Abstract
Background and Objective
Elexacaftor/tezacaftor/ivacaftor is highly effective in treating people with cystic fibrosis (pwCF) who have ≥ 1 responsive mutation. Liver disease occurs in approximately 10%–20% of pwCF. The objective of this study was to assess the safety and pharmacokinetics of elexacaftor/tezacaftor/ivacaftor in people with moderate hepatic impairment, which is necessary to inform on its use and guide dosing recommendations.
Methods
The safety and pharmacokinetics of elexacaftor/tezacaftor/ivacaftor were evaluated in subjects without CF with moderate hepatic impairment versus matched healthy controls. Twenty-two subjects (11 with moderate hepatic impairment and 11 healthy subjects) received half the standard adult daily dose of elexacaftor/tezacaftor/ivacaftor (elexacaftor 100 mg/tezacaftor 50 mg/ivacaftor 150 mg) orally for 10 days.
Results
Elexacaftor/tezacaftor/ivacaftor was safe and well tolerated in subjects with moderate hepatic impairment and healthy controls. On day 10, the mean values of the area under the curve during the dosing interval (AUCτ) for total (bound and unbound) elexacaftor and its major active metabolite M23-elexacaftor were increased 1.25-fold (95% CI 1.01, 1.54) and 1.73-fold (95% CI 1.27, 2.35), respectively, in subjects with moderate hepatic impairment compared with matched healthy subjects. The mean values of AUCτ for ivacaftor and tezacaftor were increased 1.50-fold (95% CI 1.09, 2.06) and 1.20-fold (95% CI 1.00, 1.43), respectively, while the mean value of AUCτ for the active metabolite M1-tezacaftor was 1.29-fold lower [ratio of moderate hepatic impairment to healthy subjects (95% CI): 0.778 (0.655, 0.924)] in subjects with moderate hepatic impairment.
Conclusions
A dose reduction of elexacaftor/tezacaftor/ivacaftor is warranted in people with moderate hepatic impairment. (Trial registry number 2018-002570-40; registered 2 July 2018.)
Plain Language Summary
Elexacaftor/tezacaftor/ivacaftor is a combination product (made up of the three drugs elexacaftor, tezacaftor, and ivacaftor) that can effectively treat cystic fibrosis (CF). About 10%–20% of people with CF have liver disease, and the liver plays an important role in breaking down these drugs. Thus, it is important to understand how liver disease or reduced liver function affects the amounts of these drugs in the body over time. This can help determine how much of the drug (i.e., what dose) people should take.
We gave people with reduced liver function and healthy people (with normal liver function) elexacaftor/tezacaftor/ivacaftor for 10 days. We looked at the safety of the combination and measured the amounts of elexacaftor, tezacaftor, and ivacaftor in the body over time.
We found that when people with moderately reduced liver function take elexacaftor/tezacaftor/ivacaftor, they have higher amounts of the drugs elexacaftor, tezacaftor, and ivacaftor in their bodies compared with healthy people with normal liver function. These findings mean that people with moderately reduced liver function should take a lower dose of elexacaftor/tezacaftor/ivacaftor.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Elexacaftor/tezacaftor/ivacaftor was safe and well tolerated over 10 days of treatment |
The exposures of elexacaftor, M23-elexacaftor, tezacaftor, and ivacaftor were increased in subjects with moderate hepatic impairment compared with healthy controls |
A dose reduction is warranted when elexacaftor/tezacaftor/ivacaftor is administered to people with moderate hepatic impairment; elexacaftor/tezacaftor/ivacaftor should not be administered to people with severe hepatic impairment |
1 Introduction
Cystic fibrosis (CF) is a life-shortening autosomal recessive disease that affects > 80,000 people worldwide [1,2,3,4]. It is caused by mutations in the gene encoding the cystic fibrosis transmembrane conductance regulator (CFTR) protein that lead to a reduced quantity or to reduced function of the CFTR ion channel [1, 5,6,7]. This ion channel dysfunction results in multisystemic disease, including obstructive lung disease, exocrine and endocrine pancreatic insufficiency, and hepatobiliary disease [5, 6].
CFTR modulators are small-molecule therapeutics that target the underlying cause of CF by improving the function of the CFTR protein at the cell surface (e.g., ivacaftor) or by facilitating the processing and trafficking of CFTR to the cell surface (e.g., tezacaftor and elexacaftor) [8,9,10]. Clinical trials have established the safety and efficacy of CFTR modulators [8, 11,12,13,14,15], including the triple-combination regimen of elexacaftor/tezacaftor/ivacaftor [8, 12]. Elexacaftor/tezacaftor/ivacaftor is approved for the treatment of CF with a recommended daily dose of elexacaftor 200 mg/tezacaftor 100 mg/ivacaftor 150 mg in the morning and ivacaftor 150 mg in the evening in people aged 12 years and older with normal hepatic function [16].
