiving Allografts Have a Similar Rate of Complications Including Infections and Malignancies Compared with the Non-HIV Population When Treated with Systemic Psoriasis Therapies?
The risk of rejection and complications associated with allografts is the same in PLHIV-c patients as in the non-HIV population.
Successful organ transplantations in PLHIV-s with CD4 counts > 200 cells/μL provide further indirect support for immune system reconstitution in PLHIV-c. Historically, solid organ transplant in PLHIV resulted in a higher risk of rejection compared with non-HIV patients owing to drug–drug interactions and inferior outcomes for HIV/HCV-coinfected recipients. Rejection risk improved with key developments including direct-acting antivirals that mitigate risk imposed by HCV infection [80, 81], and avoidance or modification of ART regimens interacting with immunosuppressant therapy [82,83,84]. Graft survival and patient survival rates of renal transplant in HIV positive mono-infected patients are the same as in non-HIV transplant patients; studies that include HCV-coinfected patients show slightly worse survival in the pre-Direct Acting Antiviral (DAA) era [85,86,87]. This survival disadvantage has likely become insignificant now that DAAs are incorporated into standard of care [88]. Rates of infections, including OIs, and infectious complications are similar between the general HIV and non-HIV transplanted populations [52, 87, 89].
Discussion/Limitations
The present guidance document is a first demonstration of a formal inference-based process, novel to clinical medicine, to guide practice where high-level evidence is lacking [12]. In addition to recommendation statements, we provide inference-based conclusions to guide healthcare professional discussions. This approach is useful in areas where guidance is needed but there is paucity of clinical trials, limited real-world data, and trials are unlikely to be conducted [90, 91]. Practically, clinical decisions must be made in the face of limited evidence, and the process of considering indirect evidence is reflective of what physicians do on a case-by-case basis in the clinical setting. We implemented a formalized methodology that takes the onus off the individual physician to review the data and make conclusions on their own [12]. By breaking the main question down into component parts, addressing the subcomponents, then restructuring the evidence to support a conclusion, we build confidence in the recommendations. The different topics and outcomes explored in this analysis point toward a similar truth, thereby strengthening the overall argument. Previously published guidance on systemic psoriasis therapy use in PLHIV is based on weak evidence, case reports, and case series that are subject to publication and observer bias [1, 8,9,10,11]. On the basis of the limited data reviewed, previous guidance restricts the use of methotrexate and cyclosporine owing to risk of opportunistic infections[9] and suggests the use of acitretin or apremilast [9]. Considering the indirect data, our multidisciplinary group consisting of dermatologists and HIV specialists concurred that patients who have a suppressed HIV viral load and normalized CD4 counts can be treated similarly to the general population, with caution taken for those who have discordant responses or uncontrolled HIV.
It is important to consider the limitations of this document; while comprehensive, the recommendations cannot account for every clinical situation or the needs of each individual patient. There are significant gaps in knowledge, and most of the data are extrapolated from the general population. Therefore, the authors have made the best recommendations with these limited data. Limitations related to the methodology are further discussed in Supplementary Material S1. Beyond HIV, there are other considerations that could impact patient morbidity, mortality, and the safety of agents used to treat psoriasis. These include the increased risk of coinfections such as HBV and HCV resulting from shared transmission risks due to lifestyle factors such as intravenous drug use. PLHIV may also have increased risk for tuberculosis or certain fungal infections depending on their country of origin or other epidemiology. Dose modifications and/or additional monitoring resulting from drug–drug interactions with certain ART agents should be considered prior to prescribing medication for psoriasis. Physicians should consult product monographs and online HIV drug interaction tools (https://hivclinic.ca/wp-content/plugins/php/app.php and/or https://www.hiv-druginteractions.org/).
Conclusion
We reviewed indirect evidence to make inferences about the additional risks and benefits imposed on HIV-positive patients having their psoriasis treated with systemic agents. Robust, adequately powered clinical trials are encouraged but not likely to occur in this population, and there is a need to provide guidance despite the limited evidence. On the basis of our review, we expect PLHIV-c will have similar drug-related adverse events and benefits as non-HIV patients when treated with systemic therapies for psoriasis. Prior to considering new therapies for psoriasis, HIV replication should be addressed. For patients with discordant CD4/viral load responses, additional caution should be taken on a case-by-case basis, with the guidance of an HIV specialist.
