Abstract
Tardive syndrome (TS) is an iatrogenic, often persistent movement disorder caused by drugs that block dopamine receptors. It has a broad phenotype including movement (orobuccolingual stereotypy, dystonia, tics, and others) and nonmotor features (akathisia and pain). TS has garnered increased attention of late because of the Food and Drug Administration approval of the first therapeutic agents developed specifically for this purpose. This paper will begin with a discussion on pathogenesis, clinical features, and epidemiology. However, the main focus will be treatment options currently available for TS including a suggested algorithm based on current evidence. Recently, there have been significant advances in TS therapy, particularly with the development of 2 new vesicular monoamine transporter type 2 inhibitors for TS and with new data on the efficacy of deep brain stimulation. The discussion will start with switching antipsychotics and the use of clozapine monotherapy which, despite the lack of higher-level evidence, should be considered for the treatment of psychosis and TS. Anti-dyskinetic drugs are separated into 3 tiers: 1) vesicular monoamine transporter type 2 inhibitors, which have level A evidence, are approved for use in TS and are recommended first-choice agents; 2) drugs with lower level of evidence for efficacy including clonazepam, Ginkgo biloba, and amantadine; and 3) drugs that have the potential to be beneficial, but currently have insufficient evidence including levetiracetam, piracetam, vitamin B6, melatonin, baclofen, propranolol, zolpidem, and zonisamide. Finally, the roles of botulinum toxin and surgical therapy will be examined. Current therapies, though improved, are symptomatic. Next steps should focus on the prevention and reversal of the pathogenic process.
Similar content being viewed by others
Introduction
Tardive syndrome (TS) is an iatrogenic, clinically heterogeneous, and often persistent movement disorder caused by drugs that block dopamine receptors including antipsychotics and anti-emetics. The syndrome can be seen in patients with and without psychiatric disease and can result in embarrassment, disability, and deformity. It is associated with adverse healthcare outcomes and diminished quality of life [1, 2]. Although first described in the 1950s [3,4,5], and later named in 1964 to reflect recognition that the disorder was seen after chronic use of the agents [6], it is only in the last 3 years that significant attention has turned to TS in part because of the Food and Drug Administration (FDA) approval of the first therapeutic agents developed specifically for this purpose. The terminology has evolved in recent years as well, such that the term tardive syndrome is used to include the full phenotypic spectrum of delayed and persistent movement and nonmotor disorders that occur secondary to dopamine receptor blocking agent (DRBA) exposure [7, 8]. Tardive dyskinesia in the past was used to either include the entire spectrum of tardive movement disorders or as a term for the classical repetitive orofacial syndrome. It is sometimes difficult to interpret which the authors are referring to. For the purposes of this paper, tardive syndrome is used as a term to encompass the entire spectrum, whereas tardive dyskinesia primarily refers to the classical syndrome and corresponding repetitive movements that can appear in the limbs, trunk, or pelvis (see the clinical features discussion below) [8]. The definition of TS by the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) classifies TS as “involuntary movements (lasting at least a few weeks) generally of the tongue, lower face and jaw, and extremities (but sometimes involving the pharyngeal, diaphragmatic, or trunk muscles), developing in association with the use of a neuroleptic medication for at least a few months” [9]. DSM IV previously provided specific durations of exposure of DRBAs based on the Schooler–Kane criteria [10], 3 months in general and 1 month for the elderly. In order to make a diagnosis of TS, the movement disorder must persist for at least 1 month.
Although tardive movement disorders usually appear after months or years of treatment with DRBAs, rarely they can occur even after a brief exposure (e.g., several hours or days) [8]. In this paper, we will refer to first-generation antipsychotic agents as FGA and second- and third-generation (atypical) antipsychotics combined as SGA when addressing their role in the development of TS.
This paper will include discussions on pathophysiology, clinical features, epidemiology, and treatments. Treatment will start with medications. That will be followed by discussions of botulinum toxin and surgical therapies and finished with a suggested algorithm for approaching these patients.
Pathophysiology
The pathophysiology of TS remains uncertain, but it appears to be related to a persistent hyperdopaminergic state. The prevailing hypothesis has related to an upregulation of dopamine D2 receptors with a subsequent hypersensitivity and increased affinity to dopamine [11,12,13]. This model would certainly explain why the hyperkinetic disorder develops, and why it responds to greater dopamine blockade and/or depletion of dopamine pharmacologically. However, D2 hypersensitivity alone seems to be insufficient to account for TS. It does not explain why only a fraction of patients develop TS; rodent animal models indicate that hypersensitivity of D2 receptors is present in all exposed animals, even those without the characteristic vacuous chewing movements described in the model, nor does it explain why the onset occurs after months to years of exposure since hypersensitivity in rodent models is present within days to weeks [14]. In some rodent models, both early and late (after > 6-months neuroleptic exposure) onset movements, which differ pharmacologically but not phenomenologically, have been reported with late-onset type being most likely TS from the standpoint of timing and responsiveness to anticholinergic agents [14, 15]. Another issue is that TS is often persistent, yet hypersensitivity diminishes over time in rodent models, and dopamine receptor numbers return to baseline after DRBAs are withdrawn although it takes longer with chronic exposure [15]. In rodent models, there are questions as to the relatability of the vacuous chewing movements and TS movements and the association with age and sex do not appear to impact rodent model response to antipsychotics [15]. In older rodents with an increased number of vacuous chewing movements, there may be an association with histopathological changes in the substantia nigra [16]. Further, it is not even clear that receptors become hypersensitive physiologically in rodents [17]. Attempts to develop nonhuman primate models of TS have met with species variations in incidence and phenomenology. These studies require long-term treatment and are costly [15]. Imaging, postmortem, and immunochemistry studies in humans and nonhuman primates have not been able to consistently confirm either upregulation or hypersensitivity of dopamine D2 receptors in those exposed to DRBAs [18,19,20,21,22]. As the D2 hypothesis has not found consistency, others have examined other potential mechanisms of dopamine hyperactivity. One study in nonhuman primate models found robust upregulation of D3 receptor binding in the striatum [23]. D3 hypersensitivity may potentiate D1 receptors’ enhancing activity of the direct pathway leading to hyperkinesia [14]. Alterations in the D3 receptor-dependent Akt/GSK-3β signaling cascade appear to be more specifically associated with TS in nonhuman primate models [14]. Another hypothesis relates to multifaceted changes in dopaminergic signaling. These changes include an increase in the dopamine receptors, the development of postsynaptic maladaptive synaptic plasticity with increased synapse number and synaptic morphological change (so-called perforated synapses—a splitting of synapses when the strength of dopamine signaling is increased), and presynaptic increase in dopamine release due to higher vesicular dopamine concentrations [13]. Further evidence is needed with all these hypotheses.
Two theories might explain why some patients exposed to DRBAs, but not all, develop TS. The first relates to which drug is prescribed. Some atypical agents (clozapine and quetiapine in particular) are thought to bind postsynaptic D2 receptors in the striatum loosely, they then dissociate quickly, whereas the more typical DRBAs such as haloperidol are thought to bind tightly and have long-lasting effects on the receptors [24]. In this theory, the atypical agents bind just long enough to have antipsychotic action, but only long enough to cause fewer, if any, neurological adverse effects [25, 26]. In the second theory, TS is associated with deficient adaptation of 5-HT2A, metabotropic and NMDA receptors, and vesicular monoamine transporter type 2 (VMAT2) levels in the striatum as shown in nonhuman primates chronically exposed to antipsychotic drugs [27].
Several other pathogenic hypotheses have been studied which may occur in isolation or in association with D2 hypersensitivity [28]. It is beyond the scope of this paper to discuss them in detail, but they are listed here as they are relevant to some of the drug treatments studied in TS. They include changes in glutamic acid decarboxylase and gamma-aminobutyric acid (GABA) (diminished activity) [29], opioid peptides (enkephalin and dynorphin) and their receptors (increased activity) [30], brain norepinephrine and serotonin [31], and glutamate (higher levels of N-acetylaspartate, N-acetylaspartylglutamate, and aspartate) [32]. Another theory relates to the development of oxidative stress including the finding that mitochondrial complex I activity is inhibited by neuroleptics [33]. This could conceivably lead to neurodegeneration. Structural or pathological changes have not been demonstrated consistently in humans with TS or their corresponding animal models through autopsy or neuroimaging. One hypothesis suggests that degeneration of GABAergic neurons leads to disinhibition of the nigrostriatal tract resulting in a hyperdopaminergic state. Other studies suggest there may be other regions of degeneration. Dopamine transporter imaging has demonstrated a 3-fold increase in dopamine nigrostriatal terminal loss in schizophrenia patients treated chronically with antipsychotics and may be higher in those with TS [34]. This was thought to relate to accumulation of antipsychotics in the neuromelanin of nigral dopaminergic neurons and secondary toxicity or, alternatively, reduced synthesis of dopamine transporters. A study of voxel-based structural MRI imaging demonstrated decreased volume in the caudate nucleus and putamen in chronic schizophrenia with TS compared with those without TS and healthy controls [35]. Nonhuman primate models have indicated possible degeneration of the basal nucleus and caudate nucleus [15].
Additionally, there have been several studies examining genetic variations that may explain why some patients have susceptibility to developing TS and may provide etiological clues [36, 37]. The studies are mostly small, and results are mixed but there are several standouts. For details, see the review by Zai et al. [36]. Genes that govern antipsychotic metabolism, CYP2D6, have been of great interest. It appears that high enzyme activity protects against risk for TS, whereas low functioning genotypes increase the risk. This requires further confirmation. The most promising genes associated with TS include genes impacting the dopamine system which enhance the dopamine hypersensitivity hypothesis including DRD2, DRD3, and VMAT2. In addition, heparan sulfate proteoglycan 2, serotonin 2A and 2C receptors (HTR2A, HTR2C), and manganese superoxide dismutase variants associated with TS provide potential supporting the roles of the blood–brain barrier, serotonin, and oxidative stress. One whole exome sequencing study found the regulating synaptic membrane exocytosis 2 gene as the only significant association with severe TS [38]. This requires confirmation.
Clinical Features
Tardive syndrome has a broad phenotype (shown in Table 1). There are motor and nonmotor subtypes. Motor types include the classical tardive dyskinesia syndrome characterized by orofacial dyskinesia including lip, jaw, and tongue movements but which can also include limbs and trunk. The second most common is tardive dystonia which, although it can have fairly specific features of retrocollis, truncal dystonia, and internal arm rotation, can look identical to idiopathic dystonia [39]. Other less common types include stereotypy, tic, tremor, chorea, myoclonus, and gait [40,41,42,43,44]. There are also sensory forms of TS such as akathisia and pain syndromes [45, 46]. Although they are all brought on by dopamine D2 receptor blocking agents, there are some variations in demographics and pharmacology [47]. For example, tardive dystonia is more common in young men, whereas classical tardive dyskinesia and tardive akathisia occur more frequently in older women. Tardive dystonia can improve with anticholinergic therapy, whereas the same treatment will worsen classical tardive dyskinesia and have no effect on tardive akathisia. Tardive dystonia may also be less likely to remit [48].
The onset of TS generally occurs after long-term exposure (months plus) while remaining on the antipsychotic or after lowering the dose or complete withdrawal of the drug. However, there have been cases with few or even 1 exposure, so there is no safe period. Symptoms typically begin with an insidious onset, evolving to a full syndrome over days to weeks. This is followed by a stabilization of symptoms in a chronic, but sometimes waxing and waning course [47]. The severity of TS is quite variable, ranging from mild and unnoticed by the patient to disabling and even life-threatening [49, 50]. “Withdrawal-emergent syndrome” is a form of chorea that, by definition, lasts less than a month, then remits. This is more common in children [47].
