Abstract
Introduction
Real-world evidence has demonstrated the effectiveness of secukinumab in the treatment of psoriasis; however, limited data are available on patient profiles of US secukinumab initiators over time and clinical outcomes in biologic-naive patients. This study describes clinical characteristics of secukinumab initiators by year, and the clinical outcomes in patients after 6- and/or 12-month follow-up visits, stratified by prior biologic use.
Methods
This observational study included patients enrolled in the CorEvitas (formerly Corrona) Psoriasis Registry. Analyses were conducted in two patient cohorts: (1) all secukinumab initiators, stratified by year, and (2) those who initiated and maintained secukinumab through a 6- and/or 12-month follow-up visit. For all secukinumab initiators, patient characteristics at initiation were described per calendar year; in initiators with follow-up visits, mean (SD) differences in percentage affected body surface area (BSA), five-point Investigator’s Global Assessment (IGA), and Psoriasis Area and Severity Index (PASI) scores between baseline and follow-up visits were calculated. Analyses were conducted separately for biologic-naive and biologic-experienced patients.
Results
Between 2015 and 2020, the proportion of secukinumab initiators in the registry who were biologic-naive increased each year from 12.5% to 49.7%. Overall, 1518 patients initiated secukinumab at or after enrollment; 980 (64.6%) were biologic experienced, and 538 (35.4%) were biologic naive. At 6 months, biologic-experienced and biologic-naive patients reported mean (SD) decreases in BSA (−9.3 [14.5] versus −11.7 [16.6]), IGA (−1.4 [1.3] versus −1.7 [1.4]), and PASI (−5.2 [6.6] versus −6.7 [7.8]). The proportion of patients with an IGA score of clear/almost clear (0/1) increased over fivefold, irrespective of biologic experience. At 12 months, similar improvements were seen.
Conclusions
The proportion of biologic-naive secukinumab initiators increased over time. Biologic-naive patients demonstrated similar improvements in clinical outcomes compared with biologic-experienced patients, suggesting that secukinumab may be considered as a first-line therapy for psoriasis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Secukinumab, a fully human anti-interleukin 17A monoclonal antibody approved by the US Food and Drug Administration in 2015, has shown real-world effectiveness in the treatment of moderate to severe psoriasis. |
Limited information describing the patient profiles of secukinumab initiators or their long-term clinical outcomes within the USA is available, particularly in biologic-naive patients. |
What was learned from this study? |
In US patients with psoriasis enrolled in the CorEvitas Psoriasis Registry, the proportion of biologic-naive patients initiating secukinumab increased per observation year. |
Patients who maintained secukinumab treatment through 12 months of follow-up achieved improvements in psoriasis clinical outcomes, irrespective of prior biologic use. |
Biologic-naive patients appeared to show similar improvements to biologic-experienced patients across all outcomes when stratified by prior biologic use. |
Introduction
Psoriasis is a chronic, immune-mediated disease that affects 2–4% of adults in the USA and is characterized by classic clinical symptoms, including skin itching, pain, and scaling [1, 2]. Clinical presentation of psoriasis is often heterogeneous in nature, which can cause difficulty in obtaining a comprehensive assessment of disease burden. Several established measures of disease activity have been validated for use in psoriasis and are used by dermatologists to measure disease severity. These measures can also aid in treatment strategy decisions [3,4,5].
There are numerous treatment options available for patients with moderate to severe psoriasis, including tumor necrosis factor-α inhibitors (TNFis), as well as nonbiologic systemic therapies, such as methotrexate and apremilast [6,7,8]. TNFis were the first US Food and Drug Administration (FDA)-approved biologics and have historically been prescribed as a first-line biologic therapy [9]. The subsequent development and approval of newer biologics with different mechanisms of actions, such as those targeting interleukin (IL)-17, IL-23, or IL-12/23, have provided additional promising treatment options for patients with moderate to severe psoriasis [7]. Approved by the FDA for the treatment of moderate to severe psoriasis in 2015, secukinumab is a fully human monoclonal antibody that selectively inhibits IL-17A. Multiple clinical trials have demonstrated the efficacy and safety of secukinumab and its clinical benefit over other biologics, such as etanercept and ustekinumab, in the treatment of psoriasis [10,11,12], including for difficult-to-treat areas, such as the scalp, palms, nails, and soles of the feet [13,14,15,16]. Using clinical disease activity measures, numerous studies have reported the positive impact of secukinumab effectiveness in real-world settings [17,18,19,20].
