Abstract
Introduction
Sun protection is important in skin care and requires special attention as inefficient protection might trigger skin pathologies including polymorphic light eruption (PLE). The reduce-improve-protect (RIP) concept to avoid the onset of ultraviolet (UV) irradiation-induced diseases or damage to human skin is important. Methoxy-monobenzoylmethane (MeO-MBM), which is neither a UVB nor a UVA filter, converts to the UV filter avobenzone under UV irradiation and further acts as a photoantioxidant during its conversion process and initially as an antioxidant material. The aim of this study was to understand the mechanisms by which MeO-MBM improves the condition of UV-stressed skin through its photoantioxidant properties. The improvement of the skin condition by the activity of MeO-MBM as active ingredient was also investigated.
Methods
Potential molecular targets were identified by in silico docking to numerous cellular membrane receptors on the cell surface or nuclear membrane, followed by microarray analysis of 164 genes after MeO-MBM treatment of normal human epidermal keratinocytes (NHEK). We conducted randomized, double-blinded, intra-individual comparison vs. placebo studies on ten volunteers, aged between 34 and 65 years, to assess the effect of MeO-MBM in vivo. The effect after UV-induced inflammation was assessed in a protective and curative set-up with 2% MeO-MBM vs. 1% hydrocortisone and placebo based on the change in blood flow. The barrier function of the skin was assessed by the change in transepidermal water loss (TEWL), skin scaling and skin thickness after the treatment with MeO-MBM. Additionally, the effect of MeO-MBM after UV-induced stress on the activation of ferritin in human explants was determined ex vivo.
Results
A docking simulation of MeO-MBM showed a potential interaction with the retinoic acid receptor gamma and further revealed downregulation of proteins related to inflammation. In the protective treatment set-up, after 24 h MeO-MBM significantly reduced the delta blood flow compared to placebo, while this reduction was more prominent with hydrocortisone. In the curative treatment set-up, a greater reduction in delta blood flow was also observed with MeO-MBM compared to placebo and similar to hydrocortisone. Treatment with MeO-MBM revealed an improvement in skin barrier function as a result of decreased TEWL, reduced skin scaling and increased skin thickness. Immunohistochemistry staining of ferritin on human skin explants further showed that the treatment with MeO-MBM reduced the ferritin expression.
Conclusion
Based on these results, MeO-MBM is capable of exerting an anti-aging activity via the retinoic acid receptor gamma. Its anti-inflammatory and anti-oxidative activity manifested via the downregulation of multiple anti-inflammatory genes as well as the reduction of ferritin in skin tissue. This study shows that the multidimensional functionality of MeO-MBM offers an effective approach to combat acute and chronic deleterious effects of oxidative UV damage while simultaneously enhancing the skin barrier function.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Sun protection requires special attention as inefficient protection might trigger acute and chronic deleterious effects of oxidative UV damages |
The active ingredient Methoxy-monobenzoylmethane (MeO-MBM), which is not a UV filter but converts under UV irradiation to the UV filter avobenzone, functions initially as an antioxidant material and as a photoantioxidant during its conversion process while combating cellular stress in parallel |
To understand the mechanisms of how MeO-MBM may improve the skin condition of UV-stressed skin, we conducted randomized, double-blinded studies after identifying potential molecular targets and generating a gene expression profile. In addition, we determined the effect of MeO-MBM after UV-induced stress on the activation of ferritin |
What was learned from this study? |
MeO-MBM caused downregulation of proteins related to inflammation, a preventive and curative beneficial effect on UV-irradiated skin, skin barrier improvement as preventive treatment and reduced ferritin expression |
The positive modulation of multiple signaling pathways makes MeO-MBM a suitable active ingredient with additional biological functionalities associated with anti-aging and inflammation |
Introduction
Sun protection is an important aspect of skin care. As sun protection is directly linked with disease prevention induced by the energy of ultraviolet (UV) light and indirectly by the formation of reactive species, be it oxygen or nitrogen, it is important to assure the functionality of the used active UV filters [1, 2]. Given that UV filters require regulatory approval by the Food and Drug Administration (FDA), it is desirable to add sun filter boosting materials or conversion materials to maintain the sun protection factor (SPF) in case of UV-induced degradation of the key sun filter material in sun care formulations [3]. Methoxy-monobenzoylmethane (MeO-MBM) belongs to the second class of materials as it has been shown that it converts into 4-tert-butyl-4′-methoxydibenzoylmethane (avobenzone) in vitro and in vivo after having been exposed to UV irradiation [4].
Avobenzone is a widely used organic UV-A filter and is known for its irreversible UV-driven photodegradation due to a non-adiabatic population of high S0 vibrational levels during photoexcitation leading to a less photostable form by isomerization with subsequent photodegradation into the radicals 4-methoxybenzaldehyde and 1-(4-tert-butylphenyl) ethenone by the Norrish type 1 mechanism [5,6,7,8]. This photodegradation is known to have several disadvantages ranging from skin irritation, photodermatosis, age-related extrinsic aging or phototoxicity, photoirritation and photoallergic reactions resulting from exposure to photodegradation by-products. In addition, unstable sun care formulations lead to an increased risk of sun burn, chronic skin damage and inflammaging as well as skin cancer [9].
The conversion of MeO-MBM results in the formation of two intermediate hydrogen radicals, which can directly neutralize radicals formed during the degradation of avobenzone or further react with radical species present in UV-exposed human skin protecting the skin against UV stress. This is referred to as photoantioxidative functionality [4].
