Abstract
There is still a paucity of information on how in vitro release profiles from drug-loaded contact lenses (CLs) recorded in 3D printed eye models correlate with in vivo profiles. This work aims to evaluate the release profiles of two drug-loaded CLs in a 3D in vitro eye blink model and compare the obtained results with the release in a vial and the drug levels in tear fluid previously obtained from an animal in vivo study. In vitro release in the eye model was tested at two different flow rates (5 and 10 µL/min) and a blink speed of 1 blink/10 s. Model CLs were loaded with two different drugs, hydrophilic pravastatin and hydrophobic resveratrol. The release of both drugs was more sustained and lower in the 3D eye model compared to the in vitro release in vials. Interestingly, both drugs presented similar release patterns in the eye model and in vivo, although the total amount of drugs released in the eye model was significantly lower, especially for resveratrol. Strong correlations between percentages of pravastatin released in the eye model and in vivo were found. These findings suggest that the current 3D printed eye blink model could be a useful tool to measure the release of ophthalmic drugs from medicated CLs. Nevertheless, physiological parameters such as the composition of the tear fluid and eyeball surface, tear flow rates, and temperature should be optimized in further studies.
Graphical abstract

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The use of contact lenses (CLs) as platforms for controlled delivery of ophthalmic drugs was envisioned in 1961 by Otto Wichterle and co-workers [1]. After 60 years, the first commercial drug-delivering CL has become available in Japan, Canada, and the USA [2]. Compared to eye drops, CLs may significantly extend drug residence time and increase ocular bioavailability, while unproductive drug absorption is minimized [3].
CLs are one of the most successfully commercialized biomedical devices, with nearly 150 million users worldwide [4]. However, several obstacles oppose their use as platforms for ocular drug delivery [5]. Most polymers used to prepare CLs, e.g., 2-hydroxyethyl methacrylate (HEMA) and 3-(methacryloyloxy)propyl tris(trimethylsiloxy)silane (TRIS), lack affinity for drugs; thus, typically, CLs do not uptake the required dose or release it too rapidly. A wide variety of strategies to overcome this issue is under development [6,7,8,9]. Additionally, there are no standardized methods for testing in vitro the drug release profiles from CLs. In vitro methods for mimicking the composition and dynamics of tear fluid, and the frequency and pressure of blinking are still a challenge. Thus, in most reports focused on CLs, the in vitro drug release profiles are recorded in small beakers using a variety of medium composition, volume, stirring, and replacement conditions [10, 11]. As a consequence, most in vitro results are not predictive of in vivo performance [12]. This means that in vivo testing in animal models and human preclinical studies are still needed, even to evaluate early-stage drug-CL combination products, which makes the development very costly in time and resources.
In vitro models that mimic the in vivo scenario and key ocular parameters are highly explored. Microfluidic devices have been designed to regulate the flow and volume where CLs are immersed, but other physiological conditions were not reproduced by these devices, including factors such as corneal and eyelid shape and format, tear film thickness, or blinking [13, 14]. 3D printed in vitro eye models to evaluate the in vitro performance of CLs have recently been undertaken to overcome some challenges faced by using microfluidic devices and more appropriately simulate the effects of tear flow rate, tear volume, air exposure, and eyelid blinking frequency [15, 16]. Not surprisingly, under dynamic conditions of low tear fluid flow, CLs showed slower drug release profiles compared to static release in a beaker, prolonging the release for days or weeks for some specific compounds and drugs such as red food dye [16], polyethylene glycol, hydroxypropyl methylcellulose [17], moxifloxacin [18], and fluconazole [19]. Moreover, in vitro models can provide relevant insights in the development process of drug-loaded CLs and prioritize successful materials that may go forward to in vivo testing in animal preclinical models or human clinical studies.
There is still a paucity of information on how in vitro release profiles recorded in 3D printed eye models correlate with in vivo profiles. Comparison of the behavior of the same drug-loaded CLs in both the in vitro model and the common rabbit eye model is, therefore, required for the validation of the information gathered in vitro. To gain an insight into the in vitro–in vivo correlations, the aim of this work was to analyze the release profiles of drug-loaded CLs recorded in a 3D printed in vitro eye blink model and compare the obtained results with the release in a small beaker and the tear levels previously obtained in vivo. For the sake of robustness, CLs loaded with drugs differing in physicochemical properties were tested, namely, CLs designed to uptake pravastatin (a hydrophilic statin, log P = − 0.23 [20]) and resveratrol (a highly hydrophobic antioxidant, log P = 3.09 [21]) were prepared and evaluated [22, 23].
Pravastatin sodium and resveratrol may be useful for the treatment of a wide range of anterior and posterior ocular diseases. Prolonged oral therapy for hypercholesterolemia with statins has been shown to promote corneal healing, prevent cataract formation, reduce glaucoma severity, and reduce the appearance of hard exudates and microaneurysms in patients diagnosed with diabetic macular edema; topical ocular treatment has the advantage of avoiding systemic adverse reactions [24,25,26,27]. Resveratrol is an antioxidant agent that aids the management of oxidative-stress-related eye diseases and improves the healing of corneal epithelial cells [28]. In previous studies, both drugs were incorporated in model CLs, and the in vivo performance was evaluated in New Zealand white rabbits [22, 29]. Both drug-loaded CLs provided significantly higher and more prolonged drug levels in the rabbits’ tear fluid compared to eye drops with the same dose, which favored ocular biodistribution in the anterior and posterior structures of the eye, including cornea, sclera, lens, aqueous and vitreous humors, and retina. To carry out the present work, HEMA-based CLs were copolymerized with specific functional monomers that enhance drug affinity. In the case of pravastatin, HEMA was copolymerized with ethylene glycol phenyl ether methacrylate (EGPEM) and N-(3-aminopropyl) methacrylamide hydrochloride (APMA) (Fig. 1). For resveratrol, methacryloyloxyethyl phosphorylcholine (MPC) was added as an antifouling comonomer. The developed CLs, coded as AECLs and MCLs, demonstrated adequate solvent uptake, light transmission, mechanical properties, and ocular safety. In vitro release experiments were carried out with sterile CLs loaded under specific conditions for each drug depending on their physicochemical properties. In vitro release in the 3D eye blink model was tested at two different tears fluid flow rates (5 and 10 µl/min of fluid) and a blink speed of 1 blink/10 s. The amount of drug released from the CLs was collected and quantified by high-performance liquid chromatography (HPLC). To the best of our knowledge, this is the first time that drug-loaded CL release profiles have been evaluated in an in vitro 3D eye model and in vitro–in vivo correlations (IVIVC) are attempted.