The pharmacokinetics of elexacaftor, tezacaftor, and ivacaftor have been previously characterized following the recommended daily dose in people with CF (pwCF) aged 12 years and older [16]. The median (range) values of time to reach maximum concentration (Tmax) were 6 h (4–12) for elexacaftor, 3 h (2–4) for tezacaftor, and 4 h (3–6) for ivacaftor [16]. All three drugs reached steady-state concentrations within 8 days [16]. The values of the mean (SD) apparent volume of distribution ranged from 53.7 (17.7) L for elexacaftor to 82.0 (22.3) L for tezacaftor and 293 (89.8) L for ivacaftor [16]. Elexacaftor demonstrated >99% protein binding, and both tezacaftor and ivacaftor were approximately 99% protein bound [16]. Elexacaftor and tezacaftor primarily bind to albumin, while ivacaftor primarily binds to albumin, α1-acid glycoprotein, and human γ-globulin [16]. All three drugs are predominantly metabolized by the liver, with minimal renal elimination [16]. In vitro studies showed that elexacaftor, tezacaftor, and ivacaftor are all metabolized by CYP3A [16]. The mean (SD) effective half-life (t1/2) was 27.4 (9.31) h for elexacaftor, 25.1 (4.93) h for tezacaftor, and 15.0 (3.92) h for ivacaftor [16]. All are primarily excreted in the feces and urine [16].
Among pwCF, the prevalence of liver disease of various etiologies ranges from 10 to 20% [3, 4]. The prevalence of liver disease peaks in adolescence through early adulthood, and the prevalence of liver disease in adults is approximately 11% in the United States [3]. Liver disease can affect all pharmacokinetic processes, including drug absorption, distribution, metabolism, and elimination [17, 18]. Decreased plasma protein binding, resulting from lower levels of plasma albumin and α1-acid glycoprotein and/or altered binding affinity for these proteins, can alter drug distribution in people with hepatic impairment [17, 18]. Therefore, hepatic impairment may result in altered pharmacokinetics of elexacaftor, tezacaftor, ivacaftor, and their respective metabolites, and people with impaired hepatic function may have significantly higher systemic drug concentrations if given a standard dose.
Previous studies characterized the effect of moderate hepatic impairment on the pharmacokinetics of ivacaftor and tezacaftor in a study of ivacaftor monotherapy and a study of ivacaftor administered in combination with tezacaftor [19,20,21]. In these studies, ivacaftor area under the curve (AUC) was approximately 1.5-fold to 2.0-fold higher and tezacaftor AUC was approximately 1.4-fold higher in subjects with moderate hepatic impairment relative to matched healthy subjects [19,20,21]. Based on these results, it is recommended that the dose of ivacaftor should be reduced to 50% of that recommended in people with normal hepatic function when administered alone or in combination with tezacaftor in pwCF with moderate hepatic impairment [19, 20], while no dose reduction of tezacaftor is recommended in people with moderate hepatic impairment [19].
Assessment of the safety and pharmacokinetics of elexacaftor/tezacaftor/ivacaftor in people with moderate hepatic impairment is necessary to inform on its use and guide dosing recommendations in pwCF with impaired hepatic function. The primary objective of this study was to determine the effect of moderate hepatic impairment on the pharmacokinetics of elexacaftor, tezacaftor, ivacaftor, and their respective major active metabolites (M23-elexacaftor and M1-tezacaftor: major active metabolites with similar potencies relative to elexacaftor and tezacaftor, respectively [16, 19]) following administration of elexacaftor/tezacaftor/ivacaftor. The secondary objective was to assess the safety and tolerability of multiple doses of elexacaftor/tezacaftor/ivacaftor in subjects with moderate hepatic impairment and matched healthy subjects. These assessments also highlight an effective approach to evaluating the interactions between the components of a three-drug fixed-dose combination therapy and extrinsic factors, such as hepatic impairment.
