Abstract
Tardive dyskinesia (TD) encompasses the spectrum of iatrogenic hyperkinetic movement disorders following exposure to dopamine receptor-blocking agents (DRBAs). Despite the advent of atypical or second- and third-generation antipsychotics with a presumably lower risk of complications, TD remains a persistent and challenging problem. Prevention is the first step in mitigating the risk of TD, but early recognition, gradual withdrawal of offending medications, and appropriate treatment are also critical. As TD is often a persistent and troublesome disorder, specific antidyskinetic therapies are often needed for symptomatic relief. The vesicular monoamine transporter 2 (VMAT2) inhibitors, which include tetrabenazine, deutetrabenazine, and valbenazine, are considered the treatment of choice for most patients with TD. Deutetrabenazine—a deuterated version of tetrabenazine—and valbenazine, the purified parent product of one of the main tetrabenazine metabolites, are novel VMAT2 inhibitors and the only drugs to receive approval from the US FDA for the treatment of TD. VMAT2 inhibitors deplete presynaptic dopamine and reduce involuntary movements in many hyperkinetic movement disorders, particularly TD, Huntington disease, and Tourette syndrome. The active metabolites of the VMAT2 inhibitors have high affinity for VMAT2 and minimal off-target binding. Compared with tetrabenazine, deutetrabenazine and valbenazine have pharmacokinetic advantages that translate into less frequent dosing and better tolerability. However, no head-to-head studies have compared the various VMAT2 inhibitors. One of the major advantages of VMAT2 inhibitors over DRBAs, which are still being used by some clinicians in the treatment of some hyperkinetic disorders, including TD, is that they are not associated with the development of TD. We also briefly discuss other treatment options for TD, including amantadine, clonazepam, Gingko biloba, zolpidem, botulinum toxin, and deep brain stimulation. Treatment of TD and other drug-induced movement disorders must be individualized and based on the severity, phenomenology, potential side effects, and other factors discussed in this review.


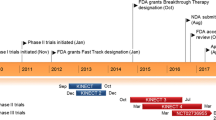
Reproduced from Jankovic [97] with permission
Similar content being viewed by others
Change history
10 March 2018
The dose (mg/day) for Clonazepam which reads:
References
Faurbye A, Rasch PJ, Petersen PB, Brandborg G, Pakkenberg H. Neurological symptoms in pharmacotherapy of psychoses. Acta Psychiatr Scand. 1964;40:10–27.
Waln O, Jankovic J. An update on tardive dyskinesia: from phenomenology to treatment. Tremor Other Hyperkinetic Mov. 2013;3:1–11.
Vijayakumar D, Jankovic J. Drug-induced dyskinesia, part 2: Treatment of tardive dyskinesia. Drugs. 2016;76:779–87.
Savitt D, Jankovic J. Tardive syndromes. J Neurol Sci. 2018 (in press).
Frei K, Truong DD, Fahn S, Jankovic J, Hauser RA. The nosology of tardive syndromes. J Neurol Sci. 2018. https://doi.org/10.1016/j.jns.2018.02.008.
Carbon M, Hsieh CH, Kane JM, Correll CU. Tardive dyskinesia prevalence in the period of second-generation antipsychotic use: a meta-analysis. J Clin Psychiatry. 2017;78:e264–78.
Correll CU, Kane JM, Citrome LL. Epidemiology, prevention, and assessment of tardive dyskinesia and advances in treatment. J Clin Psychiatry. 2017;78:1136–47.
Pillay J, Boylan K, Carrey N, Newton A, Vandermeer B, Nuspl M, et al. First- and second-generation antipsychotics in children and young adults: Systematic review update [Internet]. Agency for Healthcare Research and Quality (US); 2017 [cited 2018 Jan 20]. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28749632.
McDonagh M, Peterson K, Carson S, Fu R, Thakurta S. Drug class review: Atypical antipsychotic drugs: final update 3 report [Internet]. Portland (OR): Oregon Health & Science University; 2010. Available from: https://www-ncbi-nlm-nih-gov.ezproxyhost.library.tmc.edu/books/NBK50583/.