Materials and methods
Materials
Pravastatin sodium was supplied by Biocon Limited (Bengaluru, Karnataka, India). Resveratrol was from ChemCruz, Santa Cruz Biotechnology Inc. (Dallas, TX, USA). Di-sodium hydrogen phosphate anhydrous (NaH2PO4) and 2-hydroxyethyl methacrylate (HEMA) were from Merck (Darmstadt, Germany). N-(3-aminopropyl) methacrylamide hydrochloride (APMA) was from PolySciences Inc. (Warrington, PA, USA). Ethylene glycol dimethacrylate (EGDMA), ethylene glycol phenyl ether methacrylate (EGPEM), 2,2′-azobis(isobutyronitrile) (AIBN), 2-methacryloyloxyethyl phosphorylcholine (MPC), polyvinyl alcohol (PVA, 89–98 kDa, 99% hydrolyzed), and dimethyl sulfoxide (DMSO) were from Sigma-Aldrich (Steinheim, Germany). Sodium chloride (NaCl) was from Labkem (Barcelona, Spain), and sodium hydroxide (NaOH) was from VWR Chemicals (Leuven, Belgium). The 3D printing UV-sensitive resin was from Anycubic Technology Co. (Shenzhen, Guangdong, China). Methanol 99.9% for LC–MS grade was from Thermo Fisher Scientific (Loughborough, UK). Simulated lachrymal fluid (SLF) was prepared as previously reported [22]. Ultrapure water (resistivity > 18.2 MΩ cm; Milli-Q®; Millipore Ibérica, Madrid, Spain) was obtained by reverse osmosis.
Contact lens preparation
Two different types of HEMA-based CLs were prepared as previously described [22, 29]. Briefly, AECLs for pravastatin were prepared by mixing HEMA (3 mL) with APMA (21.45 mg), EGPEM (112.50 µL), and EGDMA (12.10 µL). The monomer solutions were magnetically stirred (200 rpm at room temperature) for 120 min, and the initiator (AIBN, 14.79 mg) was then added and solubilized by magnetic stirring for a further 30 min.
To prepare MCLs for resveratrol, HEMA (3 mL) was mixed with MPC (337.5 mg) and EGDMA (12.10 µL) under magnetic stirring (150 rpm at room temperature) for 60 min. The mixture was kept under magnetic stirring for 30 min more to ensure the complete dissolution of AIBN (32.85 mg).
Both AECLs and MCLs were synthesized by adding 60 µL of monomer solution into curved polypropylene moulds typically used for daily disposable CL preparation. The moulds were kept at 50 °C for 12 h and then at 70 °C for 24 h to complete thermal polymerization. Then, the moulds were immersed in MilliQ® water to facilitate CL separation. The obtained CLs were washed under magnetic stirring (200 rpm) in 1 L of MilliQ® water and NaCl 0.9% until complete removal of unreacted monomers occurred; the solvent was replaced at least three times per day. The absence of unreacted monomers was verified by UV–Vis spectrophotometry (Agilent 8453, Waldbronn, Germany).
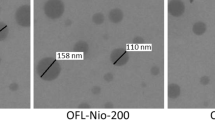
The final dimensions of hydrated CLs (immersed in phosphate buffer, pH 7.4) were approximately 12 mm diameter, 7.8 mm curvature, and 0.1 mm thickness for AECLs and approximately 14 mm diameter, 8.8 mm curvature, and 0.1 mm thickness for MCLs.
Drug loading
Pravastatin sodium
Dried AECLs (average mass 16.91 ± 1.28 mg) were packaged and sealed in polyamide/polyethylene vacuum bags filled with 10 mL of an aqueous pravastatin solution (0.1 mg/mL) for at least 48 h and sterilized by high hydrostatic pressure (HHP, 70 °C and 600 MPa for 10 min) [30]. The CLs were stored in sealed bags at room temperature and protected from light until release experiments were performed. All the experiments were carried out in quadruplicate. The amount of pravastatin loaded was quantified by HPLC, as explained in “Drug quantification methods” section.
Resveratrol
Sterile MCLs (average mass 16.8 ± 1.86 mg, sterilized by steam heat at 121 °C, 20 min) were placed in tubes containing 7 mL of a resveratrol solution (0.1 mg/mL in ethanol:water 10:90 v/v) previously filtered (Filter-Lab® polyethersulphone (PES) syringe filter 0.22 μm; Barcelona, Spain). The loading solution was added to the tubes under sterile conditions in a biological safety cabinet. The tubes were maintained protected from light to avoid resveratrol degradation at 37 °C, 180 rpm for 72 h, after which the release tests were performed (n = 4). The amount of resveratrol loaded was quantified by HPLC, as described in “Drug quantification methods” section.
Eye blink model
The fabrication and assembly of the 3D eye model were similar to those reported in previous publications by some authors of this paper [15, 16], with minor changes (Fig. 2).