2 Methods
2.1 Subjects, Trial Design, and Oversight
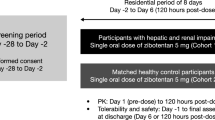
This was a phase 1, open-label, multiple-dose study evaluating the pharmacokinetics of elexacaftor/tezacaftor/ivacaftor and their respective metabolites following oral administration of elexacaftor/tezacaftor/ivacaftor in subjects without CF with moderate hepatic impairment compared with matched healthy subjects (Fig. 1). Subjects were enrolled at two sites in Europe (Czech Republic and Slovakia). Subjects aged 18 to 65 years, inclusive, were eligible. Subjects with moderate hepatic impairment were eligible if they met the criteria for Child–Pugh class B hepatic impairment in the scoring range of 7–9 [22, 23]. A complete list of eligibility criteria is provided in Table S1 in the Supplementary Information. A parallel-cohort design was used to compare the pharmacokinetics in subjects with moderate hepatic impairment with that in healthy subjects. Subjects without CF were evaluated because it is not feasible to conduct this study in subjects with CF; however, conducting hepatic impairment studies in adult subjects without CF is consistent with regulatory guidance [23]. Further, it is known that the pharmacokinetics of ELX/TEZ/IVA in subjects without CF is similar to that in subjects with CF [16]. Once a subject with moderate hepatic impairment had enrolled and completed treatment, a matched healthy subject was enrolled to ensure a 1:1 match. Healthy subjects were matched to subjects with moderate hepatic impairment for cigarette-smoking habit (nonsmoking or smoking ≤ 10 cigarettes per day), age (± 10 years, within the allowed age range), sex, and weight (± 10 kg). Subjects with moderate hepatic impairment were allowed to continue preapproved prescription medications if needed, provided they were on a stable dose and/or stable treatment regimen. A list of approved concomitant medications is provided in Table S2 in the Supplementary Information; these medications are considered the standard of care for some patients with moderate hepatic impairment, but do not include medications for the treatment of active liver disease (i.e., infectious hepatitis).
Study design. Enrollment started with subjects with moderate hepatic impairment. Once a subject with moderate hepatic impairment had been enrolled and had completed the treatment period, a matched healthy subject was enrolled. CRU clinical research unit, ELX elexcaftor, IVA ivacaftor, qd daily, TEZ tezacaftor
Elexacaftor 100 mg/tezacaftor 50 mg/ivacaftor 150 mg (administered as one elexacaftor 100 mg/tezacaftor 50 mg/ivacaftor 75 mg fixed-dose combination tablet and one ivacaftor 75 mg tablet at the same time) was administered orally daily for 10 days. The dose selected for this study was 50% of the approved daily dose in pwCF with normal hepatic function to account for any unanticipated increases in analyte exposures in the hepatically impaired population [16]. A safety follow-up visit occurred 10 (±2) days after the last dose of the study drug. Blood samples (4–6 mL) were collected at the following time points for pharmacokinetic analysis: 0 (predose), 1, 2, 3, 4, 6, 8, 12, and 24 h after the day 1 dose; 0 h (predose) on days 8 and 9; and 0 (predose), 1, 2, 3, 4, 6, 8, 12, 24, 48, 72, 96, 120, and 144 h after the day 10 dose. All investigational product and biological samples were stored in a secured area, under recommended storage conditions, and, in accordance with applicable regulatory requirements, each enrolled subject provided informed consent. This study was conducted in accordance with the current Good Clinical Practice Guidelines as described by the International Council for Harmonization, the Declaration of Helsinki, and local applicable laws and regulations. The study protocol and informed consent forms were reviewed and approved by an independent ethics committee or internal review board for each study site.
2.2 Bioanalytical Assay
Samples were analyzed using a validated liquid chromatography–tandem mass spectroscopy (LC-MS/MS) method (Vertex; data on file). Following the addition of stable isotope internal standards (25 μL of 5.00 μg/mL d5-elexacaftor and 2.50 μg/mL d5-M23-elexacaftor), analytes were extracted into ethyl acetate using a liquid–liquid extraction method. The supernatant was evaporated and reinstated in acetonitrile:water (1:1). Separation was achieved using a reversed-phase high-performance liquid chromatography column (Supelco Ascentis Express C18, 2 cm × 2.1 mm, 2.7 μm). The mobile phase consisted of 0.1% formic acid in water as mobile phase A and acetonitrile:methanol (1:1) as mobile phase B. A linear gradient was run as follows: 0 min 70% B; 1.30 min 70% B; 1.35 min 100% B; 1.70 min 20% B; 2.0 min 70% B, with a flow rate of 0.5 mL/min. The total run time was approximately 4 min per sample.