Despite the impact of secukinumab on treatment of psoriasis, limited data are available regarding the prescription initiation trends of secukinumab over time, particularly in biologic-naive patients. Understanding real-world prescription drug initiation patterns of patients with psoriasis can provide valuable insights into patient demographics, shifts in disease burden, and changes in the adoption of different therapies [21,22,23]. Adding to the knowledge gained from initiator trends, following patients through their treatment journey can provide a comprehensive understanding of the effectiveness of biologics to better inform clinical practice decisions. However, limited data on effectiveness are available for biologic-naive patients in the USA, particularly beyond 6 months.
Recent trends suggest that the number of secukinumab prescribers is increasing [24]; however, there is a knowledge gap surrounding key clinical and demographic characteristics of patients initiating secukinumab over time. The rising number of secukinumab prescribers may be an indication of the changing prescribing trends of dermatologists. The objectives of this study were to characterize patients with psoriasis initiating secukinumab over time and to describe changes in disease severity among biologic-naive and biologic-experienced patients who maintained secukinumab through 6 and/or 12 months.
Methods
Data Source
The CorEvitas Psoriasis Registry, an independent, prospective, observational cohort of patients, was launched in collaboration with the National Psoriasis Foundation in April 2015 [25]. Patients are invited to enroll in the registry if they meet the following inclusion criteria: age ≥ 18 years, diagnosed with psoriasis by a dermatologist, and initiated or switched to an FDA-approved systemic or biologic treatment for psoriasis within the 12 months preceding enrollment in the registry. Through 10 December 2020, patients were recruited by 547 practicing dermatologists from 255 private and academic clinical sites across 46 states or provinces throughout the USA and Canada.
Data were collected via questionnaires completed by patients and their treating dermatologists during routine clinical office visits occurring approximately every 6 months. All authors meet the International Committee of Medical Journal Editors criteria for authorship for this article, take responsibility for the integrity of the work as a whole, were involved in drafting and critical review of the manuscript, and approved the final version for submission. All authors agree to be accountable for all aspects of the work and attest to the accuracy and integrity of the work. Sponsor approval and continuing review were obtained through a central institutional review board (IntegReview, protocol number is Corrona-PSO-500). All registry patients were required to provide written informed consent prior to participating. Data collection was conducted in accordance with the ethical principles that have their origin in the Declaration of Helsinki and are consistent with the Guidelines for Good Clinical Practice.
Study Design and Patient Populations
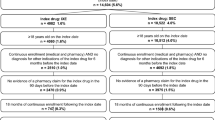
This study included US patients with psoriasis enrolled in the CorEvitas Psoriasis Registry who initiated secukinumab (baseline visit) between 15 April 2015 and 10 December 2020. Analyses included two populations: (1) all patients who initiated secukinumab treatment at or after entry into the registry (N = 1518) stratified by the year patients began secukinumab treatment and (2) patients who maintained continuous secukinumab treatment through a 6-month (n = 652) and/or 12-month follow-up visit (n = 390) (Fig. 1).
Three cohorts were created, comprising patients who maintained secukinumab and completed a 6-month and/or 12-month follow-up visit (Fig. 1). The cohorts consisted of patients who initiated and maintained secukinumab through the following: (1) a follow-up visit within 6 months of their baseline visit (window, 5–9 months; n = 652), (2) a follow-up visit within 12 months of their baseline visit (window, 11–15 months; n = 390), or (3) both a 6- and 12-month follow-up visit (n = 326).
Patients were stratified by prior exposure to biologics (biologic naive versus biologic experienced). Biologic-naive patients were defined as having no history of biologic medication use for the treatment of psoriasis at the time of secukinumab initiation. Patients who were biologic experienced had a history of prior use of ≥ 1 biologic medication for the treatment of psoriasis at the time of secukinumab initiation.
Patient and Clinical Variables
Data collected from questionnaires at the time of secukinumab initiation included patient demographics (age and insurance type), clinical characteristics (psoriasis disease duration, comorbid psoriatic arthritis, body weight, and physician-reported history of comorbidities), and treatment history (nonbiologic systemic naive status and prior and current biologic use).
Disease activity measures collected at all visits included dermatologist-assessed disease severity by percentage of affected body surface area (BSA) (0–100%), five-point Investigator’s Global Assessment (IGA) scores (0 [clear], 1 [almost clear], 2 [mild], 3 [moderate], or 4 [severe]), and Psoriasis Area and Severity Index (PASI) scores (0–72).
Data Analysis
For all secukinumab initiators, descriptive statistics for patient demographics and clinical characteristics at the time of initiation were calculated and stratified by calendar year.