Studies of the natural history of TS have been limited and reported a wide range of remission rates for different populations (1-62%) [28]. Early studies (1970s and 1980s) suggested that about 50% of cases remitted but this included withdrawal-emergent cases [5, 51]. Most of the reported studies have been conducted in patients with schizophrenia who remained on DRBAs. Two studies have examined remission of TS after complete discontinuation of the offending agents [52, 53]. One was a prospective study of 49 psychiatric patients in whom 36 could actually stop their antipsychotics. In this study, only 2% had complete resolution and 20% showed improvement [52]. In a retrospective cohort study of 108 TS patients in whom the inciting medications were completely withdrawn (mean age 59 years, 69% females, 95% nonschizophrenic diagnosis), the mean duration of antipsychotic exposure was 4.8 years [53]. Of these cases, 42% were exposed to anti-emetic drugs with dopamine blocking effects (87% metoclopramide), 36% were on SGA, and 7% were on FGA. TS remitted with just withdrawal of the neuroleptics in 2% and resolved in an additional 11% with treatment with various agents after 3.7 years of no exposure to DRBAs. Finally, longitudinal studies of tardive dystonia demonstrated a remission rate of only ~ 10% [8].
It is beyond the scope of this paper to discuss in any detail the differential diagnosis of TS. See Table 2 for a listing.
Epidemiology
The frequency of TS has been wide-ranging over the decades since antipsychotics were approved. There are various reasons for the broad ranges that have been reported including the following: patients are frequently treated with multiple medications or combinations, varied doses, and potencies; antipsychotics can mask symptoms and hence the presence of TS may fluctuate; patients may be unaware of the presence of TS; because TS is often a secondary issue to psychiatric disease, it may not be coded during visits; and there is a varied presence of different risk factors [54, 55].
Unmodifiable patient-related and illness-related risk factors for TS include older age (2-5× increased incidence in the elderly) [37], female sex, African-American descent (2× increase), intellectual disability and brain damage, affective disorders, and cognitive symptoms associated with mood disorders. Potentially modifiable comorbidity-related and treatment-related factors include diabetes mellitus (2× increase), smoking, alcohol and substance abuse, exposure to antipsychotic drugs with higher D2 blockade effect, higher cumulative and current dose or antipsychotic plasma levels, antipsychotic drug holidays (periods where the antipsychotic therapy is held), anticholinergic exposure, and acute drug-induced movement disorders such as parkinsonism and akathisia [37, 56]. The role of pharmacogenomics in evaluating the risk of TS remains to be determined. As mentioned earlier, gene polymorphisms involving antipsychotic metabolism and dopamine functioning have been of greatest interest [11, 36, 56].
Tardive syndrome is common and probably underreported [57]. Despite the variance, there are standard figures for incidence and prevalence based on the work published in 1988 by Kane et al. indicating a point prevalence of 15% and an incidence of 5% per year which grew linearly over at least the first 5 years [58]. These were confirmed in 1993 and 1995 with further data indicating higher figures for the elderly, perhaps up to 20% per year incidence [59, 60]. As SGA were developed, early figures suggested much lower TS incidence and prevalence suggesting greater safety, but the outcome over time has been a more modest change [55]. In 2004, Correll et al. [61] examined 11 studies, 2769 patients, up to the year 2003 in a meta-analysis demonstrating 0.8% incidence for SGA versus 5.4% for FGA. But in 2008, Correll et al. [62] in another meta-analysis examined 12 additional trials published between 2004 and 2008 that included 30,198 patients demonstrated incidences that were much closer: 3.9% for SGA versus 5.5% for FGA. Six of these studies directly compared incidence rates and found figures of 4.2% and 5.5% for SGA and FGA, respectively. With time, the prevalence and incidence with SGA have approached the early figures for FGA. For example, in 2010, Woods et al. [63] performed a similar study at the same institution to the 1993 paper [59] with the main difference being that 64% of patients were now on an SGA. The annual incidence for SGA was 0.053 versus 0.066 for FGA with identical prevalence (> 30%). Several more recent studies provide supportive data that incidence and prevalence rates for FGA and SGA are similar. For example, the Clinical Antipsychotic Trials of Intervention Effectiveness trial (CATIE trial-a clinical trial of nearly 1500 patients randomized to 5 separate antipsychotics) demonstrated no difference between the 2 classes of drugs [64]. Mentzel et al. examined 447 patients treated for at least 3 years (87% treated with SGA) and found an incidence rate of 4.7% [65]. Ryu et al. examined the prevalence of TS in 80 subjects with schizophrenia or schizoaffective disorder who were never exposed to FGA. The prevalence of all tardive syndromes was 35% over a period of > 1 year of therapy [66]. Finally, recent meta-analyses were completed for prevalence and incidence comparing FGA and SGA. One examined the prevalence of TS in 41 randomized clinical trials that prescribed FGA and SGA for psychotic disorders from 2000 to 2015 (n = 11,493) [67]. TS prevalence rates were 21% for SGA and 30% for FGA which were significantly different (p = 0.002). In 20 studies, the 2 drug classes were directly compared, and the prevalence was 25.3% for SGA and 30.1% for FGA (p = 0.01). However, when the analysis was restricted to patients treated with SGA and never exposed to FGA, the prevalence was 7.2%. The annualized TS incidence across FGA versus SGA from 57 randomized trials (n = 19,859) reported from 1997 to 2018 was 6.5% and. 2.6%, respectively [68]. Although the relative risk of TS appears to be, therefore, less with SGA, it is not insignificant and the fact that SGA are more widely prescribed (especially for off-label use such as affective, sleep, and behavior disorders) suggests that the absolute number of new cases of TS may actually be increasing [69]. Data indicate that prescribing overall in the USA has increased at least 3-fold with a 10-fold increase in children [69]. These findings support the notion that the incidence of TS in 2020 is similar to that examined in the 1980s and 1990s. The key point is that SGA do not provide a substantially greater safety margin. An examination of individual agents demonstrated that all SGA were associated with significantly more drug-induced movement disorders than placebo, but there is variability between agents. Clozapine appears to have the lowest risk [70], whereas lurasidone and risperidone have the highest risk. This is difficult to measure as the figures are varied by study [68].
In addition to its association with adverse healthcare outcomes and diminished quality of life [1], TS is associated with an increased mortality rate compared to patients on antipsychotics without TS although there is no apparent specific cause associated with death [71]. Causes of death include esophageal dyskinesia and respiratory dyskinesia [48, 49].
Treatment
In 2013, the American Academy of Neurology published an evidence-based treatment guideline for TS [72]. The results were disappointing and indicated that after nearly 60 years there was very limited evidence for any treatment. There were 2 drugs with level B evidence (clonazepam and Ginkgo biloba) and 2 with level C evidence (tetrabenazine and amantadine). The rest of the more than 2 dozen treatments lacked sufficient evidence. The use of antipsychotics such as risperidone was, and is currently not, recommended because they are causative agents. They also indicated that anticholinergics should not be recommended as well. This lack of evidence is in line with a substantial drop in interest and publications from the mid-1980s [73]. This guideline was followed with an update in 2018 [74] to include data from 2 new VMAT2 inhibitors (valbenazine and deutetrabenazine) that were FDA approved in the USA in 2017. These were the first with level A evidence and multicenter, randomized, double-blind clinical trials and the first to be approved specifically for the treatment of TS [75, 76].
What these guidelines also disclosed was that evidence for the generally utilized initial steps in approaching newly diagnosed TS, stopping antipsychotics, if possible, or switching to a less potent antipsychotic (for example from an FGA to SGA) remains insufficient. These approaches, based on observations made in the 1970s [5, 77], have not been studied in a formal manner. On 1 hand, this recommendation certainly seems reasonable, because some patients do improve and reversibility, although limited, tends to be unpredictable. On the other hand, one has to wonder, based on the finding that 87% of cases are irreversible, whether once TS develops it is just too late and changing the antipsychotic may not make a difference. Further study is needed.
One intriguing aspect of this approach relates to the switch from one antipsychotic (FGA or SGA) to clozapine which is often recommended for treatment of schizophrenia patients with TS. There are some reports suggesting that clozapine is actually a rare cause of TS [78,79,80]. And evidence for clozapine use in treating TS is generally insufficient [74]. Reasons for the lack of evidence relate to its use as a second- or higher-line drug to treat psychosis because of the risk of agranulocytosis and the need to perform routine monitoring of white blood cells, which limits use and requires enrollment in the clozapine REMS program. Nevertheless, a recent meta-analysis of 4 open trials of 48 patients indicates that switching to clozapine monotherapy is nearly 3 times more likely to decrease the frequency of TS [81]. Another systematic review of 13 studies and 904 patients also demonstrated an improvement in TS [82]. In a naturalistic observational study, 35 patients with schizophrenia or bipolar disorder received clozapine monotherapy as an antipsychotic drug for more than 12 months in an attempt to treat TS [83]. Nearly 90% were switched from another SGA. TS remitted in 65.7% of the cases. In addition, there are several case reports and case series of clozapine improving severe axial tardive dystonia [84, 85], which in this author’s experience occurs over a period of months. It is unlikely that the improvement reported is the result of masking TS symptoms because of its mode of action as a fast dissociating molecule [12]. Thus, it may actually act to reverse the TS through a separate, currently unknown, mechanism. Certainly, despite the lack of higher-level evidence, switching to clozapine monotherapy should be considered for treatment of psychosis and TS.
If these steps fail to improve TS, then consideration is given for treating with anti-dyskinetic drugs. Anti-TS agents can be separated into 3 groups based first on evidence and then experience: first tier—VMAT2 inhibitors, as 2 of the 3 have level A evidence and are recommended to be first-choice agents; second tier—other drugs with lesser levels of evidence; and third tier—other drugs that have been studied, have potential to be beneficial, but have insufficient evidence.
Before discussing the treatment options, it is of interest to discuss the primary measure of TS, the Abnormal Involuntary Movement Scale (AIMS), which was developed in 1976 and is a validated scoring mechanism [86]. It is a 12-item clinically rated scale. The first 7 items measure severity of movements by location, orofacial movements, and extremity and truncal movements. Additional items include global judgment and dental status. In the studies for the newer agents, only the severity portion (items 1-7) was utilized and measured by video assessment. Each question is scored 0 (none) to 4 (severe). A 2-point decrease in AIMS severity score may be considered clinically important [87]. Criticisms of the scale include that it is overweighted toward facial movements which includes 4 items versus trunk and limbs equaling a total of 3 items. Also, tremor should not to be rated, but some examiners have difficulty differentiating tremor and dyskinesia. Scores can be quite subjective, and finally, translation to clinical practice is challenging [87].
Medical Therapy
First-Tier Drugs: VMAT2 Inhibitors (Table 3)
Mechanism
VMAT2 is a key vesicular protein that traverses the membrane and is involved in recycling dopamine, norepinephrine, and serotonin after their reuptake into the neuron from the synaptic cleft. VMAT2 shifts these monoamines from the cytosol through the membrane and sequesters them into vesicles, allowing for their storage and rapid reutilization [88]. VMAT2 inhibitors block this packaging of monoamines in the vesicles leading to rapid degradation in the cytosol by monoamine oxidase. This ultimately leads to depletion of presynaptic dopamine and other monoamines proportionate to the level of VMAT2 inhibition [89]. Three such drugs exist, and each will be discussed.
