Abstract
An optimized method for bacterial strain differentiation, based on combination of Repeated Sequences and Whole Genome Alignment Differential Analysis (RS&WGADA), is presented in this report. In this analysis, 51 Acinetobacter baumannii multidrug-resistance strains from one hospital environment and patients from 14 hospital wards were classified on the basis of polymorphisms of repeated sequences located in CRISPR region, variation in the gene encoding the EmrA-homologue of E. coli, and antibiotic resistance patterns, in combination with three newly identified polymorphic regions in the genomes of A. baumannii clinical isolates. Differential analysis of two similarity matrices between different genotypes and resistance patterns allowed to distinguish three significant correlations (p < 0.05) between 172 bp DNA insertion combined with resistance to chloramphenicol and gentamycin. Interestingly, 45 and 55 bp DNA insertions within the CRISPR region were identified, and combined during analyses with resistance/susceptibility to trimethoprim/sulfamethoxazole. Moreover, 184 or 1374 bp DNA length polymorphisms in the genomic region located upstream of the GTP cyclohydrolase I gene, associated mainly with imipenem susceptibility, was identified. In addition, considerable nucleotide polymorphism of the gene encoding the gamma/tau subunit of DNA polymerase III, an enzyme crucial for bacterial DNA replication, was discovered. The differentiation analysis performed using the above described approach allowed us to monitor the distribution of A. baumannii isolates in different wards of the hospital in the time frame of several years, indicating that the optimized method may be useful in hospital epidemiological studies, particularly in identification of the source of primary infections.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The genome of each microorganism is a source of knowledge that can be applied for strain differentiation, based on bioinformatic tools and available techniques of molecular biology, suitable for epidemiological investigations. Among the species of the genus Acinetobacter, A. baumannii strains manifest the highest pathogenicity (Wong et al. 2017; Skariyachan et al. 2019). They are highly opportunistic microorganisms, responsible for hospital infections related to ability to adapt to different environmental conditions (Antunes et al. 2014). At the beginning of the twenty-first century, no complete genome sequence of Acinetobacter sp. was known. Barbe et al. (2004) published the first sequence of Acinetobacter sp. ADP1 genome, and later Smith et al. (2007) published the complete genome of A. baumannii ATCC 17,978. Subsequently, the first genomic sequence of the multidrug-resistant A. baumannii strain was published by Adams et al. (2008). Presently, complete sequences of the genomic DNA of A. baumannii are known for about 250 strains (http://www.ncbi.nlm.nih.gov, database retrieved on 10 December 2020). As indicated by various research teams, repeated sequences of A. baumannii and other microorganisms have great impact in the process of generating pathogenicity for immunocompromised hosts (Zhou et al. 2014; Shariat and Dudley 2014; Nabil et al. 2015) or adaptation skills to different environmental conditions (Zhou et al. 2014; Shariat and Dudley 2014; Karah et al. 2015).
The presence of tandem DNA repeats in genomes of A. baumannii was confirmed by several groups (Martín-Lozano et al. 2002; Turton et al. 2009; Irfan et al. 2011; Pourcel et al. 2011; Minandri et al. 2012; Ergin et al. 2013; Ahmed and Alp 2015; Villalón et al. 2015). Based on these sequences, different methods of differentiation of A. baumannii strains have been developed; however, they take into account only their diversifying power of evolutionary changes of the Acinetobacter genus (Touchon et al. 2014). Thus, their features responsible for drug resistance or pseudo-immunological bacterial responses, encoded in the Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) system, which evolved to protect the cells from exogenous phage and plasmid DNA invasion, are ignored in such analyses. On the other hand, as suggested by Touchon et al. (2014), the next step in the process of strains’ classification should be focused on confrontation of the genetic and phenotypic features related to pathogenicity of bacterial species. To address some of the above features, an optimized method for A. baumannii differential analysis is proposed in this report. It is based on combination of the previously described method based on analysis of repeated sequences (Nowak-Zaleska et al. 2008, 2016) and whole genome alignment.
