Abstract
Background and Objectives
Current anticoagulants pose an increased risk of bleeding. The development of drugs targeting factor XIa, like asundexian, may provide a safer treatment option. A human mass‑balance study was conducted to gain a deeper understanding of the absorption, distribution, metabolism, excretion, and potential for drug–drug interaction of asundexian. Additionally, an overview of the biotransformation and clearance pathways for asundexian in humans and bile-duct cannulated (BDC) rats in vivo, as well as in vitro in hepatocytes of both species, is reported.
Methods
The mass balance, biotransformation, and excretion pathways of asundexian were investigated in six healthy volunteers (single oral dose of 25 mg [14C]asundexian) and in BDC rats (intravenous [14C]asundexian 1 mg/kg).
Results
Overall recovery of radioactivity was 101% for humans (samples collected up to 14 days after dosing), and 97.9% for BDC rats (samples collected in the 24 h after dosing). Radioactivity was mainly excreted into feces in humans (80.3%) and into bile/feces in BDC rats (> 94%). The predominant clearance pathways in humans were amide hydrolysis to metabolite M1 (47%) and non-labeled M9 with subsequent N-acetylation to M10; oxidative biotransformation was a minor pathway (13%). In rats, hydrolysis of the terminal amide to M2 was the predominant pathway. In human plasma, asundexian accounted for 61.0% of total drug-related area under the plasma concentration–time curve (AUC); M10 was the major metabolite (16.4% of the total drug-related AUC). Excretion of unmetabolized drug was a significant clearance pathway in both species (human, ~ 37%; BDC rat, ~ 24%). The near-complete bioavailability of asundexian suggests negligible limitations on absorption and first-pass metabolism. Comparison with radiochromatograms from incubations with human or rat hepatocytes indicated consistency across species and a good overall in vitro/in vivo correlation.
Conclusions
Similar to preclinical experiments, total asundexian-derived radioactivity is cleared quantitatively predominantly via feces. Excretion occurs mainly via amide hydrolysis and as the unchanged drug.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Asundexian, an oral factor XIa inhibitor currently under clinical development for prevention of stroke and systemic embolism in patients with atrial fibrillation (AF) at risk of stroke and for prevention of recurrent symptomatic ischemic stroke in patients following an acute non-cardioembolic ischemic stroke or high-risk ischemic attack, is predominantly excreted via feces. |
Amide hydrolysis of the parent compound and excretion of unmetabolized asundexian are the main elimination pathways, with oxidation playing a minor role. |
In human plasma, total drug-related exposure is mainly related to asundexian and its pharmacologically inactive metabolite M10. |
1 Introduction
Thromboembolic diseases are a major cause of mortality and morbidity worldwide [1]. Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia and is associated with increased rates of death, stroke, and other thromboembolic events due to a predisposition for the development of atrial thrombi [2].
Non-cardioembolic ischemic stroke is a subset of ischemic stroke and accounts for around 75% of all ischemic strokes. The ischemic stroke recurrence rate is substantial and remains at 3 to 6% per year despite antiplatelet therapy, which represents the current standard of care.
Full anticoagulation with vitamin K antagonists (VKAs) was the recommended therapy for patients with AF until the introduction of direct oral anticoagulants (DOACs).
Although anticoagulation is a mainstay of antithrombotic therapy, the usefulness of current therapies is limited by an increased risk of bleeding, which is lessened but not eliminated with DOACs compared with VKAs [3]. Hence, a need remains for new therapies, particularly for patients at high risk of thromboembolic events and/or bleeding events.
Although the anticoagulants that are currently available have had a major impact on the prevention of thromboembolic events in both venous and arterial thrombotic conditions, the increased risk of bleeding that is inherent in their mechanism of action have led to the search for alternatives that are at least as effective and have a better safety profile. Current efforts in the development of new treatment options in thrombosis prevention have focused on factor XIa (FXIa), a component of the intrinsic coagulation pathway that is upstream of factor X and factor II (independent of the extrinsic pathway) and, therefore, unlikely to lead to an increased risk of clinically significant bleeding [4, 5].
Asundexian (BAY 2433334) is a potent, oral, direct, and reversible inhibitor of FXIa that prolonged the activated partial thromboplastin time (aPTT) in a concentration-dependent manner in phase 1 studies, is considered to have a favorable safety profile, and is well tolerated [6, 7]. Additionally, in a phase 2b trial in patients with AF (PACIFIC-AF), lower rates of bleeding were observed with pooled 20 mg and 50 mg once-daily (OD) asundexian doses compared with standard dosing of apixaban for the composite of major or clinically relevant nonmajor bleeding [8]. In two further phase 2b trials of asundexian 10, 20, or 50 mg OD in patients who had experienced a recent acute myocardial infarction (PACIFIC-AMI) or acute noncardioembolic ischemic stroke (PACIFIC-STROKE), asundexian did not significantly increase bleeding risk compared with placebo [9, 10]. Low rates of ischemic events (composite of cardiovascular death, myocardial infarction, stroke, or stent thrombosis) were observed in PACIFIC-AMI (5.5–6.8% with asundexian versus 5.5% with placebo) [9]. In PACIFIC-STROKE, there was no overall dose-response effect with asundexian on the composite endpoint of covert brain infarction or ischemic stroke; however, in post-hoc exploratory analyses, 50 mg asundexian reduced the risk of composite recurrent symptomatic ischemic stroke or transient ischemic attack by 36% relative to placebo [10]. Based on clinical pharmacology studies in healthy male participants, asundexian plasma exposure appears to increase in a dose-proportional manner between 5 mg and 150 mg administered as a single dose and between 25 mg and 100 mg administered as multiple OD doses [6, 7]. The pharmacokinetics were found to be independent of time, with low accumulation ratios for the area under the concentration–time curve (AUC; 1.5–1.7) and the maximum plasma asundexian concentration (Cmax; 1.4–1.6) after multiple OD dosing compared with the AUC and Cmax after single-dose administration, respectively [7]. After oral administration as a 25-mg amorphous solid dispersion (ASD) immediate-release (IR) tablet, asundexian was virtually completely bioavailable in humans, with a geometric mean bioavailability of 94% (after correction for the actual administered dose) [11]. Thus, first-pass metabolism in the gut and liver does not play an important role, and no clinically relevant changes were observed in the bioavailability owing to the nature of the orally received formulation (polyethylene glycol [PEG] solution, IR tablet, or ASD IR tablet), food conditions (high-fat, high-calorie breakfast), or gastric pH modulation (omeprazole or antacid) [11].