Tetrabenazine
It has been known for decades that tetrabenazine (TBZ) is effective in treating hyperkinetic movement disorders. Although it has never been specifically approved for TS, it has been used off-label for this purpose and has been considered widely to be the treatment of choice despite limited evidence [88]. The first controlled trial of TBZ in TS was published in 1972. Kazamatsuri et al. hypothesized that if abnormal movements of TS result from overactivity of dopaminergic neurons, then the abnormal movements should be suppressed by TBZ. In their study, 24 patients hospitalized with psychiatric disease (in Boston State Hospital) were enrolled in this placebo-controlled, double-blind, crossover trial. All patients were observed over a 4-week baseline period, a 4-week placebo run-in period during which neuroleptics were completely withdrawn, a 6-week TBZ treatment period while off neuroleptics, and then crossed over, after a 2-week washout, to another 6-week placebo-controlled period, again while maintained off neuroleptics. The primary outcome measure was the mean frequency of abnormal movements per minute as calculated by a blinded rater. TBZ, at doses of 100 to 150 mg/day, resulted in resolution of dyskinesia in 8 patients (33%), marked reduction in 6 (25%), and slight decrease or no change in 6 patients. There were 4 noncompleters, 2 developed severe malaise and withdrew, 1 had a “psychotic exacerbation,” and 1 was lost to follow-up after discharge. Overall, there was a significant decrease of TS movements by 60% on TBZ when compared to placebo [90]. A second trial, many years later, was reported by Ondo et al. who enrolled 20 patients, with varied underlying diagnoses including 7 with psychotic disorder and 2 with bipolar disorder, in an open-label study with doses utilized of up to 150 mg of TBZ per day. Blinded raters scored TS using the AIMS on video. A 54% (p < 0.0001) improvement was reported. Eleven patients rated themselves as markedly improved, 6 as moderately improved, and 2 as mildly improved. One patient withdrew from the study because of sedation [91]. Two retrospective reports on a larger number of subjects further supported the efficacy of TBZ for the treatment of TS [92]. One reviewed the records of 149 TS patients treated with TBZ and found a high frequency of adverse effects, including drowsiness (25%), parkinsonism (15.4%), depression (7.6%), and akathisia (7.6%) [92]. Suicidality has also been reported as a serious adverse effect of TBZ [93]. This in total represents level C evidence.
TBZ is rapidly metabolized into 2 isomers, α-dihydrotetrabenazine (DH-TBZ) and β-DH-TBZ, both of which have a high affinity for VMAT2. These isomers are metabolized by the cytochrome P450 2D6 (CYP2D6). Because of the short half-life and reliance on CYP2D6 for metabolism, TBZ is dosed 3 times daily and there is a requirement of CYP2D6 genotyping to screen for poor metabolizer status when utilizing greater than 50 mg/day. High peak concentrations and plasma fluctuations of this drug are thought to contribute to the adverse event profile [94]. These issues led to the development of 2 newer VMAT2 inhibitors to moderate the metabolic issues and improve tolerability while maintaining efficacy for TS and other hyperkinetic disorders [88].
Valbenazine
Valbenazine is a TBZ prodrug, a valine ester of a highly selective isomeric metabolite of TBZ ([+]-α-DH-TBZ) that is metabolized into the 2 most active isomers [95, 96]. Valbenazine was designed to be metabolized slowly to minimize high peak plasma concentrations, decrease peak-to-trough ratios, and reduce intersubject variability. The half-life for active metabolites is approximately 20 h allowing for once daily dosing [97]. The selectivity of these 2 metabolites also has the advantage of limiting off-target receptor binding, which may occur with other TBZ isomers [95]. Two multicenter, 6-week, randomized, double-blind, placebo-controlled trials have been reported. The first, KINECT 2, included 100 TS patients [97]. Of these, 58% had schizophrenia or schizoaffective disorder and 38% had a mood disorder. Placebo or valbenazine was given once per day starting at 25 mg and escalated by 25 mg/week to 75 mg/day based on TS response and tolerability. The primary efficacy endpoint was change in AIMS severity from baseline to week 6. The mean baseline AIMS severity score was 8.0 ± 4.0. The change in AIMS score was based on the consensus score of each video by 2 raters (movement disorder specialists) blinded to treatment group and visit. A secondary efficacy endpoint was change in clinical global impression (CGI). After titration, 76% of the subjects on active drug and 80% in the placebo group reached the 75-mg/day dose. At the 6-week endpoint, there was a mean 3.6-point decrease in AIMS severity score for valbenazine compared with 1.1 for placebo (p = 0.0005). Sixty-seven percent of valbenazine patients reached treatment success as defined by a rating on CGI of “much improved” or “very much improved” as compared with 16% of placebo subjects (p = 0.0001). Five patients (9.8%) in each treatment arm discontinued the trial after randomization. None of these discontinuations were the result of treatment-emergent adverse events (TEAEs). The overall incidence of TEAEs was 49% in the valbenazine arm and 32.7% in the placebo arm, and no deaths or serious TEAEs were reported. The most common adverse events reported by subjects on valbenazine versus placebo were fatigue (9.8% vs 4.1%) and headache (9.8% vs 4.1%).
Subsequently, KINECT 3 was completed [98]. This study used a similar design derived from the KINECT 2 trial. However, in this one, a larger N, 234 subjects (66% schizophrenia and 33% mood disorder), were randomized in a 1:1:1 manner to placebo, valbenazine 40 mg once daily, or valbenazine 80 mg once daily. Seven subjects withdrew from the trial because of adverse events: 2 in the placebo arm, 2 in the valbenazine 40-mg arm, and 3 in the valbenazine 80-mg arm. Mean AIMS score at baseline was 10.4 ± 3.6. The difference in the least squares mean change from baseline to week 6 was 3.1 points between valbenazine 80 mg (− 3.2) and placebo (− 0.1) (p < 0.001). The effect size (Cohen’s d) was large, at 0.90. The most common adverse events in the combined valbenazine groups and placebo were somnolence (5.3% and 3.9%, respectively), akathisia (3.3% and 1.3%, respectively), and dry mouth (3.3% and 1.3%, respectively). Suicidal ideation was less common in the valbenazine versus placebo groups (2.6% vs 5.3%). Parkinsonism and depression were present in less than 2% of subjects. A case series has since supported the risk of developing valbenazine-induced parkinsonism [99].
The long-term benefits of valbenazine have been demonstrated in the KINECT 3 extension study [100]. This study had a 42-week valbenazine extension period and subsequent 4-week washout period (final visit at week 52). Participants who were receiving 80 mg/day or 40 mg/day in the double-blind phase maintained these doses and those receiving placebo were randomized to 40 mg/day or 80 mg/day at a 1:1 ratio. Treatment remained blinded. Sixty-one percent of patients who enrolled in the extension (198 subjects) completed the full duration. Adverse events led to withdrawal in 15.7% and these included somnolence and suicidal ideation with 3 subjects each. The suicidal ideation and attempts occurred in 10 subjects, a rate lower than the approximate 30% lifetime history of suicidality in this patient population. Syncope, which occurred in 3 subjects, was the only serious AE thought to be possibly related to drug therapy. Valbenazine did not result in a worsening of akathisia, parkinsonism, or worsening in psychiatric disorders. AIMS score improvements in the extension study were maintained throughout the study and were significant compared to baseline. The scores worsened during the end of the study washout toward baseline level. CGI-TS and P-CGI demonstrated clinically significant global improvement throughout the extension and also worsened during the washout period. The washout effect indicated that the effect of valbenazine is reversible and symptomatic. These results supported the efficacy and tolerability of valbenazine for the treatment of TS for at least a year [98, 100]. In a second, long-term study, KINECT 4, 167 subjects (73% psychotic disorder, 27% mood disorder) were enrolled in a 48-week, open-label treatment period followed by a 4-week washout and 103 (62%) completed the full protocol [101]. Subjects were started on 40 mg and then changed to 80 mg after 4 weeks based on efficacy and tolerability. Serious TEAEs were seen in 13.7% with discontinuation occurring in 11.8%. Ninety percent of patients had > 50% improvement with those remaining on 40 mg improving by 10.2 points on the AIMS scale and those on 80 mg improving by 11. More than 90% of patients were much or very much improved on CGI and P-CGI. Among the side effects reported in > 3% of the subjects were headache, suicidal ideation, and somnolence. As older patients tend to have more difficulty tolerating TBZ, an analysis was completed using pooled data from all valbenazine studies to establish efficacy and tolerability in older patients. Patients were dichotomized at age 55. There were no significant differences between older and younger subgroups with regard to developing responsiveness based on AIMS or CGI-TD scales. Further, there were no safety signals or TEAEs of clinical concern in older participants who received long-term treatment [102]. There was also an interest in looking specifically at the impact on patients with mood disorders considering depression is a possible complication of VMAT2 inhibitors. A pooled analysis of 3 of the valbenazine studies (2 double-blind, 1 open extension) examined the impact on TS in patients with primary bipolar or depressive disorders. Valbenazine was well tolerated and demonstrated substantial improvement in AIMS and CGI-TD scales at week 6 compared to placebo in 114 patients which lasted 48 weeks (assessed in 77 patients) consistent with results of the trials described above [103]. There was no comparison with response in psychotic populations and comparison with other VMAT2 inhibitors. In all the studies, there was no notable worsening of psychiatric disorders based on standard scale measures [104]. Also, adverse events were similar in the psychotic and mood disorder groups. These studies provided level A evidence for efficacy of valbenazine in TS.
Deutetrabenazine
Deutetrabenazine contains deuterium, a nontoxic isotope of hydrogen that has increased mass relative to hydrogen and forms a substantially stronger bond with carbon than hydrogen does. Although deuterated tetrabenazine (D-TBZ) retains the VMAT2 affinity of nondeuterated TBZ, the substitution of deuterium for hydrogen at specific positions prolongs its plasma half-life and reduces metabolic variability. The longer half-life enables twice daily (BID) dosing with lower peak concentration, which is believed to result in an improved risk–benefit profile [105].
D-TBZ was studied in 2 12-week, double-blind, randomized, placebo-controlled trials. One examined an escalating dose of D-TBZ versus placebo (ARM-TD) in 117 patients (70% psychotic patients and 30% mood disorders) with moderate to severe TS (minimum AIMS severity score of ≥ 6). The dose of D-TBZ was initiated at 12 mg/day and titrated weekly by 6 mg/day until adequate dyskinesia control was achieved, a significant adverse event occurred, or maximal allowable dose of 48 mg/day was achieved. This was followed by a 6-week maintenance period. The primary efficacy endpoint was change in AIMS score from baseline to week 12 as assessed via consensus review of 2 blinded video raters. Mean baseline AIMS severity score (items 1-7) was 9.6 ± 3.9. There were 6 dropouts in the D-TBZ arm and 7 in the placebo arm. AIMS score decreased by a mean 3.0 points in the D-TBZ group compared with 1.4 points for placebo (p = 0.019). CGI for change was “much improved” or “very much improved” in 48.2% of the D-TBZ compared with 40.4% in the placebo group. D-TBZ and placebo groups showed low rates of adverse events: anxiety (3.4% vs 6.8%), depressed mood/depression (1.7% vs 1.7%), and suicidal ideation (0% vs 1.7%, respectively). No worsening of parkinsonism or akathisia, as measured on the Unified Parkinson’s Disease Rating Scale motor subscale and Barnes Akathisia scale, was noted from baseline to week 12 in either group. This data supported the tolerability and efficacy of D-TBZ in patients with TS [106].