Materials and methods
Bacterial strains
We used 51 A. baumannii isolates from diagnostic materials of the hospital environments of Antoni Jurasz University Hospital in Bydgoszcz. These isolates were derived from 11 hospital wards (Dermatology, Endocrinology, Geriatrics, General and Endocrine Surgery, General and Vascular Surgery, Intensive Care Units, Neurology, Nephrology, Neurosurgery, Orthopedic, Plastic Surgery), 2 clinics (Orthopedic Outpatient Clinic, Surgical Outpatient Clinic), and Rehabilitation Department. The isolates were collected during the period of 2003–2006 (Table 1). The following strains were isolated from different diagnostic materials: 10 from bronchoalveolar lavages, 8 from bedsores, 2 from blood, 1 from cerebrospinal fluid, 2 from drains, 2 from drain swabs, 1 from needle tip, 1 from pus, 8 from respiratory secretions, 2 from tracheostomy tube swabs, 1 from tube swab, 9 from ulceration wounds, and 4 from urine. Strains were identified based on ID GN phenotypic identification system, including drug sensitivity. This identification was conducted using Kirby–Bauer method, according to CLSI instructions (for details, see Nowak-Zaleska et al. 2008, 2016).
Locus identification with repeated sequences
The isolates of A. baumannii were differentiated on the basis of previously published polymorphisms of repeated sequences located in the CRISPR region (Touchon et al. 2014), variation in the gene encoding the EmrA homologue of E. coli (Nowak-Zaleska et al. 2016), and three newly identified (in this study) polymorphic regions (Tables 2 and 3).
DNA-technology methods
The genetic material from the isolates was obtained using Genomic Mini Set, purchased from A&A Biotechnology (Gdynia, Poland), following the manufacturer’s instruction. For the DR-PCR/RFLP genotyping method, sequences of primers, the PCR reaction conditions, and enzymatic digestion of PCR products were previously described (Nowak-Zaleska et al. 2008). Briefly, the amplification reactions were conducted according to the following time–temperature profile: 94 °C for 2 min, during the initial denaturation step, 35 cycles consisting of the DNA denaturation at 94 °C for 1 min, hybridization at 68 °C for 1 min, and extension at 72 °C for 2 min. The amplification products were subjected to the restriction fragment length polymorphism (RFLP) analysis using HaeIII and SsiI restriction enzymes. Separation of restriction fragments was performed electrophoretically, in 12% polyacrylamide gels, and results were documented using Versa Doc Imaging System, ver. 1000. The homologous region of the emrA resistance-related gene, containing 6-nt repeats, was analyzed as described previously (Nowak-Zaleska et al. 2016). Identification of three newly discovered polymorphic regions was possible after multiple alignment of nine A. baumannii genomes (see Table 2), using the MAFFT 7.271 software (Katoh et al. 2002). Subsequently, three pairs of primers, shown in Table 3, were used in the PCR analysis. The PCR reactions were conducted in 25 μl reaction mixtures, using the Eppendorf AG 22,331 thermal cycler. The PCR mixtures were as follows: 1.5 U of RUN DNA polymerase (purchased from A&A Biotechnology), PCR reaction buffer containing 10 mM KCl, 10 mM (NH4)2SO4, 0.1% Triton X-100, 20 mM Tris, pH 8.5, 2 mM of Mg2Cl, 2 mM of each deoxynucleoside triphosphates, 25 pM of suitable pairs of primers, and 50 ng/μl of template DNA. Amplified PCR products were separated using 2% agarose gel electrophoresis and standard ethidium bromide staining procedure (Sambrook et al. 1989). Images of the gels were obtained using Versa Doc Imaging System, ver. 1000.
Statistical analysis
Statistical analysis was performed using Epi Info 7.2.3.1 software using two-tailed Fisher exact test analysis. The values “1” and “0” were representing resistant and susceptible strains for different antibiotics used in our study. Similarity matrices of different genotypes and resistance features and phylogenetic trees were constructed using package MVSP ver. 3.22.
Results and discussion
To enhance the currently available methods of differentiation of A. baumannii strains, we were searching for previously unknown PCR-derived fragment length polymorphism variations in randomly identified regions of selected genomic sequences. The theoretical values of PCR fragment lengths of the newly discovered polymorphic regions for nine A. baumannii genomes are presented in Table 2. Among three identified polymorphic regions, only one was characterized by the highest length polymorphism. It was recognized as a gene fragment coding for DNA polymerase III subunit gamma/tau, with the Protein_id = AFI95102.1 in the MDR-TJ A. baumannii genome (GenBank accession no. CP003500.1) (Table 3).
In order to increase variation of analyzed A. baumannii isolates, two other previously described variable regions in the genomes of A. baumannii were included in our study (Nowak-Zaleska et al. 2008, 2016). The combined application of the three genetic aforementioned genotypic methods, DR-PCR/RFLP, different number of P-A dipeptide repeats encoded in the N-terminal part of EmrA-homologue gene, as well as three new variables, namely, Aci7 and Aci8, Aci13 and Aci14, and Aci17 and Aci18 (Table 4), combined with known information about resistance patterns for each isolate (Table 5), allowed for recognition of 31 different clusters shown in Table 1.