For patients who initiated and maintained secukinumab through follow-up visits, analyses were conducted separately for those who were biologic naive and those who were biologic experienced. Patient characteristics at secukinumab initiation (baseline) are summarized using frequency counts or percentages for categorical variables and mean and SD for continuous variables. For disease activity measures, change in IGA score from baseline to 6- and/or 12-month follow-up, as a categorical variable, is expressed as the frequency count and percentage of patients in each category at baseline and subsequent follow-ups. Categorical shifts for each domain were determined by the number and percent of patients who changed to a different category at follow-up. Mean changes in BSA, IGA, and PASI scores, along with SDs, were calculated as the difference in outcome measure at follow-up from baseline, such that a negative change indicates that the score decreased over time.
Results
Characteristics over Time in all Secukinumab Initiators
Of the 1518 patients who initiated secukinumab at or after enrollment in the registry, the average age at initiation was 50.5 years; 96.7% of patients had insurance coverage, and 45.3% had not been previously exposed to nonbiologic systemic therapies (e.g., methotrexate, cyclosporin, or apremilast) (Table 1). Between April 2015 and December 2020, the proportion of patients initiating secukinumab who were biologic naive increased from 12.5% in 2015 to 49.7% in 2020 (Fig. 2).
Among all secukinumab initiators, 980 (64.6%) were biologic experienced, while 538 (35.4%) were biologic naive (Table 1). In both the biologic-experienced and biologic-naive groups, the time between psoriasis diagnosis and secukinumab initiation decreased over time (Fig. 3A). The total proportion of secukinumab initiators without prior treatment with nonbiologic systemic therapies increased from 30.7% in 2015 to 56.0% in 2020 (Fig. 3B). The proportion of biologic-naive patients with comorbid psoriatic arthritis fluctuated over time. Conversely, the proportion of biologic-experienced patients with comorbid psoriatic arthritis was stable over time, with proportions remaining around 60% (Fig. 3C).
Clinical and treatment characteristics of secukinumab initiators per calendar year in terms of A psoriasis disease duration, B proportion of nonbiologic systemic naive patients, and C proportion of patients with comorbid psoriatic arthritis. aNonbiologic systemic therapies included methotrexate, cyclosporin, and apremilast
Secukinumab Initiators Who Completed a 6-Month or 12-Month Follow-Up Visit
A total of 652 patients maintained secukinumab through 6 months (460 [70.6%] biologic experienced;192 [29.4%] biologic naive), and 390 maintained secukinumab through 12 months (288 [73.8%] biologic experienced; 102 [26.2%] biologic naive) (Supplementary Table S1). Of all patients who initiated secukinumab and had a 6-month follow-up, the mean (SD) age at the baseline visit was 51.3 (14.0) years; about one-half of patients (52.8%) were male. Additionally, the majority of patients who completed a follow-up visit at 6 months were White (79.0%), and 50.2% were obese (body mass index ≥ 30 kg/m2). Similar demographics were seen in patients who continued to receive secukinumab through the 12-month follow-up.
In those who continued secukinumab through a follow-up visit, mean age at psoriasis diagnosis was approximately 33 years for biologic-experienced and 37 years for biologic-naive patients, regardless of follow-up duration (Supplementary Table S1). Additionally, in those who had a 6- or 12-month follow-up visit, approximately 60% who were biologic experienced and 33% who were biologic naive had comorbid psoriatic arthritis; over 20% of biologic-experienced patients had received ≥ 3 prior biologics.
Both biologic-experienced and biologic-naive patients demonstrated improvements in clinical assessment scores of disease activity at 6- or 12-month follow-up visits. The mean (SD) change from baseline in BSA was −11.7 (16.6) and −11.5 (15.0) in biologic-naive patients and −9.3 (14.5) and −9.5 (13.4) in biologic-experienced patients at 6 and 12 months, respectively (Fig. 4A). Patients who maintained continuous secukinumab experienced improvements in IGA scores. Biologic-naive patients demonstrated mean (SD) changes in IGA scores from baseline to 6- and 12-month follow-up visits (−1.7 [1.4] and −1.9 [1.3], respectively). Similar changes were seen in biologic-experienced patients (Fig. 4B). In biologic-naive patients, the mean (SD) decrease from baseline in PASI scores was −6.7 (7.8) at 6 months and −6.9 (7.2) at 12 months (Fig. 4C). Similar mean (SD) changes were observed in biologic-experienced patients.