In vitro eye blink model (Ocublink) setup. The eyelid movement spreads the tear solution, which is supplied through the tubing that is attached to the eyelid support, over the eyeball, and the contact lens (fitted on the eyeball, shown in the close-up image). The out-flow solution is collected in the collection unit located below the eyeball
Eyeball and collection unit
The eyeball, lower eyelid, and collection unit were fabricated using a combination of 3D printing and moulding techniques, as previously described [31]. The components were printed using a hydrophobic UV-polymerizable resin on an SLA (stereolithography) 3D printer (Photon S; Anycubic, Shenzhen, China) and an FDM (fused deposition modelling) 3D printer (Prusa i3 MK3S + ; Prusa Prague, Czech Republic) to ensure water-sealed parts. All printing parameters were set to the manufacturer’s default settings. The eyeball was composed of two curvatures, 11.25 mm for the larger globe and 8.6 mm for the smaller globe containing the cornea, and 8.6 mm was chosen to match the most common base curve of CLs. Compared to previous models [16], the model used in the current study did not have any coatings for the front corneal surface but instead had a 300-µm groove at the center to allow for a CL to be mounted. In preliminary tests, it was found that the resin materials for the eyeball did not absorb pravastatin and resveratrol. The collection unit of the model was designed to allow the tear film to flow from the eyeball into the wells via gravity.
Eyelid
The eyelids were designed to have a curvature of 8.8 mm, which leaves a gap of approximately 200 µm between the eyeball and the eyelid. Once a contact lens was applied on the eyeball, this gap was reduced by the thickness of the lens (75–150 µm). The eyelid was designed to rotate around the smaller globe and flexes over the larger globe.
PVA eyelids were prepared by dissolving PVA (89–98 kDa, 20% w/v) in dimethyl sulfoxide:ultrapure water 80:20 v/v mixtures following a previously described protocol [16]. Briefly, the mixture was gently stirred for 5 min and heated at 120 °C for 2 h. After heating, the mixture was stirred again to ensure proper mixing of PVA. The obtained viscous solution was cast in 3D printed moulds (allowing for the preparation of four eyelids in the same mould) and then frozen at − 30 °C for 12 h. The resulting gels were thawed at room temperature for 1 h, removed from the moulds, and immersed in ultrapure water for 3 days, replacing the medium daily to remove the dimethyl sulfoxide used to prepare the PVA solution. After the washing process, the eyelids were immersed in ultrapure water to maintain the hydration of the eyelid until being used in the release experiments.
Flow rate and blinking
A commercial syringe pump (PHD ULTRA; Harvard Apparatus, Holliston, MA) was used to simulate the dynamic tear flow in the eye blink model. Simulated lachrymal fluid (SLF) or NaCl 0.9% was delivered through a hole at the top of the eyelid and spread over the eyeball surface/CL through blinking. In this study, the blink speed was set to 1 blink/10 s, and the flow rate was adjusted to 5 and 10 µL/min to ensure enough volume for sample collection at the predetermined time points. The blink velocity used in this model was 50 rpm or 45 mm/s for both closing and opening speeds; the average physiological speeds for closing and opening of the eyelid have been reported to be approximately 134 ± 4 and 26 ± 2 mm/s, respectively [32].
Temperature and humidity
The entire system was covered with an acrylic chamber to maintain stable humidity and temperature (20 ± 1.5 °C) during the experiment. Humidity levels were maintained close to approximately 80% using a humidifier and controlled through a hygrometer.
Release sampling
At predetermined time points (5, 15, 30 min, and every hour until 10 h), the out-flow solution was pipetted from the collection unit, stored in 300 or 600 µL Eppendorf® tubes, and frozen at − 30 °C until HPLC analysis. The amount of resveratrol and pravastatin released from the CLs was quantified by HPLC previous dilution of the samples in ethanol:water 50:50 v/v and SLF, respectively. All the experiments were carried out in quadruplicate.
Drug extraction from the eyelid and CLs
After 10 h of experimentation, each PVA eyelid was removed from the system, cut into small pieces, and immersed in 1 ml of SLF or 3 ml of ethanol:water 50:50 v/v for AECLs and MCLs. The eyelids were maintained at 37 °C and 180 rpm for at least 12 h to extract the amount of drug absorbed. The same procedure was applied for the CLs after 10 h on the eye model (without cutting) to determine the remaining amount of drug in the CLs at the end of the test.
Release in a vial
Sterilized pravastatin-loaded AECLs (n = 4) were rinsed with SLF to remove excess drug from the CL surface and immersed in 2 or 10 mL of SLF (pH = 7.4) to evaluate if the release volume could have an impact on the drug release profile. The in vitro release experiments were performed at 37 °C, under oscillatory movement (180 rpm), and at predefined time points, 150 µL was removed and replaced by the same volume of fresh medium. The amount of pravastatin released from the CLs was quantified by HPLC, as described in “Drug quantification methods” section.
Resveratrol-loaded MCLs (n = 4) were rinsed with NaCl 0.9% and placed into 15 mL Falcon® tubes filled with 6 mL of NaCl 0.9%. At each predetermined timepoint, aliquots of 200 μL were removed and replaced with the same volume of fresh medium. After 8 h of release, 6 mL of fresh NaCl 0.9% was added, increasing the total volume of release medium to 12 mL to avoid medium saturation. The amount of resveratrol released from the CLs was quantified by HPLC, as described in “Drug quantification methods” section.
Drug quantification methods
The amount of pravastatin and resveratrol loaded and released from the CLs was quantified by HPLC using previously developed methods [22, 23]. In vitro release studies in vials were quantified by JASCO HPLC (AS-4140 autosampler, PU-4180 pump, LC-NetII/ADC interface box, CO-4060 column oven, MD-4010 photodiode array detector; JASCO, Tokyo, Japan) operated with the ChromNAV software v.2. In vitro release experiments using the eye blink model were quantified by Waters HPLC (Autosampler Waters 2690, Photodiode Detector 2996; Milford, MA, USA), operated with the Empower2 software.
In the case of pravastatin, the mobile phase consisted of methanol:0.02 M sodium phosphate (NaH2PO4) buffer (50:50 v/v, pH adjusted to 7.0 with NaOH) at 1.00 mL/min and 25 °C. For pravastatin analysis, both HPLC equipments were fitted with a Waters Symmetry C18 column (5 µm, 3.9 × 150 mm). The injection volume was 80 µL, and the total run time of each sample was 10 min. Pravastatin was quantified at 238 nm (retention time 5.15 min). The HPLC method was validated using pravastatin solutions in simulated lachrymal fluid between 1 and 40 µg/mL.