Change history
06 July 2023
A Correction to this paper has been published: https://doi.org/10.1007/s13555-023-00950-y
References
Fink D, Hedley L, Miller R. Systematic review of the efficacy and safety of biological therapy for inflammatory conditions in HIV-infected individuals. Int J STD AIDS. 2017;28:110–9.
Morar N, Willis-Owen SA, Maurer T, Bunker CB. HIV-associated psoriasis: pathogenesis, clinical features, and management. Lancet Infect Dis. 2010;10:470–8.
Kanada K, Schupp C, Armstrong A. Association between psoriasis and viral infections in the United States: focusing on hepatitis B, hepatitis C and human immunodeficiency virus. JEADV. 2013;27:1312–6.
Iroezindu M. Disparities in the magnitude of human immunodeficiency virus-related opportunistic infections between high and low/middle-income countries: is highly active antiretroviral therapy changing the trend? Ann Med Health Sci Res. 2016;6:4.
Ford N, Meintjes G, Vitoria M, Greene G, Chiller T. The evolving role of CD4 cell counts in HIV care. Curr Opin HIV AIDS. 2017;12:123–8.
Joint United Nations Programme on HIV/AIDS (UNAIDS). GLOBAL AIDS UPDATE | [Internet]. CONFRONTING INEQUALITIES; 2021 [cited 2020 Sep 5]. https://reliefweb.int/sites/reliefweb.int/files/resources/2021-global-aids-update_en.pdf.
Jespersen NA, Axelsen F, Dollerup J, Nørgaard M, Larsen CS. The burden of non-communicable diseases and mortality in people living with HIV (PLHIV) in the pre-, early- and late-HAART era. HIV Med. 2021;22:478–90.
Menon K, Van Voorhees AS, Bebo BF, Gladman DD, Hsu S, Kalb RE, et al. Psoriasis in patients with HIV infection: from the Medical Board of the National Psoriasis Foundation. J Am Acad Dermatol. 2010;62:291–9.
Kaushik SB, Lebwohl MG. Psoriasis: which therapy for which patient: focus on special populations and chronic infections. J Am Acad Dermatol [Internet]. 2019;80:43–53. https://doi.org/10.1016/j.jaad.2018.06.056.
Nakamura M, Abrouk M, Farahnik B, Zhu TH, Bhutani T. Psoriasis treatment in HIV-positive patients: a systematic review of systemic immunosuppressive therapies. Cutis. 2018;101:38–42.
Lambert JLW, Segaert S, Ghislain PD, Hillary T, Nikkels A, Willaert F, et al. Practical recommendations for systemic treatment in psoriasis in case of coexisting inflammatory, neurologic, infectious or malignant disorders (BETA-PSO: Belgian Evidence-based Treatment Advice in Psoriasis; part 2). J Eur Acad Dermatol Venereol. 2020;34:1914–23.
Papp K, Gooderham M, Lynde C, Poulin Y, Beecker J, Dutz J, et al. Practical and relevant guidelines for the management of psoriasis: an inference-based methodology. Dermatol Ther [Internet]. 2022;12:253–65. https://doi.org/10.1007/s13555-021-00642-5.
Vick S. Degrees of belief, subjective probability and engineering judgment. Reston: American Society of Civil Engineers; 2002.
Brouwers MC, Kho ME, Browman GP, Burgers JS, Cluzeau F, Feder G, et al. AGREE II: advancing guideline development, reporting and evaluation in health care. CMAJ. 2010;182:839–42.
Yang X, Su B, Zhang X, Liu Y, Wu H, Zhang T. Incomplete immune reconstitution in HIV/AIDS patients on antiretroviral therapy: challenges of immunological non-responders. J Leukoc Biol. 2020;107:597–612.
Thiébaut R, Morlat P, Jacqmin-Gadda H, Neau D, Mercié P, Dabis F, et al. Clinical progression of HIV-1 infection according to the viral response during the first year of antiretroviral treatment. AIDS. 2000;14:971–8.
Hughes M, Johnson V, Hirsch M, Bremer J, Elbeik T, Erice A, et al. Monitoring plasma HIV-1 RNA levels in addition to CD4+ lymphocyte count improves assessment of antiretroviral therapeutic response. Ann Intern Med. 1997;126:929–38.
Ellman TM, Alemayehu B, Abrams EJ, Arpadi S, Howard AA, El-Sadr WM. Selecting a viral load threshold for routine monitoring in resource-limited settings: optimizing individual health and population impact: optimizing. J Int AIDS Soc. 2017;20: e25007.