However, further insights are needed to understand the mechanisms related to how MeO-MBM improves the skin condition of UV-stressed skin through its photoantioxidant properties and whether MeO-MBM may additionally improve the skin condition as a non-converted material making it a suitable active ingredient with additional biological functionalities. In this work, we have identified the retinoic acid receptor as potential molecular target of MeO-MBM by in silico docking studies. To further identify mechanisms and pathways where MeO-MBM might play a role as an active ingredient, human epidermal keratinocyte (NHEK) cells were treated with active and comparative treatment with retinoic acid, and gene expression profiling was conducted to generate a hypothesis for further ex vivo and in vivo testing. Here, we show that MeO-MBM had a preventive and curative beneficial effect on UV-irradiated skin and secondly that MeO-MBM improved the skin barrier as preventive treatment. These data indicate that MeO-MBM reduces inflammation, improves the skin barrier and protects the skin from UV-induced cellular damage. To summarize based on these findings, MeO-MBM is a potent active ingredient especially in sun care formulations.
Methods
Test Substance
MeO-MBM-3-(4-tert-butylphenyl)-3-hydroxy-1-(4-methoxyphenyl) propan-1-one (CAS No. 955359-34-9) was synthesized at Merck KGaA, Darmstadt, Germany, and used for the outlined assays and in vivo studies (Fig. 1). The material was developed intentionally as conversion material that is converted to avobenzone by UV irradiation to act as an approved UV-A sunfilter and was toxicologically assessed and considered to be safe for in vivo use in humans.
Microarray Analysis of 164 Genes After MeO-MBM Treatment of Primary Keratinocytes
Normal human epidermal keratinocytes were used in passage 3 cultivated in Keratinocyte-SFM (Thermo Fisher Scientific Inc., Waltham, MA, USA) supplemented with 0.25 ng/ml epidermal growth factor (EGF), 25 µg/ml pituitary extract (Thermo Fisher Scientific Inc., Waltham, USA) and 25 µg/ml gentamycin (Sigma-Aldrich, St. Louis, MO, USA) at 37 °C and 5% CO2. The assay was conducted in Keratinocyte-SFM supplemented with 25 µg/ml gentamycin. The working concentration with no cytotoxicity observed was determined in 96-well plates seeding 104 NHEK in Keratinocyte-SFM evaluated by MTT reduction assay (Sigma-Aldrich, St. Louis, MO, USA) and morphological observation by microscopy at 100 × magnification.
The cells were treated with MeO-MBM at 1 µg/ml dissolved as stock solution at 25 µg/ml in DMSO and retinoic acid (Sigma-Aldrich) at a working concentration as reference at 10–6 M. The NHEKs were cultivated in 12-well plates in culture media for 24 h. After incubation, the medium was removed and replaced by assay media, and the cells were further incubated at 37 °C and 5% CO2. At subconfluence the cells were treated with MeO-MBM as well as treatment control and positive control (retinoic acid) for 96 h at 37 °C and 5% CO2. Finally, the cells were washed in PBS (Thermo Fisher Scientific Inc.); 300 µL TriReagent (Thermo Fisher Scientific Inc., Waltham, MA, USA) was added, and the cells were immediately frozen at − 80 °C. All conditions were performed (n = 3). The isolated mRNA was direct reverse transcribed using mRNA in the presence of [α-33P]-dATP and oligo d(T) primer. The labeled cDNA samples were hybridized to a microarray covalently coupled to 164 genes of interest in duplicate (+ controls and housekeeping genes) in the context of human skin. After extensive washing, the relative amount of a specific hybridized target was analyzed by PhosphorImaging. The analysis was performed by direct quantification using “Cyclone” PhophorImager (Packard Instruments, Meriden, CT, USA) and ImageQuantTL (Amersham Biosciences, Amersham, UK).
UV-Induced Inflammation In Vivo
A randomized, double-blinded, intra-individual comparison vs. placebo study was conducted including positive control on ten volunteers, aged between 34 and 65 (average 51.9) years with slightly dry skin. Inclusion criteria were healthy skin, normal nutritional habits and a body mass index (BMI) of 18–25 kg/m2. Exclusion criteria were pregnancy, breast-feeding, smoking, medications which affect the skin response such as antibiotics, anti-inflammatory medications and extensive sun exposure.
MeO-MBM (2% w/w) was incorporated into an oil-in-water formulation (O/W), while the same O/W without active treatment served as placebo and 1% hydrocortisone cream as positive control. A solar simulator (Multiport® 300 W, Solar Light, Glenside, PA, USA) was used as a light source. The excitation spectrum of the light source complied with the international SPF test method (COLIPA spectra). UV-induced inflammation was assessed based on the change in blood flow.
For protective MeO-MBM treatment, the test subjects applied 2 mg/cm2 of the samples twice a day on predetermined skin areas on the inner forearm over a period of 1 week. Afterwards, the test areas were irradiated with 1.25 minimal erythema dose (MED), and the test products were applied immediately afterwards on the irradiated areas. After 6 h, 24 h and 48 h, the blood flow was measured using a laser Doppler flowmeter (LEA Instruments, Giessen, Germany) oxygen-to-see device, followed by further applications of the test samples. The change in blood flow expressed by area units (AU) before irradiation to three time intervals after irradiation is given as ∆ blood flow values.