Detailed analysis of bacterial isolates and diagnostic material revealed significant differences between A. baumannii isolates from bronchoalveolar lavage (BAL) and other clinical samples (p < 0.0001), as well as significant correlation between resistance pattern II and genotype 8th (p < 0.01), presented in Table 1. In addition, significant correlation (p < 0.05) between the frequency of occurrence of 8th A. baumannii genotype in the first trimester of 2006 year in comparison to other periods of isolation time was also evident. Higher Hunter–Gaston Discriminatory Index (HGDI), presented in Table 1, was determined using the method developed in this study, in comparison to previously published genotyping methods (Nowak-Zaleska et al. 2008, 2016). Furthermore, in the course of statistical data analysis, we observed that strains representing clusters 2 and 4 from combined genetic–phenotypic analysis, shown in Table 1, were isolated in two consecutive years 2005 and 2006 (p < 0.0001). These strains represent the 15th genotype pattern, which was present in 2004 and 2005, but with different resistance patterns II, VI, IX, X, XII, and XIII (p = 0.01). In addition, three strains representing 21st cluster with the resistance pattern X appeared in years 2004 and 2006. Moreover, strains with genotypes 6, 12, and 14 were only present in 2003 (p < 0.0001), in comparison to other genotypes, and what is interesting, the resistance pattern II appeared each year, while patterns V, VI, VII, and VIII appeared only between 2003 and 2005 (p = 0.01).
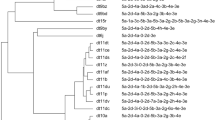
Combined analysis of similarity matrices, obtained using data from Tables 4 and 5, revealed that out of 19 combinations of genetic and resistance markers, only three were significantly different (p < 0.05) (Table 6), as indicated by χ2 value higher than 4, obtained from two phylogenetic trees presented in Fig. 1. Among significantly different mixed parameters identified, there were (1) 172 bp DNA insertion, located in the CRISPR locus, identified using the SsiI enzyme for genotypes 7 to 11, in combination with resistance to chloramphenicol and gentamycin; (2) 45 and 55 bp DNA insertions in the same locus, identified using the HaeIII enzyme, combined with trimethoprim/sulfamethoxazole resistance or susceptibility patterns; and (3) 184 or 1374 bps DNA length polymorphisms in the second genomic region (see tree new PCR region, Table 4), identified in our study for genotypes 1 to 6 and 7 to 16, in combination with imipenem resistance, characteristic for pattern I or susceptibility features, characteristic for other patterns (Table 6).
Phylogenetic trees for different pairs of genetic polymorphisms and resistance/susceptibility features. Branches order obtained based on nearest neighbor method and length–distance calculation based on χ2 method. Significant (p < 0.05) differences indicated in black boxes were identified based on cut-off χ2 value = 4
The presence of A. baumannii genotypes over a period of 4 years in the hospital wards (Table 7), and location of determined genotypes over a 4-year period in hospital wards (Table 8), was also assessed. This analysis provides a possibility to identify the presence of specific isolates in various wards over the period of several years. We suggest that such analyses may be useful in epidemiological studies on the origin and migration of particular bacterial strains between different wards of an investigated hospital. It also gives the possibility to analyze the strains regardless of the time period in which they were collected.
Conclusions
In conclusion, 16 different genotypes out of 51 MDR A. baumannii clinical isolates were identified in our study. Based on combined comparative analysis of genetic and resistance patterns, two significantly different patterns of DNA polymorphisms in the CRISPR coding region, resistance to chloramphenicol and gentamycin features, and resistance or susceptibility to trimethoprim/sulfamethoxazole, specific groups of isolates were identified. Out of 19 genetic markers and antibiotic resistance features, three of them were shown to be statistically significantly different using two statistical tools (Table 6, Fig. 1). In addition, 184 or 1374 bp DNA length polymorphisms in genomic region no. 2, located upstream of the GTP cyclohydrolase I gene, with the Locus_tag = "ABTJ_01152", associated in 94% with susceptibility to imipenem, was identified. Finally, the highest genetic diversity, determined within the DNA polymerase III subunit gamma/tau gene, can be recommended for future genotyping of multidrug-resistant A. baumannii strains. We suggest that the optimized methods, proposed in this report and based on combination of Repeated Sequences and Whole Genome Alignment Differential Analysis (RS&WGADA), can be useful in epidemiological studies concerning specific strains of pathogenic bacteria present in investigated hospitals.