Turner CT, Brown J, Shaw E, Uddin I, Tsaliki E, Roe JK, et al. Persistent T cell repertoire perturbation and T cell activation in HIV after long term treatment. Front Immunol. 2021;12: 634489.
Roul H, Mary-Krause M, Ghosn J, Delaugerre C, Pialoux G, Cuzin L, et al. CD4+ cell count recovery after combined antiretroviral therapy in the modern combined antiretroviral therapy era. AIDS. 2018;32:2605–14.
Beck CR, McKenzie BC, Hashim AB, Harris RC, Nguyen-Van-Tam JS. Influenza vaccination for immunocompromised patients: systematic review and meta-analysis by etiology. J Infect Dis. 2012;206:1250–9.
Barte H, Horvath TH, Rutherford GW. Yellow fever vaccine for patients with HIV infection. Cochrane Database Syst Rev. 2014;1: CD010929.
George VK, Pallikkuth S, Parmigiani A, Alcaide M, Fischl M, Arheart KL, et al. HIV infection worsens age-associated defects in antibody responses to influenza vaccine. J Infect Dis. 2015;211:1959–68.
Colleir AC, Corey L, Murphy VL, Handsfield HH. Antibody to human immunodeficiency virus (HIV) and suboptimal response to hepatitis B vaccination. Ann Intern Med. 1988;109:101–5.
Mena G, García-Basteiro AL, Bayas JM. Hepatitis B and A vaccination in HIV-infected adults: a review. Hum Vaccin Immunother. 2015;11:2582–98.
Huang SH, Huang CH, Wang NC, Chen TC, Lee YT, Lin SP, et al. Early seroreversion after 2 doses of hepatitis a vaccination in human immunodeficiency virus-positive patients: incidence and associated factors. Hepatology. 2019;70:465–75.
Shafran SD. Live attenuated herpes zoster vaccine for HIV-infected adults. HIV Med. 2016;17:305–10.
Frater J, Ewer KJ, Ogbe A, Pace M, Adele S, Adland E, et al. Safety and immunogenicity of the ChAdOx1 nCoV-19 (AZD1222) vaccine against SARS-CoV-2 in HIV infection: a single-arm substudy of a phase 2/3 clinical trial. Lancet HIV. 2021;8:e474–85.
Centers for Disease Control and Prevention. HIV infection and adult vaccination [Internet]; 2016 [cited 2021 Jul 2]. https://www.cdc.gov/vaccines/adults/rec-vac/health-conditions/hiv.html.
Marcus JL, Leyden WA, Alexeeff SE, Anderson AN, Hechter RC, Hu H, et al. Comparison of overall and comorbidity-free life expectancy between insured adults with and without HIV infection, 2000–2016. JAMA Netw Open. 2020;3: e207954.
Althoff KN, Chandran A, Zhang J, Arevalo WM, Gange SJ, Sterling TR, et al. Life-expectancy disparities among adults with HIV in the United States and Canada: the impact of a reduction in drug- and alcohol-related deaths using the lives saved simulation model. Am J Epidemiol. 2019;188:2097–109.
Frank TD, Carter A, Jahagirdar D, Biehl MH, Douwes-Schultz D, Larson SL, et al. Global, regional, and national incidence, prevalence, and mortality of HIV, 1980–2017, and forecasts to 2030, for 195 countries and territories: a systematic analysis for the Global Burden of Diseases, Injuries, and Risk Factors Study 2017. Lancet HIV. 2019;6:e831–59.
Lima VD, Eyawo O, Ma H, Lourenco L, Chau W, Hogg RS, et al. The impact of scaling-up combination antiretroviral therapy on patterns of mortality among HIV-positive persons in British Columbia, Canada. J Int AIDS Soc. 2015;18:20261.
Nsanzimana S, Remera E, Kanters S, Chan K, Forrest JI, Ford N, et al. Life expectancy among HIV-positive patients in Rwanda: a retrospective observational cohort study. Lancet Glob Health [Internet]. Nsanzimana et al. Open Access article distributed under the terms of CC BY-NC-SA; 2015;3:e169–77. https://doi.org/10.1016/S2214-109X(14)70364-X.