For resveratrol, the analysis was carried out under isocratic elution using a mobile phase of methanol:water 50:50 v/v at a flow rate of 1 mL/min, 35 °C, and with 8 min of run time. The injection volume was 80 μL, and the UV detector was set at 305 nm. The retention time was 4.6 min. Both HPLC equipment were fitted with a Waters Symmetry C18 column (5 μm, 4.6 × 250 mm). Validation of the method was performed using a calibration curve of resveratrol in ethanol:water 50:50 v/v in the 0.05–6 μg/mL range.
Statistical analysis
Statistical analysis was performed using Statgraphics Centurion 18 v. 18.1.13 (Statgraphics Technologies, Inc., Warrenton, VA, USA). One-way analysis of variance (ANOVA) followed by multiple range test was carried out. The descriptive data were presented as mean ± standard deviation. In all cases, statistical significance was considered significant for a value of p < 0.05.
Results and discussion
Three-dimensional eye blink model
In this work, a 3D printed eye blink model was used to mimic some physiological ocular parameters, and in vivo comparisons were carried out. To mimic the tear fluid flow in the eye, fluid flow rates of 5 and 10 µL/min were chosen to ensure there was enough volume for sample collection at every predetermined time point. Preliminary trials carried out with flow rates closer to those reported for physiological tear flow values in humans (1.4–4.3 μL/min, [33]) or in rabbits (0.47–0.66 μL/min [34]) demonstrated that these rates were insufficient to maintain a reliable, constant flow rate of fluid on the eye model required for subsequent sample collections. It should be noted that the experiments with the eye blink model were carried out at room temperature as the system still lacks internal heating.
Pravastatin
The amount of pravastatin loaded by the AECLs was approximately 3.50 ± 0.84 mg/g of dried hydrogel. Pravastatin stability against HHP sterilization was previously verified, and the chosen conditions did not trigger degradation compared to non-sterilized pravastatin CLs, which showed that this method is compatible with the sterilization of pravastatin-loaded CLs [30].
Pravastatin release was investigated in vitro by recording in parallel the amount of pravastatin released when the AECLs were placed in the eye blink model and in test tubes (Fig. 3a). In the in vitro eye blink model, the pravastatin release profiles were more sustained, and the percentage of drug released after 10 h of the experiment was lower compared to in vitro vial release. Statistically significant differences were detected between the percentage of drug released in a vial filled with 2 and 10 mL and the eye blink model (flow rate of 5 and 10 µL/min) in the first 3 h of the experiment (ANOVA, p < 0.007). The influence of the flow rate in the eye blink model on the drug released was tested with two different flow rates (5 and 10 µL/min), and a slight decrease in the percentage of pravastatin released was observed with the flow rate of 5 µL/min compared to a flow rate of 10 µL/min, but no statistical differences were detected (ANOVA, p > 0.05).
After 10 h of experimentation on the eye blink model, the CLs and eyelids were immersed in SLF in order to measure the amount of pravastatin retained in the materials (Fig. 3b). A significantly higher amount of pravastatin was detected in the PVA eyelid at 5 µL/min compared to the flow rate of 10 µL/min (ANOVA, p < 0.001). However, no significant differences were detected in the amount of drug that remained in the CLs for the different flow rates (ANOVA, p = 0.72).
a Pravastatin release profiles from AECLs experimentally recorded in a vial filled with 2 or 10 mL of SLF over 10 h and using the eye blink model (flow rate of 5 and 10 µL/min) and b amount of pravastatin retained in the PVA eyelid and CLs after 10 h on the eye blink model (n = 4, mean values and standard deviations). * Statistically significant differences in the amount of pravastatin released in vitro in 2 and 10 mL and in the eye blink model (flow rate of 5 and 10 µL/min); ** statistically different between the amount of pravastatin retained in the model eyelid with the flow rate of 5 and 10 µL/min, p < 0.05
For the in vitro vial release, two different volumes were evaluated, 10 and 2 mL of SLF. No statistically significant differences were detected between pravastatin release profiles in 2 and 10 mL of SLF (ANOVA, p > 0.05). This minor effect of the volume on the percentage of pravastatin released may be explained by the free-water solubility of pravastatin (40 mg/mL, [35]); therefore, the volume decrease did not induce a false plateau or delayed the release.
The differences between the percentages of pravastatin released in the vial and in the eye blink model could be attributed to several reasons such as the release volume and the absorption of the drug by the eye model materials, among others. Firstly, in the in vitro vial system, the CLs were immediately immersed into vials containing a volume 33 times higher than the volume delivered in the eye model (300 and 600 µL/h). This increase in fluid volume could influence the concentration gradient between the inside of the CL and the release medium, promoting a faster release in the first hours of the release. Secondly, in theory, the CLs in the eye blink model were exposed to a total fluid of 3.0 and 6.0 mL of SLF after 10 h. However, the amounts of fluid collected were 2.23 ± 0.21 mL and 5.47 ± 0.65 mL (for a flow rate of 5 and 10 µL/min, respectively), corresponding to a fluid loss of 25 and 9%. This nonspecific fluid loss due to evaporation, absorption by the eyelid, or dead volume could also contribute to a decrease in the fluid that reached the CL and consequently a decrease in the volume available for drug release. Thirdly, a portion of pravastatin was absorbed by the PVA-eyelid over 10 h of experiment, 2.42 ± 0.26 µg at 5 µL/min and 0.88 ± 0.49 µg at 10 µL/min. As a result, the drug release was slower in the eye blink model, especially in the first few hours.
Resveratrol
For resveratrol release experiments, a two-step sterilization protocol was implemented as resveratrol may degrade at high temperature [36, 37]. The MCLs were sterilized by steam heat (121 °C, 20 min) in empty Falcon® tubes, and then the tubes were filled with a previous filtered resveratrol solution (0.1 mg/mL in ethanol:water 10:90 v/v). MCLs loaded, on average, approximately 13.20 ± 0.90 mg of resveratrol per g of dried hydrogel after being immersed in the drug solution for 72 h.