An AB Sciex API-4000 LC–MS/MS system with positive electrospray ionization and multiple reaction monitoring was used to quantify elexacaftor and M23-elexacaftor. The source settings for temperature, curtain gas, entrance potential, collision gas, and collision cell exit potential were 500 °C, 20 psi, 10 V, 6 psi, and 12 V, respectively. The multiple reaction monitoring transitions are listed in Table S3 in the Supplementary Information. Data were collected using Analyst version 1.63 (AB Sciex) and analyzed using Watson LIMS version 7.5 (Thermo Scientific). The calibration curve ranged from 10.0 to 10,000 ng/mL for elexacaftor and from 5.00 to 5000 ng/mL for M23-elexacaftor. Quality control standards were prepared at 0.500/0.250 μg/ml, 1.00/0.500 μg/ml, 5.00/2.50 μg/ml, 1 0./5.00 μg/ml, 20.0/10.0 μg/ml, 200/100 μg/ml, 450/225 μg/ml, and 500/250 μg/ml for elexacaftor/M-23-elexacaftor. The assay met the criteria for linearity, precision, recovery, sensitivity, selectivity, specificity, stability, and dilution effects specified by FDA and EMA guidance on bioanalytical method validation. Samples below the limit of quantification were reported as such; samples above the limit of quantification were diluted within the assay range and re-assayed per a validated dilution process.
2.3 Endpoints
The primary endpoints were pharmacokinetic parameters, including maximum observed concentration (Cmax), tmax, area under the concentration versus time curve during the dosing interval (AUCτ), and t1/2 values of elexacaftor, tezacaftor, ivacaftor, and their respective metabolites, and the fraction of unbound elexacaftor in the plasma (the unbound fraction of elexacaftor was evaluated in accordance with regulatory guidance [22] as it is highly plasma protein bound [19, 20]; the unbound fractions of tezacaftor and ivacaftor have been previously characterized and were not evaluated in this study). The secondary endpoint was the safety and tolerability of elexacaftor in combination with tezacaftor and ivacaftor, as determined by adverse events (AEs), clinical laboratory assessments, standard 12-lead electrocardiograms (ECGs), and vital signs.
AEs were assessed, documented, and reported in accordance with the Good Clinical Practice Guidelines as described by the International Council for Harmonization. An AE was defined as any untoward medical occurrence in a subject during the study, including any newly occurring event or worsening of a pre-existing condition. Events did not need to have a causal relationship with the study drug to be considered AEs. The severity of AEs was graded according to US Food and Drug Administration guidance [24] and is described in Table S4 in the Supplementary Information. A serious adverse event (SAE) was defined as any AE that was fatal, life-threatening, resulted in inpatient hospitalization or prolongation of hospitalization, resulted in persistent or significant disability or incapacity, resulted in a congenital anomaly or birth defect, or required medical or surgical intervention to prevent any of the aforementioned outcomes.
2.4 Statistical Analysis
Assuming that AUCτ and Cmax values are log-normally distributed with coefficients of variation (CVs) of < 20% for elexacaftor and tezacaftor and < 30% for ivacaftor (unpublished data), it was determined that data from 10 subjects in each cohort would provide ≥90% confidence that the estimated mean ratios between the two cohorts for AUCτ and Cmax would be within approximately 15% of the true ratios for elexacaftor and tezacaftor and within approximately 25% of the true ratios for ivacaftor.
The following pharmacokinetic parameters of elexacaftor, tezacaftor, ivacaftor, and the metabolites M23-elexacaftor and M1-tezacaftor in plasma were determined by noncompartmental analysis via Phoenix WinNonlin and summarized using descriptive statistics: tmax, Cmax, AUCτ, and t1/2. Body weight was not included in the pharmacokinetic calculations because all subjects received the same dose, regardless of weight. The effect of hepatic impairment on the pharmacokinetics of elexacaftor, tezacaftor, ivacaftor, and their respective metabolites was evaluated by performing analysis of natural log transformations of Cmax and AUCτ using linear mixed-effects models with cohort as a fixed variable. The ratios for the geometric least-squares means of the pharmacokinetic parameters between the two cohorts and 90% CIs were calculated. Safety was assessed with descriptive statistics based on all subjects who received ≥1 dose of study drug.
3 Results
3.1 Population
A total of 22 subjects (n = 11 subjects with moderate hepatic impairment and n = 11 matched healthy subjects) were enrolled at two sites in Europe: in the Czech Republic and Slovakia. All subjects completed treatment. Demographics and baseline characteristics were similar between subjects with moderate hepatic impairment and matched healthy subjects (Table 1). The mean (SD) age of all subjects was 51.8 (9.2) years, and the mean (SD) body mass index (BMI) was 28.35 (4.07) kg/m2. All subjects were white, and 18 (81.8%) were male.