In a second trial (AIM-TD), 298 subjects (60% psychotic disorders, 36% mood disorders) were randomized 1:1:1:1 to receive placebo, D-TBZ 12 mg/day, 24 mg/day, or 36 mg/day. All patients in the active treatment arms were started on D-TBZ 12 mg/day, and the dose was increased through week 4 until the assigned dose was reached. The target dose was maintained for the next 8 weeks. The primary efficacy endpoint was the same as the ARM-TD study. From baseline to week 12, change in least squares mean AIMS severity score based on consensus scoring by 2 blinded reviewers improved by − 3.3 points in the D-TBZ 36-mg/day group, − 3.24 in the 24-mg/day group, and − 2.1 points in the 12-mg/day group, with a significant treatment difference of − 1.9 points (p = 0.001), − 1.8 points (p = 0.003), and − 0.7 points (p = 0.217), respectively, compared with placebo. CGI-C of “much improved” or “very much improved” was achieved in 26% of patients on placebo, 28% receiving 12 mg/day, 49% receiving 24 mg/day, and 44% on 36 mg/day. The rate of adverse events was similar for D-TBZ and placebo groups. Serious adverse events were reported in 6% of the placebo group, 3% of the 12-mg/day group, 8% of the 24-mg/day group, and 5% of those in the 36 mg/day. Three (1%) patients had suicidal ideation. The most common adverse effect was headache (5%). The side effects limiting tolerability of TBZ were rare with D-TBZ and included somnolence (2%), parkinsonism (< 1%), akathisia (< 1%), depression (2%), and suicidality (1%). These results supported the efficacy and tolerability of D-TBZ at a dose of 24 mg/day or 36 mg/day for the treatment of TS [107]. Based on these studies, D-TBZ showed level A evidence of efficacy for TS.
Subjects completing the double-blind trials entered an open-label, single-arm study that consisted of a 6-week dose-escalation phase and a long-term maintenance phase. Patients titrated up to a maximum of 48 mg/day, or 36 mg/day for those prescribed strong cytochrome P450 2D6 (CYP2D6) inhibitors. Subjects were followed out to week 80. A total of 343 patients enrolled and there were 331 patient-years of exposure in this analysis. The exposure-adjusted incidence rates of AEs with long-term treatment were similar to the randomized clinical trials. Most common nervous system–related AEs included headache, somnolence, depression, and anxiety. The mean (S.E.) change in AIMS score was − 4.9 (0.4) at week 54 (n = 146) and − 6.3 (0.7) at week 80 (n = 66) [108]. This study demonstrated long-term efficacy and tolerability with D-TBZ for TS.
All 3 VMAT2 inhibitors are metabolized by CYP2D6. They also have the potential to cause Qtc prolongation. This is especially true in poor metabolizers.
Second-Tier Drugs: Clonazepam, Ginkgo biloba, and Amantadine (Table 4)
There are 3 other agents with evidence of efficacy for treating TS, although less than level A. These are clonazepam, Ginkgo biloba (EGb-761), and amantadine, all with different mechanisms of action. Should VMAT2 inhibitors not result in improvement or if intolerability occurs, these agents are a reasonable next step. The use of clonazepam, an indirect GABAA agonist, has level B evidence. In a randomized, double-blind, placebo-controlled crossover trial published in 1990, 19 psychiatric outpatients with TS completed a 1-week placebo run-in followed by 4 weeks of randomized therapy, a 2-week washout, a 4-week crossover therapy phase followed by a 1-week placebo washout [109]. Results demonstrated a 37% reduction of the Maryland Psychiatric Research Center Movement Disorder Scale dyskinesia score with 2 to 3.5 mg/day and a reversal of this effect with placebo. Mild to moderate sedation occurred in 6 subjects and ataxia in 3. In 5 subjects followed long term, the effectiveness waned after 5 to 8 months suggesting tolerance.
Extract of Ginkgo biloba (EGb-761), a potent antioxidant, also demonstrated efficacy for TS with level B evidence. The antioxidant vitamin E was the first hypothesized, based on this mechanism, to be a potential treatment for TS, but a large, multicenter double-blind trial was ultimately negative [110]. The largest EGb trial, from China, included 157 inpatients with schizophrenia [111]. This was a single-site, double-blind, placebo-controlled, parallel group trial of 240 mg/day of EGb-761. All subjects were male and under age 60. The study included a 1-week single blind, placebo run-in in which any subjects experiencing a 25% improvement with placebo were removed from randomization. The rest were treated for 12 weeks with either placebo or EGb-761 (1:1 ratio). The primary outcome measures were change in AIMS total score and the proportion of patients with > 30% improvement (responders). Ninety-seven percent of subjects completed the trial. AIMS scores decreased significantly in subjects receiving EGb-761 treatment relative to the placebo group (2.13 ± 1.75 vs − 0.10 ± 1.69; p < 0.0001). In the active group, 51% were responders versus only 5% in the placebo group (p < 0.001). No worsening of psychopathology or cognition was seen. There were no significant adverse effects. A meta-analysis of 3 randomized controlled trials of EGb augmentation of antipsychotics versus antipsychotics plus placebo or antipsychotic monotherapy was completed. The primary outcome measure was the severity of TS symptoms assessed by the AIMS. The 3 studies included 299 patients from China with a mean age of 55.9 ± 13.4 years. EGb (240 mg/day) outperformed the control group in reducing the severity of TS as measured by the AIMS (2.30 (95% CI − 3.04, − 1.55), p < 0.00001) [112].
There is level C evidence for effectiveness of amantadine, postulated to relate to NMDA receptor blocking properties of this drug [113]. Three small, blinded trials have been reported [74]. One, from 1971, was very small, n = 6, but demonstrated clinical improvement after 3 weeks [114]. Of the other 2 trials, 1, reported in 1997, demonstrated improvement in 16 hospitalized psychiatric patients [115]. A 2-week baseline period was followed by a 7-week placebo-controlled randomized trial and, in turn, followed by a 1-week washout and a 7-week crossover phase. The primary outcome variable was the median AIMS score during the 3-week period when subjects received 300 mg/day or placebo. The study demonstrated a 15% reduction in the overall AIMS score (p = 0.05) and 10 of the 16 patients improved by ≥ 20%. A second trial, reported in 2010 [116], involved 22 outpatients with schizophrenia and TS who received amantadine (400 mg/day) or placebo in a 2-week double-blind, randomized trial followed by a 4-day washout and a 2-week crossover phase. The primary outcome was the change in AIMS score at the end of each treatment phase. Results demonstrated a statistically significant reduction in AIMS severity scores by 22% with 10 subjects improving by > 20%. Little or no placebo effect was seen in these 2 trials. There was no worsening of psychotic symptoms.
Third-Tier Drugs: Levetiracetam, Piracetam, Vitamin B6, Melatonin, Baclofen, Propranolol, Zolpidem, and Zonisamide (Table 5)
Several currently available agents are either listed as having insufficient evidence or are not addressed at all in the guidelines that might have potential for the treatment of TS. When considering these agents, the treating physician needs to weigh the risks and potential benefits closely considering the lack of adequate evidence.
Levetiracetam is an anti-epileptic that has been examined in trials as a possible treatment of TS [117]. The mechanism of action is unclear but may relate to N-type calcium channel blockade [118] or to its binding to synaptic vesicle protein 2A which may play a role in the stability of synaptic vesicles containing neurotransmitters. The drug has been shown to successfully improve TS in several case reports and open studies [118,119,120,121]. One double-blind, placebo-controlled, randomized, 12-week, parallel group study has been reported [117] in 50 subjects who were enrolled, 25 randomized to each group. At 12 weeks, the active group (mean dose 1900 mg/day) improved 44% in the AIMS score, while the placebo group improved 19% (p = 0.02). Three adverse effects occurred in the active group and were seen in 2 subjects each, including ataxia, irritability, and decreased appetite [117]. This trial is considered insufficient evidence, in part, because only 72% of the subjects completed.
Piracetam, a chemically similar drug to levetiracetam used predominantly for myoclonus in Europe and Asia, was initially shown to improve TS symptoms nearly 40 years ago [122]. More recently, 40 subjects with schizophrenia or schizoaffective disorder and TS in a randomized, double-blind, placebo-controlled crossover study [123] were treated while remaining on their antipsychotic regimen. They were first randomized for 4 weeks of placebo or piracetam (4800 mg/day), followed by a 1-week washout and then a 4-week crossover phase. The primary outcome measure was change in the Extrapyramidal Symptom Rating Scale (ESRS) score. There was a mean decrease in the TS subscale of 3 points in the piracetam group versus a deterioration in the placebo group by − 0.2 points (p = 0.003) [123].
Vitamin B6, an antioxidant, has been used for treating TS in case series [124] and a single-blinded trial [125]. The randomized, double-blind, placebo-controlled trial [125] was a 26-week study of 50 inpatients with schizophrenia or schizoaffective disorder and TS. They were randomly assigned to 1200 mg of vitamin B6 or placebo in the first 12 weeks of treatment followed by a 2-week washout, then completed a 12-week crossover phase. The primary outcome was change in ESRS. The mean change in ESRS clinical global impression from baseline to endpoint was 2.4 points in patients treated with vitamin B6 and 0.2 points in the placebo group (p < 0.0001). The mean decrease in the parkinsonism subscale score was 18.5 points and 1.4 points, respectively (p < 0.00001), and the mean decrease in the dyskinesia subscale score was 5.2 points and − 0.8 points, respectively (p < 0.0001).
Melatonin is another antioxidant that reverses the oxidative effects of DRBAs [126]. Melatonin is thought to be a more powerful antioxidant than other agents used and also alters dopamine release in the brain [127] and, hence, has also been examined in TS. The studies, however, have been limited and the findings related to its effectiveness in treating TS are conflicting. There is 1 small double-blind, placebo-controlled crossover study published in 2001 that demonstrated response [128]. Twenty-two patients were treated with 10 mg of melatonin and placebo in a crossover study for a 6-week period with an intervening 4-week washout. Melatonin resulted in a 2.45 ± 1.92-point decrease in the AIMS score versus 0.77 ± 1.11-point drop by placebo (p < 0.001). An improvement of ≥ 30% was seen in 40% of the melatonin-treated patients and 0% in the placebo arm. There were no adverse events. A second smaller 12-week, randomized, double-blind, placebo-controlled trial comparing melatonin 20 mg/day (7 patients) to placebo (6 patients) was negative [129]. A recent meta-analysis of 4 randomized controlled trials (N = 130) including a large trial from China did not demonstrate a significant difference between melatonin and placebo [130].
Baclofen is another GABA agonist tested for TS in the late 1970s and early 1980s. In 1 double-blind, placebo-controlled, crossover trial completed in 1976, 20 patients were treated for 2 weeks, washed out for 1 week, and crossed over for another 2-week period with up to 60 mg/day. The evaluation was based on a 1 to 5 scale for TS severity. After 14 days of treatment, 15 patients showed improvement of baclofen (TS completely disappeared in 5 patients, and in the remaining responders, the condition improved from scores 3-4 to score 1), whereas none showed improvement on placebo (p < 0.0005). Adverse effects included sedation, muscular hypotonia, dizziness, vomiting, and muscular rigidity [131]. A study reported in 1978 was a double-blind, crossover study in 18 TD patients. Each treatment phase lasted 3 weeks. The primary outcome was via an assessment of video recordings. Baclofen (20-120 mg daily) reduced dyskinesia by a median score from 5 to 3 (p < 0.05). The effect on the oral movement pattern of tardive dyskinesia was characterized by a reduced frequency. Side effects included sedation, muscular weakness, and confusion which were observed in 50% of the patients [132]. In a third study completed in 1982, 33 patients who were maintained on a constant dose of their antipsychotic completed a randomized 6-week, double-blind, placebo-controlled trial which was followed by a 6-week open-label trial. Baclofen dose was 30 to 90 mg/day and TS severity was assessed by the AIMS scale (responder status was defined by a reduction of 25%). During the double-blind portion, there was a reduction in total AIMS score (p < 0.05); 67% of baclofen-treated patients and 47% of placebo-treated patients were responders. The open-labeled portion included 7 of 9 baclofen responders and 9 of 9 placebo nonresponders. The baclofen response rate for the original placebo nonresponders was 77%, but a loss of efficacy was seen in 23% of the original baclofen responders, and there was an attenuation of response in others. Side effects included nausea, somnolence, and ataxia [133]. Another double-blind, randomized, placebo-controlled study involving 31 patients had negative results [134]. There was also an interesting single case of axial tardive dystonia that improved with intrathecal baclofen [135].