Edwards JK, Cole SR, Breger TL, Rudolph JE, Filiatreau LM, Buchacz K, et al. Mortality among persons entering HIV care compared with the general U.S. population. Ann Intern Med. 2021;174:1197–206.
Trickey A, May MT, Vehreschild JJ, Obel N, Gill MJ, Crane HM, et al. Survival of HIV-positive patients starting antiretroviral therapy between 1996 and 2013: a collaborative analysis of cohort studies. Lancet HIV. 2017;4:e349–56.
Glesby MJ, Gulick RM. HIV: closing the mortality gap. Ann Intern Med. 2021;174:1311–2.
Obel N, Omland LH, Kronborg G, Larsen CS, Pedersen C, Pedersen G, et al. Impact of non-HIV and HIV risk factors on survival in HIV-infected patients on HAART: a population-based nationwide cohort study. PLoS One. 2011;6: e22698.
Deeks SG. HIV infection, inflammation, immunosenescence, and aging. Annu Rev Med. 2011;62:141–55.
Lebrun D, Hentzien M, Cuzin L, Rey D, Joly V, Cotte L, et al. Epidemiology of autoimmune and inflammatory diseases in a French nationwide HIV cohort. AIDS. 2017;31:2159–66.
Parperis K, Abdulqader Y, Myers R, Bhattarai B, Al-Ani M. Rheumatic diseases in HIV-infected patients in the post-antiretroviral therapy era: a tertiary care center experience. Clin Rheumatol. 2019;38:71–6.
Tan J, Pina A, Borges-Costa J. Skin diseases in the era of highly active antiretroviral therapy: a retrospective study of 534 patients. J Int Assoc Provid AIDS Care. 2018;17:2325957417752255.
Alpalhão M, Borges-Costa J, Filipe P. Psoriasis in HIV infection: an update. Int J STD AIDS. 2019;30:596–604.
Chiricozzi A, Saraceno R, Cannizzaro MV, Nisticò SP, Chimenti S, Giunta A. Complete resolution of erythrodermic psoriasis in an HIV and HCV patient unresponsive to antipsoriatic treatments after highly active antiretroviral therapy (Ritonavir, Atazanavir, Emtricitabine, Tenofovir). Dermatology. 2012;225:333–7.
Bartlett BL, Khambaty M, Mendoza N, Tremaine AM, Gewirtzman A, Tyring SK, et al. Dermatological management of human immunodeficiency virus (HIV). Ski Ther Lett. 2007;12:1–3.
Vano-Galvan S, Jaen P. Severe psoriasis due to cessation of antiretroviral therapy in a patient with human immunodeficiency virus. Isr Med Assoc J. 2008;10:557–8.
Tripathi SV, Leslie KS, Maurer TA, Amerson EH. Psoriasis as a manifestation of HIV-related immune reconstitution inflammatory syndrome. J Am Acad Dermatol [Internet]. 2015;72:e35–6. https://doi.org/10.1016/j.jaad.2014.09.032.
Motswaledi MH, Visser W. The spectrum of HIV-associated infective and inflammatory dermatoses in pigmented skin. Dermatol Clin [Internet]. 2014;32:211–25. https://doi.org/10.1016/j.det.2013.12.006.
Collin A, Le Marec F, Vandenhende MA, Lazaro E, Duffau P, Cazanave C, et al. Incidence and risk factors for severe bacterial infections in people living with HIV. ANRS CO3 Aquitaine cohort, 2000–2012. PLoS One. 2016;11: e0152970.
Brecher CW, Aviram G, Boiselle PM. CT and radiography of bacterial respiratory infections in AIDS patients. Am J Roentgenol. 2003;180:1203–9.
Armstrong-James D, Meintjes G, Brown GD. A neglected epidemic: fungal infections in HIV/AIDS. Trends Microbiol [Internet]. 2014;22:120–7. https://doi.org/10.1016/j.tim.2014.01.001.
Ailioaie O, Arzouk N, Valantin MA, Tourret J, Calin RO, Turinici M, et al. Infectious complications in HIV-infected kidney transplant recipients. Int J STD AIDS. 2018;29:341–9.
Miro JM, Lopez JC, Podzamczer D, Peña JM, Alberdi J, Martínez E, et al. Discontinuation of primary and secondary Toxoplasma gondii prophylaxis is safe in HIV-infected patients after immunological restoration with highly active antiretroviral therapy: results of an open, randomized, multicenter clinical trial. Clin Infect Dis. 2006;43:79–89.