Human mass-balance studies are central to the clinical pharmacology package for new drug applications [12]. Along with mass-balance studies in animals (e.g., bile-duct cannulated [BDC] rats), they provide important information regarding exposure to parent compounds and their metabolites [12, 13]. This paper presents the results of a human mass‑balance study for asundexian, which was conducted to gain a deeper understanding of the absorption, distribution, metabolism, and excretion of the compound, as well as its potential for drug–drug interactions. The current investigations were also designed to provide an overview of the biotransformation and clearance pathways for asundexian in humans and BDC rats in vivo as well as in vitro in hepatocytes of both species.
2 Materials and Methods
2.1 Reagents and Reference Compounds
[14C]asundexian (4-({(2S)-2-[4-{5-chloro-2-[4-(trifluoromethyl)-1H-1,2,3-triazol-1-yl]phenyl}-5-methoxy-2-oxopyridin-1(2H)-yl]-[14C]butanoyl}amino)-2-fluorobenzamide) was labeled at the central amide carbonyl group. Radiolabeled [3H]asundexian was labeled at both phenyl rings. [14C]asundexian and [3H]asundexian as well as non-labeled asundexian and the metabolites M1, M2, M9, M10, and M15 were synthetized at Bayer AG (Wuppertal, Germany). [14C]asundexian had a radiochemical purity of > 98% and a specific radioactivity of approximately 1.9 MBq/mg, while the [3H]asundexian had a radiochemical purity of > 98% and a specific activity of 10–30 MBq/mg. Cryopreserved hepatocytes were obtained from KaLy-Cell (Illkirch, France), Triangle Research Labs (now Lonza), Lonza (Basel, Switzerland), BioreclamationIVT (now BioIVT; Baltimore, MD, USA), and Biopredic International (Rennes, France).
2.2 Human Mass-Balance Study: Design and Sample Collection
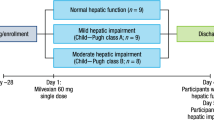
A single-center, open-label, nonrandomized study in healthy, white, male volunteers aged 18–55 years with a body mass index of 18.0–29.9 kg/m2 was performed to study the pharmacokinetics of asundexian, with a focus on metabolism and excretion patterns, mass balance, and safety and tolerability, after oral administration of a single nominal dose of 25 mg asundexian containing about 3.7 MBq [14C]asundexian (study 1). Study exclusion criteria are detailed in Table S1 of the Electronic Supplemental Material (ESM). The study was conducted at PRA Health Sciences (now ICON plc, Groningen, Netherlands) in accordance with Good Clinical Practice, the ethical principles specified in the Declaration of Helsinki, and was approved by an accredited institutional ethics committee. The radioactive dose was calculated to comply with the International Commission on Radiological Protection category IIa guidelines [14]; that is, it resulted in a radioactive exposure not exceeding 1 mSv. After overnight fasting for at least 10 hours, six participants received 25 mg [14C]asundexian (as oral solution in 6.25 mL) administered with 240 mL water [6]. The participants stayed at the study center for at least 10 days, during which time safety parameters (including blood pressure, pulse rate, and electrocardiogram [ECG]), urine drug screening parameters, and adverse events were monitored and a physical examination was performed. Four of the participants were discharged at 240 h after dosing, one was discharged at 312 hours after dosing, and another was discharged at 336 hours after dosing, once the release criteria—individual excretion of total radioactivity corresponding to at least 90% of the administered dose and less than 1% of the radioactivity excreted in two consecutive 24-hour collection intervals—had been fulfilled.
Blood samples (5.4 mL [2 × 2.7 mL] for total radioactivity analysis, 2.7 mL for pharmacokinetic analysis, and 10 mL for metabolite profiling) were collected before dosing and at 0.5, 1, 2, 3, 4, 6, 8, 12, 15, 24, 48, 72, 96, 120, 144, 168, 192, 216, and 240 hours after dosing. If on day 10 after asundexian administration the criteria for discharge were not met, sample collection was extended to 264, 288, 312, 336, or 360 hours with sample collection every 24 hours, depending on the excreted radioactivity. Total radioactivity was analyzed in blood using one of the 2.7 mL blood samples and in plasma following its preparation using the second 2.7 mL sample. Samples of urine and feces were collected in 12-hour intervals on day 1 and in 24-hour intervals thereafter up to day 10 after dosing (depending on whether the discharge criteria were met). Total radioactivity in plasma, blood, feces, and urine was determined at PRA Health Sciences (now ICON plc, Assen, Netherlands) by liquid scintillation counting (LSC) using Ultima Gold and PermaFluor E LSC cocktails (PerkinElmer, Rotterdam, Netherlands) and a Tri-Carb 3100TR liquid scintillation counter (PerkinElmer, Rotterdam, Netherlands).
Samples from two additional clinical pharmacology studies were used for metabolite scouting in plasma and have been published previously. In a single-dose-escalation study (study 2), samples were taken between 0 h and 72 h [6] for the 25 mg asundexian dose step (liquid service formulation) and between 0 h and 96 h in a multiple-dose-escalation study (study 3) for 100 mg asundexian IR tablet OD [7]. Analysis was performed on pooled samples (study 2, n = 7; study 3, n = 9).
2.3 Preparation of Samples for Radioactive Metabolite Profiling by High-Performance Liquid Chromatography With Liquid Scintillation Counting
Extraction recoveries of total asundexian-related radioactivity from samples of human plasma and feces, and as a control for human urine, were determined by LSC using Ultima Gold, a high-flash-point scintillation cocktail (PerkinElmer LAS [Germany] GmbH, Rodgau, Germany), and Tri-Carb 2910TR and 4910TR counters (PerkinElmer LAS [Germany] GmbH, Rodgau, Germany) with automatic quench correction by the external standard channel ratio method at 13 °C.