Kwei K, Frucht S. Acute presentation of nonmotor symptoms in parkinson’s disease. Int Rev Neurobiol. 2017;134:973–86.
Patel N, Jankovic J, Hallett M. Sensory aspects of movement disorders. Lancet Neurol. 2014;13:100–12.
Caroff SN, Campbell EC. Drug-induced extrapyramidal syndromes: implications for contemporary practice. Psychiatr Clin North Am. 2016;39:391–411.
Obeso JA. The movement disorders journal 2016 and onward. Mov Disord. 2016;31:1–2.
Walker RH. Thoughts on selected movement disorder terminology and a plea for clarity. Tremor Other Hyperkinet Mov (N Y). 2013;3. https://doi.org/10.7916/D8R49PG6.
Medication-induced movement disorders and other adverse effects of medication. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013. p. 709–14.
Emsley R, Niehaus DJH, Oosthuizen PP, Koen L, Chiliza B, Fincham D. Subjective awareness of tardive dyskinesia and insight in schizophrenia. Eur Psychiatry. 2011;26:293–6.
Cloud LJ, Zutshi D, Factor SA. Tardive dyskinesia: therapeutic options for an increasingly common disorder. Neurotherapeutics. 2014;11:166–76.
Mehta SH, Morgan JC, Sethi KD. Drug-induced movement disorders. Neurol Clin. 2015;33:153–74.
Lorberboym M, Treves TA, Melamed E, Lampl Y, Hellmann M, Djaldetti R. [123I]-FP/CIT SPECT imaging for distinguishing drug-induced parkinsonism from Parkinson’s disease. Mov Disord. 2006;21:510–4.
Lo Y-C, Peng Y-C. Amisulpride withdrawal dyskinesia: a case report. Ann Gen Psychiatry. 2017;16:25.
Blanchet PJ, Popovici R, Guitard F, Rompré PH, Lamarche C, Lavigne GJ. Pain and denture condition in edentulous orodyskinesia: comparisons with tardive dyskinesia and control subjects. Mov Disord. 2008;23:1837–42.
Shin H-Y, Yoon WT, Lee WY. Anticholinergic agents can induce oromandibular dyskinesia. J Mov Disord. 2009;2:69–71.
Vijayakumar D, Jankovic J. Drug-induced dyskinesia, part 1: treatment of levodopa-induced dyskinesia. Drugs. 2016;76:759–77.
Fekete R, Jankovic J. Upper facial chorea in Huntington disease. J Clin Mov Disord. 2014;1:7.
Cardoso F. Differential diagnosis of Huntington’s disease: what the clinician should know. Neurodegener Dis Manag. 2014;4:67–72.
Singer HS, Mink JW, Gilbert DL, Jankovic J. Inherited metabolic disorders with associated movement abnormalities. In: Movement disorders in childhood. 2nd ed. London: Academic Press; 2016. p. 337–407.
Thenganatt MA, Jankovic J. Recent advances in understanding and managing Tourette syndrome [version 1; referees: 3 approved]. F1000Research 2016, 5(F1000 Faculty Rev):152. https://doi.org/10.12688/f1000research.7424.1.
Baizabal-Carvallo JF, Jankovic J. Movement disorders in autoimmune diseases. Mov Disord. 2012;27:935–46.
Benazzi F. Rapid onset of tardive dyskinesia in Huntington disease with olanzapine. J Clin Psychopharmacol. 2002;22:438–9.
Singh SK, Jankovic J. Tardive dystonia in patients with Tourette’s syndrome. Mov Disord. 1988;3:274–80.
Kane JM, Woerner M, Lieberman J. Tardive dyskinesia: prevalence, incidence, and risk factors. J Clin Psychopharmacol. 1988;8:52S–6S.
Yassa R, Jeste DV. Gender differences in tardive dyskinesia: a critical review of the literature. Schizophr Bull. 1992;18:701–15.
Gardos G, Casey DE, Cole JO, Perenyi A, Kocsis E, Arato M, et al. Ten-year outcome of tardive dyskinesia. Am J Psychiatry. 1994;151:836–41.