For curative MeO-MBM treatment, the test areas were irradiated with 1.25 MED-fold UVB MED. The test subjects applied 2 mg/cm2 of the samples immediately afterwards on the irradiated areas. After 6 h, 24 h and 48 h, the blood flow was measured using a laser Doppler flowmeter oxygen-to-see device, followed by further applications of the test samples. The change in blood flow as expressed by AU before irradiation at three time intervals after irradiation is given as ∆ blood flow values.
Skin Barrier Function Testing In Vivo
A randomized, double-blind, intra-individual comparison vs. placebo study was conducted on ten volunteers, aged between 34 and 65 (average 51.9) years, with slightly dry skin. The products were applied twice a day on predetermined different skin areas on the inner forearm. The effectiveness of the products was evaluated at baseline, after 2 weeks as a midpoint evaluation and after 4 weeks. One test area remained untreated, which was used as a negative control. MeO-MBM (2% w/w) was incorporated into an O/W formulation, while the same O/W without active treatment served as placebo.
Skin barrier function was assessed on the basis of the change in transepidermal water loss (TEWL), skin scaling (SESC) and skin thickness.
TEWL was measured using a Tewameter® TM 300 (Courage & Khazaka, Cologne, Germany). Skin scaling was evaluated utilizing Visioscan® VC98 UVA light video camera (Courage & Khazaka, Cologne, Germany). The device consists of a measuring head containing two special metal-halogenide lights, arranged on opposite sides, that illuminate the 15 × 17-mm measuring area of the skin uniformly. The spectra of the lamps, their intensity and their location were chosen so that only the skin surface, without reflections of deeper layers, is monitored. Using the additional Surface Evaluation of Living Skin software, the skin-specific parameter skin scaling was then calculated. Skin thickness was analyzed with an ultrasound device with 20-MHz frequency (Derma Scan C, version 3) with 2D configuration (Cortex Technology, Hadsund, Denmark).
Ferritin Explant Immunohistochemistry (IHC) Staining After MeO-MBM Treatment
From an abdoplasty from a 51-year-old Caucasian woman, 21 skin explants of 11 mm (± 1 mm) average diameter were prepared. The explants were kept in culture medium at 37 °C and 5% CO2 atmosphere. MeO-MBM (2% w/w) was applied topically at 2 mg/cm2 and spread using a spatula on day 0, day 1, day 2 and day 5. Half of the culture medium (1 ml) was renewed on day 1, day 2 and day 5. On day 5, the culture media of all the batches were replaced by 1 ml Hank’s balanced saline solution (HBBS, Sigma-Aldrich, St. Louis, MO, USA). The skin explants were irradiated using a RMX 3-W UV simulator (Vilber Lourmat, Marne La Vallée, France) using 4.5 J/cm2 UVA equivalent to 1 MED. After additional 24 h in culture, the explants were fixed for 24 h in buffered formalin, and the samples were dehydrated and impregnated in paraffin using a Leica TP 1010 dehydration automat (Leica Biosystems, Wetzlar, Germany). The samples were embedded using a Leica EG 1160 embedding station (Leica Biosystems, Wetzlar, Germany). Sections of 5 µm were sliced using a Leica RM 2125 Minot microtome (Leica Biosystems, Wetzlar, Germany), and the sections were mounted on Superfrost® histological glass slides. The microscopical observations were conducted using a Leica DMLB or Olympus BX43 microscope (Leica Biosystems, Wetzlar, Germany). Pictures were digitized with a numeric DP72 camera with CellD software (Olympus, Tokyo, Japan). The immunostaining of ferritin was performed on paraffin formol sections with a polyclonal rabbit anti-ferritin antibody (Sigma-Aldrich), diluted at 1/50, for 2 h at room temperature. The staining was enhanced with a streptavidin/peroxidase system and revealed using VIP vector (SA 1001, Thermo Fisher Scientific Inc.). The immunostaining was performed using an AutostainerPlus automated horizontal slide-processing system (Dako, Carpinteria, CA, USA) and assessed by microscopic observation.
Compliance with Ethics Guidelines
This study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Toxicological and Regulatory Affairs Review Board of Merck KGaA, Darmstadt, Germany. All participants were informed of the aims and methods of the study and gave their written consent.
Results
The active ingredient MeO-MBM was developed as a conversion material that undergoes a transformation to avobenzone after UV irradiation. Besides the benefits in maintaining the UV protection in formulations, the following experiments focus on the biological properties and the linked endpoints in vivo after MeO-MBM treatment. In a first step, the molecular structure of MeO-MBM was evaluated, and potential molecular targets were identified by in silico docking to numerous cellular membrane receptors on the cell surface or nuclear membrane including nuclear retinoic acid receptor gamma (RAR-γ, Fig. 2).
MeO-MBM molecular structure and docking to retinoic acid receptor gamma. Molecular structure of MeO-MBM (A) and molecular docking of MeO-MBM to the retinoic acid receptor (RAR-γ). B (S)-MeO-MBM in retinoic acid receptor gamma (PDB Structure 2LBD). Software used Glide from Schrödinger, docking with default settings in SP mode. (S)-MeO-MBM structure in green. C Two pi-stacking interactions with phenylalanine 304 and 288 predicted (D)
A docking simulation of MeO-MBM to retinoic acid receptor gamma (RAR-γ) revealed a potential interaction with phenylalanine 304 and 288 (Fig. 2).
