Abstract
Background
The incidence of comorbidity between type 2 diabetes mellitus (T2DM) and metabolic-associated fatty liver disease (MAFLD) is high, and patients tend to be younger. When people develop metabolic diseases such as T2DM and MAFLD, the original homeostasis of the gut microbiota in the body is disrupted, and gut flora drift occurs. This study investigated the relationship between the number of gut flora and MAFLD in young-onset T2DM.
Methods
This retrospective study analyzed 44 adolescent T2DM patients who were divided into a non-MAFLD group and a MAFLD group. Anthropometric measurements, clinical and biochemical markers, inflammatory markers, thyroid function assessments, and stool specimens were collected. Real-time PCR was performed to quantify several important gut flora constituents at the genus level. Student’s t-test and the chi-square test were applied for group comparisons, and binary regression models were used to explore the relationship between gut flora and MAFLD in young-onset T2DM.
Results
Among the 44 subjects, 26 (59.1%) were diagnosed with MAFLD, and 18 (40.9%) were not. Compared with the non-MAFLD group, body mass index (BMI), abdominal circumference, and levels of blood uric acid and thyroid stimulating hormone (TSH) in the MAFLD group were significantly increased, and age level and high-density lipoprotein cholesterol (HDL-C) were significantly decreased (p < 0.05). Compared with the non-MAFLD group, the abundance of Faecalibacterium prausnitzii and Bifidobacterium in the MAFLD group was significantly reduced, and the abundance of Enterococcus and Lactobacillus was significantly increased (p < 0.05). In the multivariate regression analysis, Faecalibacterium prausnitzii and Bifidobacterium were independent protective factors for MAFLD in young-onset T2DM, after excluding confounding factors.
Conclusion
In young-onset T2DM, there was a difference in gut flora between patients with MAFLD and those without MAFLD. Faecalibacterium prausnitzii and Bifidobacterium were independent protective factors for MAFLD in young-onset T2DM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Type 2 diabetes mellitus (T2DM) has emerged as one of the most severe health concerns worldwide and is traditionally considered to be a chronic disease of older individuals. However, due to changing lifestyles, including a sedentary lifestyle, sleep structure alterations, physical inactivity, and overeating, the largest increase in T2DM in this century has occurred among adolescents and adults under the age of 40. [1] We classified patients as having young-onset diabetes if they were diagnosed before the age of 40 years and as having late-onset diabetes if they were diagnosed at 40 years or older [2]. Metabolic-associated fatty liver disease (MAFLD) is a chronic liver disease that involves genetic susceptibility and metabolic and environmental factors, and its incidence rate has been increasing annually, affecting approximately 25% of the global population. [3] The diagnostic criteria for MAFLD are based on evidence of hepatic steatosis in addition to one of the following three criteria, namely, overweight/obesity, presence of type 2 diabetes mellitus, or evidence of metabolic dysregulation [4]. Metabolic disorders such as impaired glycemic control, insulin resistance (IR), and visceral obesity are considered to be the major risk factors for MAFLD, as well as T2DM. Therefore, the prevalence of MAFLD is high in T2DM patients. According to a meta-analysis that included 80 studies from 20 different countries, 47.3–63.7% of patients with T2DM are perceived to have MAFLD. [5] Huang et al. revealed that patients with MAFLD diagnosed by diabetes alone are more susceptible to hepatic fibrosis, which may eventually lead to cirrhosis and cardiovascular disease. [6]
The gut flora are considered the second genome in the human body. It has been established that crosstalk occurs between gut microbiota and human health, as the gut flora have the ability to aid in absorption and metabolism, fight against harmful bacteria, improve immunity, and fight tumors. [7] There is growing evidence that the gut microbiota can act as an endocrine organ involved in the dynamic regulation of the body’s energy homeostasis and immune response. [8] When genetics, environmental factors, diet, and behavioral patterns change, the previously stable gut flora in the body drift. Recent years have shown that patients with T2DM and NAFLD exhibit drifting intestinal flora. A study examined the gut flora of people with normal glucose tolerance (NGT), prediabetes (pre-DM), and newly diagnosed T2DM. The results indicated that the abundance of butyrate-producing bacteria was higher in the NGT group than in the pre-DM group and that the abundance of the genus Bacteroides in the T2DM group was only half that of the NGT and pre-DM groups. [9] Loomba et al. found that among 86 patients with biopsy-proven MAFLD, those with advanced liver fibrosis had a higher abundance of the phylum Proteobacteria, those with stage 0–2 liver fibrosis had a higher abundance of the phylum Firmicutes, and 37 (of 40) predictors of advanced liver fibrosis were associated with gut flora [10]. Impaired intestinal barrier function and increased mucosal permeability in T2DM patients lead to increased absorption of lipopolysaccharide, which is the initiator of the inflammatory cascade and leads to chronic inflammation and insulin resistance by activating specific Toll-like receptor signaling pathways on the surface of hepatocytes, thereby accelerating the formation of MAFLD [11]. However, there is a lack of animal experiments and clinical studies on the changes in gut flora with the coexistence of MAFLD and T2DM, and we found many young-onset T2DM patients with MAFLD in clinical practice. The characteristics of gut flora drift in this group of patients are still unknown.