2.3.1 Human
For details of the preparation and storage of plasma samples, please refer to Table S4 of the ESM. Aliquots from individual plasma samples collected at each time point (0.5 mL) were treated with 2 mL of acetonitrile/10 mM ammonium formate, pH 3 (9/1, v/v), and the precipitated proteins were removed by centrifugation. The supernatants were separated and concentrated stepwise in an iterative process. Separately, an undiluted plasma extract (100 µL) was diluted with 10 mM ammonium formate, pH 3 (100 µL), and subsequently added to the previously concentrated plasma extracts. Aliquots (30 µL) of the final samples were analyzed using high-performance liquid chromatography (HPLC) with offline radioactivity detection. The mean workup recovery from samples prepared as described above for the various sampling time points was 105.5%. Aliquots of individual urine samples were centrifuged and directly analyzed using HPLC with offline radioactivity detection. Samples of homogenized feces (about 0.5–1.4 g) were extracted twice with acetonitrile/10 mM ammonium formate pH 3 (9:1, v/v; 1.5 mL and 1 mL, respectively). The suspensions obtained were centrifuged and the supernatants were collected separately. The two combined extracts were homogenized, and aliquots were concentrated in an iterative process to about 20–50 µL. Separately, an unconcentrated feces extract (100 µL) was diluted with 10 mM ammonium formate, pH 3 (100 µL), and subsequently added to the concentrated feces extracts detailed above. Aliquots of 30 µL or 50 µL of the final samples were analyzed using HPLC with offline radioactivity detection. Mean workup recovery for the feces samples was 95.8%.
2.3.2 Rat
Details of the preparation of rat study samples for radioactive metabolite profiling are provided in Table S3 of the ESM.
2.4 Radioactive Metabolite Profiling
Samples were analyzed using HPLC-LSC on an XBridge C18 reversed-phase (RP) column (Waters, Milford, MA, USA) with ammonium acetate/methanol (human) gradient elution or an Atlantis T3 RP column (Waters, Milford, MA, USA) with formic acid (0.05%)/acetonitrile (rat) gradient elution, both with offline radioactivity detection using the Ultima-Flo AP scintillation cocktail (PerkinElmer LAS [Germany] GmbH, Rodgau, Germany) with 1450 (human and rat) and 2450 (human) MicroBeta2 liquid scintillation counters (PerkinElmer, Turku, Finland) and a 10-s sampling time.
The radioactivity concentration for each component in the respective species and matrices was calculated by multiplying the total radioactivity present in plasma, urine, feces, bile, or the gastrointestinal tract (GIT) by the percentage peak area obtained after HPLC separation, fractionation, and offline radioactivity detection using LSC. Pharmacokinetic parameters for analytes obtained from metabolite profiling of rat samples via HPLC-LSC were determined using ToxKin software (Entimo, Berlin, Germany).
2.5 Quantification of Asundexian and Metabolite M10 in Human Plasma
Bioanalysis of asundexian and metabolite M10 in human plasma was performed at Swiss BioQuant AG (Reinach, Switzerland). Asundexian and M10 were determined in plasma after protein precipitation with methanol and subsequent separation using HPLC with tandem mass spectrometry (MS/MS). Method validation and analysis of the study samples were performed in compliance with the pertinent guidelines on bioanalytical method validation [15, 16]. [13C7,15N]asundexian racemate and [13C7,15N]M10 were used as internal standards (100 µg/L for both standards). For asundexian, the calibration concentrations ranged from 5.00 µg/L (lower limit of quantification [LLQ]) to 5000 µg/L (upper limit of quantification [ULQ]). Quality control (QC) samples in the concentration range 15.0–3750 µg/L were determined with an accuracy of 96.0–101.0% and a precision of 2.3–3.4%.
For metabolite M10, the calibration range was from 0.500 µg/L (LLQ) to 500 µg/L (ULQ). QC samples in the concentration range 1.50–375 µg/L were determined with an accuracy of 93.3–96.3% and a precision of 2.0–2.4%. All samples were stored at or below −20 °C and analyzed in the 49 days after sampling. Stability data indicated that the analytes were stable during this time period.
Further details of method validation and the methods used for the quantification of asundexian and its metabolites are provided in the ESM (Tables S5 and S6).
2.6 Quantification of Metabolites M1, M2, M9, M10, and M15 in Human Plasma
Calibration samples with authentic reference standards were prepared by diluting the stock solutions of asundexian and its metabolites with respective volumes of acetonitrile and blank plasma (acetonitrile first and then blank plasma). Human plasma samples from the clinical studies, namely single dose escalation (single dose of 25 mg [6]) and multiple dose escalation (multiple doses of 100 mg OD [7]), were used for metabolite scouting. Participant plasma samples from these studies were pooled per time point by equal volume (100 µL per participant and per time point). To 100 µL or 200 µL of each of the obtained corresponding pools per time point, 300 µL or 600 µL, respectively, of an acetonitrile/0.5% formic acid solution containing the internal standards was added to precipitate proteins, and the resultant solution was thoroughly mixed. All samples were centrifuged for 5 minutes. For samples from the single-dose study, 300 µL aliquots of the supernatants were concentrated to approximately 100 µL before analysis using HPLC with high-resolution mass spectrometry (HRMS). Aliquots from the multiple dose study were analyzed directly using HPLC-HRMS.
2.7 Chemical Structure Elucidation
Metabolites were investigated using HPLC-HRMS and offline radioactivity detection as described below (see the “Biotransformation in Hepatocytes” section). Metabolites were assigned by comparison of retention time and mass spectrometric data from in vivo samples to data obtained from in vitro incubations with hepatocytes or authentic reference compounds (M1, M2, M9, M10, M15). Structural proposals for metabolites were made based on the exact mass, leading to the molecular formula and characteristic mass spectrometric fragmentation patterns.
2.8 Data Evaluation and Pharmacokinetic Analysis
For asundexian and metabolite M10, the calculation of pharmacokinetic parameters was performed based on concentrations determined by LC-MS/MS in plasma. The blood/plasma ratio was determined using the total radioactivity measurements obtained using LSC.
Noncompartmental analysis (NCA) of asundexian and M10 (LC-MS/MS data) and of total radioactivity data (blood, plasma) was performed using Phoenix 8.1 software (Certara, Princeton, NJ, USA) in conjunction with the NCA Tool plugin (release 1.0). From the plasma concentration–time data for asundexian, the Cmax, time to Cmax (tmax), AUC from time zero to the time of the last quantifiable concentration (AUClast), the AUC from time zero extrapolated to infinity (AUC∞), and the elimination half-life (t½) were calculated. In addition, the ratio of whole blood to plasma was derived for the total radioactivity parameter AUC; that is, Ratio(AUC) = (AUCblood/AUCplasma). For the metabolites quantifiable in plasma from the metabolite scouting, respective pharmacokinetic parameters were determined using ToxKin software (Entimo, Berlin, Germany).