Motivated by this finding, we generated a gene expression profile by comparing retinoic acid as natural RAR-g ligand vs. MeO-MBM treatment of NHEK (Fig. 3) and normalized to untreated and solvent control treated NHEK (data not shown).
Gene expression profiling after retinoic acid or MeO-MBM treatment: microarray analysis of [α-33P]-labeled cDNA with 164 covalently linked skin relevant genes. NHEKs were treated for 96 h with A: 1 µM retinoic acid; B: 3.2 µM MeO-MBM. Examples of genes downregulated compared to retinoic acid treatment (green) and examples of genes upregulated after MeO-MBM treatment (red). All data are normalized vs. untreated control using housekeeping genes in similar abundance. C Gene list and localization of analyzed molecular target RNA
Exemplarily, upon MeO-MBM treatment, the expression of genes encoding matrix metalloproteinase 9 (MMP9), which is involved in the breakdown of extracellular matrix and the regulation and degradation of type IV collagen, was downregulated (Fig. 2) [10, 11]. Also the pro-inflammatory cytokine interleukin 1 beta (IL1B) expression was significantly downregulated, which may be related to MeO-MBM anti-inflammatory activity. In addition, superoxide dismutase 2 (SOD2), a mitochondrial activated stress gene, was found to be less expressed, and zinc-alpha-2-glycoprotein (AZGP1), a protein that is known to be activated by stress-induced cells while its expression is downregulated in atopic dermatitis, was upregulated. In addition, serpine 1, a protein active during wound healing, is reduced as is PLAU, a protein activated by IL8 [12,13,14,15]. MeO-MBM significantly upregulated the expression of the fatty acid binding protein 5 (FABP5), which encodes a transporter of intracellular fatty acids in the human epidermis and contributes to the water barrier function in normal skin. Also loricrin (LOR), a major protein of the cornified envelope in terminally differentiated epidermal cells, was upregulated at the mRNA level [16,17,18,19]. Further upregulated proteins involved in the skin barrier maintenance are Calmodulin Like 5 (CALML5), involved in epidermal differentiation, and Corneodesmosin (CDSN), building corneodesmosomes, thus improving the skin barrier [20, 21]. Cystatin-A (CSTA), a cystine protease inhibitor known to reduce the degradation of skin-related structure proteins and thus contributing to reduced signs of irradiation-induced degradation of elastic and collagen fibers, is upregulated [22, 23]. Moreover, Krueppel-like factor 4 (KLF4), a transcription factor known to be involved in skin renewal processes [24], is upregulated. A further indication that MeO-MBM improves the skin barrier by strengthening the cornification process is the increased expression of the small proline-rich proteins (SPPR1A, 1B and 2B), which are strongly induced during differentiation of human epidermal keratinocytes [25,26,27]. The SPRR protein family constitutes a class of cornified precursor proteins. To improve the skin barrier, constant cell renewal is required, and also here S100A8, a member of the A100 family proteins, was shown to be involved in the regulation of cell cycle progression and differentiation in the keratinization process upon MeO-MBM treatment [28, 29]. Other genes involved in MeO-MBM dependent up- or downregulation, mainly related to cornification and cell barrier improvement, were identified but are not further described in detail here.
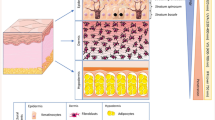
The above gained gene expression data provide evidence that the MeO-MBM treatment after UV-A stress evokes anti-inflammatory properties on skin and improves the skin barrier and the cornification process. We observed that MeO-MBM shows an inverse effect compared to retinoic acid acid, which exhibited an anti-differentiating effect, whereas MeO-MBM modulates relative expressions associated with pro-differentiating effects, e.g., through the expression of KI67 for proliferation and proteins supporting differentiation such as the above-mentioned SPRP1A, 1B, 2B and LOR [30]. Besides the potential functionalities of MeO-MBM in anti-inflammation and skin barrier improvement, the question arose whether MeO-MBM, upon conversion by UV irradiation into avobenzone, displays radical scavenging properties and might reduce signs of cellular reactive oxygen species (ROS)-induced stress. It is important to note that in preventive treatment cells are supported in the basic functions of energy production, associated with mitochondrial health and cellular self-renewal and detoxification as cellular readouts. If MeO-MBM improves the overall health status of various cell types in skin, the assumption was that with beneficial properties of an active ingredient after UV irradiation, the development of inflammatory reactions and the build-up of edema were decreased by reducing the blood flow in living skin, as healthy skin has optimal nutrient and oxygen supply to support the vital functions of the different cell types in skin more quickly and counteracts the stress more efficient [31,32,33]. Therefore, we conducted an in vivo study to determine the effect of MeO-MBM on the microcirculation of blood compared to hydrocortisone, a well-described anti-inflammatory drug, to reduce signs of UV-induced skin irritation.
As shown in Fig. 4, the protective treatment of skin with MeO-MBM at 2% reduced the delta blood flow by 24.6% compared to the placebo after 6 h and by 38.2% after 24 h, whereas all delta blood flow values were reduced again at 48 h after the irradiation, where the preventive treatment with 2% MeO-MBM reduced the delta blood flow by 39.5% compared to the placebo. At all three tested time points, the treatment with 1% hydrocortisone showed the strongest reduction in the delta blood flow with 54.5% after 6 h, 66.3% after 24 h and 67.5% after 48 h, respectively.