Concomitant medications were used by 11 subjects (100.0%) with moderate hepatic impairment and one matched healthy subject (9.1%). The most common concomitant medications among subjects with moderate hepatic impairment (taken by ≥20% of subjects) were carvedilol (n = 6 [54.5%]), Silybum marianum (milk thistle; n = 6 [54.5%]), ursodiol (n = 6 [54.5%]), furosemide (n = 4 [36.4%]), and omeprazole (n = 4 [36.4%]). One matched healthy subject (9.1%) received cholecalciferol, calcium, and formoterol.
3.2 Pharmacokinetics
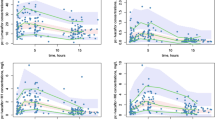
The pharmacokinetic parameters of elexacaftor and its active metabolite, M23-elexacaftor, are summarized in Table 2. On day 10, the median tmax of elexacaftor was similar between groups (approximately 4 h), and the median tmax of M23-elexacaftor was 3 h in subjects with moderate hepatic impairment and approximately 4 h in matched healthy subjects. The mean t1/2 of elexacaftor was approximately 37 h in the moderate hepatic impairment group, compared with approximately 21 h in matched healthy subjects, and the mean t1/2 of M23-elexacaftor was approximately 37 h in the moderate hepatic impairment group and approximately 24 h in matched healthy subjects (Table 2). The mean metabolic ratio of M23-elexacaftor was 0.457 in the moderate hepatic impairment group and 0.341 in matched healthy subjects. Elexacaftor AUCτ and Cmax on day 10 were 1.25-fold and 1.12-fold higher, respectively, in subjects with moderate hepatic impairment relative to matched healthy subjects (Table 3). M23-elexacaftor AUCτ and Cmax on day 10 were 1.73-fold and 1.70-fold higher, respectively, in the moderate hepatic impairment group relative to matched healthy subjects (Table 3). The combined elexacaftor and M23-elexacftor AUCτ and Cmax were 1.36-fold and 1.24-fold higher, respectively, in subjects with moderate hepatic impairment relative to matched healthy subjects (Table 3, Fig. 2, and Fig. S1 in the Supplementary Information). The mean percentages of unbound elexacaftor and M23-elexacaftor were 26% and 28% higher, respectively, in subjects with moderate hepatic impairment relative to matched healthy subjects (Table S5 in the Supplementary Information). The mean plasma concentrations of elexacaftor and M23-elexacaftor on day 10 are shown in Fig. S2 in the Supplementary Information.
Area under the curve (AUC) of A combined elexacaftor (ELX) and M23-elexacftor (M23-ELX), B, D tezacaftor (TEZ), and C, E, F ivacaftor (IVA) in subjects with moderate hepatic impairment versus matched healthy subjects.a,b AUC0-inf AUC from time 0 to infinity, AUCτ AUC during the dosing interval. a The line inside the box represents the median. The ends of the box are the 25th and 75th percentiles. The whiskers denote the lowest and highest values (excluding values considered to be outliers). Values beyond the whiskers (shown as triangles) are considered outliers. b Panels A–C reflect the AUCτ following 10 days of elexacaftor/tezacaftor/ivacaftor. Panels D–E reflect the AUCτ after 10 days of tezacaftor/ivacaftor in a previous study. Panel F reflects the AUC0-inf after a single dose of ivacaftor in a previous study
The pharmacokinetic parameters of tezacaftor and the metabolite M1-tezacaftor are summarized in Table 2. On day 10, the median tmax values for tezacaftor and M1-tezacaftor were similar between subjects with moderate hepatic impairment and matched healthy subjects (Table 2). The mean t1/2 of tezacaftor was 99.5 h in subjects with moderate hepatic impairment and 74.8 h in matched healthy subjects on day 10 (Table 2). Tezacaftor AUCτ was 1.20-fold higher in subjects with moderate hepatic impairment, while tezacaftor Cmax was similar between groups (Table 3, Fig. 2, and Fig. S1). M1-tezacaftor AUCτ was 1.29-fold lower and M1-tezacaftor Cmax was 1.25-fold lower in subjects with moderate hepatic impairment relative to matched healthy subjects (Table 3). The mean plasma concentrations of tezacaftor on day 10 are shown in Fig. S3 in the Supplementary Information.