The total radioactivity in urine and feces was determined by multiplying the volume or weight of the samples by the respective total radioactivity concentration. The amount of radioactivity recovered in the excreta (Ae) was related to the actual administered radioactive dose to establish the radioactive balance. Arithmetic means and percentage coefficients of variation (%CVs) were calculated for these percentages. Urine and feces were collected as completely as possible up to day 15 after asundexian administration on day 1. Cumulative excretion was calculated as the sum of the excretions during the collection intervals. The concentration/amount of each analyte for each sample/time point was calculated by multiplying the total radioactivity concentration/amount of each sample by the percentage area of each analyte obtained after HPLC fractionation and offline radioactivity detection. Means were calculated if results for at least four of the six participants were available.
2.9 Statistical Evaluation
Pharmacokinetic parameters were evaluated by descriptive data analysis without formal hypothesis testing by calculating the arithmetic mean/standard deviation (Ae parameters), median/range (tmax) or geometric mean/%CV (remaining parameters). Statistical evaluation of the results was performed using SAS software, version 9.4 (SAS Institute Inc., Cary, NC, USA).
Given the exploratory nature of the study, no formal sample size estimation was performed for the study in humans. According to the FDA guidance 2022, due to the low to moderate interindividual variability observed in clinical pharmacology studies, a sample size of six participants was considered sufficient. A similar rationale was applied to the rat studies, which were considered exploratory in nature. Thus, a sample size of 4 animals was considered sufficient.
2.10 Safety Analysis
Safety was monitored through the reporting of adverse events (AEs) by the participants. The investigator was responsible for detecting, documenting, and recording events that met the definition of an AE, a serious AE, or an AE of special interest (see Table S2 of the ESM). Additional safety evaluations included physical examinations and blood pressure/heart rate, body temperature, and 12-lead ECG assessments.
2.11 Animal Studies
Animal studies were conducted at Bayer AG (Wuppertal, Germany) in accordance with Directive 2010/63/EU of the European Parliament and of the Council of 22 September 2010 on the Protection of Animals Used for Scientific Purposes and the German Animal Protection Act of 4 July 2013 (Deutsches Tierschutzgesetz, approval no. N0820a0206). All institutional as well as national guidelines for the care of the laboratory animals were followed.
2.11.1 Mass Balance Study in Bile-Duct Cannulated Rats
The mass balance was studied in male (Crl:WI[Han]) BDC Wistar rats (N = 4) after intravenous (IV) administration of [14C]asundexian (1.96 MBq/mg) 1 mg/kg dissolved in a mixture of 1% dimethyl sulfoxide (DMSO) and 99% rat plasma (v/v; 0.2 mg/mL). Urine, feces, bile, and GIT samples (complete GIT content including retained feces) and the remaining body (carcass) were collected over various time periods during the 24 hours after administration (urine: 0–7 hours and 7–24 hours; feces: 0–24 hours; bile: 0–7 hours and 7–24 hours; GIT: 24 hours, carcass: 24 hours).
2.12 In Vitro Studies
2.12.1 Biotransformation in Hepatocytes
Cryopreserved hepatocytes from humans (mixed gender pool of five donors) and Wistar rats were incubated with 1 µM [3H]asundexian in William’s E medium at 37 °C in suspension culture at a cell density of 106 viable cells/mL. Aliquots taken at 0 hours and 4 hours of incubation time were mixed with acetonitrile to a final content of about 30% (v/v), and samples were stored at −20 °C. Before analysis, the samples were thawed and centrifuged for 5 min. To control for the recovery of radioactivity, an aliquot of 10 μL of the supernatant was analyzed by LSC using a Tri‑Carb 2900TR counter (PerkinElmer, Turku, Finland) with automatic quench correction (workup recoveries were > 88%). Further aliquots of the supernatants were analyzed by HPLC-HRMS using a 1290 Infinity II LC system (Agilent, Waldbronn, Germany) and a Q Exactive Plus with a heated electrospray ionization source used in positive ionization mode (Thermo Fisher Scientific, Bremen, Germany) and a 1:10 split to a fraction collector (Gilson robotic liquid handler 222 XL, Abimed Analysen-technik, Langenfeld, Germany). Fractions were mixed with 150 µL Ultima-Flo AP scintillation cocktail, and offline radioactivity monitoring was conducted using a 1450 MicroBeta2 counter (PerkinElmer, Turku, Finland).
2.12.2 Stability of Asundexian in Human Feces
Under anaerobic conditions, a suspension of fresh human feces (about 0.5 g) in degassed water (final volume of 5 mL) was treated with a solution of [14C]asundexian (1 mg/mL in acetonitrile; final concentration of 10 μM). The suspension was incubated for 19 hours at 37 °C and centrifuged before the incubation was terminated by the addition of acetonitrile (5 mL). The resulting supernatant was directly analyzed using HPLC with offline radioactivity detection. Positive controls for microbial activity of the used feces were applied under the same experimental conditions [17,18,19]. The corresponding negative control experiments were performed in water under the same experimental conditions.
2.13 Evaluation of the Impact of Metabolite M10 on FXIa and on the Plasma Clotting Time
Potential inhibitory activities of M10 on human FXIa or on the clotting process in human plasma after contact activation were investigated in enzymatic assays in buffer and in the aPTT assay in human plasma, respectively, as described previously [20]. In brief, different solutions of M10 in DMSO were prepared to yield final assay concentrations up to 50 µM. For the buffer assay, a solution of M10 in DMSO (1 µL), a buffer solution (pH 7.4) consisting of 50 mM Tris/HCl, 100 mM NaCl, 5 mM CaCl2, and 0.1% bovine serum albumin (20 μL), a solution of human FXIa (20 μL), and a solution containing a fluorogenic peptidic FXIa substrate (20 μL) were mixed. The fluorescence (excitation wavelength: 360 nm; emission wavelength: 460 nm) was measured over time to determine the enzymatic activity at different M10 concentrations and thereby calculate the half-maximal inhibitory concentration (IC50). For the clotting-time determination, 49 µL of human plasma was incubated for 3 minutes with different concentrations of M10 in 1 µL DMSO. To this mixture, 50 µL of a kaolin/cephalin suspension (C.K. Prest, Diagnostica Stago, France) was added. After 3 minutes the clotting process was initiated with 50 µL of a calcium dichloride solution. The clotting time was determined in an automated coagulometer (AMAX 200, Trinity Biotech Plc, Ireland) and compared with the clotting time without M10.