Propranolol was examined as a treatment of TS in the 1980s. The reports involved a total of 26 subjects examined in open-label single cases or case series of which 65% improved rapidly and often dramatically (including complete reversal) to low doses of the drug, up to 80 mg/day [136,137,138,139]. There was also a double-blind, crossover design study evaluating only 4 patients utilizing 10 times the dose of the open trials (up to 800 mg/day) in which 2 improved [140]. The patients were examined weekly up to 20 weeks with the AIMS scale and videotaped. Patients were treated with alternating periods of active drug or placebo. The study showed variable response in the blinded portion of the study but significant long-term improvement in an open-label follow-up [140]. Interest in propranolol waned when it was found that it increased neuroleptic plasma levels possibly leading to suppression of symptoms [141]. However, it is noteworthy that many of the responsive patients were, in fact, not treated with neuroleptics at the time. This author “revisited” the impact of propranolol in TS patients. Two cases show dramatic results [142]. This led to frequent use of propranolol in our clinic. In a later retrospective record review of 47 patients, mean age 63 years, we further examined the impact of propranolol on TS. DRBAs were discontinued in all patients and the mean duration of TS at the time propranolol was initiated was 17 months. Propranolol resulted in improvement in 64% of the patients and 77% of those had a moderate to complete or near-complete response. Mean daily dose was 69 mg and duration of therapy was 14 months. Three patients stopped propranolol because of adverse effects: hypotension (2) and nightmares (1). Severity of TS and duration of propranolol therapy were associated with response [143].
There has been some experience with zolpidem, a nonbenzodiazepine hypnotic medication that binds to the GABA–benzodiazepine receptor complex in the basal ganglia, is structurally related to melatonin, and has been reported to possess antioxidant effects [144, 145]. In rodent model, zolpidem reduced haloperidol and chlorpromazine-induced hyperkinetic orofacial chewing movements [145]. The mechanism of this effect was thought to be through reduced lipid peroxidation and possible via reversal of secondary monoamine changes. The first experience in 3 TS patients, including akathisia, treated with 5 to 10 mg twice per day demonstrated a notable improvement [144].
Finally, a 4-week open-label study with zonisamide 50 to 100 mg/day in 11 patients with schizophrenia and mental retardation demonstrated significant improvement in AIMS score with nearly 40% of patients having at least 20% improvement [146].
Botulinum Toxins
For classical tardive dyskinesia, there is little evidence to support the use of botulinum toxin. There is 1 small single blind study which showed benefit [147]. In this study, patients were videoed at baseline, then prior to and 4 weeks after 3 injection sessions. The videos were rated in random order by 2 raters using the AIMS severity scale items 2 to 4. Patients were injected with onabotulinumtoxinA in the orbicularis oris muscle at 4 sites (0.5 cm bilaterally above the upper and below the lower lips). The maximum dose was 80 U. Twelve patients were included but 4 had a change of their antipsychotic agents during the study. When those 4 were included in the analysis, a nonsignificant decrease from baseline to the last visit (mean difference on the AIMS items 2-4) was seen. But in a separate analysis of the 8 patients with stable antipsychotic treatment, there was a small but significant improvement (mean difference on the AIMS items 2-4 was 1.8, S.D. = 2.4; p = 0.035). Fifty percent of these patients wanted to continue the study.
In the case of tardive dystonia, particularly craniocervical distribution, botulinum toxin has been widely utilized based on the response of patients with idiopathic dystonia. Several open-label retrospective reports support its use [148,149,150,151,152] for oromandibular, lingual, and cervical tardive dystonia. For the most part, the response of tardive dystonia is similar to that of idiopathic dystonia.
Surgical Therapy
Deep brain stimulation of the globus pallidus interna (GPi-DBS) has been reported to treat TS, particularly tardive dystonia and classical tardive dyskinesia, that is severe and refractory to medical therapy. The GPi target was initially selected because of the responsiveness of idiopathic dystonia and levodopa-induced dyskinesia to stimulation in that region. Multiple case reports showing substantial improvement in TS [153,154,155] were followed by 1 small, prospective, phase 2, multicenter study with double-blind evaluations that showed a mean decrease in 50% in tardive dystonia symptoms according to validated rating scales [156]. More recently, larger prospective trials with a blinded assessment have been published. One was an examination of 19 patients receiving GPi-DBS for combined tardive dystonia/dyskinesia. There was a double-blind evaluation at 6 months after surgery which provided class II evidence for the effectiveness of the procedure [157]. Greater than 50% improvement in AIMS and ESRS scores was found and sustained as long as 11 years after surgery. Adverse events within 1 year of surgery included falls in 5 individuals, psychiatric morbidity in 8, and complications of equipment in 6. In another randomized, delayed start, double-blind, sham stimulation–controlled trial of GPi-DBS [158], tardive dystonia/dyskinesia severity was assessed in a blinded manner at 3 months and then an open assessment was performed at 6 months in 25 patients. Primary endpoint was the percent change in the Burke–Fahn–Marsden Dystonia Rating Scale (BFMDRS) between active versus sham stimulation using blinded video assessment. A prespecified sample size was not met indicating that the study may have been underpowered. The group difference in BFMDRS at month 3 was not significant (23% vs 12% change), but there was a significant difference in AIMS scores. At 6 months of stimulation, both groups improved by 42% along with significant improvement in quality of life. Adverse events related mainly to surgical implantation of the DBS device; all reversed. The lack of significant response of the BFMDRS scale at 3 months may relate to the tendency of dystonia to improve to peak level over many months [159].
The relative efficacy of GPi-DBS for improving tardive dystonia of different body parts and the temporal course of improvement were assessed in 8 patients in another study [160]. Although improvements were marked in all body parts, the time course of response varied from weeks to months and tended to be slower in the neck and trunk.
There is less experience with DBS of the subthalamic nucleus for treating TS. A retrospective examination of 10 patients found improvements of greater than 50% in the BFMDRS and the AIMS at 1 week after surgery [161]. With continued follow-up, mean improvements increased to over 80% and were sustained for the mean of 65 months. One patient demonstrated improvement for 12 years.
The data suggests good efficacy of GPi-DBS for TS with a reasonable safety profile. Such treatments should be used for those that are severely impaired by the TS and unresponsive to medical therapy and performed in centers with ample experience. Nevertheless, further controlled trials are needed to raise the currently low level of evidence (level C) [74].
Conclusion
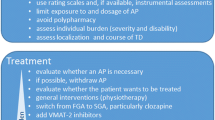
TS is becoming an increasing health concern with the increased off-label use of antipsychotics. Data suggests that prevalence level of up to 1.2 million patients may be impacted at this time [69]. Importantly, in the last several years, there have been significant advances in TS therapy, particularly with the FDA approval of 2 VMAT2 inhibitors specifically for TS and with new data on the efficacy of GPi DBS [74]. These additions to the information gathered over 5 decades put into focus how the many options can be utilized. Based on the data reviewed in this paper and the classification of drugs into tiers based on evidence, an algorithm has been developed that may provide guidance to the treatment of TS in clinical practice (Fig. 1). This algorithm has some modifications from recently published options [11, 69, 162].
Suggested algorithm for treating TS based on evidence and experience. For tier 1, valbenazine or deutetrabenazine would be considered first line in the USA, but it would be tetrabenazine if these newer agents are not available in other countries. The use of 2nd and 3rd tier drugs could be tried in combination with tier 1 or alone. “If further treatment is still needed” refers to either no response if intolerability occurs
Step 1, after the diagnosis of clinically significant TS is made and after assessment indicates a need for therapy, would be to consider discontinuing DRBAs. For patients treated with anti-emetics or treated with antipsychotics for diagnoses other than psychosis, this may be possible. For patients with psychiatric disorders such as schizophrenia or schizoaffective disorder, this may not be possible. In such cases, consider changing to a less potent antipsychotic. Perhaps the best option, if possible, is switching to clozapine monotherapy. After follow-up of weeks to months, if symptoms remain troublesome, then the clinician should initiate anti-dyskinetic drugs. The first-line treatment should be VMAT2 inhibitors, which are first tier. For those in the USA, the newer agents would be considered first line, but in those countries where these are not available, then TBZ would be first line. Not all patients will respond or tolerate these agents. If that is the case, then patients can be prescribed 1 or more second-tier agents (clonazepam, Ginkgo biloba, or amantadine), based on risk–benefit review. Not all patients will respond or tolerate these agents. If that is the case, then 1 can consider prescribing 1 or more of the many third-tier drugs, again based on a risk–benefit review. The role of botulinum toxin depends on the phenotype. For tardive dystonia such as craniocervical dystonia, it may be first-line treatment. If the problem is classical tardive dyskinesia of the orobuccolingual distribution, then it can be used as part of the third tier. Once all medical and toxin therapies have been exhausted then, based on patient medical status, surgical therapy can be considered. GPi DBS has the most evidence and should be the primary target. There is a need for further data for using subthalamic nucleus. It is possible that this algorithm will be beneficial to a large portion of TS patients.
It should be made clear that these approaches to treating TS are symptomatic. They do not reverse the pathogenic process that causes TS. When these treatments are withdrawn, including VMAT2 inhibitors or DBS, the symptoms return. In addition, the data from clinical trials rarely indicate the impact of the therapy on individual phenotypes of TS, for example tardive dystonia or akathisia. There is still a great need to develop new improved treatments. This should include prevention with the diminished use of off-label use of antipsychotics. Further, there is a need to develop new antipsychotics that are safer and cause lower rates or no drug-induced movement disorders. This could include further controlled trials with clozapine monotherapy. Further, studies on individual phenotypes would be helpful in directing therapy. There is also a need to gain a better understanding of the pathophysiology in order to develop drugs that can reverse the process. It appears nonhuman primate models are the better route to delineating the mechanisms for TS. The work completed in the last several years represents a significant advancement for the treatment of TS but represents only an initial step toward improving care for this population of patients.
References
Caroff SN, Leong SH, Roberts C, Berkowitz RM, Campbell EC. Cumulative burden of illness in veterans with tardive dyskinesia and serious mental disorders. J Clin Psychopharmacol. 2020;40(1):38-45.
Citrome L, Saklad SR. Revisiting tardive dyskinesia: focusing on the basics of identification and treatment. J Clin Psychiatry. 2020;81(2):TV18059AH3C.
Schonecker M. Paroxysmal dyskinesia as the effect of megaphen. Der Nervenarzt. 1957;28(12):550-3.
Sigwald J, Bouttier D, Raymondeaud C, Piot C. 4 Cases of facio-bucco-linguo-masticatory dyskinesis of prolonged development following treatment with neuroleptics. Rev Neurol (Paris). 1959;100:751-5.
Caroff SN, Ungvari GS, Cunningham Owens DG. Historical perspectives on tardive dyskinesia. Journal of the Neurological Sciences. 2018;389:4-9.
Faurbye A, Rasch PJ, Petersen PB, Brandborg G, Pakkenberg H. Neurological symptoms in pharmacotherapy of psychoses. Acta Psychiatrica Scandinavica. 1964;40(1):10-27.