Improvements in mean (SD) A BSA, B IGA, and C PASI scores from baseline to follow-up in patients with psoriasis who initiated and maintained secukinumaba. BSA body surface area, IGA five-point Investigator’s Global Assessment, PASI Psoriasis Area and Severity Index. aLabels across baseline and follow-up visits represent mean (SD) differences
The proportion of biologic-experienced patients who had IGA scores of 0/1 (clear/almost clear) increased from baseline to the 6-month follow-up visit (9.6–56.5%) or the 12-month follow-up visit (8.7–60.8%) (Fig. 5A). Similar and slightly greater increases from baseline were reported in the proportion of biologic-naive patients who had IGA scores of 0/1 with a 6-month (8.3–66.1%) or 12-month follow-up visit (6.9–72.3%) (Fig. 5B).
Secukinumab Initiators with Both 6- and 12-Month Follow-Up Visits
Of the 326 patients who completed both 6- and 12-month follow-up visits, 244 (74.8%) were biologic experienced, and 82 (25.2%) were biologic naive. The majority of patients with 6- and 12-month follow-up visits were male (58.9%), White (76.4%), and had no history of smoking (56.9%) (Supplementary Table S2). In patients who had both 6- and 12-month follow-up visits and continued secukinumab use through 12 months, mean age at psoriasis diagnosis was 33.1 (16.0) and 38.7 (16.2) years in the biologic-experienced and biologic-naive groups, and 58% and 35% of biologic-experienced and biologic-naive patients had comorbid psoriatic arthritis, respectively.
Both biologic-experienced and biologic-naive patients demonstrated improvements in disease activity measures (BSA, IGA, and PASI scores) from baseline through 6- and 12-month follow-up visits (Supplementary Fig. S1). The proportion of patients who had IGA scores 0/1 (clear/almost clear) increased from baseline (8.6% and 7.4%) to 6-month follow-up (64.8% and 75.3%) and was similar through 12 months of continuous secukinumab treatment (61.1% and 74.1%) in those who were biologic experienced and those who were biologic naive, respectively (Supplementary Fig. S2).
Discussion
This is among the first real-world, US registry-based studies to characterize secukinumab initiators over time and assess clinical outcomes in biologic-naive and biologic-experienced patients during an extended follow-up period. In US patients with psoriasis enrolled in the CorEvitas Psoriasis Registry, the proportion of patients initiating secukinumab who were biologic naive increased over time. Patients who continued secukinumab through follow-up experienced improvements in BSA, IGA, and PASI scores, irrespective of prior biologic use.
The findings in this study demonstrate a trend in prescribing patterns, as evident by the progressive increase in the number of biologic-naive patients who initiated secukinumab over time. This trend may be, in part, attributed to the increased development of additional approved biologics for the treatment of psoriasis. A US-based retrospective study of insurance claims data evaluated longitudinal patterns of psoriasis therapies and found that the annual growth rate for biologic treatment was 10.5% between 2008 and 2012 [26]. Furthermore, an analysis of Medicare Part D public files from 2013 to 2017 reported that biologics made up 86.4% of psoriasis drug costs incurred to Medicare Part D by dermatologists [24]. From its approval for psoriasis in 2015 through 2017, secukinumab was reported to have an average percent increase of 433% per year in the number of prescribing physicians, compared with 5-year averaged changes in older biologics such as adalimumab (13.7%) or etanercept (−5.7%) [24]. Additionally, a 10-year observational study in Spain found a shift in prescription trends from TNFis to IL-inhibitor biologics as the first biologic prescription for patients with psoriasis between 2008 and 2018 [23]. This increase in prescribing may be, in part, attributed to the initial growth associated with the new approval of a biologic. Therefore, further research to assess the prescribing patterns and patient characteristics of initiators may provide better insight into clinical practice behaviors to help identify which type of patient would benefit most from secukinumab as first-line treatment.