Glazer WM, Morgenstern H, Doucette JT. Predicting the long-term risk of tardive dyskinesia in outpatients maintained on neuroleptic medications. J Clin Psychiatry. 1993;54:133–9.
Chakos MH, Alvir JM, Woerner MG, Koreen A, Geisler S, Mayerhoff D, et al. Incidence and correlates of tardive dyskinesia in first episode of schizophrenia. Arch Gen Psychiatry. 1996;53:313–9.
Jeste DV, Caligiuri MP, Paulsen JS, Heaton RK, Lacro JP, Harris MJ, et al. Risk of tardive dyskinesia in older patients. A prospective longitudinal study of 266 outpatients. Arch Gen Psychiatry. 1995;52:756–65.
Woerner MG, Alvir JMJ, Saltz BL, Lieberman JA, Kane JM. Prospective study of tardive dyskinesia in the elderly: rates and risk factors. Am J Psychiatry. 1998;155:1521–8.
Correll CU, Leucht S, Kane JM. Lower risk for tardive dyskinesia associated with second-generation antipsychotics: a systematic review of 1-year studies. Am J Psychiatry. 2004;161:414–25.
O’Brien A. Comparing the risk of tardive dyskinesia in older adults with first-generation and second-generation antipsychotics: a systematic review and meta-analysis. Int J Geriatr Psychiatry. 2016;31:683–93.
Leucht S, Cipriani A, Spineli L, Mavridis D, Örey D, Richter F, et al. Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis. Lancet. 2013;382:951–62.
Arnt J, Skarsfeldt T. Do novel antipsychotics have similar pharmacological characteristics? A review of the evidence. Neuropsychopharmacology. 1998;18:63–101.
Correll CU, Schenk EM. Tardive dyskinesia and new antipsychotics. Curr Opin Psychiatry. 2008;21:151–6.
Miller DD, Caroff SN, Davis SM, Rosenheck RA, McEvoy JP, Saltz BL, et al. Extrapyramidal side-effects of antipsychotics in a randomised trial. Br J Psychiatry. 2008;193:279–88.
Peluso MJ, Lewis SW, Barnes TRE, Jones PB. Extrapyramidal motor side-effects of first- and second-generation antipsychotic drugs. Br J Psychiatry. 2012;200:387–92.
Hazari N, Kate N, Grover S. Clozapine and tardive movement disorders: a review. Asian J Psychiatr. 2013;6:439–51.
Li C-R, Chung Y-C, Park T-W, Yang J-C, Kim K-W, Lee K-H, et al. Clozapine-induced tardive dyskinesia in schizophrenic patients taking clozapine as a first-line antipsychotic drug. World J Biol Psychiatry. 2009;10:919–24.
Davé M. Clozapine-related tardive dyskinesia. Biol Psychiatry. 1994;35:886–7.
Molho ES, Factor SA. Possible tardive dystonia resulting from clozapine therapy. Mov Disord. 1999;14:873–4.
Peña MS, Yaltho TC, Jankovic J. Tardive dyskinesia and other movement disorders secondary to aripiprazole. Mov Disord. 2011;26:147–52.
Paulson GW, Rizvi CA, Crane GE. Tardive dyskinesia as a possible sequel of long-term therapy with phenothiazines. Clin Pediatr (Phila). 1975;14:953–5.
Campbell M, Armenteros JL, Malone RP, Adams PB, Eisenberg ZW, Overall JE. Neuroleptic-related dyskinesias in autistic children: a prospective, longitudinal study. J Am Acad Child Adolesc Psychiatry. 1997;36:835–43.
McAndrew JB, Case Q, Treffert DA. Effects of prolonged phenothiazine intake on psychotic and other hospitalized children. J Autism Child Schizophr. 1972;2:75–91.
Mejia NI, Jankovic J. Tardive dyskinesia and withdrawal emergent syndrome in children. Expert Rev Neurother. 2010;10:893–901.
Wonodi I, Reeves G, Carmichael D, Verovsky I, Avila MT, Elliott A, et al. Tardive dyskinesia in children treated with atypical antipsychotic medications. Mov Disord. 2007;22:1777–82.