Lopez Bernaldo de Quiros J, Miro J, Peña J, Podzamczer D, Alberdi J, Martínez E, et al. A randomized trial of the discontinuation of primary and secondary prophylaxis against Pneumocystis carinii pneumonia after highly active antiretroviral therapy in patients with HIV infection. Grupo de Estudio del SIDA 04/98. N Engl J Med. 2001;344:159–67.
Gebo KA, Kalyani R, Moore RD, Polydefkis MJ. The incidence of, risk factors for, and sequelae of herpes zoster among HIV patients in the highly active antiretroviral therapy era. J Acquir Immune Defic Syndr. 2005;40:169–74.
Blank L, Polydefkis M, Moore R, Gebo M. Herpes zoster among persons living with HIV in the current antiretroviral therapy era. J Acquir Immune Defic Syndr. 2012;61:203–7.
Grabar S, Tattevin P, Selinger-Leneman H, De La Blanchardiere A, De Truchis P, Rabaud C, et al. Incidence of herpes zoster in HIV-infected adults in the combined antiretroviral therapy era: results from the FHDH-ANRS CO4 cohort. Clin Infect Dis. 2015;60:1269–77.
Gilbert L, Wang X, Deiss R, Okulicz J, Maves R, Schofield C, et al. Herpes zoster rates continue to decline in people living with human immunodeficiency virus but remain higher than rates reported in the general US population. Clin Infect Dis. 2019;69:155–8.
Vafai A, Berger M. Zoster in patients infected with HIV: a review. Am J Med Sci. 2001;321:372–80.
Attallah MA, Jarrin Jara MD, Gautam AS, Peesapati VSR, Khan S. A review of the use of biological agents in human immunodeficiency virus positive patients with rheumatological diseases. Cureus. 2020;12: e10970.
Lurain K, Yarchoan R, Ramaswami R. The changing face of HIV-associated malignancies: advances, opportunities, and future directions. Am Soc Clin Oncol Educ B. 2019;36–40.
Vangipuram R, Tyring S. AIDS-associated malignancies. In: Meyers C, editor. HIV/AIDS-Assoc Viral Oncog. Cancer Treat Res. 2nd ed. Cham: Springer; 2019. p. 1–22.
Grulich AE, van Leeuwen MT, Falster MO, Vajdic CM. Incidence of cancers in people with HIV/AIDS compared with immunosuppressed transplant recipients: a meta-analysis. Lancet. 2007;370:59–67.
Cobucci RNO, Lima PH, de Souza PC, Costa VV, Cornetta M da C de M, Fernandes JV, et al. Assessing the impact of HAART on the incidence of defining and non-defining AIDS cancers among patients with HIV/AIDS: a systematic review. J Infect Public Health. 2015;8:1–10.
Geller S, Xu H, Lebwohl M, Nardone B, Lacouture ME, Kheterpal M. Malignancy risk and recurrence with psoriasis and its treatments: a concise update. Am J Clin Dermatol. 2018;19:363–75.
Vaengebjerg S, Skov L, Egeberg A, Loft ND. Prevalence, incidence, and risk of cancer in patients with psoriasis and psoriatic arthritis: a systematic review and meta-analysis. JAMA Dermatol. 2020;156:421–9.
Montes-Torres A, Aparicio G, Rivera R, Vilarrasa E, Marcellán M, Notario J, et al. Safety and effectiveness of conventional systemic therapy and biological drugs in patients with moderate to severe psoriasis and HIV infection: a retrospective multicenter study. J Dermatolog Treat. 2019;30:461–5.
Lebwohl M, Deodhar A, Griffiths CEM, Menter MA, Poddubnyy D, Bao W, et al. The risk of malignancy in patients with secukinumab-treated psoriasis, psoriatic arthritis and ankylosing spondylitis: analysis of clinical trial and postmarketing surveillance data with up to five years of follow-up. Br J Dermatol. 2021;185:935–44.
Peleva E, Exton LS, Kelley K, Kleyn CE, Mason KJ, Smith CH. Risk of cancer in patients with psoriasis on biological therapies: a systematic review. Br J Dermatol. 2018;178:103–13.
Bonovas S, Minozzi S, Lytras T, González-Lorenzo M, Pecoraro V, Colombo S, et al. Risk of malignancies using anti-TNF agents in rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis: a systematic review and meta-analysis. Expert Opin Drug Saf [Internet]. 2016;15:35–54. https://doi.org/10.1080/14740338.2016.1238458.