The pharmacokinetic parameters of ivacaftor are summarized in Table 2. On day 10, the median tmax for ivacaftor was similar between subjects with moderate hepatic impairment and matched healthy subjects (Table 2). The mean t1/2 of ivacaftor was 23.5 h in the moderate hepatic impairment group and 14.0 h in matched healthy subjects (Table 2). Ivacaftor AUCτ was 1.50-fold higher in subjects with moderate hepatic impairment relative to matched healthy subjects, and ivacaftor Cmax was 1.10-fold higher in subjects with moderate hepatic impairment (Table 3, Fig. 2, and Fig. S1). The mean plasma concentrations of ivacaftor on day 10 are shown in Fig. S3.
3.3 Safety
There were no deaths, serious AEs, or AEs leading to treatment interruption or discontinuation. Four (18.2%) subjects had AEs: three (27.3%) subjects with moderate hepatic impairment (body temperature increased [n = 1], gastroenteritis [n = 1], and headache [n = 1]) and one (9.1%) healthy subject (γ-glutamyl transferase increased). All AEs were mild or moderate in severity. There were no clinically meaningful trends in laboratory values, vital signs, physical examinations, or ECG parameters.
4 Discussion
In this phase 1 open-label study, we evaluated the safety and pharmacokinetics of the three-drug, fixed-dose combination of elexacaftor/tezacaftor/ivacaftor in subjects without CF with moderate hepatic impairment in order to inform on its use and guide dosing recommendations in pwCF with impaired hepatic function.
Elexacaftor/tezacaftor/ivacaftor administered for 10 days at 50% of the dose recommended for pwCF with normal hepatic function was safe and well tolerated in subjects with moderate hepatic impairment and matched healthy subjects. The exposures of elexacaftor, M23-elexacaftor, tezacaftor, and ivacaftor were higher in subjects with moderate hepatic impairment compared with matched healthy subjects, while M1-tezacaftor exposures were lower. Relative exposures of tezacaftor and ivacaftor were consistent with previous studies of subjects with moderate hepatic impairment [19,20,21]. Given that M23-elexacaftor has a similar potency to elexacaftor [16] and accounts for approximately 17% of the total elexacaftor exposure (unpublished data), the exposures of elexacaftor combined with M23-elexacaftor were also evaluated. The resultant combined exposures of elexacaftor and M23-elexacaftor were higher in subjects with moderate hepatic impairment relative to matched healthy subjects.
The decreased exposure of the metabolite M1-tezacaftor is likely due to a reduced capacity to metabolize tezacaftor to form M1-tezacaftor in subjects with moderate hepatic impairment. In contrast, the exposure of M23-elexacaftor was increased in subjects with moderate hepatic impairment. Because M23-elexacaftor is not a terminal metabolite [16], this may be attributed to a reduced ability to further metabolize M23-elexacaftor into its respective metabolites in subjects with moderate hepatic impairment [19,20,21].
A limitation of this study was its population of otherwise healthy subjects, who, aside from moderate hepatic impairment, may have different pathophysiologies of liver disease than pwCF. However, similar exposures are expected among pwCF compared with healthy subjects [16]. Additionally, all subjects in this study were white, and most were male. Although a large majority of pwCF are white (> 90% in 2020), almost 50% of pwCF are female [3, 4, 25]. However, it is known that the pharmacokinetics of ELX/TEZ/IVA are similar in males and females [16]; therefore, despite this limitation, the results of this study are likely generalizable to both sexes. Potential interactions with concomitant medications, including ursodiol, which—like elexacaftor, tezacaftor, and ivacaftor—is metabolized by CYP3A [26], cannot be excluded. Finally, the relatively small sample size (n = 22) of this study may limit the interpretation of these results; however, the sample size is consistent with regulatory guidance [22].
This study demonstrates that exposures of elexacaftor and M23-elexacaftor are increased in subjects without CF with moderate hepatic impairment relative to matched healthy controls following administration of elexacaftor in combination with tezacaftor and ivacaftor. Exposures of tezacaftor and ivacaftor are also increased, while exposures of M1-tezacaftor are decreased in subjects with moderate hepatic impairment, consistent with earlier studies. Use of ELX/TEZ/IVA is not recommended in patients with moderate hepatic impairment unless the benefit exceeds the risk and, if used, ELX/TEZ/IVA should be used with caution at a reduced dose according to the prescribing information [16]. Dosing recommendations for a combination product in people with hepatic impairment derived from each component studied separately as monotherapy may not account for unexpected interactions between each of the components when given together in this population. For example, an increase in exposure of one component could alter drug–drug interactions between the components and lead to a different recommendation than would be made from studying each component alone. In this hepatic impairment study, we evaluated all components of a three-drug combination product together to ensure that the exposures of all components and their metabolites were fully characterized. Furthermore, we utilized all available data from the individual components studied as monotherapy and as combination products to inform the final dose recommendation.