In the in vitro vial conditions, the MCLs released 54.43 ± 7.29% resveratrol in the first 10 h (Fig. 4a). As to what happened with pravastatin, the amount of resveratrol released in the eye blink model was significantly lower: 0.37 ± 0.22% at 5 µL/min and 0.47 ± 0.26% at 10 µL/min (ANOVA p < 0.001) than the amount released in the vial. The difference between the vial results and eye blink model might be related to the diffusion resistance associated with the hydrophobic nature of resveratrol [38] since resveratrol solubility in NaCl 0.9% was quantified to be approximately 27.4 μg/mL [23]. In the case of the vial tests, the volume of the release medium was increased up to 12 mL to avoid medium saturation and false plateaus.
a Resveratrol release profiles from MCLs experimentally recorded in a vial filled with 6 mL of NaCl 0.9% over 10 h and on the eye blink model (flow rate of 5 and 10 µL/min) and b amount of resveratrol retained in the PVA eyelid and CLs after 10 h on the eye blink model (n = 4, mean values and standard deviations). * Statistically different between the amount of resveratrol retained in the model eyelid with the flow rate of 5 and 10 µL/min, p < 0.05
The amount of resveratrol absorbed by the PVA eyelid was about tenfold higher compared to pravastatin, showing a higher affinity between resveratrol and the PVA eyelid (Fig. 4b). This higher affinity could also contribute to the decrease in resveratrol detected in the fluid collected from the eye blink model. The higher fluid flow rate (10 µL/min) induced a higher amount of resveratrol absorbed by the eyelid (ANOVA, p < 0.001). As a consequence of the slow release from the MCLs, the amount of resveratrol remaining in the CLs after 10 h of the release tests was approximately 40% of the drug loaded (91.29 ± 13.85 µg for 5 µL/min and 71.37 ± 8.77 µg for 10 µL/min). No statistical differences were detected between both flow rates (ANOVA, p = 0.10).
In vivo release eye blink model comparisons
The release profiles from the eye blink model for both pravastatin and resveratrol (concentration versus time) obtained were also compared to the in vivo rabbit data already reported for these same CLs [22, 29]. Briefly, six healthy male New Zealand white rabbits were selected for the in vivo release studies wearing drug-loaded CLs. Drug-loaded CLs were removed from the loading solutions, rinsed with sterile saline solution for CLs, and carefully placed on the rabbits’ right eye below the nictitating membrane and without local anesthesia. Samples of the tear fluid were collected using Schirmer test strips before and after CL wearing (t = 5, 15, 30 min, and every hour until 8 or 10 h). The drug concentration in the tear fluid was quantified by immersing the Schirmer strips in SLF or ethanol:water (50:50 v/v), and the resulting solutions were quantified by HPLC [22, 29].
Pravastatin
Pravastatin release profiles from the AECLs during the in vivo experiment and in the eye blink model for both flow rates are compared in Fig. 5. The maximum concentration for both experiments was obtained after 30 min of CL application. Pravastatin maximum levels were 177.5 ± 116.8 μg/mL for in vivo and 28.39 ± 3.00 μg/mL and 39.13 ± 20.48 μg/mL for the eye blink model with a flow rate of 5 μL/min and 10 μL/min, respectively. The peak of maximum concentration was followed by a smooth decrease in drug concentration in the tear fluid and in the fluid collected from the eye blink model. No burst release was observed.
a In vivo tear fluid levels of pravastatin were recorded during wear of pravastatin-loaded AECLs for 8 and 10 h (n = 6 for 8 h and n = 3 for 9 and 10 h), data taken from Pereira-da-Mota et al. [22]. b Normalized released pravastatin concentration in SLF from pravastatin-loaded AECLs over 10 h on the eye model (flow rate of 5 and 10 µL/min) (n = 4, mean values and standard deviations)
Despite the similar release patterns, the amount of pravastatin released from the CLs in the eye blink model was about fivefold lower than that recorded in the in vivo studies (ANOVA, p < 0.05). This finding might be related to several factors: (i) the drug absorption into the PVA eyelid in the model, (ii) the composition of the release medium, (iii) the temperature, and (iv) the complexity of the eyeball piece. Firstly, the PVA eyelid absorbed approximately 2.42 ± 0.26 µg pravastatin when tested under 5 µL/min and 0.89 ± 0.49 µg for 10 µL/min. Secondly, the physiological tear fluid contains proteins, lipids, and mucin that can promote drug release from the CLs [39]. In previous studies, the influence of BSA and lysozyme on pravastatin release rate from CLs was evaluated, and an increase in the amount of pravastatin released was observed with the incorporation of both proteins in 2 mL of SLF [22]. The effect of proteins, lipids, and other components of the tear fluid on the release kinetics from CLs is an important aspect to take into account in further studies. Thirdly, in this work, a stable room temperature of 20 ± 1.5 °C was maintained during the release experiments in the eye model, but an increase in temperature from 20 to 34 °C was previously shown to enhance 20% of the fractional mass released from pHEMA hydrogels after 48 h in vitro in vials [40, 41]. This phenomenon could be related to higher kinetic energy of the drug molecules when the temperature increases, leading to faster diffusional transport [42]. The effect of temperature on pravastatin solubility could also contribute to a higher amount of drug released from the CLs in vivo [43]. Fourthly, another limitation that could compromise the release from CLs in the eye blink model pertains to the composition of the eyeball piece. In the present study, the eyeball piece was printed with a hydrophobic UV-polymerizable resin, which does not represent corneal surface properties. Ninety percent of the cornea consists of the stroma, which contains a high percentage of water and consists of collagen fibril lamellae oriented parallel to each other, which is more comparable to a hydrophilic hydrogel. In in vivo conditions, corneal osmosis adds water to the post-lens tear film (the tear film between the back surface of the CL and the corneal epithelium), diluting the concentration of the drug in the post-lens tear film, which could increase the drug release from the drug-loaded CL.
Comparing the release profiles from the different flow rates in the eye blink model, a slightly faster release was observed for the flow rate of 10 µL/min, achieving a higher maximum concentration at 30 min, followed by a decrease in the concentration of drug present in the fluid collected (ANOVA, p > 0.05).