Protective effect of MeO-MBM on the delta micro-blood flow. Difference in blood flow at 6 h, 24 h and 48 h after 1.25 MED UV irradiation compared to baseline before irradiation. Data points represent the mean value ± standard deviations of ten test subjects (n = 10). Statistically different values were calculated using two-sided Wilcoxon rank sum test: *p < 0.05
After evaluating the protective effect of MeO-MBM in vivo, the next point that required scientific evaluation was the testing of this compound at similar conditions in a curative in vivo approach. In the curative approach, no pre-treatment with active ingredients was done, and the formulation was applied only after UV irradiation with 1.25 MED. Subsequently, how quickly the skin could recover was determined.
As shown in Fig. 5, the curative treatment with MeO-MBM at 2% reduced the delta blood flow by 41.7% compared to the placebo after 6 h and by 25.8% after 24 h, whereas all delta blood flow values were reduced again at 48 h after the irradiation; also here the curative treatment with 2% MeO-MBM reduced the delta blood flow by 27.6% compared to the placebo. The three tested time points for the treatment with 1% hydrocortisone showed a reduction in the delta blood flow of 39.1% after 6 h, 13.8% after 24 h and 13.5% after 48 h. In the curative in vivo set-up, 2% MeO-MBM treatment was superior to all hydrocortisone treatment time points using 1% of the approved drug substance.
Curative effect of MeO-MBM treatment on the delta micro-blood flow. Difference in blood flow at 6 h, 24 h and 48 h after 1.25 MED UV irradiation compared to baseline before irradiation. Data points represent the mean value ± standard deviations of ten test subjects (n = 10). Statistically different values were calculated using two-sided Wilcoxon rank sum test: *p < 0.05
After the evaluation of the delta blood flow improvements as indicator of faster recovery from UV-induced erythema in healthy skin, the next point for testing aimed to understand the effect of using the measurement of the TEWL as a marker for skin barrier integrity on the skin barrier.
As shown in Fig. 6, the TEWL decreased by 3% after 2 weeks, but this did not reach statistical significance (p = 0.61). However, the TEWL was significantly decreased by 10% (p = 0.04) after 4 weeks of product application vs. the starting value at time point zero on the respective skin area treated. In the untreated control, the TEWL increased by 7% after 2 weeks. Also, a 2% increase of the TEWL after 4 weeks compared to baseline at t0 was observed. This did not reach statistical significance after either 2 weeks with a p value of 0.20 or 4 weeks with a p value of 0.47. Thus, these data indicate a significant improvement of the skin barrier after 4 weeks of MeO-MBM application.
Beside the determination of physiological parameters such as TEWL in vivo, the question of whether the improvement of the skin barrier is visible on a morphological level arose. Therefore, we tested whether 2% MeO-MBM reduces the scaling of human skin as a sign of smoother skin with an improved skin barrier with fewer dry cornified plaques in the process of desquamation.
As shown in Fig. 7, the treatment with 2% MeO-MBM after 2 weeks reduced skin scaling by − 32% and after 4 weeks by − 25% after application twice daily compared to baseline at the same skin area at t0. A decrease, albeit considerably smaller, was observed in the untreated control after 2 weeks by − 8% and 4 weeks by − 2%, respectively. A decrease of skin scaling was observed when applying MeO-MBM, but this was not statistically significant after 2 weeks with a p value of 0.10 and after 4 weeks with a p value of 0.28. Also for the untreated control no significance was reached after 2 weeks with a p value of 0.70 and after 4 weeks with a p value of 0.93. Thus, these data indicate a trend of improving skin scaling and need to be further evaluated. Another in vivo measurement to monitor potential skin barrier improvement is the skin thickness, as thicker epidermis and dermis layers are more efficient in retaining water and when interacting prevent the invasion of allergens, microbes and other skin-irritating factors such as chemicals. Thus, MeO-MBM was tested next to determine the effect on skin thickness in vivo.
As shown in Fig. 8, the skin thickness was not improved by the treatment with 2% MeO-MBM after 2 weeks with a delta skin thickness of 0% and a p value of 0.71, but after 4 weeks a slight improvement by + 4% with a p value of 0.42 compared to baseline at t0 was detectable. Interestingly, a decrease in skin thickness was observed in the untreated control and treated volunteer group after 2 weeks by − 6% and after 4 weeks by − 3%. The data for MeO-MBM indicate a trend of improving the skin thickness after 4 weeks of product application using 2% MeO-MBM in vivo.
Considering MeO-MBM's efficacy in vivo in improving the skin barrier function and downregulation of proteins in the context of inflammation, the question arose whether MeO-MBM is a classical antioxidative molecule or whether the functionality is attributed to reduction of ROS and reactive nitrogen species (RNS) by downregulation of enzymes keeping the reactive species machinery active, e.g., superoxide dismutase 1 and 2 (SOD 1 and 2), which are known to modulate the free iron content in living cells upon cellular stress. Free iron is toxic to mammalian cells and typically binds to ferritin to avoid ferroptosis—a subform of apoptosis [34, 35]. Therefore, a final experiment was conducted to determine the effect of MeO-MBM after UV-induced stress on the activation of ferritin in ex-vivo human explants.
As shown in the immunohistochemical staining of ferritin (Fig. 9) on human skin explants, the placebo-treated skin expressed a moderate amount of ferritin mainly located close to the basal lamina visible as a brownish precipitate (A). In the MeO-MBM-treated representative skin biopsy, only a faint ferritin stain was detectable. Based on these data, the treatment using 2% MeO-MBM was able to reduce the activation of ferritin after UV irradiation in stressed human explants and protected skin from UV-induced reactions as a result of radical formation induced upregulation of ferritin.