3 Results
3.1 Excretion and Mass Balance
In the human study, 6 healthy male participants (mean age [SD; range] 27.0 [7.6; 20.0–37.0] years, mean [SD; range] BMI 21.8 kg/m2 [2.3;19.7–26.0 kg/m2]) received the study drug and completed the study. Mean recovery of drug-derived radioactivity in excreta up to 14 days after the dosing of [14C]asundexian was 101% (range: 97.0–103.3%) of the administered dose, with 80.3% (range: 73.6–84.6%) in feces and 20.3% (range: 14.8–26.7%) in urine (Fig. 1).
In BDC rats, radioactivity recovered from urine, feces, bile, GIT, residues (total body excluding GIT), and cage wash samples in the 24 hours after [14C]asundexian dosing amounted to 97.9% of the administered dose. Radioactivity was predominantly recovered from bile (66.8%) and to a lesser extent from feces (20.0%) and urine (0.7%). In total, 7.5% of the administered radioactivity was recovered from the GIT.
3.2 Pharmacokinetics in Humans
[14C]asundexian-associated radioactivity in blood and plasma was absorbed in a median tmax of 1.52 hours after administration of 25 mg [14C]asundexian as oral solution; the geometric mean Cmax was 269 µg-eq/L in blood and 434 µg-eq/L in plasma. The geometric mean exposure (AUC) of total radioactivity was 6530 µg-eq × h/L and 10,800 µg-eq × h/L in blood and plasma, respectively. Based on individual values, the geometric mean blood to plasma ratio of radioactivity was 0.605 for the AUC, indicating that asundexian and/or its metabolites were mainly present in plasma (Table 1, Fig. 2). In plasma, a maximum asundexian concentration of 338 µg/L (geometric mean) was reached in a median of 1.50 hours after dosing, and the geometric mean AUC was 7880 µg-eq × h/L (Table 1, Fig. 2). Based on these results, the radioactivity in plasma was mainly attributed to the parent compound.
Plasma concentration–time profiles for total drug-related components, total radioactivity, asundexian, and metabolite M10 (geometric mean [standard deviation]) in humans after oral administration of a single dose of 25 mg asundexian containing 3.7 MBq [14C]asundexian (N = 6). eq equivalent, LLQ lower limit of quantification
3.3 Metabolite Profiles in Plasma and Excreta
The structures of asundexian and the proposed metabolites identified during in vivo and in vitro investigations are shown in Fig. 3. Pharmacokinetic parameters obtained for asundexian and the relevant metabolites in plasma are presented in Table 1; their excretion patterns (dose percentages recovered from urine and feces of human and rat and from bile and GIT for the BDC rat) as observed in the respective mass-balance studies are given in Table 2. Representative chromatograms obtained from human plasma, urine, and feces are shown in Fig. 4; chromatograms for rat bile, urine, feces, and GIT are presented in Fig. S1 of the ESM.
Radiochromatograms for human plasma (a), urine (b), and feces (c) after oral administration of a single dose of 25 mg [14C]asundexian that are representative of the participant and time range (metabolite M10 is not depicted as it does not include the radiolabel). BKG background, cps counts per second
3.3.1 Human
Two major primary biotransformation pathways were identified: (a) hydrolysis at the central amide moiety of asundexian leading to the formation of the carboxylic acid metabolite M1 and aniline metabolite M9 (nonlabeled) and the subsequent N-acetylation of M9 to produce metabolite M10 (nonlabeled) as well as hydrolysis at the terminal amide moiety to form the respective carboxylic acid metabolite M2; and (b) several oxidative biotransformation reactions leading to the formation of demethylated metabolite M3 and monohydroxylated metabolites M4, M5, and M6. In humans, hydrolysis to M1 and M9 (and subsequently to M10) was more pronounced than the hydrolysis to M2, whereas the opposite trend was observed in rats (Table 2). Metabolites were also identified further downstream; for example, ketone metabolite M7, aldehyde metabolite M8, carboxylic acid metabolite M14, and the glucuronide metabolite M16. Extraction recovery of radiolabeled asundexian-associated analytes after workup from plasma and feces was high. In human plasma, only asundexian was detectable via HPLC-LSC up to 120 hours after dosing, and thus asundexian solely accounted for the radioactivity present (Figs. 2 and 4a). However, besides unlabeled metabolite M10, metabolites M1 to M6 were found in trace amounts by HPLC-HRMS in representative human plasma samples from this study. As M10 does not contain the [14C] label, the exposure of M10 was also determined using HPLC-MS/MS and not related to total radioactivity. Geometric mean exposure of M10 in plasma was 10.2 µg/L (30.7 µg-eq/L) and 700 µg × h/L (2120 µg-eq × h/L) for Cmax and AUC, respectively. As a consequence, the geometric mean plasma AUC of total drug-related components as a sum of total radioactivity and M10 content was 12,900 μg-eq × h/L (21.8 μmol × h/L). Based on the total cumulated AUC of all drug-related components in plasma, 61.0% could be attributed to the parent compound asundexian. M10 accounted on average for 16.4% of the total drug-related AUC, thus representing a major human metabolite in plasma (Table 1). HPLC-HRMS analysis demonstrated that in healthy male participants, asundexian accounted for 75.0% of the total cumulative AUC, calculated as the sum of asundexian and all quantified metabolites (M1, M2, M9, M10, M15 [M15 after 100 mg OD only; Table 1, study 3]), after a single dose of 25 mg asundexian administered as a PEG solution and monitored for up to 72 hours after dosing (Table 1). Following multiple OD dose administration of 100 mg asundexian (IR tablets), asundexian accounted for 71.2% of total cumulative AUC(0–24)md (Table 1) [6, 7]. Metabolite M10 (24.0% of the cumulative AUC after single-dose administration, 27.0% of the cumulative AUC(0–24)md after multiple OD dose administration) was found to be the only major human plasma metabolite (Table 1). In contrast, metabolites M1 (about 0.6–1% of the cumulative AUC after single-dose or AUC(0–24)md after multiple dose administration), M9, and M15 (each accounting for ≤ 2.7% of the cumulative AUC or AUC(0–24)md) were clearly regarded as minor human plasma metabolites. Furthermore, several other metabolites were also detected in plasma in trace amounts (e.g., M4, M5, M6). Others were below the limit of detection (e.g., M2, M3, M7, M8, M9, M14, M16) after oral single-dose administration of 25 mg asundexian, but were detected after multiple-dose administration of 100 mg asundexian OD (e.g., M2, M9, M14, M16).