Real-world evidence on the effectiveness of continuous treatment with secukinumab in patients with psoriasis was demonstrated in this study. Irrespective of biologic experience, the mean decrease in PASI scores in the population was over 50%, which represents a clinically meaningful change [27]. Additionally, over 66% of patients maintaining secukinumab reported categorical IGA scores of 0/1 (clear/almost clear) at a 6-month follow-up, suggesting that their disease was below mild severity [4]. Throughout this analysis, biologic-naive patients experienced comparable or slightly greater improvements than biologic-experienced patients across all outcomes. These trends are consistent with those seen in several real-world studies in Europe and the USA that assessed the impact of secukinumab in biologic-experienced and biologic-naive patients. A retrospective multicenter study in Italy reported that biologic-naive patients achieved significantly greater mean (SD) improvements in PASI scores at week 48 compared with biologic-experienced patients (1.0 [1.7] versus 1.9 [3.0]; P < 0.05) [28]. Additionally, that study also reported that changes in mean (SD) BSA scores between the two patient cohorts were not statistically different; however, they followed similar trends seen in our analysis after 48 weeks of continuous secukinumab use (1.6 [3.0] versus 2.9 [4.7]; P = 0.16). Furthermore, a retrospective analysis performed in secukinumab initiators across 11 centers in Europe reported that biologic-naive patients achieved lower mean (SD) PASI scores than biologic-experienced patients at week 52 (1.0 [2.2] versus 2.1 [2.3]; P < 0.01) [29]. Similar trends were seen in an analysis of US electronic medical record data: patients achieved and sustained high levels of treatment satisfaction with secukinumab (80–85%) through 24 months [30]. Additionally, biologic-naive patients showed absolute greater improvements from baseline to 24 months compared with biologic-experienced patients (36.6% versus 21.7%, respectively). While the current descriptive analysis presented here did not directly compare clinical outcomes between biologic-experienced and biologic-naive patients, our findings are in line with the outcomes of previous real-world studies. This analysis is one of the first to include a comprehensive assessment of disease activity using BSA, IGA, and PASI scores in a US-based cohort of patients with psoriasis through 12 months of follow-up. The comparable improvements in disease activity measures achieved with secukinumab use in the biologic-naive cohort may impact provider decisions to initiate secukinumab treatment earlier in the patient disease journey.
Of note, fewer patients initiating secukinumab were previously exposed to nonbiologic therapies, such as methotrexate, cyclosporin, or apremilast, over time. These trends suggest that, over time, dermatologists may have been increasingly more likely to prescribe secukinumab as first-line therapy. Conventional systemic treatments have a number of limitations to consider, including a large number of contraindications, poor tolerance, high risk of drug–drug interactions, and substantial safety concerns [6, 31, 32]. In addition, a retrospective cross-sectional study comparing the efficacy of biologic versus conventional systemic therapies reported that patients with psoriasis experience greater clinical benefit, as measured by BSA Physician’s Global Assessment, when prescribed biologics versus conventional systemic therapies (70% improvement versus 40% improvement) [33]. These trends may reflect increased confidence of dermatologists to prescribe biologic treatments earlier in the psoriasis disease journey. Additional analyses that directly compare secukinumab effectiveness in patients with or without prior nonbiologic therapy use are required to determine whether secukinumab is more effective as a first-line therapy.
This study is subject to some limitations. Participation in the CorEvitas Psoriasis Registry by patients and their dermatologists is voluntary; therefore, data from this registry may not be generalizable to all patients with psoriasis or the greater prescribing population. This study was one of the first to describe the characteristics of secukinumab initiators over time and to describe the change in clinical disease activity measures in biologic-naive patients. This analysis did not, however, explore the cause of any initiator trends over time, and no assumptions can be made regarding secukinumab compared with the prescribing patterns of other biologics. Secukinumab was approved in January 2015, and the CorEvitas Psoriasis Registry was launched later that same year, in April, indicating that data for 2015 do not include a full year and should be interpreted with caution. Additionally, beginning in March 2020, the coronavirus disease 2019 (COVID-19) pandemic likely affected how US dermatologists and their patients interacted, which may have impacted subsequent prescribing behavior for psoriasis treatment [34, 35]. Consequently, data from 2015 and 2020 may reflect prescribing patterns that were inconsistent with trends between 2016 and 2019. Factors that impact the prescriber environment, such as drug availability, improved access, or payer limitations on prescriber drugs, may have influenced some trends presented here; however, identifying reasons for the apparent trends was outside the scope of the study.
Conclusion
In this real-world study of US patients with psoriasis, the proportion of secukinumab initiators who were biologic naive increased over time. The observed decrease in the time since the diagnosis of the disease and an increase in the proportion of patients who were nonbiologic systemic naive may reflect dermatologists’ increased confidence in prescribing secukinumab earlier in the psoriasis disease journey. These findings suggest that secukinumab is effective in patients who continue receiving treatment, irrespective of prior exposure to biologics. Both biologic-experienced and biologic-naive patients showed improvements in clinical outcomes after 6 and 12 months of continuous secukinumab use, and these descriptive findings indicate that biologic-naive patients may demonstrate slightly greater improvements than biologic-experienced patients.
References
Rachakonda TD, Schupp CW, Armstrong AW. Psoriasis prevalence among adults in the United States. J Am Acad Dermatol. 2014;70(3):512–6.