Hauser RA, Truong D. Tardive dyskinesia: out of the shadows. Journal of the Neurological Sciences. 2018;389:1-3.
Frei K, Truong DD, Fahn S, Jankovic J, Hauser RA. The nosology of tardive syndromes. Journal of the Neurological Sciences. 2018;389:10-6.
Association AP. Diagnostic and statistical manual of mental disorders, revised (DSM-5). Fifth ed 2019.
Schooler NR, Kane JM. Research diagnoses for tardive dyskinesia. Arch Gen Psychiatry. 1982;39(4):486-7.
Revuelta GJ, Cloud LJ, Aia PG, Factor SA. Tardive dyskinesia. In: Albanese A JJ, editor. Hyperkinetic movement disorders: diagnosis, etiology, and treatment. Oxford, England: Wiley Blackwell; 2012. p. 331-352.
Seeman P. Dopamine D2 receptors as treatment targets in schizophrenia. Clin Schizophr Relat Psychoses. 2010;4(1):56-73.
Ali Z, Roque A, El-Mallakh RS. A unifying theory for the pathoetiologic mechanism of tardive dyskinesia. Med Hypotheses. 2020;140:109682.
Blanchet PJ, Levesque D. Time for a new slate in tardive dyskinesia research. Mov Disord. 2020.
Blanchet PJ, Parent MT, Rompre PH, Levesque D. Relevance of animal models to human tardive dyskinesia. Behavioral and Brain Functions: BBF. 2012;8:12.
Andreassen OA, Ferrante RJ, Aamo TO, Beal MF, Jorgensen HA. Oral dyskinesias and histopathological alterations in substantia nigra after long-term haloperidol treatment of old rats. Neuroscience. 2003;122(3):717-25.
Jiang LH, Kasser RJ, Altar CA, Wang RY. One year of continuous treatment with haloperidol or clozapine fails to induce a hypersensitive response of caudate putamen neurons to dopamine D1 and D2 receptor agonists. J Pharmacol Exp Ther. 1990;253(3):1198-205.
Silvestri S, Seeman MV, Negrete JC, Houle S, Shammi CM, Remington GJ, et al. Increased dopamine D2 receptor binding after long-term treatment with antipsychotics in humans: a clinical PET study. Psychopharmacology (Berl). 2000;152(2):174-80.
Ashby CR, Jr., Hitzemann R, Rubinstein JE, Wang RY. One year treatment with haloperidol or clozapine fails to alter neostriatal D1- and D2-dopamine receptor sensitivity in the rat. Brain Res. 1989;493(1):194-7.
Casey DE. Tardive dyskinesia: pathophysiology and animal models. J Clin Psychiatry. 2000;61 Suppl 4:5-9.
Blin J, Baron JC, Cambon H, Bonnet AM, Dubois B, Loc'h C, et al. Striatal dopamine D2 receptors in tardive dyskinesia: PET study. J Neurol Neurosurg Psychiatry. 1989;52(11):1248-52.
Kornhuber J, Riederer P, Reynolds GP, Beckmann H, Jellinger K, Gabriel E. 3H-spiperone binding sites in post-mortem brains from schizophrenic patients: relationship to neuroleptic drug treatment, abnormal movements, and positive symptoms. J Neural Transm. 1989;75(1):1-10.
Mahmoudi S, Levesque D, Blanchet PJ. Upregulation of dopamine D3, not D2, receptors correlates with tardive dyskinesia in a primate model. Mov Disord. 2014;29(9):1125-33.
Seeman P. Atypical antipsychotics: mechanism of action. Can J Psychiatry. 2002;47(1):27-38.
Stahl SM. “Hit-and-run” actions at dopamine receptors, part 2: illustrating fast dissociation from dopamine receptors that typifies atypical antipsychotics. J Clin Psychiatry. 2001;62(10):747-8.
Stahl SM. “Hit-and-run” actions at dopamine receptors, part 1: mechanism of action of atypical antipsychotics. J Clin Psychiatry. 2001;62(9):670-1.
Levesque C, Hernandez G, Mahmoudi S, Calon F, Gasparini F, Gomez-Mancilla B, et al. Deficient striatal adaptation in aminergic and glutamatergic neurotransmission is associated with tardive dyskinesia in non-human primates exposed to antipsychotic drugs. Neuroscience. 2017;361:43-57.
Cloud LJ, Zutshi D, Factor SA. Tardive dyskinesia: therapeutic options for an increasingly common disorder. Neurotherapeutics. 2014;11(1):166-76.
Thaker GK, Tamminga CA, Alphs LD, Lafferman J, Ferraro TN, Hare TA. Brain gamma-aminobutyric acid abnormality in tardive dyskinesia. Reduction in cerebrospinal fluid GABA levels and therapeutic response to GABA agonist treatment. Arch Gen Psychiatry. 1987;44(6):522-9.
Auchus AP, Pickel VM. Quantitative light microscopic demonstration of increased pallidal and striatal met5-enkephalin-like immunoreactivity in rats following chronic treatment with haloperidol but not with clozapine: implications for the pathogenesis of neuroleptic-induced movement disorders. Exp Neurol. 1992;117(1):17-27.
Bishnoi M, Chopra K, Kulkarni SK. Neurochemical changes associated with chronic administration of typical antipsychotics and its relationship with tardive dyskinesia. Methods Find Exp Clin Pharmacol. 2007;29(3):211-6.
Andreassen OA, Meshul CK, Moore C, Jorgensen HA. Oral dyskinesias and morphological changes in rat striatum during long-term haloperidol administration. Psychopharmacology (Berl). 2001;157(1):11-9.
Maurer I, Moller HJ. Inhibition of complex I by neuroleptics in normal human brain cortex parallels the extrapyramidal toxicity of neuroleptics. Molecular and Cellular Biochemistry. 1997;174(1-2):255-9.
Seeman P, Tinazzi M. Loss of dopamine neuron terminals in antipsychotic-treated schizophrenia; relation to tardive dyskinesia. Prog Neuropsychopharmacol Biol Psychiatry. 2013;44:178-83.
Sarro S, Pomarol-Clotet E, Canales-Rodriguez EJ, Salvador R, Gomar JJ, Ortiz-Gil J, et al. Structural brain changes associated with tardive dyskinesia in schizophrenia. Br J Psychiatry. 2013;203(1):51-7.
Zai CC, Maes MS, Tiwari AK, Zai GC, Remington G, Kennedy JL. Genetics of tardive dyskinesia: promising leads and ways forward. Journal of the Neurological Sciences. 2018;389:28-34.
Frei K. Tardive dyskinesia: who gets it and why. Parkinsonism & Related Disorders. 2019;59:151-4.
Alkelai A, Greenbaum L, Heinzen EL, Baugh EH, Teitelbaum A, Zhu X, et al. New insights into tardive dyskinesia genetics: implementation of whole-exome sequencing approach. Prog Neuropsychopharmacol Biol Psychiatry. 2019;94:109659.
Kang UJ, Burke RE, Fahn S. Natural history and treatment of tardive dystonia. Mov Disord. 1986;1(3):193-208.
Little JT, Jankovic J. Tardive myoclonus. Mov Disord. 1987;2(4):307-11.
Stacy M, Jankovic J. Tardive tremor. Mov Disord. 1992;7(1):53-7.
Kuo SH, Jankovic J. Tardive gait. Clinical Neurology and Neurosurgery. 2008;110(2):198-201.
FitzGerald PM, Jankovic J. Tardive oculogyric crises. Neurology. 1989;39(11):1434-7.
Fountoulakis KN, Samara M, Siapera M, Iacovides A. Tardive Tourette-like syndrome: a systematic review. Int Clin Psychopharmacol. 2011;26(5):237-42.
Burke RE, Kang UJ, Jankovic J, Miller LG, Fahn S. Tardive akathisia: an analysis of clinical features and response to open therapeutic trials. Mov Disord. 1989;4(2):157-75.
Ford B, Greene P, Fahn S. Oral and genital tardive pain syndromes. Neurology. 1994;44(11):2115-9.
Savitt D, Jankovic J. Tardive syndromes. Journal of the Neurological Sciences. 2018;389:35-42.
Burke RE, Fahn S, Jankovic J, Marsden CD, Lang AE, Gollomp S, et al. Tardive dystonia: late-onset and persistent dystonia caused by antipsychotic drugs. Neurology. 1982;32(12):1335-46.
Samie MR, Dannenhoffer MA, Rozek S. Life-threatening tardive dyskinesia caused by metoclopramide. Mov Disord. 1987;2(2):125-9.
Horiguchi J, Shingu T, Hayashi T, Kagaya A, Yamawaki S, Horikawa Y, et al. Antipsychotic-induced life-threatening ‘esophageal dyskinesia’. Int Clin Psychopharmacol. 1999;14(2):123-7.
Jeste DV, Potkin SG, Sinha S, Feder S, Wyatt RJ. Tardive dyskinesia--reversible and persistent. Arch Gen Psychiatry. 1979;36(5):585-90.
Glazer WM, Morgenstern H, Schooler N, Berkman CS, Moore DC. Predictors of improvement in tardive dyskinesia following discontinuation of neuroleptic medication. Br J Psychiatry. 1990;157:585-92.
Zutshi D, Cloud LJ, Factor SA. Tardive syndromes are rarely reversible after discontinuing dopamine receptor blocking agents: experience from a university-based movement disorder clinic. Tremor and Other Hyperkinetic Movements. 2014;4:266.
D'Abreu A, Akbar U, Friedman JH. Tardive dyskinesia: epidemiology. Journal of the Neurological Sciences. 2018;389:17-20.
Aquino CC, Lang AE. Tardive dyskinesia syndromes: current concepts. Parkinsonism & Related Disorders. 2014;20 Suppl 1:S113-7.
Solmi M, Pigato G, Kane JM, Correll CU. Clinical risk factors for the development of tardive dyskinesia. Journal of the Neurological Sciences. 2018;389:21-7.
Martino D, Morgante F. Movement disorders and chronic psychosis: five new things. Neurology Clinical Practice. 2017;7(2):163-9.
Kane JM, Woerner M, Lieberman J. Tardive dyskinesia: prevalence, incidence, and risk factors. J Clin Psychopharmacol. 1988;8(4 Suppl):52S-6S.
Glazer WM, Morgenstern H, Doucette JT. Predicting the long-term risk of tardive dyskinesia in outpatients maintained on neuroleptic medications. J Clin Psychiatry. 1993;54(4):133-9.
Jeste DV, Caligiuri MP, Paulsen JS, Heaton RK, Lacro JP, Harris MJ, et al. Risk of tardive dyskinesia in older patients. A prospective longitudinal study of 266 outpatients. Arch Gen Psychiatry. 1995;52(9):756-65.
Correll CU, Leucht S, Kane JM. Lower risk for tardive dyskinesia associated with second-generation antipsychotics: a systematic review of 1-year studies. Am J Psychiatry. 2004;161(3):414-25.
Correll CU, Schenk EM. Tardive dyskinesia and new antipsychotics. Current Opinion in Psychiatry. 2008;21(2):151-6.
Woods SW, Morgenstern H, Saksa JR, Walsh BC, Sullivan MC, Money R, et al. Incidence of tardive dyskinesia with atypical versus conventional antipsychotic medications: a prospective cohort study. J Clin Psychiatry. 2010;71(4):463-74.
Miller DD, Caroff SN, Davis SM, Rosenheck RA, McEvoy JP, Saltz BL, et al. Extrapyramidal side-effects of antipsychotics in a randomised trial. Br J Psychiatry. 2008;193(4):279-88.