In this retrospective study, we collected clinical data from adolescent T2DM patients and compared the differences in several major gut flora (e.g., Faecalibacterium prausnitzii, Escherichia coli, Bifidobacterium, Lactobacillus, Enterococcus, Bacteroides, and the phylum Firmicutes) between MAFLD patients and non-MAFLD patients. This study investigated the relationship between the number of gut flora and MAFLD in young-onset T2DM.
Materials and methods
Study participants
A total of 44 patients with T2DM who visited our hospital and received liver ultrasound from October 2020 to July 2021 were recruited for the study. The recruitment criteria were as follows: 1) adolescents and adults less than 40 years old, 2) sex not limited, 3) complete clinical data, and 4) informed consent. The exclusion criteria were as follows: 1) pregnant or lactating women; 2) acute complications such as diabetic ketoacidosis and hyperosmolar coma; 3) patients with acute and chronic infections; 4) patients with acute cardiac, hepatic, gastrointestinal, renal and cerebrovascular lesions; 5) patients with serious trauma or surgery within 6 months; 6) patients with malignant tumors and clinical connective tissue diseases; or 7) other serious endocrine metabolic diseases (such as hyperthyroidism, hypothyroidism, Cushing’s syndrome). This retrospective study was approved by the Ethics Committee of XXX Hospital (No. 2020018), and the participants provided written informed consent for personal information collection. Finally, the participants were divided into a non-MAFLD group (n = 18) and a MAFLD group (n = 26) according to MAFLD diagnostic criteria. [4]
Real-time qPCR and microbial quantification
Early morning fecal samples were collected from all patients, and the fresh fecal samples (10 ± 5 g) were snap frozen in a − 80 °C refrigerator within 2 h. Total microbial DNA was extracted from all stool specimens using a QIAamp DNA Stool Mini Kit (QIAGEN, Frankfurt, Germany). Quantitative real-time PCRs (qPCRs) were performed with FTC-3000TM real-time quantitative thermal cycler (Funglyn, Shanghai, China). All qPCRs were run with 3 replicates per DNA. Standard curves were set up by serially diluting the pMD18-T vector plasmid with the appropriate insert from 107 to 102 target gene copies µl−1 for every primer set. The standard curve was obtained using linear regression of threshold cycle numbers (ct) versus log copy numbers of targets. Real-time qPCRs were performed in 25 µl reaction mixtures that were composed of 12.5 µl SRBR Premix Ex Taq (Takara, Osaka, Japan), 1 µl of each forward and reverse primer, 5 µl of template DNA, and sterilized deionized water. The primers are described in Table 1. Melting curve analyses were performed from 60 to 96 °C with increments of 0.1 °C per cycle. The amounts of gut flora were log transformed for analysis.
Measurements
Baseline characteristics such as age, sex duration of diabetes, history of smoking, history of drinking, and family history of diabetes were collected by reviewing medical records. Anthropometric measurements (height, weight, abdominal circumference) were collected according to a standard protocol. Measurements of routine blood tests, fasting plasma glucose (FPG), 2-h postprandial blood glucose (2hPG), glycosylated hemoglobin (HbA1c), triglycerides (TGs), total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), serum uric acid, serum creatinine, thyroid stimulating hormone (TSH), free triiodothyronine (fT3), and free thyroxine (fT4) were performed using standard laboratory methods.