5 Conclusions
Based on these findings, treatment with elexacaftor/tezacaftor/ivacaftor should be modified in pwCF with moderate hepatic impairment according to the prescribing information [16]. If used in pwCF with moderate hepatic impairment, elexacaftor/tezacaftor/ivacaftor should be used with caution at a reduced dose [16]. Elexacaftor/tezacaftor/ivacaftor should not be used in patients with severe hepatic impairment [16]. ELX/TEZ/IVA may used in pwCF with mild hepatic impairment, and no dose adjustment is needed in patients with mild hepatic impairment [16].
References
Bell SC, Mall MA, Gutierrez H, Macek M, Madge S, Davies JC, et al. The future of cystic fibrosis care: a global perspective. Lancet Respir Med. 2020;8(1):65–124.
Elborn JS. Cystic fibrosis. Lancet. 2016;388(10059):2519–31.
Cystic Fibrosis Foundation. 2019 Patient registry annual data report. https://www.cff.org/Research/Researcher-Resources/Patient-Registry/2019-Patient-Registry-Annual-Data-Report/. Accessed 3 Sep 2021.
ECFS. 2018 Patient registry annual report. https://www.ecfs.eu/sites/default/files/general-content-files/working-groups/ecfs-patient-registry/ECFSPR_Report_2018_v1.4.pdf. Accessed 3 Sep 2021.
O’Sullivan BP, Freedman SD. Cystic fibrosis. Lancet. 2009;373(9678):1891–904.
Ratjen F, Bell SC, Rowe SM, Goss CH, Quittner AL, Bush A. Cystic fibrosis. Nat Rev Dis Primers. 2015;1:15010.
Riordan JR, Rommens JM, Kerem B, Alon N, Rozmahel R, Grzelczak Z, et al. Identification of the cystic fibrosis gene: cloning and characterization of complementary DNA. Science. 1989;245(4922):1066–73.
Keating D, Marigowda G, Burr L, Daines C, Mall MA, McKone EF, et al. VX-445-tezacaftor-ivacaftor in patients with cystic fibrosis and one or two Phe508del alleles. N Engl J Med. 2018;379(17):1612–20.
Sala MA, Jain M. Tezacaftor for the treatment of cystic fibrosis. Expert Rev Respir Med. 2018;12(9):725–32.
Van Goor F, Hadida S, Grootenhuis PD, Burton B, Cao D, Neuberger T, et al. Rescue of CF airway epithelial cell function in vitro by a CFTR potentiator, VX-770. Proc Natl Acad Sci USA. 2009;106(44):18825–30.
De Boeck K, Munck A, Walker S, Faro A, Hiatt P, Gilmartin G, et al. Efficacy and safety of ivacaftor in patients with cystic fibrosis and a non-G551D gating mutation. J Cyst Fibros. 2014;13(6):674–80.
Middleton PG, Mall MA, Drevinek P, Lands LC, McKone EF, Polineni D, et al. Elexacaftor-tezacaftor-ivacaftor for cystic fibrosis with a single Phe508del allele. N Engl J Med. 2019;381(19):1809–19.
Ramsey BW, Davies J, McElvaney NG, Tullis E, Bell SC, Drevinek P, et al. A CFTR potentiator in patients with cystic fibrosis and the G551D mutation. N Engl J Med. 2011;365(18):1663–72.
Rowe SM, Daines C, Ringshausen FC, Kerem E, Wilson J, Tullis E, et al. Tezacaftor-ivacaftor in residual-function heterozygotes with cystic fibrosis. N Engl J Med. 2017;377(21):2024–35.
Taylor-Cousar JL, Munck A, McKone EF, van der Ent CK, Moeller A, Simard C, et al. Tezacaftor-ivacaftor in patients with cystic fibrosis homozygous for Phe508del. N Engl J Med. 2017;377(21):2013–23.
Vertex Pharmaceuticals Incorporated. Trikafta prescribing information. Boston, MA: Vertex Pharmaceuticals Incorporated; 2020. https://pi.vrtx.com/files/uspi_elexacaftor_tezacaftor_ivacaftor.pdf. Accessed 16 Nov 2021.