Correlations for in vivo-in vitro in the eye blink model or in vitro–in vitro (in a vial versus eye blink model) were investigated using Levy plots (Fig. 6). Release tests in the eye blink model with a flow rate of 10 µL/min led to a correlation coefficient (r2) closer to 1 (0.993) compared to the Levy plot obtained for 5 µL/min (Fig. 6a). The intercepts at the origin were + 6.25 and + 1.93; the slopes were 1.83 and 1.62 for the flow rate of 5 and 10 µL/min, respectively. Thus, a stronger correlation was observed with the 10 µL/min flow rate that favored the in vivo-in vitro correlations. Also, a higher correlation coefficient was obtained for the Levy plot comparing the in vitro tests in a vial (2 and 10 mL) and eye blink model with the flow rate of 10 µL/min (Fig. 6b).
Levy plots for in vivo (a) or in vitro (b) vs. eye blink model percentage of pravastatin released. The eye blink model experiments were carried out with 5 and 10 µL/min of flow rate (eye blink model 5/model 5 and eye blink model 10/model 10, respectively). The in vitro tests in a vial were carried out in 2 and 10 mL of SLF
Resveratrol
Resveratrol-loaded CLs presented a sustained release in the eye blink model similar to what occurred in vivo (Fig. 7). However, the concentration of resveratrol detected in the fluid collected in the eye blink model was approximately 150-fold lower than in vivo (ANOVA, p < 0.001), likely associated with several factors that also conditioned the release of the hydrophilic statin in the eye blink model, plus the low solubility of resveratrol in an aqueous medium, as previously mentioned. No statistical differences were detected between the two different flow rates (ANOVA, p > 0.05).
a In vivo tear fluid levels of resveratrol were recorded during wear of resveratrol-loaded MCLs for 8 and 10 h (n = 6 for 8 h and n = 3 for 9 and 10 h), data taken from Vivero-Lopez et al. [29]. b Normalized resveratrol released concentrations in NaCl 0.9% from resveratrol-loaded MCLs over 10 h on the eye model (flow rate of 5 and 10 µL/min) (n = 4, mean values and standard deviations)
For resveratrol experiments, plots of in vivo release versus in vitro release in the eye blink model presented slopes that were remarkably high: 333.96 and 245.16 for the flow rate of 5 and 10 µL/min, respectively (Fig. 8), which supported that the percentage of resveratrol released in vivo was significantly higher than that recorded in the eye blink model. In comparison, no differences were obtained for in vitro vial release and the eye blink model. This finding highlights the difficulties in developing in vitro release models that can predict the in vivo performance of CLs loaded with hydrophobic drugs, which represent about 40% of current pharmaceutical treatments [44].
Conclusions
In the current study, the usefulness of the developed 3D printed eye blink model for the evaluation of drug release profiles of medicated CLs has been explored in detail. To our knowledge, this was one of the first studies that have attempted to correlate the release of drugs from lenses from an in vivo rabbit study with a blink model. It may serve as an important starting point to understand areas that need to be further developed and investigated to create better simulations. There are numerous factors in the eye that can affect drug release kinetics, and understanding the contribution/effect of each factor individually to drug release kinetics is not obvious. For instance, in this study, increasing the flow rate by 2 times was expected to increase the drug release rate by 2 times. However, this was not the case: increasing the flow by 2 times only resulted in a marginal increase in the amounts of drugs released, which was not obvious. The release profile of both drugs was more sustained and lower in the in vitro eye blink model compared to the in vitro release in vials, especially for the hydrophobic drug resveratrol. Both drug-loaded CLs showed similar release patterns in the eye blink model as in in vivo studies. However, the amount of drug released in the eye blink model was significantly lower compared to previously obtained in vivo data. More linear Levy plots were recorded for pravastatin release in the eye model (flow rate of 10 µL/min) and in vivo data. The information gathered in the present study may serve to gain an insight into relevant physiological parameters that influence the in vivo release from CLs, such as the composition of the tear fluid, tear flow rates, temperature of the system, and composition of the eyeball surface. The obtained results may serve as a guide for further improvements of the 3D printed eye blink model.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Wichterle O. U.S. Patents. 3,660,545; 3,408,429; 3,496,254; 3,499,862.
https://www.jjvision.com/press-release/johnson-johnson-vision-care-receives-fda-approval-acuvuer-theravisiontm-ketotifen. Accessed Oct 2022.
Lanier OL, Christopher KG, Macoon RM, Yu Y, Sekar P, Chauhan A. Commercialization challenges for drug eluting contact lenses. Expert Opin Drug Deliv. 2020;17:1133–49. https://doi.org/10.1080/17425247.2020.1787983.
https://www.reviewofcontactlenses.com/article/material-gains-50-years-of-the-soft-contact-lens. Accessed Oct 2022.
Jones L, Hui A, Phan CM, Read ML, Azar D, Buch J, Ciolino JB, Naroo SA, Pall B, Romond K, Sankaridurg P, Schnider CM, Terry L, Willcox M. CLEAR - contact lens technologies of the future. Cont Lens Anterior Eye. 2021;44:398–430. https://doi.org/10.1016/j.clae.2021.02.007.
Minami T, Ishida W, Kishimoto T, Nakajima I, Hino S, et al. In vitro and in vivo performance of epinastine hydrochloride-releasing contact lenses. PLoS ONE. 2019;14: e0210362. https://doi.org/10.1371/journal.pone.0210362.
Sekar P, Chauhan A. Effect of vitamin-E integration on delivery of prostaglandin analogs from therapeutic lenses. J ColloidInterfaceSci. 2019;539:457–67. https://doi.org/10.1016/j.jcis.2018.12.036.
Alvarez-Lorenzo C, Anguiano-Igea S, Varela-Garcia A, Vivero-Lopez M, Concheiro A. Bioinspired hydrogels for drug-eluting contact lenses. Acta Biomater. 2019;84:49–62. https://doi.org/10.1016/j.actbio.2018.11.020.