Statistical analysis
IBM SPSS Statistics 24.0 (IBM Corp., Armonk, NY, USA) was used for the statistical analysis. Variables were examined for normality (normal plots), and nonnormally distributed variables were log transformed. The independent-samples t-test (for normally distributed variables) or the Mann‒Whitney test (if nonparametric tests were required) was used to evaluate the significant differences in continuous variables, while the chi-squared test was used to evaluate the significant differences in categorical variables. Correlations of gut flora with BMI, abdominal circumference, FBG, and other variables were examined using Pearson correlation coefficients. Binary logistic regression analyses were used to evaluate the association between the amounts of gut flora and risk of MAFLD in young-onset T2DM after correction for potential confounders. A p value < 0.05 was considered statistically significant.
Results
Participant characteristics
A total of 44 participants were divided into a non-MAFLD group (n = 18) and a MAFLD group (n = 26). There was no statistically significant difference between the two groups in sex, DM course, history of smoking or alcohol consumption, or family history of diabetes (p > 0.05). The MAFLD group was younger than the non-MAFLD group (p < 0.05).
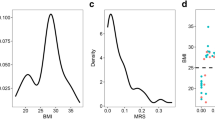
The MAFLD group had a larger BMI (28.97 ± 5.12 kg/m2 versus 23.75 ± 3.95 kg/m2, p < 0.05) and abdominal circumference (98.79 ± 13.24 cm versus 86.33 ± 9.00 cm, p < 0.05) than the non-MAFLD group. Regarding biochemical features, HDL-C in the MAFLD group was lower than that in the non-MAFLD group (0.97 ± 0.21 mmol/l versus 1.14 ± 0.32 mmol/l, p < 0.05), while the blood uric acid level was higher than that in the non-MAFLD group (460.66 ± 190.90 µmol/l versus 367.07 ± 91.89 µmol/l, p < 0.05). Regarding thyroid function, TSH was higher in the MAFLD group than in the non-MAFLD group (1.90 ± 0.88 mIU/l versus 1.47 ± 0.37 mIU/l, p < 0.05). No significant difference was observed in FPG or 2hPG between the two groups, although the values were relatively abundant in the MAFLD group compared to the non-MAFLD group (p = 0.123 and p = 0.418, respectively). HbA1c, other lipid profiles (TC, TG, and LDL-C values), and inflammation indicators (NLR, PLR) did not differ between the two groups. The participant characteristics are reported in Table 2.
Quantitative PCR analysis of gut flora
The MAFLD group had lower amounts of Faecalibacterium prausnitzii (8.76 ± 0.69 versus 9.45 ± 0.74, p < 0.05) and Bifidobacterium (6.56 ± 0.78 versus 7.35 ± 1.13, p < 0.05) and larger amounts of Enterococcus (7.27 ± 1.01 versus 6.66 ± 0.81, p < 0.05) and Lactobacillus (7.11 ± 0.70 versus 6.51 ± 1.03, p < 0.05). We did not observe any significant differences in the amounts of other gut flora (Bacteroides fragilis, Escherichia coli, Firmicutes) between the MAFLD groups and the non-MAFLD group (Table 3).
Correlation between gut flora and clinical data
Pearson correlation analysis was performed between the significantly different gut flora and related clinical indicators between the two groups. We reported a negative correlation between abdominal circumference, blood uric acid level, NLR, and the abundance of Faecalibacterium prausnitzii. We also found that the amount of Enterococcus was positively correlated with abdominal circumference; the amount of Lactobacillus was positively correlated with abdominal circumference, HbA1c, and LDL cholesterol; and the amounts of Bifidobacterium were negatively correlated with abdominal circumference and NLR (Table 4).
Association between the amounts of gut flora and risk of MAFLD in young-onset T2DM
Multivariate binary linear regression analysis was performed to assess the influence of gut flora on the risk of MAFLD (Table 5). The model was adjusted for age, sex, whether diabetes was newly diagnosed, and BMI. The results suggested that after adjusting for confounders, Faecalibacterium prausnitzii (OR = 0.197, 95% CI = 0.047–0.820) and Bifidobacterium (OR = 0.340, 95% CI = 0.121–0.959) remained as independent protective factors for MAFLD in adolescent T2DM. In other words, as the amounts of Faecalibacterium prausnitzii and Bifidobacterium increased, the probability of MAFLD decreased in young-onset T2DM.