In human feces (mean amount of the total radioactivity excreted into feces [Aefec(0–tlast)]: 80.3%), metabolite M1 (formed by amide hydrolysis), and the parent drug were the most prominent components, covering on average 37.7% and 28.0% of the administered dose, respectively (Table 2). Furthermore, metabolites resulting from oxidative biotransformation (M3, M4, M5, M6, M7, M8, M14) were detected in feces, and together they covered 11.6% of the administered dose: metabolite M4 (hydroxylation) accounted for 5.2% and metabolites M3 (demethylation) and M7 (oxidation) each accounted for approximately 2.0% of the administered dose. Metabolites M5 and M6 (formed by hydroxylation), aldehyde metabolite M8, and carboxylic acid metabolite M14 in feces each accounted for less than 1.5% of the dose. Metabolite M2, formed by terminal amide hydrolysis, was also detected in feces and accounted for 2.5% of the dose. The stability of asundexian against the microbial environment was investigated under anaerobic incubations of [14C]asundexian with human feces. No relevant degradation of asundexian was observed in human feces compared with the respective positive and negative control experiments (Fig. S2 of the ESM).
In human urine (mean amount of the total radioactivity excreted into urine [Aeur(0–tlast)]: 20.3%), the parent drug and metabolite M1 were the predominant components, covering on average 9.4% and 8.8% of the administered dose, respectively (Table 2). Furthermore, metabolites resulting from oxidative biotransformation (M3, M4, M5, M6, M7, M8, M14) were present in low amounts (totaling 1.5% of the dose), with each representing less than 1% of the administered dose. Unlabeled metabolites M9 and M10 were detected qualitatively by HPLC-HRMS. The mean proportion of the dose excreted into urine in humans (Aeur(0–tlast)) as M10 was 5.5%, as determined using HPLC-MS/MS.
3.3.2 Rat
Following IV administration of [14C]asundexian to BDC rats (N = 4; age, ~ 8 weeks; weight, 267–290 g), total radioactivity was mainly excreted via the biliary/fecal route (> 94%). Approximately 67% of the total radioactivity was excreted with bile, mainly as M2 (~ 41%) and M7 (~ 11%) together with several other components (parent drug: 0.3%; M1, M3/M5, M4, M6/M8, M14: each < 2.5%), as seen in Table 2. Less than 1% of the dose was found in urine (parent drug: < 0.1%; M4, M5: each < 0.3%; M2, M3, M6, M7, and M8: each < 0.1%). Indicative of direct secretion, 20.0% and 7.5% of the total radioactivity was found in feces and GIT, respectively, predominantly as the parent drug (sum of feces and GIT: 24.0% of dose) together with minor metabolites (M2, M3, M4, M5, M6: each < 1%); see Table 2.
3.3.3 In Vitro Data
3.3.3.1 Hepatocytes
In male rat and human hepatocytes, turnover of [3H]asundexian (1 µM) was about 48% and 19% after 4 hours of incubation, respectively. Chromatograms obtained from incubates are represented in Fig. S3 in the ESM. Two major biotransformation pathways were identified: (a) in humans, hydrolysis of the central amide leading to the formation of M1, M9, and subsequently M10, or in rats, hydrolysis of the terminal amide leading to M2 formation; and (b) oxidative pathways leading through O‑demethylation to the formation of M3 or through hydroxylation to the formation of M4, M5, and M6 with further oxidation or conjugation reactions.
3.4 Evaluation of the Impact of Metabolite M10 on Factor XIa Activity and on the Plasma Clotting Time
Metabolite M10 did not reach 50% inhibition at concentrations up to 50 µM (IC50 > 50 µM). In addition, no prolongation of the human clotting time in the aPTT assay was observed (effective concentration needed to achieve 50% prolongation [EC150] > 37.5 µM) [20].
3.5 Safety Results
Of the six participants, only one (16.7%) experienced treatment-emergent AEs (TEAEs). The events (one TEAE of catheter-site bruising and one of vessel puncture-site bruising) were assessed as being related to procedures required by the protocol but not as being related to the study drug. Both TEAEs were mild in severity. No AEs of special interest or TEAEs leading to discontinuation were reported. Furthermore, no deaths or serious AEs occurred in this study. No clinically relevant effects of asundexian on vital signs or ECG parameters were observed.
4 Discussion
Asundexian has the potential to prevent thromboembolic events, such as ischemic stroke, without significantly increasing the risk of bleeding when compared with apixaban or placebo, and is currently under investigation in confirmatory phase 3 clinical trials (OCEANIC-AF and OCEANIC-STROKE). However, to fulfill this potential, the metabolic pathways of the parent compound and its metabolites must be elucidated to highlight any possible issues with absorption, distribution, excretion, or drug–drug interactions.
The pharmacokinetics of asundexian in humans investigated in this mass-balance study were in accordance with those reported in previous clinical pharmacology studies in healthy participants receiving various oral doses of asundexian as liquid or solid IR formulations [6, 7]. Based on clinical pharmacology studies, asundexian has been shown to be virtually completely absorbed [11], with maximum plasma concentrations observed at a median of 1.0–1.5 hours after administration of the oral solution and, as expected, slightly later (at about 2.0–4.0 hours and 4.0–4.5 hours) after administration as IR or ASD IR tablets, respectively [6, 7]. Asundexian was eliminated from plasma with a geometric mean t½ of about 14.0–19.5 hours after oral administration in healthy participants, with a low apparent plasma clearance after oral dosing of about 3.19–4.40 L/h [6, 7]. The low observed plasma clearance of asundexian with known near-complete bioavailability and negligible first-pass metabolism [11] indicated that asundexian is a low-clearance drug when compared to the hepatic plasma flow of approximately 53 L/h.
Asundexian is distributed in the whole body (volume of distribution at steady state of about 70.5 L; unpublished data from study 1 in [11]) and is preferentially located in plasma (geometric mean blood to plasma ratio of 0.605 for total radioactivity).