Ferritin reduction after MeO-MBM treatment. Human living skin explants were treated with placebo (A) and MeO-MBM (B) topically at 2 mg/cm2. The UV irradiation was exposed to the explants on day 5 with 4.5 J/cm2 of UVA (1 MED). The IHC staining was conducted on day 6. The cell culture media were changed on D1, D2 and D5. The scale bar indicates 50 µm
The results that MeO-MBM reduced the ferritin expression ex vivo confirm that the antioxidant enzyme activity is a key factor in controlling intracellular iron levels, and hence maintenance of cell antioxidant capacity is vitally important in prevention of skin aging and inflammation initiated by labile iron and UVA-irradiated skin [36, 37].
Discussion
The novel active ingredient MeO-MBM bundles activities that in sum are described as the reduce-improve-protect (RIP) concept ideally used as preventive treatment to protect against sun irradiation-induced DNA damage and cellular stress. In addition, the UV-triggered signs of inflammation such as the delta micro-blood flow are reduced like in the well-described approved drug hydrocortisone (Figs. 4, 5). To protect skin and reduce the signs of inflammation, improving and strengthening the skin barrier are beneficial and work in concert as effective UV-related anti-aging ingredients. Interestingly, MeO-MBM acts as a conversion material and thus reduces UV irradiation-induced physical damage, but when exposed to living cell layers of skin, it is a potent ingredient to modulate signal transduction and reduces ROS and RNS generation [4]. Typically for a conversion material the release of hydrogen and the following reaction with UV-induced radicals come first to mind as the key functionality of MeO-MBM as it releases two hydrogens via the conversion to avobenzone. However, this study clearly shows that MeO-MBM also has a direct effect on the improvement of the skin barrier and the reduction of inflammation induced by UV irradiation. As shown in the gene expression profiling, IL1 beta is downregulated (Fig. 3) in primary cell culture, and in vivo the delta micro-blood flow is reduced as a further sign of reducing inflammatory signs attributed to UV irradiation (Figs. 4, 5). Reduction in inflammation is important for cells to recover from stress and to keep the metabolism and pathways that are required for continuous nutrient and energy supply and cellular maintenance and repair mechanisms activated. Classical antioxidative materials are used to support cells to neutralize radicals before damaging the cells or macromolecules associated with loss of function such as lipid peroxidation. MeO-MBM exhibits dose-dependent antioxidative properties with and without irradiation which are in contrast to avobenzone, where no DPPH reduction was measured [4].
Here it is shown that the characteristics of MeO-MBM, in addition to the conventional antioxidative properties, are linked via the downregulation of SOD 1 and 2 (Fig. 3). This key step in reducing the release of free iron from cells under stress induces the expression of ferritin, a globular protein complex of about 450 kDa consisting of 24 protein subunits, which is the primary intracellular iron store in eukaryotes because free iron is toxic to cells by acting as a catalyst in the formation of free radicals from ROS via the Fenton reaction.
Ferritin binds to free ferrous iron and stores it in its non-toxic form, the ferric state. In the skin, ferritin is ubiquitously expressed in basal keratinocytes as a constitutive protective response in low concentrations and its expression is induced upon UVA exposure.
UVA irradiation of human dermal fibroblasts and endothelial cells induces an immediate transient increase in cytosolic Fe(II) and a decrease in superoxide dismutase (SOD) and shortens the cytosolic Fe(II) signal after UVA irradiation. Hence, control of cytosolic ferritin iron release is key to preventing UVA-induced inflammation. Given that MeO-MBM converts into avobenzone upon UV irradiation and thus contributes to UV protection in addition to the skin care properties shown in this study, it appears to be most sensible to apply formulations containing MeO-MBM before UV irradiation appears. In this way, the multifunctional properties of MeO-MBM can be optimally utilized and their full potential exploited.
In summary, MeO-MBM is a potent molecule in sun care formulations capable of maintaining the SPF by converting to avobenzone and releasing two hydrogen radicals that reduce the overall production of reactive radical species, thus improving the health status of cells and skin [4]. By that reduced radical formation, the onset of inflammatory reactions which accelerate the chronic age-related inflammation processes called inflammaging is decreased. In this work, we could show that the abundance of ferritin is lowered, and this reduces the likelihood of initiating ferroptosis, which is a highly regulated ROS-dependent type of cell death resulting from free iron overload (FIO), ROS generation, lipid peroxidation and ultimately membrane damage.
Typically, FIO and lipid peroxidation are biochemical hallmarks of ferroptosis [38]. FIO develops as a consequence of disturbed iron metabolism and accumulation of intracellular or extracellular iron. Mechanistically, FIO may provoke intense ROS production through the Fenton reaction in organelles, which culminates in DNA oxidative injury, lipid peroxidation and membrane damage [38,39,40]. These aspects are associated with molecular damage accelerating senescence in human skin and potentially disrupting the circadian rhythm by clockophagy, a selective type of autophagy that sequesters and degrades the cardinal circadian clock protein ARNTL [37, 41, 42]. The data show that MeO-MBM is effective against acute and chronic adverse effects of oxidative UV damage and needs to be further elucidated under clinical conditions.