Garcia-Doval I, Descalzo MA, Mason KJ, Cohen AD, Ormerod AD, Gómez-García FJ, et al. Cumulative exposure to biological therapy and risk of cancer in patients with psoriasis: a meta-analysis of Psonet studies from Israel, Italy, Spain, the U.K. and Republic of Ireland. Br J Dermatol. 2018;179:863–71.
Mease PJ, Gladman DD, Gomez-Reino JJ, Hall S, Kavanaugh A, Lespessailles E, et al. Long-term safety and tolerability of apremilast versus placebo in psoriatic arthritis: a pooled safety analysis of three phase III, randomized controlled trials. ACR Open Rheumatol. 2020;2:459–70.
Blanche P. Acitretin and AIDS-related Reiter’s disease. Clin Exp Rheumatol. 1999;17:105–6.
Glowacka P, Rudnicka L, Warszawik-Hendzel O, Sikora M, Goldust M, Gajda P, et al. The antiviral properties of cyclosporine. Focus on coronavirus, hepatitis C virus, influenza virus, and human immunodeficiency virus infections. Biology (Basel). 2020;9:192.
Pasquereau S, Kumar A, Herbein G. Targeting TNF and TNF receptor pathway in HIV-1 infection: from immune activation to viral reservoirs. Viruses. 2017;9:64.
Rosenberg ZF, Fauci AS. Immunopathogenic mechanisms of HIV infection: cytokine induction of HIV expression. Immunol Today. 1990;11:176–80.
Herbein G, Khan KA. Is HIV infection a TNF receptor signalling-driven disease? Trends Immunol. 2008;29:61–7.
Gavegnano C, Detorio M, Montero C, Bosque A, Planelles V, Schinazi RF. Ruxolitinib and tofacitinib are potent and selective inhibitors of HIV-1 replication and virus reactivation in vitro. Antimicrob Agents Chemother. 2014;58:1977–86.
Marconi V, Moser C, Gavegnano C, Deeks S, Lederman M, Overton E, et al. Randomized trial of ruxolitinib in antiretroviral-treated adults with HIV vincent. Clin Infect Dis. 2021;ciab212 [ePub].
Moreno-Ramirez M, Villanego F, Vigara LA, Cazorla JM, Naranjo J, Garcia T, et al. Direct-acting antiretroviral therapy in renal transplant recipients with human immunodeficiency virus-hepatitis C virus coinfection: report of our experience and literature review. Transplant Proc. 2020;52:523–6.
Grottenthaler JM, Werner CR, Steurer M, Spengler U, Berg T, Engelmann C, et al. Successful direct acting antiviral (DAA) treatment of HCV/HIV-coinfected patients before and after liver transplantation. PLoS One. 2018;13: e0197544.
Camargo JF, Rosa R, Suarez JF, Lorio MA, Morris MI, Abbo LM, et al. Impact of antiretroviral therapy on clinical outcomes in HIV+ kidney transplant recipients: review of 58 cases. F1000Research. 2016;5:2893.
Sawinski D, Shelton BA, Mehta S, Reed RD, MacLennan PA, Gustafson S, et al. Impact of protease inhibitor-based anti-retroviral therapy on outcomes for HIV+ kidney transplant recipients. Am J Transplant. 2017;17:3114–22.
Primeggia J, Timpone JG, Kumar PN. Pharmacologic issues of antiretroviral agents and immunosuppressive regimens in HIV-infected solid organ transplant recipients. Infect Dis Clin North Am. 2013;27:473–86.
Locke JE, Mehta S, Reed RD, MacLennan P, Massie A, Nellore A, et al. A national study of outcomes among HIV-infected kidney transplant recipients. J Am Soc Nephrol. 2015;26:2222–9.
Sawinski D, Forde KA, Eddinger K, Troxel AB, Blumberg E, Tebas P, et al. Superior outcomes in HIV-positive kidney transplant patients compared with HCV-infected or HIV/HCV-coinfected recipients. Kidney Int. 2015;88:341–9.
Alfano G, Mori G, Fontana F, Dolci G, Baisi A, Ligabue G, et al. Clinical outcome of kidney transplantation in HIV-infected recipients: a retrospective study. Int J STD AIDS. 2018;29:1305–15.