In human plasma, the parent molecule represents the majority of all asundexian-related components. The pharmacologically inactive non-labeled metabolite M10, formed by the hydrolysis of the central amide (M9) and subsequent N-acetylation, was identified as a major human plasma metabolite, with a total drug-related exposure in human plasma of 16.4%. Conversely, M9, which is the precursor of M10, also lacks the 14C label and was identified only in trace amounts in human plasma and urine after a single dose of 25 mg asundexian or multiple doses of 100 mg asundexian OD. The remaining percentage of drug-related components in plasma was attributed to the sum of several minor metabolites detected in trace amounts below the sensitivity limit of radiochromatographic profiling but detectable with HPLC-HRMS methods. Qualitative HPLC-HRMS analyses of plasma samples from this human mass-balance study are in agreement with the data obtained from exploratory metabolite scouting. About half of the radioactivity excreted into urine could be attributed to the parent compound, which was in accordance with results from previous studies (~ 8–13% of the dose) assuming glomerular filtration or a well-balanced sum of excretion and reabsorption to be the main mechanism for renal elimination [7]. The other half predominantly comprised M1 (8.8%) with minor amounts of M2, M3, M4, M5, M6, M8, M14, and M16. Furthermore, HPLC-MS/MS analysis revealed that unlabeled M10 was also excreted into urine. In feces, a major proportion of the radioactivity could be attributed to metabolites, with M1 being the predominant component. Compared with the hydrolytic M1 pathway, oxidative metabolites (M3, M4, M5, M6, M8, M14) and M2 accounted for a minor part of the total radioactivity. In addition, asundexian was present in feces, contributing to 28.0% of the total radioactivity in humans. Cross-study comparisons showing similar exposure of the oral solution under investigation here to that of the ASD IR tablet used in the dedicated absolute bioavailability study (study 1 in [11]) as well as to that of the ASD IR tablet to be used in phase 3 clinical trials (study 3 in [11]) suggest high bioavailability for asundexian in the study reported here. Subsequently, the unchanged drug found in the feces is not a result of limited absorption or first-pass metabolism but of biliary or extrabiliary excretion.
Similar results to the human data were observed in the BDC rat mass-balance study, in which approximately 24% of the administered asundexian was excreted unchanged into feces and the GIT. Furthermore, the unchanged asundexian found in feces and GIT in BDC rats mainly resulted from direct secretion into the GIT and not from biliary secretion, suggesting that direct excretion of asundexian into the GIT could also be at least a potential excretion pathway in humans, despite complete absorption after administration [11].
Additionally, there is no indication of any long-lasting retention of radioactivity in humans, which is supported by the finding of complete recovery of total radioactivity in the 14 days after administration.
The preclinical and clinical data presented in this paper provide an in-depth insight into the metabolic fate and excretion patterns of asundexian in humans. After IV administration of [14C]asundexian to BDC rats, radioactivity was almost exclusively excreted via the biliary/fecal route, with negligible amounts in urine, compared with approximately 20% in human urine. Although some quantitative differences between rats and humans were observed regarding the preferred clearance pathways of asundexian, overall, the results show high consistency, with the same pattern of metabolic reactions observed in rats and humans studied in vitro and in vivo. Results indicate that the main difference is that hydrolysis in rats preferentially occurs at the terminal amide moiety, leading to the formation of M2, whereas the site of hydrolysis in humans is located at the central amide bond, leading to the formation of M1 and M9 and subsequently M10. The in vivo data obtained in this study reflect the in vitro results, with the hydrolysis pathway favored over the oxidative biotransformation. In rats, the carboxylic acid metabolites are predominantly excreted in feces, while in humans, urinary excretion was also observed; this may be potentially related to interspecies differences in the molecular weight cutoffs for organ excretion [21, 22].
Several limitations of this study should be noted. First, owing to the lack of data from reproductive studies, the study population was limited to healthy white men. Second, data from rat models investigating the mechanism of unchanged excretion may not extrapolate to humans and should consequently only be used for hypothesis generation.
5 Conclusion
These results suggest that, in humans, asundexian is cleared in a quantitative manner during the period up to 14 days after administration, predominantly via feces and to a lesser extent via urine. The predominant clearance pathways of asundexian involve amide hydrolysis to M1 and unchanged excretion, while oxidative biotransformation is of minor importance. The clinical data presented here, taken together with preclinical experiments in BDC rats and hepatocytes, have provided information on the metabolism and clearance of asundexian. Metabolite M10, which exhibits no pharmacological activity, was identified as a major metabolite of asundexian in human plasma.
References
Wendelboe AM, Raskob GE. Global burden of thrombosis: epidemiologic aspects. Circ Res. 2016;118(9):1340–7. https://doi.org/10.1161/CIRCRESAHA.115.306841.
Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991;22(8):983–8. https://doi.org/10.1161/01.str.22.8.983.
Marano G, Vaglio S, Pupella S, et al. How we treat bleeding associated with direct oral anticoagulants. Blood Transfus. 2016;14(5):465–73. https://doi.org/10.2450/2016.0180-15.
Gailani D, Gruber A. Factor XI as a therapeutic target. Arterioscler Thromb Vasc Biol. 2016;36(7):1316–22. https://doi.org/10.1161/ATVBAHA.116.306925.
Zhang H, Lowenberg EC, Crosby JR, et al. Inhibition of the intrinsic coagulation pathway factor XI by antisense oligonucleotides: a novel antithrombotic strategy with lowered bleeding risk. Blood. 2010;116(22):4684–92. https://doi.org/10.1182/blood-2010-04-277798.
Thomas D, Kanefendt F, Schwers S, et al. First evaluation of the safety, pharmacokinetics, and pharmacodynamics of BAY 2433334, a small molecule targeting coagulation factor XIa. J Thromb Haemost. 2021;19(10):2407–16. https://doi.org/10.1111/jth.15439.
Kubitza D, Heckmann M, Distler J, et al. Pharmacokinetics, pharmacodynamics and safety of BAY 2433334, a novel activated factor XI inhibitor, in healthy volunteers: a randomized phase 1 multiple-dose study. Br J Clin Pharmacol. 2022;88:3447–62. https://doi.org/10.1111/bcp.15230.
Piccini JP, Caso V, Connolly SJ, et al. Safety of the oral factor XIa inhibitor asundexian compared with apixaban in patients with atrial fibrillation (PACIFIC-AF): a multicentre, randomised, double-blind, double-dummy, dose-finding phase 2 study. Lancet. 2022;399:1383–90. https://doi.org/10.1016/S0140-6736(22)00456-1.
Rao SV, Kirsch B, Bhatt DL, et al. A multicenter, phase 2, randomized, placebo-controlled, double-blind, parallel-group, dose-finding trial of the oral factor XIa inhibitor Asundexian to prevent adverse cardiovascular outcomes after acute myocardial infarction. Circulation. 2022;146(16):1196–206. https://doi.org/10.1161/CIRCULATIONAHA.122.061612.
