Abstract
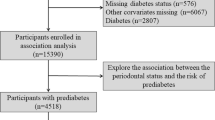
Periodontal disease often develops in patients with diabetes, and further exacerbated with diabetic complications. It would be clinically important to clarify the relationship between diabetic microvascular diseases and periodontal disease. This study aimed to evaluate the association between periodontal disease and diabetic complications in patients with type 2 diabetes with poor glycemic control. A total of 447 patients with type 2 diabetes hospitalized at Rakuwakai Otowa Hospital, Japan, were initially recruited in this study. After excluding 134 patients who lacked clinical data or were edentulous, 312 were included in our study. The severity of periodontal disease was evaluated based on the average bone resorption rate. Patients with diabetic nephropathy developed severe periodontal disease (multivariate-adjusted odds ratio, 3.00 [95% CI 1.41–5.19]). Diabetic neuropathy was positively associated with the severity of periodontal disease; the multivariate-adjusted odds ratio (95% CI) was 1.62 (0.87‒2.99) for moderate and 4.26 (2.21‒8.20) for severe periodontal disease. In contrast, diabetic retinopathy was linked with moderate periodontal disease (multivariate-adjusted odds ratio 2.23 [95% CI 1.10–4.10]), but not with severe conditions (multivariate-adjusted odds ratio 0.92 [95% CI 0.67–3.07]). In conclusion, periodontal disease, evaluated by average bone resorption rate, was associated with diabetic nephropathy and neuropathy.

Similar content being viewed by others
References
Taylor GW, Burt BA, Becker MP, Genco RJ, Shlossman M, Knowler WC, et al. Severe periodontitis and risk for poor glycemic control in patients with non-insulin-dependent diabetes mellitus. J Periodontol. 1996;67:1085–93. https://doi.org/10.1902/jop.1996.67.10s.1085.
Demmer RT, Jacobs DR Jr, Desvarieux M. Periodontal disease and incident type 2 diabetes: results from the First National Health and Nutrition Examination Survey and its epidemiologic follow-up study. Diabetes Care. 2008;31:1373–9. https://doi.org/10.2337/dc08-0026.
Costa FO, Miranda Cota LO, Pereira Lages EJ, Soares Dutra Oliveira AM, Dutra Oliveira PA, Cyrino RM, et al. Progression of periodontitis and tooth loss associated with glycemic control in individuals undergoing periodontal maintenance therapy: a 5-year follow-up study. J Periodontol. 2013;84:595–605. https://doi.org/10.1902/jop.2012.120255.
Nelson RG, Shlossman M, Budding LM, Pettitt DJ, Saad MF, Genco RJ, et al. Periodontal disease and NIDDM in Pima Indians. Diabetes Care. 1990;13:836–40. https://doi.org/10.2337/diacare.13.8.836.
Tsai C, Hayes C, Taylor GW. Glycemic control of type 2 diabetes and severe periodontal disease in the US adult population. Community Dent Oral Epidemiol. 2002;30:182–92. https://doi.org/10.1034/j.1600-0528.2002.300304.x.
Löe H. Periodontal disease. The sixth complication of diabetes mellitus. Diabetes Care. 1993;16(329):34. https://doi.org/10.2337/diacare.16.1.329.
Koh GC, Peacock SJ, van der Poll T, Wiersinga WJ. The impact of diabetes on the pathogenesis of sepsis. Eur J Clin Microbiol Infect Dis. 2012;31:379–88. https://doi.org/10.1007/s10096-011-1337-4.
Jafar N, Edriss H, Nugent K. The effect of short-term hyperglycemia on the innate immune system. Am J Med Sci. 2016;351:201–11. https://doi.org/10.1016/j.amjms.2015.11.011.
Lalla E, Papapanou PN. Diabetes mellitus and periodontitis: a tale of two common interrelated diseases. Nat Rev Endocrinol. 2011;7:738–48. https://doi.org/10.1038/nrendo.2011.106.
Demmer RT, Squillaro A, Papapanou PN, Rosenbaum M, Friedewald WT, Jacobs DR Jr, et al. Periodontal infection, systemic inflammation, and insulin resistance: results from the continuous National Health and Nutrition Examination Survey (NHANES) 1999–2004. Diabetes Care. 2012;35:2235–42. https://doi.org/10.2337/dc12-0072.
Katagiri S, Nitta H, Nagasawa T, Izumi Y, Kanazawa M, Matsuo A, et al. Effect of glycemic control on periodontitis in type 2 diabetic patients with periodontal disease. J Diabetes Investig. 2013;4:320–5. https://doi.org/10.1111/jdi.12026.
Munenaga Y, Hiroshima Study Group, Yamashina T, Tanaka J, Nishimura F. Improvement of glycated hemoglobin in Japanese subjects with type 2 diabetes by resolution of periodontal inflammation using adjunct topical antibiotics: results from the Hiroshima Study. Diabetes Res Clin Pract. 2013;100:53–60. https://doi.org/10.1016/j.diabres.2013.01.028.
Sun WL, Chen LL, Zhang SZ, Wu YM, Ren YZ, Qin GM. Inflammatory cytokines, adiponectin, insulin resistance and metabolic control after periodontal intervention in patients with type 2 diabetes and chronic periodontitis. Intern Med. 2011;50:1569–74. https://doi.org/10.2169/internalmedicine.50.5166.