Greb JE, Goldminz AM, Elder JT, et al. Psoriasis. Nat Rev Dis Primers. 2016;2:16082.
Feldman SR, Krueger GG. Psoriasis assessment tools in clinical trials. Ann Rheum Dis. 2005;64(Suppl 2):ii65–8 (discussion ii9-73).
Langley RG, Feldman SR, Nyirady J, van de Kerkhof P, Papavassilis C. The 5-point Investigator’s Global Assessment (IGA) scale: a modified tool for evaluating plaque psoriasis severity in clinical trials. J Dermatol Treat. 2015;26(1):23–31.
Armstrong AW, Siegel MP, Bagel J, et al. From the Medical Board of the National Psoriasis Foundation: treatment targets for plaque psoriasis. J Am Acad Dermatol. 2017;76(2):290–8.
Menter A, Gelfand JM, Connor C, et al. Joint American Academy of Dermatology–National Psoriasis Foundation guidelines of care for the management of psoriasis with systemic nonbiologic therapies. J Am Acad Dermatol. 2020;82(6):1445–86.
Menter A, Strober BE, Kaplan DH, et al. Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with biologics. J Am Acad Dermatol. 2019;80(4):1029–72.
Paul C, Cather J, Gooderham M, et al. Efficacy and safety of apremilast, an oral phosphodiesterase 4 inhibitor, in patients with moderate-to-severe plaque psoriasis over 52 weeks: a phase III, randomized controlled trial (ESTEEM 2). Br J Dermatol. 2015;173(6):1387–99.
Mease PJ, Goffe BS, Metz J, VanderStoep A, Finck B, Burge DJ. Etanercept in the treatment of psoriatic arthritis and psoriasis: a randomised trial. Lancet. 2000;356(9227):385–90.
Langley RG, Elewski BE, Lebwohl M, et al. Secukinumab in plaque psoriasis–results of two phase 3 trials. N Engl J Med. 2014;371(4):326–38.
Puig L, Augustin M, Blauvelt A, et al. Effect of secukinumab on quality of life and psoriasis-related symptoms: a comparative analysis versus ustekinumab from the CLEAR 52-week study. J Am Acad Dermatol. 2018;78(4):741–8.
Bagel J, Blauvelt A, Nia J, et al. Secukinumab maintains superiority over ustekinumab in clearing skin and improving quality of life in patients with moderate to severe plaque psoriasis: 52-week results from a double-blind phase 3b trial (CLARITY). J Eur Acad Dermatol Venereol. 2020;35:135–42.
Bagel J, Duffin KC, Moore A, et al. The effect of secukinumab on moderate-to-severe scalp psoriasis: results of a 24-week, randomized, double-blind, placebo-controlled phase 3b study. J Am Acad Dermatol. 2017;77(4):667–74.
Gottlieb A, Sullivan J, van Doorn M, et al. Secukinumab shows significant efficacy in palmoplantar psoriasis: results from GESTURE, a randomized controlled trial. J Am Acad Dermatol. 2017;76(1):70–80.
Gottlieb AB, Kubanov A, van Doorn M, et al. Sustained efficacy of secukinumab in patients with moderate-to-severe palmoplantar psoriasis: 2·5-year results from GESTURE, a randomized, double-blind, placebo-controlled trial. Br J Dermatol. 2020;182(4):889–99.
Reich K, Sullivan J, Arenberger P, et al. Secukinumab shows high and sustained efficacy in nail psoriasis: 2.5-year results from the randomized placebo-controlled TRANSFIGURE study. Br J Dermatol. 2021;184(3):425–36.
Strober BE, Germino R, Guana A, et al. US real-world effectiveness of secukinumab for the treatment of psoriasis: 6-month analysis from the Corrona Psoriasis Registry. J Dermatolog Treat. 2019;31:333–341.
Thaçi D, Körber A, von Kiedrowski R, et al. Secukinumab is effective in treatment of moderate-to-severe plaque psoriasis: real-life effectiveness and safety from the PROSPECT study. J Eur Acad Dermatol Venereol. 2020;34(2):310–8.
Huang H, Cai ML, Hong XJ, et al. Real-world data on the use of secukinumab as treatment for moderate-to-severe psoriasis in Chinese patients. Eur J Dermatol. 2020;30(5):554–60.
Nguyen HT, Pham NTU, Tran TNA, Nguyen NTT, Vu TTP. Secukinumab demonstrated high effectiveness in Vietnamese patients with moderate-to-severe plaque psoriasis in a real-world clinical setting: 16 week results from an observational study. Dermatol Ther (Heidelb). 2021;11:1613–21.