Peters MG, Kottilil S, Terrault N, Amara D, Husson J, Huprikar S, et al. Retrospective-prospective study of safety and efficacy of sofosbuvir-based direct-acting antivirals in HIV/HCV-coinfected participants with decompensated liver disease pre- or post-liver transplant. Am J Transplant. 2021;21:1780–8.
Zheng X, Gong L, Xue W, Zeng S, Xu Y, Zhang Y, et al. Kidney transplant outcomes in HIV-positive patients: a systematic review and meta-analysis. AIDS Res Ther [Internet]. 2019;16:37. https://doi.org/10.1186/s12981-019-0253-z.
O’Hagan A, Buck C, Daneshkhah A, Eiser J, Garthwaite P, Jenkinson D, et al. Uncertain judgements: eliciting experts’ probabilities. New York: Wiley; 2006.
Expert OA, Elicitation K. Subjective but scientific. Am Stat. 2019;73:69–81.
Acknowledgements
We thank the following professional and patient organizations for their support and endorsement of this guideline’s initiative: Alberta Society of Dermatologists, Atlantic Provinces Dermatology Association, Association des médecins spécialistes dermatologues du Québec, Dermatology Association of Ontario, The Dermatologic Society of Manitoba, Saskatchewan Dermatology Association, Canadian Association of Psoriasis Patients, Canadian Skin Patient Alliance.
Funding
This project was initiated and financially sponsored by the Dermatology Association of Ontario. Unrestricted educational grants have been provided by the following industry partners (listed alphabetically): AbbVie Inc., Amgen Inc., Janssen Inc., LEO Pharma Inc., Novartis Pharmaceuticals Inc., SUN Pharmaceuticals Ltd., and UCB Canada Inc. These grants were pooled and used to pay for the journal’s Rapid Service Fee as well as medical writing assistance as outlined below. Funders did not influence the content of the project.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
All authors contributed to the study conception, writing of the draft related to their section (see Supplementary Material S1), review and editing of the manuscript.
Methodology: Kim A. Papp, Jan P. Dutz, Mark G. Kirchhof, Robert Gniadecki, Catherine Maari.
Data analysis, Resources and Supervision: Kim A. Papp.
Funding acquisition: Kim A. Papp, Melinda J. Gooderham, Charles W. Lynde, Yves Poulin.
Medical Writing, Editorial, and Other Assistance
Anna Czerwonka, H BSc, Malwina Mencel, PhD, Stephanie Swift, PhD, and Elodie Varin, PhD, of FUSE Health (Toronto, ON) provided professional medical writing services and organizational support for this manuscript as detailed in funding section above.
Disclosures
Dr. Kim Papp has served as an investigator, speaker, advisor/consultant for and/or received grants/honoraria from AbbVie, Akros, Amgen, Anacor, Arcutis, Astellas, AstraZeneca, Bausch Health, Baxalta, Baxter, Boehringer Ingelheim, Bristol Myers Squibb, CanFite, Celgene, Coherus, Dermira, Dermavant, Dow Pharma, Eli Lilly, Forward Pharma, Galderma, Genentech, GlaxoSmithKline, Janssen, Kyowa Hakko Kirin, LEO Pharma, Meiji Seika Pharma, Merck (MSD), Merck-Serono, Mitsubishi Pharma, Novartis, Pfizer, Regeneron, Roche, Sanofi Genzyme, Takeda, and UCB.
Dr. Jennifer Beecker has served as an investigator, speaker, advisor/consultant for and/or received grants/honoraria from AbbVie, Amgen, Boehringer Ingelheim, Bristol Myers Squibb, Celgene, Concert, Galderma, Eli Lilly, Incyte, Janssen, Johnson and Johnson, Leo Pharma, L’Oréal Group, Novartis, Pfizer, Reistone, Sanofi Genzyme, and UCB.
Dr. Curtis Cooper has served as a speaker and advisor for AbbVie, Astra Zeneca, Gilead Sciences, and ViiV Healthcare.
Dr. Mark Kirchhof has served as an advisor/consultant for AbbVie, Actelion, Amgen, Bausch Health, Celgene, Eli Lilly, Janssen, LEO Pharma, Novartis, UCB, Sanofi Genzyme, and served as a speaker for AbbVie, Janssen, LEO Pharma, Novartis, Pfizer, UCB, Sanofi Genzyme.
Dr. Anton Pozniak is a member of the advisory boards and symposia for ViiV, Gilead, Janssen and Merck.