Conclusion
Based on these results, MeO-MBM is capable of exerting an anti-aging activity via the retinoic acid receptor gamma. Its anti-inflammatory and anti-oxidative activity manifest via the downregulation of multiple anti-inflammatory genes as well as the reduction of ferritin in skin tissue. From this study, it can be concluded that the multidimensional functionality of MeO-MBM offers an effective approach against acute and chronic deleterious effects of oxidative UV damage while simultaneously enhancing the skin barrier function. The combined effects of MeO-MBM are promising as a future skin care treatment for sensitive skin especially under UV exposure and thus might be of value in sun care formulations. MeO-MBM further positively modulates several signaling pathways associated with anti-aging and inflammatory trends in skin care, such as circadian rhythm, senescence and autophagy, which need to be further elucidated to reveal additional benefits of MeO-MBM.
References
Gonzaga ER. Role of UV light in photodamage, skin aging, and skin cancer. AM J Clin Dermatol. 2009;10(1):19–24.
D’Orazio J, Jarrett S, Amaro-Ortiz A, Scott T. UV radiation and the skin. Int J Mol Sci. 2013;14(6):12222–48.
Ziosi P, Manfredini S, Brazzo F, Vaccarelli C, Vertuani S, Reggio S, Bustacchini S. SPF BOOSTER Nuovo approccio nello sviluppo di Prodotti Solari. Valutazione di efficacia in vitro ed in vivo. Cosmet Technol. 2006;9:11–5.
Termer M, Carola C, Salazar A, Keck CM, von Hagen J. Methoxy-monobenzoylmethane protects human skin against UV-induced damage by conversion to avobenzone and radical scavenging. Molecules. 2021;26:6141.
Berenbeim JA, Wong NGK, Cockett MCR, Berden G, Oomens J, Rijs AM, Dessent CEH. Unravelling the Keto-Enol tautomer dependent photochemistry and degradation pathways of the protonated UVA filter avobenzone. J Phys Chem A. 2020;124(15):2919–30.
Schwack W, Rudolph T. Photochemistry of dibenzoyl methane UVA filters part 1. J Photochem Photobiol B. 1995;28:229–34.
Roscher NM, Lindemann MKO, Bin Kong S, Cho CG, Jiang P. Photodecomposition of several compounds commonly used as sunscreen agents. J Photochem Photobiol A. 1994;80:417–21.
Afonso S, Horita K, Sousa e Silva JP, Almeida IF, Amaral MH, Lobão PA, Costa PC, Miranda MS, da Silva JCE, Lobo JMS. Photodegradation of avobenzone: stabilization effect of antioxidants. J Photochem Photobiol B. 2014;140:36–40.
Nash JF, Tanner PR. Relevance of UV filter/sunscreen product photostability to human safety. Photodermatol Photoimmunol Photomed. 2014;30(2–3):88–95.
Cawston TE, Young DA. Proteinases involved in matrix turnover during cartilage and bone breakdown. Cell Tissue Res. 2009;339(1):221.
Lu P, Takai K, Weaver VM, Werb Z. Extracellular matrix degradation and remodeling in development and disease. Cold Spring Harb Perspect Biol. 2011;3(12):a005058.
Luk E, Yang M, Jensen LT, Bourbonnais Y, Culotta VC. Manganese activation of superoxide dismutase 2 in the mitochondria of Saccharomyces cerevisiae*. J Biol Chem. 2005;280(24):22715–20.
Noh JY, Shin JU, Kim JH, Kim SH, Kim B-M, Kim YH, et al. ZAG regulates the skin barrier and immunity in atopic dermatitis. J Investig Dermatol. 2019;139(8):1648–57.
Sun H, Mi X, Gao N, Yan C, Yu F-S. Hyperglycemia-suppressed expression of serpine1 contributes to delayed epithelial wound healing in diabetic mouse corneas. Investig Ophthalmol Vis Sci. 2015;56(5):3383–92.
Han Y-P, Hughes MW, Nien Y-D, Garner WL. IL-8-stimulated expression of urokinase-type plasminogen activator in human skin and human epidermal cells. J Surg Res. 2002;106(2):328–34.
Chmurzyńska A. The multigene family of fatty acid-binding proteins (FABPs): function, structure and polymorphism. J Appl Genet. 2006;47(1):39–48.
Furuhashi M, Hotamisligil GS. Fatty acid-binding proteins: role in metabolic diseases and potential as drug targets. Nat Rev Drug Discov. 2008;7(6):489–503.
Kalinin A, Marekov LN, Steinert PM. Assembly of the epidermal cornified cell envelope. J Cell Sci. 2001;114(17):3069–70.
Candi E, Schmidt R, Melino G. The cornified envelope: a model of cell death in the skin. Nat Rev Mol Cell Biol. 2005;6(4):328–40.
Lessard JC, Kalinin A, Bible PW, Morasso MI. Calmodulin 4 is dispensable for epidermal barrier formation and wound healing in mice. Exp Dermatol. 2015;24(1):55–7.
Oji V, Eckl K-M, Aufenvenne K, Nätebus M, Tarinski T, Ackermann K, et al. Loss of corneodesmosin leads to severe skin barrier defect, pruritus, and atopy: unraveling the peeling skin disease. Am J Hum Genet. 2010;87(2):274–81.
Barrett AJ. The cystatins: a new class of peptidase inhibitors. Trends Biochem Sci. 1987;12:193–6.
Takahashi M, Tezuka T, Katunuma N. Phosphorylated cystatin α is a natural substrate of epidermal transglutaminase for formation of skin cornified envelope. FEBS Lett. 1992;308(1):79–82.