Palatini P, De Martin S. Pharmacokinetic drug interactions in liver disease: an update. World J Gastroenterol. 2016;22(3):1260–78.
Verbeeck RK. Pharmacokinetics and dosage adjustment in patients with hepatic dysfunction. Eur J Clin Pharmacol. 2008;64(12):1147–61.
Vertex Pharmaceuticals Incorporated. Symdeko prescribing information. Boston, MA: Vertex Pharmaceuticals Incorporated; 2020.
Vertex Pharmaceuticals Incorporated. Kalydeco prescribing information. Boston, MA: Vertex Pharmaceuticals Incorporated; 2020.
Viswanathan L, Lekstrom-Himes J, Garg V, Agarwal S. P024 Effects of food and moderate hepatic impairment on the pharmacokinetics (PK) of tezacaftor/ivacaftor (TEZ/IVA). J Cyst Fibros. 2018;17:S65–6.
US Food and Drug Administration. Pharmacokinetics in patients with impaired hepatic function: study design, data analysis, and impact on dosing and labeling. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/pharmacokinetics-patients-impaired-hepatic-function-study-design-data-analysis-and-impact-dosing-and. Accessed 3 Sep 2021.
European Medicines Agency. Guideline on the evaluation of the pharmacokinetics of medicinal products in patients with impaired hepatic function. https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-evaluation-pharmacokinetics-medicinal-products-patients-impaired-hepatic-function_en.pdf. Accessed 3 Sep 2021.
US Food and Drug Administration. Toxicity grading scale for healthy adult and adolescent volunteers enrolled in preventive vaccine clinical trials. https://www.fda.gov/media/73679/download. Accessed 21 Jul 2022.
UK Cystic Fibrosis Trust. UK Cystic Fibrosis Registry 2020 annual data report. https://www.cysticfibrosis.org.uk/the-work-we-do/uk-cf-registry/reporting-and-resources. Accessed 17 Jun 2022.
Bodin K, Lindborn U, Diczfalusy U. Novel pathways of bile acid metabolism involving CYP3A4. Biochim Bophys Acta Mol Cell Biol Lipids. 2005;1687:84–93.
Acknowledgments
Editorial coordination and support were provided by Morgan Deng, PharmD, and Mazen Saeed, PharmD, of Vertex Pharmaceuticals Incorporated. MD and MS may own stock or stock options in that company. Medical writing and editorial support were provided under the direction of the authors by Jaclyn Highland, PhD, and Liz Phipps, PhD, CMPP. JH and LP are employees of ArticulateScience LLC, which received funding from Vertex Pharmaceuticals Incorporated.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
All authors received nonfinancial assistance (assistance with manuscript preparation) from ArticulateScience LLC, which received funding from Vertex Pharmaceuticals Incorporated. All authors are current or former employees of Vertex Pharmaceuticals and may own stock or stock options in the company.
Funding
This study was funded by Vertex Pharmaceuticals Incorporated.
Availability of Data and Material
Vertex is committed to advancing medical science and improving patient health. This includes the responsible sharing of clinical trial data with qualified researchers. Proposals for the use of these data will be reviewed by a scientific board. Approvals are at the discretion of Vertex and will be dependent on the nature of the request, the merit of the research proposed, and the intended use of the data. Please contact CTDS@vrtx.com if you would like to submit a proposal or need more information.
Code Availability
Not applicable.
Ethics Approval
This study was conducted in accordance with the current Good Clinical Practice Guidelines as described by the International Council for Harmonization, the Declaration of Helsinki, and local applicable laws and regulations. The study protocol and informed consent forms were reviewed and approved by an independent ethics committee or internal review board for each study site.
Consent to Participate
Each enrolled subject provided informed consent.
Consent for Publication
Not applicable.
Author Contributions
The study was designed by Vertex Pharmaceuticals Incorporated. Data gathering and analysis were performed by Vertex Pharmaceuticals Incorporated. All authors contributed to the study concept or design. LV and EB were responsible for the acquisition of data. All authors participated in the analysis and interpretation of study data, drafted and critically revised the manuscript, and gave final approval of the manuscript for publication.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Viswanathan, L., Bachman, E., Tian, S. et al. Phase 1 Study to Assess the Safety and Pharmacokinetics of Elexacaftor/Tezacaftor/Ivacaftor in Subjects Without Cystic Fibrosis With Moderate Hepatic Impairment. Eur J Drug Metab Pharmacokinet 47, 817–825 (2022). https://doi.org/10.1007/s13318-022-00791-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13318-022-00791-8