Dr. Juergen Rockstroh has served as an advisor/consultant and/or a speaker for Abivax, Gilead, Merck, Abbvie, Janssen, Theratechnologies, and ViiV.
Dr. Jan Dutz has served as an advisor/consultant for AbbVie, Amgen, Bausch, Celgene, Janssen, LEO Pharma, Lilly, Novartis, Sanofi, has received grants and honoraria from AbbVie, Janssen, Corbis, Lilly, and has served as a speaker for Celgene, Janssen. JD is supported by a Senior Scientist Award of the BC Children’s Hospital Research Institute.
Dr. Melinda Gooderham has served as an investigator, speaker, advisor and/or consultant for AbbVie, Akros, Amgen, AnaptysBio, Arena, Arcutis, Asana, Aslan, Bausch Health, Boehringer Ingelheim, Bristol Myers Squibb, Celgene, Coherus, Dermira, Dermavant, Eli Lilly, Galderma, GlaxoSmithKline, Incyte, Janssen, Kyowa Kirin, LEO Pharma, MedImmune, Merck, Novartis, Pfizer, Regeneron, Roche, Sanofi Genzyme, Sun Pharma, Takeda, and UCB.
Dr. Robert Gniadecki has served as an advisor/consultant for AbbVie, Bausch, Celgene, Janssen, LEO Pharma, Lilly, Novartis, Mallinckrodt Pharmaceuticals, Sanofi, and served as a speaker for Mallinckrodt Pharmaceuticals, Janssen, Sanofi.
Dr. Chih-ho Hong has served as an investigator, speaker, advisor and/or consultant for AbbVie, Amgen, Actelion, Akros, Arcutis, Bristol Myers Squibb, Boehringer-Ingelheim, Celgene, Dermira, Dermavant, Eli-Lilly, Galderma, GlaxoSmithKline, Incyte, Janssen, LEO Pharma, MedImmune, Merck, Novartis, Pfizer, Regeneron, Roche, Sanofi-Genzyme, Sun Pharma, UCB and Valeant (Bausch Health).
Dr. Charles W Lynde has served as an Advisory Board Member, Speaker, Consultant for and/or received honoraria or grants from, AbbVie, Amgen, Bausch Health, Celgene, Eli Lilly, Janssen, GlaxoSmithKline, LEO Pharma, Merck, Novartis, Pfizer, UCB, Valeant.
Dr. Catherine Maari has served as an Investigator, Advisory Board Member, Speaker, Consultant for, and/or received honoraria or grants from, AbbVie, UCB, Boehringer Ingelheim, Celgene, Eli Lilly, Galderma, LEO Pharma, GlaxoSmithKline-Stiefel, Janssen, Novartis, Bausch and Pfizer.
Dr. Yves Poulin has received grants/honoraria from AbbVie, Amgen, Aquinox, Aralez, Baxalta, Biogen, Boehringer Ingelheim, Bristol Myers Squibb, Celgene, Dermira, DS Biopharma, Eli Lilly, EMD Serono, Galderma, GlaxoSmithKline, Janssen, LEO Pharma, MedImmune, Merck, Novartis, Pfizer, Regeneron, Takeda, UCB Pharma, and Valeant.
Dr. Ronald Vender has served as an advisor/consultant and speaker, and received grants and honoraria, from AbbVie, Amgen, Bausch-Health, Celgene, Janssen, Lilly, Merck, Novartis, Pfizer, and UCB.
Dr. Sharon Walmsley has served as an advisor/consultant and speaker, and received grants and honoraria, from ViiV Healthcare, Gilead, GlaxoSmithKline, Janssen and Merck.
Compliance with ethics guidelines
Ethics committee approval was not required as per section 2.3b of the TCPS2 since experts who participated in the surveys are published authors on this work and therefore have no expectation of privacy.
Data availability
Data available in article supplementary material.
Author information
Authors and Affiliations
Corresponding author
Additional information
The original online version of this article was revised: Funding note “UCB Canada” added to the list of funders.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Papp, K.A., Beecker, J., Cooper, C. et al. Use of Systemic Therapies for Treatment of Psoriasis in People Living with Controlled HIV: Inference-Based Guidance from a Multidisciplinary Expert Panel. Dermatol Ther (Heidelb) 12, 1073–1089 (2022). https://doi.org/10.1007/s13555-022-00722-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-022-00722-0