Discussion
The main risk of T2DM is the damage to target organs caused by its chronic hyperglycemic state, and MAFLD is the main form of liver damage in T2DM. [12] For the past few years, it has been shown that gut flora can participate in the development of T2DM, MAFLD, and other metabolic diseases by regulating host energy metabolism and improving the inflammatory response. [13,14,15] In this study, we compared the clinical characteristics and differences in gut flora between MAFLD and non-MAFLD patients in young-onset T2DM and explored the relationship between the amounts of gut flora and MAFLD in young-onset T2DM. We found that F. prausnitzii and Bifidobacterium were protective factors for MAFLD in young-onset T2DM, independent of age, sex, DM course, and other confounders.
F. prausnitzii is considered one of the most important members of Firmicutes and is one of the most abundant flora in the intestines of healthy individuals, and its absence inevitably induces gut microbiota disturbance. [16] Recent studies have shown that F. prausnitzii is strongly associated with intestinal inflammatory diseases such as ulcerative colitis and Crohn’s disease; a LACK of F. prausnitzii is associated with the diseases and that its presence improves health benefits. [17, 18] F. prausnitzii induces the secretion of IL-10, an anti-inflammatory cytokine, in peripheral blood mononuclear cells (PBMCs). Munukka et al. reported that F. prausnitzii–treated mice had lower liver fat content, aspartate aminotransferase, and alanine aminotransferase and increased fatty acid oxidation and adiponectin signaling in the liver compared to high-fat control mice. [19] Its exact mechanism is related to an increase in adiponectin expression in visceral adipose tissue, an increase in insulin sensitivity, and decrease in inflammation in subcutaneous and visceral adipose tissue. Our study found that the amounts of F. prausnitzii were lower in the MAFLD population and were negatively correlated with SUA and NLR. SUA causes oxidative stress in mitochondria, activates the NLRP3 inflammatory complex, and exacerbates the hepatic inflammatory response and insulin resistance (IR), while NLR is considered a biomarker that reflects the inflammatory state of the body, and when NLR is increased, MAFLD patients are more likely to further develop hepatitis and liver fibrosis. [20] Martin et al. isolated strains of F. prausnitzii from the feces of healthy volunteers. [21] By studying their products, antibiotic resistance, immunomodulatory functions, and metabolic characteristics, the researchers found that F. prausnitzii has good anti-inflammatory effects and is a good candidate for the next generation of probiotics.
Bifidobacterium is extensively used as a probiotic, and 72 subspecies have been identified and sequenced that play an essential role in maintaining intestinal function and human homeostasis. [22] A metagenomics analysis of the duodenal microbiota of obese patients with T2DM revealed that the abundance of Bifidobacterium was significantly lower in obese individuals and obese patients with T2DM than in non-obese individuals. [23] Using a multiomics approach, Turroni et al. analyzed the interactions between four strains of human intestinal commensals (Bifidobacterium bifidum PRL2010, Bifidobacterium adolescentis 22L, Bifidobacterium breve 12L, and Bifidobacterium longum subsp. infantis ATCC15697) in the intestine of mice. [24] The results revealed that Bifidobacterium cooperated and established a symbiotic relationship with each other in a competitive environment through glycan harvesting, glycan breakdown, and crossfeeding behavior. The composition of the rat cecal microflora significantly changed with the introduction of Bifidobacterium, and the abundance of sugar-degrading flora such as Lactobacillus increased. Therefore, the intestinal degradation of plant carbohydrates and host polysaccharides was enhanced. Animal research demonstrated that probiotics from the combination of Lactobacillus and Bifidobacterium delayed the progression of high-fat-diet-induced NAFLD in rats, with significant reductions in body weight, serum free fatty acid, TG, ALT, IL-1β, and IL-18 levels; significant reductions in Gpr109a expression in liver and adipose tissue; and significant increases in butyric acid levels. [25] The aforementioned study suggested that Bifidobacterium was negatively associated with obesity, low-grade inflammation, insulin resistance, and glucose metabolism disorders. Our study also found that the amounts of Bifidobacterium were lower in MAFLD patients and were negatively correlated with BMI, abdominal circumference, and NLR, but not significantly correlated with glucose metabolism indicators (FBG, 2hPG, HAb1c).