Atella V, Piano Mortari A, Kopinska J, et al. Trends in age-related disease burden and healthcare utilization. Aging Cell. 2019;18(1): e12861.
Muddasani S, Fleischer AB Jr. United States systemic psoriasis treatments: increases in the use of biologic agents and plateau of methotrexate and oral small molecule inhibitors. J Dermatolog Treat. 2020;33:143–5.
Ruiz-Genao DP, Carretero G, Rivera R, et al. Changing trends in drug prescription and causes of treatment discontinuation of first biologic over ten years in psoriasis in the Spanish Biobadaderm Registry. Actas Dermosifiliogr (Engl Ed). 2020;111(9):752–60.
Yang JJ, Pham AT, Maloney NJ, Aly O, Cheng K. Psoriasis drugs in the medicare population: dermatologists' spending and prescription patterns. J Dermatolog Treat. Published online January 20, 2021.
Strober B, Karki C, Mason M, et al. Characterization of disease burden, comorbidities, and treatment use in a large, US-based cohort: results from the Corrona Psoriasis Registry. J Am Acad Dermatol. 2018;78(2):323–32.
Armstrong AW, Koning JW, Rowse S, Tan H, Mamolo C, Kaur M. Under-treatment of patients with moderate to severe psoriasis in the united states: analysis of medication usage with health plan data. Dermatol Ther (Heidelb). 2017;7(1):97–109.
Carlin CS, Feldman SR, Krueger JG, Menter A, Krueger GG. A 50% reduction in the Psoriasis Area and Severity Index (PASI 50) is a clinically significant endpoint in the assessment of psoriasis. J Am Acad Dermatol. 2004;50(6):859–66.
Megna M, Di Costanzo L, Argenziano G, et al. Effectiveness and safety of secukinumab in Italian patients with psoriasis: an 84 week, multicenter, retrospective real-world study. Expert Opin Biol Ther. 2019;19(8):855–61.
Chiricozzi A, Balato A, Conrad C, et al. Secukinumab demonstrates improvements in absolute and relative psoriasis area severity indices in moderate-to-severe plaque psoriasis: results from a European, multicentric, retrospective, real-world study. J Dermatolog Treat. 2020;31(5):476–83.
Armstrong AW, Patil D, Levi E, et al. Real-world satisfaction with secukinumab in clearing the skin of patients with plaque psoriasis through 24 months of follow-up: results from US Dermatology Electronic Medical Records. Dermatol Ther (Heidelb). 2021;11:1733–49.
Nast A, Gisondi P, Ormerod AD, et al. European S3-Guidelines on the systemic treatment of psoriasis vulgaris–Update 2015–Short version–EDF in cooperation with EADV and IPC. J Eur Acad Dermatol Venereol. 2015;29(12):2277–94.
Carretero G, Puig L, Dehesa L, et al. Guidelines on the use of methotrexate in psoriasis. Actas Dermosifiliogr. 2010;101(7):600–13.
Au SC, Madani A, Alhaddad M, Alkofide M, Gottlieb AB. Comparison of the efficacy of biologics versus conventional systemic therapies in the treatment of psoriasis at a comprehensive psoriasis care center. J Drugs Dermatol. 2013;12(8):861–6.
Muddasani S, Housholder A, Fleischer AB. An assessment of United States dermatology practices during the COVID-19 outbreak. J Dermatol Treat. 2020;31(5):436–8.
Bhargava S, McKeever C, Kroumpouzos G. Impact of COVID-19 pandemic on dermatology practices: results of a web-based, global survey. Int J Womens Dermatol. 2021;7(2):217–23.
Acknowledgements
Funding
This study was sponsored by CorEvitas, LLC, Waltham, MA, USA, and the analysis and the journal’s Rapid Service Fee were funded by Novartis Pharmaceuticals Corporation, East Hanover, NJ, USA. Access to study data was limited to CorEvitas, and CorEvitas statisticians completed all of the analysis; all authors contributed to the interpretation of the results. CorEvitas has been supported through contracted subscriptions in the last two years by AbbVie, Amgen, Arena, Boehringer Ingelheim, Bristol Myers Squibb, Celgene, Chugai, Eli Lilly and Company, Genentech, Gilead, GSK, Janssen, LEO, Novartis, Ortho Dermatologics, Pfizer Inc, Regeneron, Sanofi, Sun, and UCB. The CorEvitas Psoriasis Registry was developed in collaboration with the National Psoriasis Foundation.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Bruce Strober, Dhaval Patil, Robert R. McLean, Melissa Moore-Clingenpeel, Eugenia Levi, and Mark Lebwohl conceived and designed the study. Bruce Strober, Melissa Moore-Clingenpeel, Ning Guo, and Mark Lebwohl acquired and analyzed the data. Bruce Strober, Robert R. McLean, Melissa Moore-Clingenpeel, Dhaval Patil, Ning Guo, Eugenia Levi, and Mark Lebwohl verified and interpreted the data. All authors read and approved the final manuscript.