Segre JA, Bauer C, Fuchs E. Klf4 is a transcription factor required for establishing the barrier function of the skin. Nat Genet. 1999;22(4):356–60.
Steinert PM, Candi E, Kartasova T, Marekov L. Small proline-rich proteins are cross-bridging proteins in the cornified cell envelopes of stratified squamous epithelia. J Struct Biol. 1998;122(1):76–85.
Carregaro F, Stefanini ACB, Henrique T, Tajara EH. Study of small proline-rich proteins (SPRRs) in health and disease: a review of the literature. Arch Dermatol Res. 2013;305(10):857–66.
Tesfaigzi J, Carlson DM. Expression, regulation, and function of the SPR family of proteins. Cell Biochem Biophys. 1999;30(2):243–65.
Zhong A, Xu W, Zhao J, Xie P, Jia S, Sun J, et al. S100A8 and S100A9 are induced by decreased hydration in the epidermis and promote fibroblast activation and fibrosis in the dermis. Am J Pathol. 2016;186(1):109–22.
Kim MJ, Im MA, Lee J-S, Mun JY, Kim DH, Gu A, et al. Effect of S100A8 and S100A9 on expressions of cytokine and skin barrier protein in human keratinocytes. Mol Med Rep. 2019;20(3):2476–83.
Sun X, Kaufman PD. Ki-67: more than a proliferation marker. Chromosoma. 2018;127(2):175–86.
Biniek K, Levi K, Dauskardt RH. Solar UV radiation reduces the barrier function of human skin. PNAS. 2012;109(42):17111–6.
Pandel R, Poljšak B, Godic A, Dahmane R. Skin photoaging and the role of antioxidants in its prevention. ISRN Dermatol. 2013;2013:930164.
Jariashvili K, Madhan B, Brodsky B, Kuchava A, Namicheishvili L, Metreveli N. Uv damage of collagen: Insights from model collagen peptides. Biopolymers. 2012;97(3):189–98.
Yu H, Guo P, Xie X, Wang Y, Chen G. Ferroptosis, a new form of cell death, and its relationships with tumourous diseases. J Cell Mol Med. 2017;21(4):648–57.
Pu F, Chen F, Zhang Z, Shi D, Zhong B, Lv X, et al. Ferroptosis as a novel form of regulated cell death: Implications in the pathogenesis, oncometabolism and treatment of human cancer. Genes & Diseases [Internet]. 2020 Dec 4; https://www.sciencedirect.com/science/article/pii/S2352304220301562. Accessed 12 Oct 2021.
Smith MJ, Fowler M, Naftalin RJ, Siow RCM. UVA irradiation increases ferrous iron release from human skin fibroblast and endothelial cell ferritin: consequences for cell senescence and aging. Free Radic Biol Med. 2020;155:49–57.
Applegate LA, Scaletta C, Panizzon R, Frenk E. Evidence that ferritin is UV inducible in human skin: part of a putative defense mechanism. J Investig Dermatol. 1998;111(1):159–63.
Tang D, Kroemer G. Ferroptosis. Curr Biol. 2020;30(21):R1292–7.
Latunde-Dada GO. Ferroptosis: role of lipid peroxidation, iron and ferritinophagy. Biochim Biophys Acta Gen Subj. 2017;1861(8):1893–900.
Tang D, Chen X, Kang R, Kroemer G. Ferroptosis: molecular mechanisms and health implications. Cell Res. 2021;31:107–25.
Yang M, Chen P, Liu J, Zhu S, Kroemer G, Klionsky DJ, et al. Clockophagy is a novel selective autophagy process favoring ferroptosis. Sci Adv. 2019;5(7):eaaw238.
Liu J, Yang M, Kang R, Klionsky DJ, Tang D. Autophagic degradation of the circadian clock regulator promotes ferroptosis. Autophagy. 2019;15(11):2033–5.
Acknowledgements
We thank Christin Rakers from Merck HealthCare for the docking studies of MeO-MBM to the retinoic acid receptor. We thank René Scheurich and Hans-Juergen Driller for planning in vivo studies and the synthesis of MeO-MBM.
Funding
This research and the journal’s Rapid Service Fees were funded by Merck KGaA, Darmstadt, Germany.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author contributions
Michael Termer, Anita Jaeger and Joerg von Hagen contributed to the conception and design of the study. Material preparation, data collection and analysis were performed by all authors. The first draft of the manuscript was written by Michael Termer, Anita Jaeger and Joerg von Hagen, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Prior presentation
This manuscript has not been published or presented elsewhere in part or in entirety and is not under consideration by another journal.
Disclosures
Michael Termer, Anita Jaeger, Cornelia M. Keck and Harald Kolmar can have nothing to disclose. Christophe Carola, Andrew Salazar and Joerg von Hagen are employees of Merck KGaA.
Compliance with ethics guidelines
This study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Toxicological and Regulatory Affairs Review Board of Merck KGaA, Darmstadt, Germany. All participants were informed of the aims and methods of the study and gave their written consent.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Termer, M., Jaeger, A., Carola, C. et al. Methoxy-Monobenzoylmethane Protects Skin from UV-Induced Damages in a Randomized, Placebo Controlled, Double-Blinded Human In Vivo Study and Prevents Signs of Inflammation While Improving the Skin Barrier. Dermatol Ther (Heidelb) 12, 435–449 (2022). https://doi.org/10.1007/s13555-021-00652-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-021-00652-3