Although they were not an independent risk factor for MAFLD in young-onset T2DM, we observed that the amounts of Enterococcus and Lactobacillus were higher in patients with MAFLD. Enterococcus are considered the second most common cause of nosocomial infections (following Escherichia coli). Based on mouse models and human data, Llorente et al. found that proton pump inhibitors can lead to liver inflammation and hepatocyte death by increasing the amounts of Enterococcus in the intestine and promoting their translocation. [26] Interestingly, as a probiotic, several studies have observed a positive correlation between Lactobacillus and obesity. [27,28,29] It has also been found that Lactobacillus rhamnosus GG, the most common probiotic, prevents the development of fatty liver by competing with the host intestine for fatty acids and inhibiting fatty acid metabolism and absorption in the intestine to inhibit liver fat accumulation. [30] Since dysbiosis of Lactobacillus is common in patients with T2DM and MAFLD, the mechanisms by which it acts on these two metabolic diseases need to be further explored.
In addition, exploring the clinical characteristics of patients with combined MAFLD in T2DM, we found that even among adolescents and adults less than 40 years old, patients with MAFLD were younger (35.4 ± 7.3 years versus 29.2 ± 7.3 years, p = 0.008), which may be related to the multiple burdens of study, career, and family in younger T2DM patients and more unhealthy living, eating, and sleeping habits, thus increasing the metabolic disorder risk. We also found that adolescent T2DM combined with MAFLD was characterized by high BMI, high abdominal circumference, low HDL-C, and high SUA (p < 0.05). It is worth mentioning that TSH levels were higher in the MAFLD group. A cross-sectional study showed that in a T2DM population with HbA1c ≥ 7%, elevated levels of TSH were associated not only with the prevalence of MAFLD but also with the degree of MAFLD steatosis. [31] Existing research has shown the following mechanism: TSH acts on hormone-sensitive triglyceride lipase (HSL) and adipose triglyceride lipase (ATGL) to promote adipocyte differentiation and thus inhibit adipose tissue breakdown. In addition, TSH increases triglyceride synthesis by regulating the expression activity of sterol regulatory element-binding protein-1c (SREBP-1c) in hepatocytes. [32]
This study entailed some limitations. First, the sample size was small, and the results were limited by geographic constraints. Second, a detailed medication history was not taken, and the effect of glucose-lowering drugs on gut flora could not be excluded. Third, due to the retrospective nature of this study, a causative relationship between gut flora and MAFLD in young-onset T2DM could not be established. Therefore, in further research, we should design multicenter prospective studies based on large sample sizes and collect medication histories that may affect the gut flora.
Conclusion
In conclusion, our study revealed that the gut flora of MAFLD patients and non-MAFLD patients in young-onset T2DM were different. The amounts of F. prausnitzii and Bifidobacterium were lower and the amounts of Enterococcus and Lactobacillus were higher in the MAFLD group. F. prausnitzii and Bifidobacterium were protective factors for MAFLD in young-onset T2DM, independent of age, sex, DM course, and other confounders. These results suggest that we might prevent or treat MAFLD in young onset with T2DM by regulating the corresponding gut flora.
Data Availability
The data used to support the findings of this study are available from the corresponding author upon request.
References
Magliano D, Sacre J, Harding J, et al. Young-onset type 2 diabetes mellitus - implications for morbidity and mortality. Nat Rev Endocrinol. 2020;16:321–31. https://doi.org/10.1038/s41574-020-0334-z.
Yeung RO, Zhang Y, Luk A, et al. Metabolic profiles and treatment gaps in young-onset type 2 diabetes in Asia (the JADE programme): a cross-sectional study of a prospective cohort [published correction appears in Lancet Diabetes Endocrinol. Lancet Diabetes Endocrinol. 2014;2(12):935–43. https://doi.org/10.1016/S2213-8587(14)70137-8.
Ye Q, Zou B, Yeo Y, et al. Global prevalence, incidence, and outcomes of non-obese or lean non-alcoholic fatty liver disease: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2020;5:739–52. https://doi.org/10.1016/s2468-1253(20)30077-7.