DiPasquale SA, Wuchte LD, Mosley RJ, Demarest RM, Voyles ML, Byrne ME. One week sustained in vivo therapeutic release and safety of novel extended-wear silicone hydrogel contact lenses. Adv Healthc Mater. 2022;11(7): e2101263. https://doi.org/10.1002/adhm.202101263.
Hui A, Willcox M. In vivo studies evaluating the use of contact lenses for drug delivery. Optom Vis Sci. 2016;93(4):367–76. https://doi.org/10.1097/OPX.0000000000000809.
Pereira-da-Mota AF, Phan CM, Concheiro A, Jones L, Alvarez-Lorenzo C. Testing drug release from medicated contact lenses: the missing link to predict in vivo performance. J Control Release. 2022;343:672–702. https://doi.org/10.1016/j.jconrel.2022.02.014.
Minami T, Ishida W, Kishimoto T, Nakajima I, Hino S, Arai R, Matsunaga T, Fukushima A, Yamagami S. In vitro and in vivo performance of epinastine hydrochloride-releasing contact lenses. PLoS ONE. 2019;14(1): e0210362. https://doi.org/10.1371/journal.pone.0210362.
Tieppo A, Pate KM, Byrne ME. In vitro controlled release of an anti-inflammatory from daily disposable therapeutic contact lenses under physiological ocular tear flow. Eur J Pharm Biopharm. 2012;81(1):170–7. https://doi.org/10.1016/j.ejpb.2012.01.015.
Pimenta AF, Valente A, Pereira JM, Pereira JC, Filipe HP, Mata JL, Colaço R, Saramago B, Serro AP. Simulation of the hydrodynamic conditions of the eye to better reproduce the drug release from hydrogel contact lenses: experiments and modeling. Drug Deliv Transl Res. 2016;6(6):755–62. https://doi.org/10.1007/s13346-016-0303-1.
Phan CM, Walther H, Qiao H, Shinde R, Jones L. Development of an eye model with a physiological blink mechanism. Trans Vis Sci Tech. 2019;8(5):1. https://doi.org/10.1167/tvst.8.5.1.
Phan CM, Shukla M, Walther H, Heynen M, Suh D, Jones L. Development of an in vitro blink model for ophthalmic drug delivery. Pharmaceutics. 2021;13(3):300. https://doi.org/10.3390/pharmaceutics13030300.
Phan CM, Walther H, Smith RW, Riederer D, Lau C, Osborn Lorenz K, Subbaraman LN, Jones L. Determination of the release of PEG and HPMC from nelfilcon A daily disposable contact lenses using a novel in vitro eye model. J Biomater Sci Polym Ed. 2018;29(17):2124–36. https://doi.org/10.1080/09205063.2018.1514192.
Phan CM, Bajgrowicz-Cieslak M, Subbaraman LN, Jones L. Release of moxifloxacin from contact lenses using an in vitro eye model: impact of artificial tear fluid composition and mechanical rubbing. Transl Vis Sci Technol. 2016;5(6):3. https://doi.org/10.1167/tvst.5.6.3.
Phan CM, Bajgrowicz M, Gao H, Subbaraman LN, Jones LW. Release of fluconazole from contact lenses using a novel in vitro eye model. Optom Vis Sci. 2016;93(4):387–94. https://doi.org/10.1097/OPX.0000000000000760.
Murphy C, Deplazes E, Cranfield CG, Garcia A. The role of structure and biophysical properties in the pleiotropic effects of statins. Int J Mol Sci. 2020;21(22):8745. https://doi.org/10.3390/ijms21228745.
Yang SC, Tseng CH, Wang PW, Lu PL, Weng YH, Yen FL, Fang JY. Pterostilbene, a methoxylated resveratrol derivative, efficiently eradicates planktonic, biofilm, and intracellular MRSA by topical application. Front Microbiol. 2017;8:1103. https://doi.org/10.3389/fmicb.2017.01103.
Pereira-da-Mota AF, Vivero-Lopez M, Serramito M, Diaz-Gomez L, Serro AP, Carracedo G, Huete-Toral `F, Concheiro A, Alvarez-Lorenzo C. Contact lenses for pravastatin delivery to eye segments: design and in vitro-in vivo correlations. J Control Release. 2022;348:431–43. https://doi.org/10.1016/j.jconrel.2022.06.001.
Vivero-Lopez M, Muras A, Silva D, Serro AP, Otero A, Concheiro A, Alvarez-Lorenzo C. Resveratrol-loaded hydrogel contact lenses with antioxidant and antibiofilm performance. Pharmaceutics. 2021;13(4):532. https://doi.org/10.3390/pharmaceutics13040532.
Ooi KG, Khoo P, Vaclavik V, Watson SL. Statins in ophthalmology. SurvOphthalmol. 2019;64(3):401–32. https://doi.org/10.1016/j.survophthal.2019.01.013.
Gupta A, Gupta V, Thapar S, Bhansali A. Lipid-lowering drug atorvastatin as an adjunct in the management of diabetic macular edema. Am J Ophthalmol. 2004;137(4):675–82. https://doi.org/10.1016/j.ajo.2003.11.017.
Ozkiris A, Erkiliç K, Koç A, Mistik S. Effect of atorvastatin on ocular blood flow velocities in patients with diabetic retinopathy. Br J Ophthalmol. 2007;91(1):69–73. https://doi.org/10.1136/bjo.2006.098285.
Nielsen SF, Nordestgaard BG. Statin use before diabetes diagnosis and risk of microvascular disease: a nationwide nested matched study. Lancet Diabetes Endocrinol. 2014;2(11):894–900. https://doi.org/10.1016/S2213-8587(14)70173-1.
Tsai TY, Chen TC, Wang IJ, Yeh CY, Su MJ, Chen RH, Tsai TH, Hu FR. The effect of resveratrol on protecting corneal epithelial cells from cytotoxicity caused by moxifloxacin and benzalkonium chloride. Invest Ophthalmol Vis Sci. 2015;56(3):1575–84. https://doi.org/10.1167/iovs.14-15708.