Mentzel TQ, Lieverse R, Bloemen O, Viechtbauer W, van Harten PN, Genetic R, et al. High incidence and prevalence of drug-related movement disorders in young patients with psychotic disorders. J Clin Psychopharmacol. 2017;37(2):231-8.
Ryu S, Yoo JH, Kim JH, Choi JS, Baek JH, Ha K, et al. Tardive dyskinesia and tardive dystonia with second-generation antipsychotics in non-elderly schizophrenic patients unexposed to first-generation antipsychotics: a cross-sectional and retrospective study. J Clin Psychopharmacol. 2015;35(1):13-21.
Carbon M, Hsieh CH, Kane JM, Correll CU. Tardive dyskinesia prevalence in the period of second-generation antipsychotic use: a meta-analysis. J Clin Psychiatry. 2017;78(3):e264-e78.
Carbon M, Kane JM, Leucht S, Correll CU. Tardive dyskinesia risk with first- and second-generation antipsychotics in comparative randomized controlled trials: a meta-analysis. World Psychiatry : official journal of the World Psychiatric Association. 2018;17(3):330-40.
Factor SA, Burkhard PR, Caroff S, Friedman JH, Marras C, Tinazzi M, et al. Recent developments in drug-induced movement disorders: a mixed picture. Lancet Neurology. 2019;18(9):880-90.
Leucht S, Cipriani A, Spineli L, Mavridis D, Orey D, Richter F, et al. Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis. Lancet. 2013;382(9896):951-62.
Chong SA, Tay JA, Subramaniam M, Pek E, Machin D. Mortality rates among patients with schizophrenia and tardive dyskinesia. J Clin Psychopharmacol. 2009;29(1):5-8.
Bhidayasiri R, Fahn S, Weiner WJ, Gronseth GS, Sullivan KL, Zesiewicz TA, et al. Evidence-based guideline: treatment of tardive syndromes: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2013;81(5):463-9.
Salem H, Pigott T, Zhang XY, Zeni CP, Teixeira AL. Antipsychotic-induced Tardive dyskinesia: from biological basis to clinical management. Expert Review of Neurotherapeutics. 2017;17(9):883-94.
Bhidayasiri R, Jitkritsadakul O, Friedman JH, Fahn S. Updating the recommendations for treatment of tardive syndromes: a systematic review of new evidence and practical treatment algorithm. Journal of the Neurological Sciences. 2018;389:67-75.
McEvoy JP. FDA-approved medications to treat tardive dyskinesia. J Clin Psychiatry. 2019;81(1):NU18041BR3C.
Citrome LL. Medication options and clinical strategies for treating tardive dyskinesia. J Clin Psychiatry. 2020;81(2).
Quitkin F, Rifkin A, Gochfeld L, Klein DF. Tardive dyskinesia: are first signs reversible? Am J Psychiatry. 1977;134(1):84-7.
Li CR, Chung YC, Park TW, Yang JC, Kim KW, Lee KH, et al. Clozapine-induced tardive dyskinesia in schizophrenic patients taking clozapine as a first-line antipsychotic drug. World J Biol Psychiatry. 2009;10(4 Pt 3):919-24.
Mendhekar DN, Duggal HS. Clozapine-induced tardive dyskinesia and hypothyroidism. J Neuropsychiatry Clin Neurosci. 2006;18(2):245-6.
Molho ES, Factor SA. Possible tardive dystonia resulting from clozapine therapy. Mov Disord. 1999;14(5):873-4.
Mentzel TQ, van der Snoek R, Lieverse R, Oorschot M, Viechtbauer W, Bloemen O, et al. Clozapine monotherapy as a treatment for antipsychotic-induced tardive dyskinesia: a meta-analysis. J Clin Psychiatry. 2018;79(6).
Pardis P, Remington G, Panda R, Lemez M, Agid O. Clozapine and tardive dyskinesia in patients with schizophrenia: a systematic review. Journal of Psychopharmacology. 2019;33(10):1187-98.
Lee D, Baek JH, Bae M, Choi Y, Hong KS. Long-term response to clozapine and its clinical correlates in the treatment of tardive movement syndromes: a naturalistic observational study in patients with psychotic disorders. J Clin Psychopharmacol. 2019;39(6):591-6.
Trugman JM, Leadbetter R, Zalis ME, Burgdorf RO, Wooten GF. Treatment of severe axial tardive dystonia with clozapine: case report and hypothesis. Mov Disord. 1994;9(4):441-6.
Lieberman JA, Saltz BL, Johns CA, Pollack S, Borenstein M, Kane J. The effects of clozapine on tardive dyskinesia. Br J Psychiatry. 1991;158:503-10.
Kane JM, Correll CU, Nierenberg AA, Caroff SN, Sajatovic M, Tardive Dyskinesia Assessment Working G. Revisiting the abnormal involuntary movement scale: proceedings from the Tardive Dyskinesia Assessment Workshop. J Clin Psychiatry. 2018;79(3).
Stacy M, Sajatovic M, Kane JM, Cutler AJ, Liang GS, O’Brien CF, et al. Abnormal involuntary movement scale in tardive dyskinesia: minimal clinically important difference. Mov Disord. 2019;34(8):1203-9.
Scorr LM, Factor SA. VMAT2 inhibitors for the treatment of tardive dyskinesia. Journal of the Neurological Sciences. 2018;389:43-7.
Stahl SM. Mechanism of action of vesicular monoamine transporter 2 (VMAT2) inhibitors in tardive dyskinesia: reducing dopamine leads to less “go” and more “stop” from the motor striatum for robust therapeutic effects. CNS Spectrums. 2018;23(1):1-6.
Kazamatsuri H, Chien C, Cole JO. Treatment of tardive dyskinesia. I. Clinical efficacy of a dopamine-depleting agent, tetrabenazine. Arch Gen Psychiatry. 1972;27(1):95-9.
Ondo WG, Hanna PA, Jankovic J. Tetrabenazine treatment for tardive dyskinesia: assessment by randomized videotape protocol. Am J Psychiatry. 1999;156(8):1279-81.
Kenney C, Hunter C, Jankovic J. Long-term tolerability of tetrabenazine in the treatment of hyperkinetic movement disorders. Mov Disord. 2007;22(2):193-7.
Gimenez-Roldan S, Mateo D. Huntington disease: tetrabenazine compared to haloperidol in the reduction of involuntary movements. Neurologia. 1989;4(8):282-7.
Tetrabenazine as antichorea therapy in Huntington disease: a randomized controlled trial. Neurology. 2006;66(3):366-72.
Muller T. Valbenazine granted breakthrough drug status for treating tardive dyskinesia. Expert Opin Investig Drugs. 2015;24(6):737-42.
Yao Z, Wei X, Wu X, Katz JL, Kopajtic T, Greig NH, et al. Preparation and evaluation of tetrabenazine enantiomers and all eight stereoisomers of dihydrotetrabenazine as VMAT2 inhibitors. European Journal of Medicinal Chemistry. 2011;46(5):1841-8.
O’Brien CF, Jimenez R, Hauser RA, Factor SA, Burke J, Mandri D, et al. NBI-98854, a selective monoamine transport inhibitor for the treatment of tardive dyskinesia: a randomized, double-blind, placebo-controlled study. Mov Disord. 2015;30(12):1681-7.
Hauser RA, Factor SA, Marder SR, Knesevich MA, Ramirez PM, Jimenez R, et al. KINECT 3: a phase 3 randomized, double-blind, placebo-controlled trial of valbenazine for tardive dyskinesia. Am J Psychiatry. 2017;174(5):476-84.
Akbar U, Kim DS, Friedman JH. Valbenazine-induced parkinsonism. Parkinsonism & Related Disorders. 2020;70:13-4.
Factor SA, Remington G, Comella CL, Correll CU, Burke J, Jimenez R, et al. The effects of valbenazine in participants with tardive dyskinesia: results of the 1-year KINECT 3 extension study. J Clin Psychiatry. 2017;78(9):1344-50.
Marder SR, Singer C, Lindenmayer JP, Tanner CM, Comella CL, Verghese C, et al. A phase 3, 1-year, open-label trial of valbenazine in adults with tardive dyskinesia. J Clin Psychopharmacol. 2019;39(6):620-7.
Sajatovic M, Alexopoulos GS, Burke J, Farahmand K, Siegert S. The effects of valbenazine on tardive dyskinesia in older and younger patients. Int J Geriatr Psychiatry. 2020;35(1):69-79.
McIntyre RS, Calabrese JR, Nierenberg AA, Farahmand K, Yonan C, Siegert S, et al. The effects of valbenazine on tardive dyskinesia in patients with a primary mood disorder. Journal of Affective Disorders. 2019;246:217-23.
Josiassen RC, Kane JM, Liang GS, Burke J, O’Brien CF. Long-term safety and tolerability of valbenazine (NBI-98854) in subjects with tardive dyskinesia and a diagnosis of schizophrenia or mood disorder. Psychopharmacol Bull. 2017;47(3):61-8.
Huntington Study G, Frank S, Testa CM, Stamler D, Kayson E, Davis C, et al. Effect of deutetrabenazine on chorea among patients with Huntington disease: a randomized clinical trial. JAMA. 2016;316(1):40-50.
Fernandez HH, Factor SA, Hauser RA, Jimenez-Shahed J, Ondo WG, Jarskog LF, et al. Randomized controlled trial of deutetrabenazine for tardive dyskinesia: the ARM-TD study. Neurology. 2017;88(21):2003-10.
Anderson KE, Stamler D, Davis MD, Factor SA, Hauser RA, Isojarvi J, et al. Deutetrabenazine for treatment of involuntary movements in patients with tardive dyskinesia (AIM-TD): a double-blind, randomised, placebo-controlled, phase 3 trial. The Lancet Psychiatry. 2017;4(8):595-604.
Fernandez HH, Stamler D, Davis MD, Factor SA, Hauser RA, Jimenez-Shahed J, et al. Long-term safety and efficacy of deutetrabenazine for the treatment of tardive dyskinesia. J Neurol Neurosurg Psychiatry. 2019;90(12):1317-23.
Thaker GK, Nguyen JA, Strauss ME, Jacobson R, Kaup BA, Tamminga CA. Clonazepam treatment of tardive dyskinesia: a practical GABAmimetic strategy. Am J Psychiatry. 1990;147(4):445-51.
Adler LA, Rotrosen J, Edson R, Lavori P, Lohr J, Hitzemann R, et al. Vitamin E treatment for tardive dyskinesia. Veterans Affairs Cooperative Study #394 Study Group. Arch Gen Psychiatry. 1999;56(9):836-41.
Zhang WF, Tan YL, Zhang XY, Chan RC, Wu HR, Zhou DF. Extract of Ginkgo biloba treatment for tardive dyskinesia in schizophrenia: a randomized, double-blind, placebo-controlled trial. J Clin Psychiatry. 2011;72(5):615-21.
Zheng W, Xiang YQ, Ng CH, Ungvari GS, Chiu HF, Xiang YT. Extract of Ginkgo biloba for tardive dyskinesia: meta-analysis of randomized controlled trials. Pharmacopsychiatry. 2016;49(3):107-11.
Jackisch R, Link T, Neufang B, Koch R. Studies on the mechanism of action of the antiparkinsonian drugs memantine and amantadine: no evidence for direct dopaminomimetic or antimuscarinic properties. Arch Int Pharmacodyn Ther. 1992;320:21-42.
Decker BL, Davis JM, Jonowsky DS, el-Yousef MK, Sekerke HJ. Amantadine hydrochloride treatment of tardive dyskinesia. N Engl J Med. 1971;285(15):860.