Garcia-Amador M, Merchán-Naranjo J, Tapia C, Moreno C, Castro-Fornieles J, Baeza I, et al. Neurological adverse effects of antipsychotics in children and adolescents. J Clin Psychopharmacol. 2015;35:686–93.
Hugenholtz GWK, Heerdink ER, Stolker JJ, Meijer WEE, Egberts ACG, Nolen WA. Haloperidol dose when used as active comparator in randomized controlled trials with atypical antipsychotics in schizophrenia: comparison with officially recommended doses. J Clin Psychiatry. 2006;67:897–903.
Rakesh G, Muzyk A, Szabo ST, Gupta S, Pae C-U, Masand P. Tardive dyskinesia: 21st century may bring new treatments to a forgotten disorder. Ann Clin Psychiatry. 2017;29:108–19.
Achalia RM, Chaturvedi SK, Desai G, Rao GN, Prakash O. Prevalence and risk factors associated with tardive dyskinesia among Indian patients with schizophrenia. Asian J Psychiatr. 2014;9:31–5.
van Harten PN, Hoek HW, Matroos GE, Koeter M, Kahn RS. Intermittent neuroleptic treatment and risk for tardive dyskinesia: Curaçao Extrapyramidal Syndromes Study III. Am J Psychiatry. 1998;155:565–7.
Xiang Y-T, Wang C-Y, Si T-M, Lee EHM, He Y-L, Ungvari GS, et al. Sex differences in use of psychotropic drugs and drug-induced side effects in schizophrenia patients: findings of the research on Asia psychotropic prescription (REAP) studies. Aust N Zeal J Psychiatry. 2011;45:193–8.
Zhang XY, Chen DC, Qi LY, Wang F, Xiu MH, Chen S, et al. Gender differences in the prevalence, risk and clinical correlates of tardive dyskinesia in Chinese schizophrenia. Psychopharmacology. 2009;205:647–54.
Tenback DE, van Harten PN, van Os J. Non-therapeutic risk factors for onset of tardive dyskinesia in schizophrenia: a meta-analysis. Mov Disord. 2009;24:2309–15.
Wijemanne S, Jankovic J, Evans RW. Movement disorders from the use of metoclopramide and other antiemetics in the treatment of migraine. Headache J Head Face Pain. 2016;56:153–61.
Kenney C, Hunter C, Davidson A, Jankovic J. Metoclopramide, an increasingly recognized cause of tardive dyskinesia. J Clin Pharmacol. 2008;48:379–84.
Pasricha PJ, Pehlivanov N, Sugumar A, Jankovic J. Drug Insight: from disturbed motility to disordered movement—a review of the clinical benefits and medicolegal risks of metoclopramide. Nat Clin Pract Gastroenterol Hepatol. 2006;3:138–48.
Mejia NI, Jankovic J. Metoclopramide-induced tardive dyskinesia in an infant. Mov Disord. 2005;20:86–9.
Loonen AJM, Ivanova SA. New insights into the mechanism of drug-induced dyskinesia. CNS Spectr. 2013;18:15–20.
Stahl SM. Neuronal traffic signals in tardive dyskinesia: not enough “stop” in the motor striatum. CNS Spectr. 2017;22:427–34.
Turrone P, Remington G, Kapur S, Nobrega JN. The relationship between dopamine D2 receptor occupancy and the vacuous chewing movement syndrome in rats. Psychopharmacology. 2003;165:166–71.
Silvestri S, Seeman MV, Negrete JC, Houle S, Shammi CM, Remington GJ, et al. Increased dopamine D2 receptor binding after long-term treatment with antipsychotics in humans: a clinical PET study. Psychopharmacology. 2000;152:174–80.
Strange PG. Antipsychotic drugs: importance of dopamine receptors for mechanisms of therapeutic actions and side effects. Pharmacol Rev. 2001;53:119–33.
Seeman P. Dopamine D2 receptors as treatment targets in schizophrenia. Clin Schizophr Relat Psychoses. 2010;4:56–73.
Shi J, Tan YL, Wang ZR, An HM, Li J, Wang YC, et al. Ginkgo biloba and vitamin E ameliorate haloperidol-induced vacuous chewingmovement and brain-derived neurotrophic factor expression in a rat tardive dyskinesia model. Pharmacol Biochem Behav. 2016;148:53–8.