Vivero-Lopez M, Pereira-da-Mota AF, Carracedo G, Huete-Toral F, Parga A, Otero A, Concheiro A, Alvarez-Lorenzo C. Phosphorylcholine-based contact lenses for sustained release of resveratrol: design, antioxidant and antimicrobial performances, and in vivo behavior. ACS Appl Mater Interf. 2022. https://doi.org/10.1021/acsami.2c18217
Pereira-da-Mota AF, Vivero-Lopez M, Topete A, Serro AP, Concheiro A, Alvarez-Lorenzo C. Atorvastatin-eluting contact lenses: effects of molecular imprinting and sterilization on drug loading and release. Pharmaceutics. 2021;13(5):606. https://doi.org/10.3390/pharmaceutics13050606.
Phan CM, Walther H, Gao H, Rossy J, Subbaraman LN, Jones L. Development of an in vitro ocular platform to test contact lenses. J Vis Exp. 2016;6(110):e53907. https://doi.org/10.3791/53907.
Kwon KA, Shipley RJ, Edirisinghe M, Ezra DG, Rose G, Best SM, Cameron RE. High-speed camera characterization of voluntary eye blinking kinematics. J R Soc Interface. 2013;10(85):20130227. https://doi.org/10.1098/rsif.2013.0227.
Glasson MJ, Stapleton F, Keay L, Willcox MD. The effect of short term contact lens wear on the tear film and ocular surface characteristics of tolerant and intolerant wearers. Cont Lens Anterior Eye. 2006;29(1):41–7. https://doi.org/10.1016/j.clae.2005.12.006.
Chrai SS, Patton TF, Mehta A, Robinson JR. Lacrimal and instilled fluid dynamics in rabbit eyes. J Pharm Sci. 1973;62(7):1112–21. https://doi.org/10.1002/jps.2600620712.
European Directorate for the Quality of Medicines & HealthCare. European Pharmacopeia. 6th ed. Council of Europe. 2008.
Zupančič Š, Lavrič Z, Kristl J. Stability and solubility of trans-resveratrol are strongly influenced by pH and temperature. Eur J Pharm Biopharm. 2015;93:196–204. https://doi.org/10.1016/j.ejpb.2015.04.002.
Silva RCD, Teixeira JA, Nunes WDG, Zangaro GAC, Pivatto M, Caires FJ, Ionashiro M. Resveratrol: a thermoanalytical study. Food Chem. 2017;237:561–5. https://doi.org/10.1016/j.foodchem.2017.05.146.
Salehi B, Mishra AP, Nigam M, Sener B, Kilic M, Sharifi-Rad M, Fokou PVT, Martins N, Sharifi-Rad J. Resveratrol: a double-edged sword in health benefits. Biomedicines. 2018;6(3):91. https://doi.org/10.3390/biomedicines6030091.
Mahomed A, Wolffsohn JS, Tighe BJ. Structural design of contact lens-based drug delivery systems; in vitro and in vivo studies of ocular triggering mechanisms. Cont Lens Anterior Eye. 2016;39(2):97–105. https://doi.org/10.1016/j.clae.2015.07.007.
Tieppo A, Boggs AC, Pourjavad P, Byrne ME. Analysis of release kinetics of ocular therapeutics from drug releasing contact lenses: best methods and practices to advance the field. Cont Lens Anterior Eye. 2014;37(4):305–13. https://doi.org/10.1016/j.clae.2014.04.005.
Miyazaki S, Suzuki S, Kawasaki N, Endo K, Takahashi A, Attwood D. In situ gelling xyloglucan formulations for sustained release ocular delivery of pilocarpine hydrochloride. Int J Pharm. 2001;229(1–2):29–36. https://doi.org/10.1016/s0378-5173(01)00825-0.
Ferreira JA, Oliveira P, Silveira E. Drug release enhanced by temperature: an accurate discrete model for solutions in H3. Comput Math Appl. 2020;79(3):852–75. https://doi.org/10.1016/j.camwa.2019.08.002.
Jia C, Yin Q, Song J, Hou G, Zhang M. Solubility of pravastatin sodium in water, methanol, ethanol, 2-propanol, 1-propanol, and 1-butanol from (278 to 333) K. J Chem Eng Data. 2008;53(10):2466–8. https://doi.org/10.1021/je800196k.
Torres-Luna C, Fan X, Domszy R, Hu N, Wang NS, Yang A. Hydrogel-based ocular drug delivery systems for hydrophobic drugs. Eur J Pharm Sci. 2020;154: 105503. https://doi.org/10.1016/j.ejps.2020.105503.
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. This project was funded by the European Union’s Horizon 2020 research and innovation programme under the Marie Skłodowska-Curie Actions grant agreement N° 813440 (ORBITAL–Ocular Research by Integrated Training And Learning). The work was also partially supported by MCIN [PID 2020-113881RB-I00/AEI/10.13039/501100011033], Spain, Xunta de Galicia [ED431C 2020/17], FEDER, and the Hong Kong Special Administrative Region Government and InnoHK. M. Vivero-Lopez acknowledges Xunta de Galicia (Consellería de Cultura, Educación e Ordenación Universitaria) for a predoctoral research fellowship [ED481A-2019/120]. P. Garg acknowledges the support of the Collaborative Research and Training Experience (CREATE) Program awarded by the Natural Sciences and Engineering Research Council of Canada (NSERC).
Author information
Authors and Affiliations
Contributions
All the authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Ana F. Pereira-da-Mota, Maria Vivero-Lopez, Piyush Garg, and Chau-Minh Phan. The first draft of the manuscript was written by Ana F. Pereira-da-Mota, and all the authors commented on previous versions of the manuscript. All the authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors have no relevant financial or non-financial interests to disclose. Author Lyndon Jones has served on advisory boards for Alcon, CooperVision, Johnson and Johnson Vision, Menicon, Ophtecs, and Visioneering.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pereira-da-Mota, A.F., Vivero-Lopez, M., Garg, P. et al. In vitro–in vivo correlation of drug release profiles from medicated contact lenses using an in vitro eye blink model. Drug Deliv. and Transl. Res. 13, 1116–1127 (2023). https://doi.org/10.1007/s13346-022-01276-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13346-022-01276-6