Data availability
Not applicable.
Code availability
Not applicable.
References
Adams MD, Goglin K, Molyneaux N, Hujer KM, Lavender H, Jamison JJ, MacDonald IJ, Martin KM, Russo T, Campagnari AA, Hujer AM, Bonomo RA, Gill SR (2008) Comparative genome sequence analysis of multidrug-resistant Acinetobacter baumannii. J Bacteriol 190:8053–8064. https://doi.org/10.1128/JB.00834-08
Ahmed SS, Alp E (2015) Genotyping methods for monitoring the epidemic evolution of Acinetobacter baumannii strains. J Infect Dev Ctries 9:347–354. https://doi.org/10.3855/jidc.6201
Antunes LC, Visca P, Towner KJ (2014) Acinetobacter baumannii: evolution of a global pathogen. Pathogens and Disease 71:292–301. https://doi.org/10.1111/2049-632X.12125
Barbe V, Vallenet D, Fonknechten N, Kreimeyer A, Oztas S, Labarre L, Cruveiller S, Robert C, Duprat S, Wincker P, Ornston LN, Weissenbach J, Marlière P, Cohen GN, Médigue C (2004) Unique features revealed by the genome sequence of Acinetobacter sp. ADP1, a versatile and naturally transformation competent bacterium. Nucleic Acids Res 32:5766–5779. https://doi.org/10.1093/nar/gkh910
Ergin A, Hascelik G, Eser OK (2013) Molecular characterization of oxacillinases and genotyping of invasive Acinetobacter baumannii isolates using repetitive extragenic palindromic sequence-based polymerase chain reaction in Ankara between 2004 and 2010. Scand J Infect Dis 45:26–31. https://doi.org/10.3109/00365548.2012.708782
Irfan S, Turton JF, Mehraj J, Siddiqui SZ, Haider S, Zafar A, Memon B, Afzal O, Hasan R (2011) Molecular and epidemiological characterisation of clinical isolates of carbapenem-resistant Acinetobacter baumannii from public and private sector intensive care units in Karachi, Pakistan. J Hosp Infect 78:143–148. https://doi.org/10.1016/j.jhin.2011.01.029
Karah N, Samuelsen Ø, Zarrilli R, Sahl JW, Wai SN, Uhlin BE (2015) CRISPR-cas Subtype I-Fb in Acinetobacter baumannii: evolution and utilization for strain subtyping. PLoS ONE 10(2):e0118205. https://doi.org/10.1371/journal.pone.0118205
Katoh K, Misawa K, Kuma K, Miyata T (2002) MAFFT: a novel method for rapid multiple sequence alignment based on fast Fourier transform. Nucleic Acids Res 15:3059–3066
Martín-Lozano D, Cisneros JM, Becerril B, Cuberos L, Prados T, Ortíz-Leyba C, Cañas E, Jachón P (2002) Comparison of a repetitive extragenic palindromic sequence-based PCR method and clinical and microbiological methods for determining strain sources in cases of nosocomial Acinetobacter baumannii bacteremia. J Clin Microbiol 40:4571–4575
Minandri F, D’Arezzo S, Antunes LCS, Pourcel C, Principe L, Petrosillo N, Visca P (2012) Evidence of diversity among epidemiologically related carbapenemase-producing Acinetobacter baumannii strains belonging to international clonal lineage II. J Clin Microbiol 50:590–597. https://doi.org/10.1128/JCM.05555-11
Nabil K, Samuelsen Ø, Zarrilli R, Sahl JW, Wai SN, Uhlin BE (2015) CRISPR-cas subtype I-Fb in Acinetobacter baumannii: evolution and utilization for strain subtyping. PLoS ONE 10(2):e0118205. https://doi.org/10.1371/journal.pone.0118205
Nowak-Zaleska A, Krawczyk B, Kotłowski R, Mikucka A, Gospodarek E (2008) Amplification of a single-locus variable-number direct repeats with restriction fragment length polymorphism (DR-PCR/RFLP) for genetic typing of Acinetobacter baumannii strains. Pol J Microbiol 57:11–17
Nowak-Zaleska A, Wieczór M, Czub J, Nierzwicki Ł, Kotłowski R, Mikucka A, Gospodarek E (2016) Correlation between the number of Pro-Ala repeats in the EmrA homologue of Acinetobacter baumannii and resistance to netilmicin, tobramycin, imipenem and ceftazidime. J Glob Antimicrob Resist 7:145–149. https://doi.org/10.1016/j.jgar.2016.09.004