Engebretson SP, Hyman LG, Michalowicz BS, Schoenfeld ER, Gelato MC, Hou W, et al. The effect of nonsurgical periodontal therapy on hemoglobin A1c levels in persons with type 2 diabetes and chronic periodontitis: a randomized clinical trial. JAMA. 2013;310:2523–32. https://doi.org/10.1001/jama.2013.282431.
Chen L, Luo G, Xuan D, Wei B, Liu F, Li J, et al. Effects of non-surgical periodontal treatment on clinical response, serum inflammatory parameters, and metabolic control in patients with type 2 diabetes: a randomized study. J Periodontol. 2012;83:435–43. https://doi.org/10.1902/jop.2011.110327.
Nishimura F, Yamazaki K, Nomura Y, Minabe M, Miyata T, Morita M. Report from periodontal medicine committee (in Japanese). J Jpn Assoc Periodontol. 2011;53:197–200. https://doi.org/10.2329/perio.53.197.
Friedewald VE, Kornman KS, Beck JD, Genco R, Goldfine A, Libby P, et al. The American Journal of Cardiology and Journal of Periodontology Editors’ Consensus: periodontitis and atherosclerotic cardiovascular disease. Am J Cardiol. 2009;104:59–68. https://doi.org/10.1016/j.amjcard.2009.05.002.
Schei O, Waerhaug J, Lovdal A, Arno A. Alveolar bone loss as related to oral hygiene and age. J Periodontol. 1959;30:7–16. https://doi.org/10.1902/jop.1959.30.1.7.
Nakarai H, Yamashita A, Takagi M, Adachi M, Sugiyama M, Noda H, et al. Periodontal disease and hypertriglyceridemia in Japanese subjects: potential association with enhanced lipolysis. Metabolism. 2011;60:823–9. https://doi.org/10.1016/j.metabol.2010.07.034.
Nakajima T, Honda T, Domon H, Okui T, Kajita K, Ito H, et al. Periodontitis-associated up-regulation of systemic inflammatory mediator level may increase the risk of coronary heart disease. J Periodontal Res. 2010;45:116–22. https://doi.org/10.1111/j.1600-0765.2009.01209.x.
Haneda M, Utsunomiya K, Koya D, Babazono T, Moriya T, Makino H, et al. Classification of diabetic Nephropathy 2014. Nihon Jinzo Gakkai Shi. 2014;56:547–52.
Sadzeviciene R, Paipaliene P, Zekonis G, Zilinskas J. The influence of microvascular complications caused by diabetes mellitus on the inflammatory pathology of periodontal tissues. Stomatologija. 2005;7:121–4.
Nitta H, Katagiri S, Nagasawa T, Izumi Y, Ishikawa I, Izumiyama H, et al. The number of microvascular complications is associated with an increased risk for severity of periodontitis in type 2 diabetes patients: results of a multicenter hospital-based cross-sectional study. J Diabetes Investig. 2017;8:677–86. https://doi.org/10.1111/jdi.12633.
Honda T, Domon H, Okui T, Kajita K, Amanuma R, Yamazaki K. Balance of inflammatory response in stable gingivitis and progressive periodontitis lesions. Clin Exp Immunol. 2006;144:35–40. https://doi.org/10.1111/j.1365-2249.2006.03028.x.
Eitner F, Westerhuis R, Burg M, Weinhold B, Gröne HJ, Ostendorf T, et al. Role of interleukin-6 in mediating mesangial cell proliferation and matrix production in vivo. Kidney Int. 1997;51:69–78. https://doi.org/10.1038/ki.1997.9.
Sawa Y, Takata S, Hatakeyama Y, Ishikawa H, Tsuruga E. Expression of toll-like receptor 2 in glomerular endothelial cells and promotion of diabetic nephropathy by Porphyromonas gingivalis lipopolysaccharide. PLoS One. 2014;9: e97165. https://doi.org/10.1371/journal.pone.0097165.
Alvarenga MOP, Miranda GHN, Ferreira RO, Saito MT, Fagundes NCF, Maia LC, et al. Association between diabetic retinopathy and periodontitis—a systematic review. Front Public Health. 2020;8: 550614. https://doi.org/10.3389/fpubh.2020.550614.
Wu HQ, Wei X, Yao JY, Qi JY, Xie HM, Sang AM, et al. Association between retinopathy, nephropathy, and periodontitis in type 2 diabetic patients: a meta-analysis. Int J Ophthalmol. 2021;14:141–7. https://doi.org/10.18240/ijo.2021.01.20.
Acknowledgements
We would like to thank Editage (http://www.editage.com) for English language editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflict interest associated with this manuscript.
Human rights statement and informed consent
This study was conducted with the Ethics Review Committee of Rakuwakai Otowa Hospital (The approval number 17-014), which was approved on Apr. 27. 2017, and the Ethics Committee of Okayama University (The approval number 1706-041), which was approved on June.16, 2017. Written informed consent was waived due to its retrospective nature. An opt-out procedure was conducted to allow patients to withdraw from the study by informing them of the study protocol on the hospital homepage website, as advised by the committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Sugi, N., Eguchi, E., Tsuboi, A. et al. Periodontal diseases assessed by average bone resorption are associated with microvascular complications in patients with type 2 diabetes. Diabetol Int 14, 32–39 (2023). https://doi.org/10.1007/s13340-022-00591-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13340-022-00591-0