Eslam M, Newsome P, Sarin S, et al. A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement. J Hepatol. 2020;73:202–9. https://doi.org/10.1016/j.jhep.2020.03.039.
Younossi ZM, Golabi P, de Avila L, et al. The global epidemiology of NAFLD and NASH in patients with type 2 diabetes: A systematic review and meta-analysis. J Hepatol. 2019;71(4):793–801. https://doi.org/10.1016/j.jhep.2019.06.021.
Huang J, Ou W, Wang M, et al. MAFLD criteria guide the subtyping of patients with fatty liver disease. Risk Manag Healthc Policy. 2021;14:491–501. https://doi.org/10.2147/rmhp.S285880.
Plata C, Cruz C, Cervantes L, et al. The gut microbiota and its relationship with chronic kidney disease. Int Urol Nephrol. 2019;51:2209–26. https://doi.org/10.1007/s11255-019-02291-2.
Clarke G, Stilling R, Kennedy P, et al. Minireview: gut microbiota: the neglected endocrine organ. Mol Endocrinol. 2014;28:1221–38. https://doi.org/10.1210/me.2014-1108.
Zhang X, Shen D, Fang Z, et al. Human gut microbiota changes reveal the progression of glucose intolerance. PLoS ONE. 2013;8:e71108. https://doi.org/10.1371/journal.pone.0071108.
Loomba R, Seguritan V, Li W, et al. Gut Microbiome-based metagenomic signature for non-invasive detection of advanced fibrosis in human nonalcoholic fatty liver Disease. Cell Metab. 2017;25:1054-1062.e1055. https://doi.org/10.1016/j.cmet.2017.04.001.
Machado MV, Cortez-Pinto H. Diet, Microbiota, Obesity, and NAFLD: a dangerous quartet. Int J Mol Sci. 2016;17(4):481. https://doi.org/10.3390/ijms17040481.
Targher G, Corey K, Byrne C, et al. The complex link between NAFLD and type 2 diabetes mellitus - mechanisms and treatments. Nat Rev Gastroenterol Hepatol. 2021. https://doi.org/10.1038/s41575-021-00448-y.
Caussy C, Loomba R. Gut microbiome, microbial metabolites and the development of NAFLD. Nat Rev Gastroenterol Hepatol. 2018;15:719–20. https://doi.org/10.1038/s41575-018-0058-x.
Ng S, Xu Z, Mak J, et al. Microbiota engraftment after faecal microbiota transplantation in obese subjects with type 2 diabetes: a 24-week, double-blind, randomised controlled trial. Gut. 2021. https://doi.org/10.1136/gutjnl-2020-323617.
Zhao L, Zhang F, Ding X, et al. Gut bacteria selectively promoted by dietary fibers alleviate type 2 diabetes. Science. 2018;359:1151–6. https://doi.org/10.1126/science.aao5774.
Flint H, Scott K, Louis P, et al. The role of the gut microbiota in nutrition and health. Nat Rev Gastroenterol Hepatol. 2012;9:577–89. https://doi.org/10.1038/nrgastro.2012.156.
Machiels K, Joossens M, Sabino J, et al. A decrease of the butyrate-producing species Roseburia hominis and Faecalibacterium prausnitzii defines dysbiosis in patients with ulcerative colitis. Gut. 2014;63:1275–83. https://doi.org/10.1136/gutjnl-2013-304833.
Miquel S, Martín R, Rossi O, et al. Faecalibacterium prausnitzii and human intestinal health. Curr Opin Microbiol. 2013;16:255–61. https://doi.org/10.1016/j.mib.2013.06.003.
Munukka E, Rintala A, Toivonen R, et al. Faecalibacterium prausnitzii treatment improves hepatic health and reduces adipose tissue inflammation in high-fat fed mice. ISME J. 2017;11:1667–79. https://doi.org/10.1038/ismej.2017.24.
Abdel-Razik A, Mousa N, Shabana W, et al. A novel model using mean platelet volume and neutrophil to lymphocyte ratio as a marker of nonalcoholic steatohepatitis in NAFLD patients: multicentric study. Eur J Gastroenterol Hepatol. 2016;28:e1-9. https://doi.org/10.1097/meg.0000000000000486.