Pourcel C, Minandri F, Hauck Y, D’Arezzo S, Imperi F, Vergnaud G, Visca P (2011) Identification of variable-number tandem-repeat (VNTR) sequences in Acinetobacter baumannii and interlaboratory validation of an optimized multiple-locus VNTR analysis typing scheme. J Clin Microbiol 49:539–548. https://doi.org/10.1128/JCM.02003-10
Sambrook J, Fritsch EF, Maniatis T (1989) Molecular cloning: a laboratory manual, 2nd edn. Cold Spring Harbor Laboratory Press, Cold Spring Harbor
Shariat N, Dudley EG (2014) CRISPRs: molecular signatures used for pathogen subtyping. Appl Environ Microbiol 80:430–439. https://doi.org/10.1128/AEM.02790-13
Skariyachan S, Taskeen N, Ganta M, Krishna BV (2019) Recent perspectives on the virulent factors and treatment options for multidrug-resistant Acinetobacter baumannii. Crit Rev Microbiol 45:315–333. https://doi.org/10.1080/1040841X.2019.1600472
Smith MG, Gianoulis TA, Pukatzki S, Mekalanos JJ, Ornston LN, Gerstein M, Snyder M (2007) New insights into Acinetobacter baumannii pathogenesis revealed by high-density pyrosequencing and transposon mutagenesis. Genes Dev 21:601–614. https://doi.org/10.1101/gad.1510307
Touchon M, Cury J, Yoon E-J, Krizova L, Cerqueira GC, Murphy C, Feldgarden M, Wortman J, Clermont D, Lambert T, Grillot-Courvalin C, Nemec A, Courvalin P, Rocha EPC (2014) The genomic diversification of the whole Acinetobacter genus: origins, mechanisms, and consequences. Genome Biol Evol 6:2866–2882. https://doi.org/10.1093/gbe/evu225
Turton JF, Matos J, Kaufmann ME, Pitt TL (2009) Variable number tandem repeat loci providing discrimination within widespread genotypes of Acinetobacter baumannii. Eur J Clin Microbiol Infect Dis 28:499–507. https://doi.org/10.1007/s10096-008-0659-3
Villalón P, Valdezate S, Cabezas T, Ortega M, Garrido N, Vindel A, Medina-Pascual MJ, Saez-Nieto JA (2015) Endemic and epidemic Acinetobacter baumannii clones: a twelve-year study in a tertiary care hospital. BMC Microbiol 15:47. https://doi.org/10.1186/s12866-015-0383-y
Wong D, Nielsen TB, Bonomo RA, Pantapalangkoor P, Luna B, Spellberg B (2017) Clinical and pathophysiological overview of Acinetobacter infections: a century of challenges. Clin Microbiol Rev 30:409–447. https://doi.org/10.1128/CMR.00058-16
Zhou K, Aertsen A, Michiels CW (2014) The role of variable DNA tandem repeats in bacterial adaptation. FEMS Microbiol Rev 38:119–141. https://doi.org/10.1111/1574-6976.12036
Funding
This work was partly supported by the State Committee for Scientific Research, grant no. KBN 2P05D 10128.
Author information
Authors and Affiliations
Contributions
R.K.: data curation, investigation, writing—original draft, writing—editing and review, supervision. A.N-Z.: data curation, investigation, writing—original draft and review. G.W.: writing—editing and review.
Corresponding author
Ethics declarations
Ethics approval
The Bioethics Committee waived the need for consent from all patients from whom bacterial strains were isolated and used in this study. Decision no. KB 248/2016 was issued by the Local Bioethics Committee at the Nicolaus Copernicus University Ludwik Rydygier Collegium Medicum in Bydgoszcz, Poland.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflicts of interest
The authors declare that they have no conflict of interest.
Additional information
Communicated by Agnieszka Szalewska-Palasz.
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kotłowski, R., Nowak-Zaleska, A. & Węgrzyn, G. Discrimination of hospital isolates of Acinetobacter baumannii using repeated sequences and whole genome alignment differential analysis. J Appl Genetics 62, 511–521 (2021). https://doi.org/10.1007/s13353-021-00640-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13353-021-00640-5