Angus S, Sugars J, Boltezar R, Koskewich S, Schneider NM. A controlled trial of amantadine hydrochloride and neuroleptics in the treatment of tardive dyskinesia. J Clin Psychopharmacol. 1997;17(2):88-91.
Pappa S, Tsouli S, Apostolou G, Mavreas V, Konitsiotis S. Effects of amantadine on tardive dyskinesia: a randomized, double-blind, placebo-controlled study. Clinical Neuropharmacology. 2010;33(6):271-5.
Woods SW, Saksa JR, Baker CB, Cohen SJ, Tek C. Effects of levetiracetam on tardive dyskinesia: a randomized, double-blind, placebo-controlled study. J Clin Psychiatry. 2008;69(4):546-54.
McGavin CL, John V, Musser WS. Levetiracetam as a treatment for tardive dyskinesia: a case report. Neurology. 2003;61(3):419.
Bona JR. Treatment of neuroleptic-induced tardive dyskinesia with levetiracetam: a case series. J Clin Psychopharmacol. 2006;26(2):215-6.
Konitsiotis S, Pappa S, Mantas C, Mavreas V. Levetiracetam in tardive dyskinesia: an open label study. Mov Disord. 2006;21(8):1219-21.
Meco G, Fabrizio E, Epifanio A, Morgante F, Valente M, Vanacore N, et al. Levetiracetam in tardive dyskinesia. Clinical Neuropharmacology. 2006;29(5):265-8.
Kabes J, Sikora J, Pisvejc J, Hanzlicek L, Skondia V. Effect of piracetam on extrapyramidal side effects induced by neuroleptic drugs. International Pharmacopsychiatry. 1982;17(3):185-92.
Libov I, Miodownik C, Bersudsky Y, Dwolatzky T, Lerner V. Efficacy of piracetam in the treatment of tardive dyskinesia in schizophrenic patients: a randomized, double-blind, placebo-controlled crossover study. J Clin Psychiatry. 2007;68(7):1031-7.
Lerner V, Kaptsan A, Miodownik C, Kotler M. Vitamin B6 in treatment of tardive dyskinesia: a preliminary case series study. Clinical Neuropharmacology. 1999;22(4):241-3.
Lerner V, Miodownik C, Kaptsan A, Bersudsky Y, Libov I, Sela BA, et al. Vitamin B6 treatment for tardive dyskinesia: a randomized, double-blind, placebo-controlled, crossover study. J Clin Psychiatry. 2007;68(11):1648-54.
Naidu PS, Singh A, Kaur P, Sandhir R, Kulkarni SK. Possible mechanism of action in melatonin attenuation of haloperidol-induced orofacial dyskinesia. Pharmacology, Biochemistry, and Behavior. 2003;74(3):641-8.
Zisapel N, Egozi Y, Laudon M. Inhibition of dopamine release by melatonin: regional distribution in the rat brain. Brain Res. 1982;246(1):161-3.
Shamir E, Barak Y, Shalman I, Laudon M, Zisapel N, Tarrasch R, et al. Melatonin treatment for tardive dyskinesia: a double-blind, placebo-controlled, crossover study. Arch Gen Psychiatry. 2001;58(11):1049-52.
Castro F, Carrizo E, Prieto de Rincon D, Rincon CA, Asian T, Medina-Leendertz S, et al. Effectiveness of melatonin in tardive dyskinesia. Invest Clin. 2011;52(3):252-60.
Sun CH, Zheng W, Yang XH, Cai DB, Ng CH, Ungvari GS, et al. Adjunctive melatonin for tardive dyskinesia in patients with schizophrenia: a meta-analysis. Shanghai Archives of Psychiatry. 2017;29(3):129-36.
Korsgaard S. Baclofen (Lioresal) in the treatment ofneuroleptic-induced tardive dyskinesia. Acta Psychiatrica Scandinavica. 1976;54(1):17-24.
Gerlach J, Rye T, Kristjansen P. Effect of baclofen on tardive dyskinesia. Psychopharmacology (Berl). 1978;56(2):145-51.
Stewart RM, Rollins J, Beckham B, Roffman M. Baclofen in tardive dyskinesia patients maintained on neuroleptics. Clinical Neuropharmacology. 1982;5(4):365-73.
Glazer WM, Moore DC, Bowers MB, Bunney BS, Roffman M. The treatment of tardive dyskinesia with baclofen. Psychopharmacology (Berl). 1985;87(4):480-3.
Dressler D, Oeljeschlager RO, Ruther E. Severe tardive dystonia: treatment with continuous intrathecal baclofen administration. Mov Disord. 1997;12(4):585-7.
Bacher NM, Lewis HA. Low-dose propranolol in tardive dyskinesia. Am J Psychiatry. 1980;137(4):495-7.
Wilbur R, Kulik FA. Propranolol (Inderal) for tardive dyskinesia and extrapyramidal side effects from neuroleptics: possible involvement of beta-adrenergic mechanisms. Progress in Neuro-psychopharmacology. 1980;4(6):627-32.
Perenyi A, Farkas A. Propranolol in the treatment of tardive dyskinesia. Biol Psychiatry. 1983;18(3):391-4.
Chaudhry R, Radonjic D, Waters B. Efficacy of propranolol in a patient with tardive dyskinesia and extrapyramidal syndrome. Am J Psychiatry. 1982;139(5):674-6.
Schrodt GR, Jr., Wright JH, Simpson R, Moore DP, Chase S. Treatment of tardive dyskinesia with propranolol. J Clin Psychiatry. 1982;43(8):328-31.
Silver JM, Yudofsky SC, Kogan M, Katz BL. Elevation of thioridazine plasma levels by propranolol. Am J Psychiatry. 1986;143(10):1290-2.
Factor SA. Propranolol therapy for tardive dyskinesia revisited. Mov Disord. 2012;27(13):1703.
Hatcher-Martin JM, Armstrong KA, Scorr LM, Factor SA. Propranolol therapy for tardive dyskinesia: a retrospective examination. Parkinsonism & Related Disorders. 2016;32:124-6.
Waln O, Jankovic J. Zolpidem improves tardive dyskinesia and akathisia. Mov Disord. 2013;28(12):1748-9.
Bishnoi M, Chopra K, Kulkarni SK. Possible anti-oxidant and neuroprotective mechanisms of zolpidem in attenuating typical anti-psychotic-induced orofacial dyskinesia: a biochemical and neurochemical study. Prog Neuropsychopharmacol Biol Psychiatry. 2007;31(5):1130-8.
Iwata Y, Irie S, Uchida H, Suzuki T, Watanabe K, Iwashita S, et al. Effects of zonisamide on tardive dyskinesia: a preliminary open-label trial. Journal of the Neurological Sciences. 2012;315(1-2):137-40.
Slotema CW, van Harten PN, Bruggeman R, Hoek HW. Botulinum toxin in the treatment of orofacial tardive dyskinesia: a single blind study. Prog Neuropsychopharmacol Biol Psychiatry. 2008;32(2):507-9.
Tarsy D, Kaufman D, Sethi KD, Rivner MH, Molho E, Factor S. An open-label study of botulinum toxin A for treatment of tardive dystonia. Clinical Neuropharmacology. 1997;20(1):90-3.
Brashear A, Ambrosius WT, Eckert GJ, Siemers ER. Comparison of treatment of tardive dystonia and idiopathic cervical dystonia with botulinum toxin type A. Mov Disord. 1998;13(1):158-61.
Molho ES, Feustel PJ, Factor SA. Clinical comparison of tardive and idiopathic cervical dystonia. Mov Disord. 1998;13(3):486-9.
Tan EK, Jankovic J. Tardive and idiopathic oromandibular dystonia: a clinical comparison. J Neurol Neurosurg Psychiatry. 2000;68(2):186-90.
Esper CD, Freeman A, Factor SA. Lingual protrusion dystonia: frequency, etiology and botulinum toxin therapy. Parkinsonism & Related Disorders. 2010;16(7):438-41.
Eltahawy HA, Feinstein A, Khan F, Saint-Cyr J, Lang AE, Lozano AM. Bilateral globus pallidus internus deep brain stimulation in tardive dyskinesia: a case report. Mov Disord. 2004;19(8):969-72.
Kefalopoulou Z, Paschali A, Markaki E, Vassilakos P, Ellul J, Constantoyannis C. A double-blind study on a patient with tardive dyskinesia treated with pallidal deep brain stimulation. Acta neurologica Scandinavica. 2009;119(4):269-73.
Schrader C, Peschel T, Petermeyer M, Dengler R, Hellwig D. Unilateral deep brain stimulation of the internal globus pallidus alleviates tardive dyskinesia. Mov Disord. 2004;19(5):583-5.
Damier P, Thobois S, Witjas T, Cuny E, Derost P, Raoul S, et al. Bilateral deep brain stimulation of the globus pallidus to treat tardive dyskinesia. Arch Gen Psychiatry. 2007;64(2):170-6.
Pouclet-Courtemanche H, Rouaud T, Thobois S, Nguyen JM, Brefel-Courbon C, Chereau I, et al. Long-term efficacy and tolerability of bilateral pallidal stimulation to treat tardive dyskinesia. Neurology. 2016;86(7):651-9.
Gruber D, Sudmeyer M, Deuschl G, Falk D, Krauss JK, Mueller J, et al. Neurostimulation in tardive dystonia/dyskinesia: a delayed start, sham stimulation-controlled randomized trial. Brain Stimul. 2018;11(6):1368-77.
Reese R, Volkmann J. Deep brain stimulation for the dystonias: evidence, knowledge gaps, and practical considerations. Movement Disorders Clinical Practice. 2017;4(4):486-94.
Shaikh AG, Mewes K, DeLong MR, Gross RE, Triche SD, Jinnah HA, et al. Temporal profile of improvement of tardive dystonia after globus pallidus deep brain stimulation. Parkinsonism & Related Disorders. 2015;21(2):116-9.
Deng ZD, Li DY, Zhang CC, Pan YX, Zhang J, Jin H, et al. Long-term follow-up of bilateral subthalamic deep brain stimulation for refractory tardive dystonia. Parkinsonism & Related Disorders. 2017;41:58-65.
Waln O, Jankovic J. An update on tardive dyskinesia: from phenomenology to treatment. Tremor and Other Hyperkinetic Movements. 2013;3.
Stacy M, Cardoso F, Jankovic J. Tardive stereotypy and other movement disorders in tardive dyskinesias. Neurology. 1993;43(5):937-41.
Fernandez HH, Friedman JH. Classification and treatment of tardive syndromes. Neurologist. 2003;9(1):16-27.
Acknowledgments
The author would like to thank Rachel H. Factor, PharmD, and Laura M. Scorr, MD, for their careful review and constructive comments.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Funding
The study received funding from Sartain Lanier Family Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Factor has the following disclosures: honoraria: Lundbeck, Sunovion, Biogen, Acadia, Impel, Acorda, and CereSpir; grants: Medtronics, Boston Scientific, Biohaven, Impax, Lilly, US World Meds, Sunovion Therapeutics, Vaccinex, Voyager, Jazz Pharmaceuticals, Cure Huntington's Disease Initiative Foundation, Michael J. Fox Foundation, National Institutes of Health (U10 NS077366), and Parkinson Foundation; and royalties: Demos, Blackwell Futura, Springer for textbooks, Uptodate, Other Bracket Global Limited Liability Company, and Clinical Neuroscience Solutions Ratings Limited Liability Company.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
ESM 1
(PDF 1225 kb)
Rights and permissions
About this article
Cite this article
Factor, S.A. Management of Tardive Syndrome: Medications and Surgical Treatments. Neurotherapeutics 17, 1694–1712 (2020). https://doi.org/10.1007/s13311-020-00898-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13311-020-00898-3