Medical Writing, Editorial, and Other Assistance
Medical writing support was provided by Samantha O’Dwyer, PhD, of Health Interactions, Inc, and was funded by Novartis Pharmaceuticals Corporation. This manuscript was developed in accordance with Good Publication Practice (GPP3) guidelines. Authors had full control of the content and made the final decision on all aspects of this publication.
Disclosures
Bruce Strober is an honoraria consultant for AbbVie, Almirall, Amgen, Arcutis, Arena, Aristea, Asana, Boehringer Ingelheim, Immunic Therapeutics, Bristol Myers Squibb, Connect Biopharma, Dermavant Sciences, EPI Health, Equillium, Evelo Biosciences, Janssen, LEO, Eli Lilly, Maruho, Meiji Seika Pharma, Mindera Health, Novartis, Pfizer, UCB Pharma, Sun Pharma, Regeneron, Sanofi Genzyme, Ventyx Biosciences, vTv Therapeutics; a shareholder of Connect Biopharma, Mindera Health; received speakers fees from AbbVie, Eli Lilly, Janssen, Regeneron, Sanofi Genzyme; served as an investigator for: Dermavant, AbbVie, CorEvitas, LLC (formally Corrona, LLC) Psoriasis Registry, Dermira, Cara, and Novartis; receives consulting fees as a co-scientific director for the CorEvitas Psoriasis Registry; and receives honoraria as the editor-in-chief for the Journal of Psoriasis and Psoriatic Arthritis. Dhaval Patil and Eugenia Levi are employees of Novartis Pharmaceuticals Corporation. Robert R. McLean, Melissa Moore-Clingenpeel, and Ning Guo are employees of CorEvitas, LLC (formerly known as Corrona, LLC). Mark Lebwohl is an employee of Mount Sinai and receives research funds from AbbVie, Amgen, Arcutis, Avotres, Boehringer Ingelheim, Cara Therapeutics, Dermavant Sciences, Eli Lilly, Incyte, Janssen Research & Development, LLC, Ortho Dermatologics, Regeneron, and UCB, Inc., and is a consultant for Aditum Bio, Almirall, AltruBio Inc., AnaptysBio, Arcutis, Inc., Arena Pharmaceuticals, Aristea Therapeutics, Arrive Technologies, Avotres Therapeutics, BiomX, Brickell Biotech, Boehringer-Ingelheim, Bristol Myers Squibb, Cara Therapeutics, Castle Biosciences, CorEvitas, LLC, Dermavant Sciences, Dr. Reddy’s Laboratories, Evelo Biosciences, Evommune, Inc., Facilitation of International Dermatology Education, Forte Biosciences, Foundation for Research and Education in Dermatology, Helsinn Therapeutics, Hexima Ltd., LEO Pharma, Meiji Seika Pharma, Mindera, Pfizer, Seanergy, and Verrica.
Compliance with Ethics Guidelines
All authors meet the International Committee of Medical Journal Editors criteria for authorship for this article, take responsibility for the integrity of the work as a whole, were involved in drafting and critical review of the manuscript, and approved the final version for submission. All authors agree to be accountable for all aspects of the work and attest to the accuracy and integrity of the work. Sponsor approval and continuing review were obtained through a central institutional review board (IntegReview, protocol number is Corrona-PSO-500). All registry patients were required to provide written informed consent prior to participating. Data collection was conducted in accordance with the ethical principles that have their origin in the Declaration of Helsinki and are consistent with the Guidelines for Good Clinical Practice.
Data Availability
Data are available from CorEvitas, LLC through a commercial subscription agreement and are not publicly available. No additional data are available from the authors.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Strober, B., Patil, D., McLean, R.R. et al. Utilization Trends and Impact of Secukinumab Treatment on Clinical Outcomes in Biologic-Naive Patients with Psoriasis in a US Real-World Setting. Dermatol Ther (Heidelb) 12, 1351–1365 (2022). https://doi.org/10.1007/s13555-022-00740-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-022-00740-y