Shoamanesh A, Mundl H, Smith EE, et al. Factor XIa inhibition with asundexian after acute non-cardioembolic ischaemic stroke (PACIFIC-STROKE): an international, randomised, double-blind, placebo-controlled, phase 2b trial. Lancet. 2022;400(10357):997–1007. https://doi.org/10.1016/S0140-6736(22)01588-4.
Kanefendt F, Brase C, Unger S, et al. Effects of tablet formulation, food, or gastric pH on the bioavailability of asundexian. Clin Pharmacol Drug Dev. 2023;12(2):219–30. https://doi.org/10.1002/cpdd.1207.
Coppola P, Andersson A, Cole S. The importance of the human mass balance study in regulatory submissions. CPT Pharmacometr Syst Pharmacol. 2019;8(11):792–804. https://doi.org/10.1002/psp4.12466.
Burden N, Kendrick J, Knight L, et al. Maximizing the success of bile duct cannulation studies in rats: recommendations for best practice. Lab Anim. 2017;51(5):457–64. https://doi.org/10.1177/0023677217698001.
International Commission on Radiological Protection. The 2007 recommendations of the International Commission on Radiological Protection. ICRP Publication 103. Ann ICRP. 2007;37:2–4.
US Food and Drug Administration. Bioanalytical method validation: guidance for industry. 2018. https://www.fda.gov/files/drugs/published/Bioanalytical-Method-Validation-Guidance-for-Industry.pdf. Accessed 17 August 2022.
European Medicines Agency. Guideline on bioanalytical method validation. 2011. https://www.ema.europa.eu/documents/scientific-guideline/guideline-bioanalytical-method-validation_en.pdf. Accessed 17 August 2022.
Gerisch M, Hafner FT, Lang D, et al. Mass balance, metabolic disposition, and pharmacokinetics of a single oral dose of regorafenib in healthy human subjects. Cancer Chemother Pharmacol. 2018;81(1):195–206. https://doi.org/10.1007/s00280-017-3480-9.
Kenyon EM, Calabrese EJ. Extent and implications of interspecies differences in the intestinal hydrolysis of certain glucuronide conjugates. Xenobiotica. 1993;23(4):373–81. https://doi.org/10.3109/00498259309057025.
Parker RJ, Hirom PC, Millburn P. Enterohepatic recycling of phenolphthalein, morphine, lysergic acid diethylamide (LSD) and diphenylacetic acid in the rat. Hydrolysis of glucuronic acid conjugates in the gut lumen. Xenobiotica. 1980;10(9):689–703. https://doi.org/10.3109/00498258009108376.
Heitmeier S, Visser M, Tersteegen A, et al. Pharmacological profile of asundexian, a novel, orally bioavailable inhibitor of factor XIa. J Thromb Haemost. 2022;20(6):1400–11. https://doi.org/10.1111/jth.15700.
Hirom PC, Millburn P, Smith RL, et al. Species variations in the threshold molecular-weight factor for the biliary excretion of organic anions. Biochem J. 1972;129(5):1071–7. https://doi.org/10.1042/bj1291071.
Sharifi M, Ghafourian T. Estimation of biliary excretion of foreign compounds using properties of molecular structure. AAPS J. 2014;16(1):65–78. https://doi.org/10.1208/s12248-013-9541-z.
Acknowledgments
The authors thank all the volunteers who participated in the study and also the investigator, Renger Tiessen, MD, PRA Health Science (now ICON plc), Groningen, Netherlands, for their assistance in conducting the study. The following also receive thanks: Susanne Huke for conducting the BDC rat experiment; Martina Blombach, Torsten Löffler, and Andreas Schreiber for technical support with the analyses conducted for the mass-balance studies; Dirk Gäfke for performing HPLC-HRMS quantification of metabolites and technical support with the in vitro incubations and chemical structure elucidation; Dorina van der Mey, PhD, for pharmacokinetic support in designing the study; and Alexander Schriewer, PhD, Swiss BioQuant AG, Reinach, Switzerland for bioanalytical support for the quantification of asundexian and metabolite M10 in human plasma. The authors also thank Jim Purvis, PhD, of Oxford PharmaGenesis, Oxford, UK, for providing medical writing support in accordance with Good Publication Practice 2022 (GPP 2022) guidelines (https://www.ismpp.org/gpp-2022). Editorial support was provided by Oxford PharmaGenesis, Oxford, UK.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The studies were funded by Bayer AG. Medical writing and editorial assistance were provided by Oxford PharmaGenesis, Oxford, UK, funded by Bayer AG.
Conflicts of Interest
IP, DL, SS, CB, WJ, LF, SH, and FK are employees of Bayer AG and own shares or share options. AE and MG were employees of Bayer AG at the time of conducting the study and data analysis.
Availability of Data and Material
The data that support the findings of this study are available from the corresponding author, FK, upon reasonable request.
Ethics Approval
The conduct of this clinical study met all local legal and regulatory requirements. The study was conducted in accordance with the ethical principles that have their origin in the Declaration of Helsinki and the International Council for Harmonisation guideline E6, Good Clinical Practice, and in accordance with Dutch drug law. The protocol was reviewed and approved by the study site’s Independent Ethics Committee (IEC, Stichting Beoordeling Ethiek Biomedisch Onderzoek, Assen, Netherlands).
Consent to Participate
A signed informed consent form was provided by each participant after being allowed ample time to read the form and ask questions about the procedures.
Consent for Publication
Not applicable.
Code Availability
Not applicable.
Authorship Contribution (Alphabetical Order)
Participated in research design: Dieter Lang, Friederike Kanefendt, Isabel Piel, Lukas Fiebig, Michael Gerisch, Simone I. Schulz. Conducted experiments: Anna Engelen, Dieter Lang, Isabel Piel, Simone I. Schulz, Stefan Heitmeier, Wiebke Janssen. Performed data analysis: Anna Engelen, Christine Brase, Dieter Lang, Friederike Kanefendt, Isabel Piel, Lukas Fiebig, Michael Gerisch, Simone I. Schulz, Stefan Heitmeier. Wrote or contributed to the writing of the manuscript: Anna Engelen, Christine Brase, Dieter Lang, Friederike Kanefendt, Isabel Piel, Lukas Fiebig, Michael Gerisch, Simone I. Schulz, Stefan Heitmeier, Wiebke Janssen.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Piel, I., Engelen, A., Lang, D. et al. Metabolism and Disposition of the Novel Oral Factor XIa Inhibitor Asundexian in Rats and in Humans. Eur J Drug Metab Pharmacokinet 48, 411–425 (2023). https://doi.org/10.1007/s13318-023-00838-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13318-023-00838-4