Martín R, Miquel S, Benevides L, et al. Faecalibacterium prausnitziifunctional characterization of novel strains isolated from healthy volunteers: a step forward in the use of as a next-generation probiotic. Front Microbiol. 2017;8:1226. https://doi.org/10.3389/fmicb.2017.01226.
Lugli G, Duranti S, Albert K, et al. Unveiling Genomic Diversity among Members of the Species Bifidobacterium pseudolongum, a Widely Distributed Gut Commensal of the Animal Kingdom. Appl Environ Microbiol. 2019;85(8):e03065-18. https://doi.org/10.1128/aem.03065-18.
Sroka-Oleksiak A, Młodzińska A, Bulanda M, et al. Metagenomic analysis of duodenal microbiota reveals a potential biomarker of dysbiosis in the course of obesity and type 2 diabetes: a pilot study. J Clin Med. 2020;9(2):369. https://doi.org/10.3390/jcm9020369.
Turroni F, Milani C, Duranti S, et al. Deciphering bifidobacterial-mediated metabolic interactions and their impact on gut microbiota by a multi-omics approach. ISME J. 2016;10:1656–68. https://doi.org/10.1038/ismej.2015.236.
Liang Y, Lin C, Zhang Y, et al. Probiotic mixture of Lactobacillus and Bifidobacterium alleviates systemic adiposity and inflammation in non-alcoholic fatty liver disease rats through Gpr109a and the commensal metabolite butyrate. Inflammopharmacology. 2018;26:1051–5. https://doi.org/10.1007/s10787-018-0479-8.
Llorente C, Jepsen P, Inamine T, et al. Gastric acid suppression promotes alcoholic liver disease by inducing overgrowth of intestinal Enterococcus. Nat Commun. 2017;8:837. https://doi.org/10.1038/s41467-017-00796-x.
Armougom F, Henry M, Vialettes B, et al. Monitoring bacterial community of human gut microbiota reveals an increase in Lactobacillus in obese patients and Methanogens in anorexic patients. PLoS ONE. 2009;4:e7125. https://doi.org/10.1371/journal.pone.0007125.
Khan M, Raoult D, Richet H, et al. Growth-promoting effects of single-dose intragastrically administered probiotics in chickens. Br Poult Sci. 2007;48:732–5. https://doi.org/10.1080/00071660701716222.
Million M, Maraninchi M, Henry M, et al. Obesity-associated gut microbiota is enriched in Lactobacillus reuteri and depleted in Bifidobacterium animalis and Methanobrevibacter smithii. Int J Obes. 2012;36:817–25. https://doi.org/10.1038/ijo.2011.153.
Jang H, Park H, Kang D, et al. A protective mechanism of probiotic Lactobacillus against hepatic steatosis via reducing host intestinal fatty acid absorption. Exp Mol Med. 2019;51:1–14. https://doi.org/10.1038/s12276-019-0293-4.
Tan Y, Tang X, Mu P, et al. High-normal serum thyrotropin levels increased the risk of non-alcoholic fatty liver disease in euthyroid subjects with type 2 diabetes. Diabetes Metab Syndr Obes Targets Ther. 2021;14:2841–9. https://doi.org/10.2147/dmso.S313224.
Reinehr T, de Sousa G, Andler W. Hyperthyrotropinemia in obese children is reversible after weight loss and is not related to lipids. J Clin Endocrinol Metab. 2006;91:3088–3091. 2006/05/11. https://doi.org/10.1210/jc.2006-0095.
Funding
The study was funded by Fuzhou Science and Technology Plan Project (Project: Correlation of inflammation, oxidative stress, liver fibrosis and sleep deprivation in adolescent diabetic MAFLD rats; Grant No. 2021-S-155) and Fuzhou Health Science and Technology Innovation Platform Construction Project (Project: Building an integrated platform for diabetes chronic disease management; Grant No. 2020-S-wp4).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This retrospective study was approved by the Ethics Committee of XXX Hospital (No. 2020018), and the participants provided written informed consent for personal information collection..
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chen, S., Cai, S., Xu, J. et al. Lack of Faecalibacterium prausnitzii and Bifidobacterium is associated with a higher risk of metabolic associated fatty liver disease in young-onset type 2 diabetes. Int J Diabetes Dev Ctries 44, 167–174 (2024). https://doi.org/10.1007/s13410-022-01161-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13410-022-01161-5