Teo JT, Edwards MJ, Bhatia K. Tardive dyskinesia is caused by maladaptive synaptic plasticity: a hypothesis. Mov Disord. 2012;27:1205–15.
Lanning RK, Zai CC, Müller DJ. Pharmacogenetics of tardive dyskinesia: an updated review of the literature. Pharmacogenomics. 2016;17:1339–51.
Guy W. AIMS: ECDEU assessment manual for psychopharmacology. Washington, DC: Government Printing Office; 1976. p. 534–7.
Munetz MR, Benjamin S. How to examine patients using the Abnormal Involuntary Movement Scale. Hosp Community Psychiatry. 1988;39:1172–7.
Bark N, Florida D, Gera N, Varardi R, Harghel L, Adlington K. Evaluation of the routine clinical use of the Brief Psychiatric Rating Scale (BPRS) and the Abnormal Involuntary Movement Scale (AIMS). J Psychiatr Pract. 2011;17:300–3.
Suzuki T. Which rating scales are regarded as “the standard” in clinical trials for schizophrenia? A critical review. Psychopharmacol Bull. 2011;44:18–31.
Lane RD, Glazer WM, Hansen TE, Berman WH, Kramer SI. Assessment of tardive dyskinesia using the Abnormal Involuntary Movement Scale. J Nerv Ment Dis. 1985;173:353–7.
Gerlach J, Korsgaard S, Clemmesen P, Lauersen AM, Magelund G, Noring U, et al. The St. Hans Rating Scale for extrapyramidal syndromes: reliability and validity. Acta Psychiatr Scand. 1993;87:244–52.
Domino ME, Swartz MS. Who are the new users of antipsychotic medications? Psychiatr Serv. 2008;59:507–14.
Huskamp HA, Horvitz-Lennon M, Berndt ER, Normand S-LT, Donohue JM. Patterns of antipsychotic prescribing by physicians to young children. Psychiatr Serv. 2016;67:1307–14.
Hálfdánarson Ó, Zoëga H, Aagaard L, Bernardo M, Brandt L, Fusté AC, et al. International trends in antipsychotic use: a study in 16 countries, 2005–2014. Eur Neuropsychopharmacol. 2017;27:1064–76.
Seeberger LC, Hauser RA. Valbenazine for the treatment of tardive dyskinesia. Expert Opin Pharmacother. 2017;18:1279–87.
Ehrenpreis ED, Deepak P, Sifuentes H, Devi R, Du H, Leikin JB. The metoclopramide black box warning for tardive dyskinesia: effect on clinical practice, adverse event reporting, and prescription drug lawsuits. Am J Gastroenterol. 2013;108:866–72.
Lehman AF, Lieberman JA, Dixon LB, McGlashan TH, Miller AL, Perkins DO, et al. Practice guideline for the treatment of patients with schizophrenia, second edition. Am J Psychiatry. 2004;161:1–56.
Viguera AC, Baldessarini RJ, Hegarty JD, van Kammen DP, Tohen M. Clinical risk following abrupt and gradual withdrawal of maintenance neuroleptic treatment. Arch Gen Psychiatry. 1997;54:49–55.
Bhidayasiri R, Fahn S, Weiner WJ, Gronseth GS, Sullivan KL, Zesiewicz TA, et al. Evidence-based guideline: treatment of tardive syndromes: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2013;81:463–9.
Sahli ZT, Tarazi FI. Pimavanserin: novel pharmacotherapy for Parkinson’s disease psychosis. Expert Opin Drug Discov. 2018;13:103–10.
Glazer WM, Morgenstern H, Schooler N, Berkman CS, Moore DC. Predictors of improvement in tardive dyskinesia following discontinuation of neuroleptic medication. Br J Psychiatry. 1990;157:585–92.
Zutshi D, Cloud LJ, Factor SA. Tardive syndromes are rarely reversible after discontinuing dopamine receptor blocking agents: experience from a university-based movement disorder clinic. Tremor Other Hyperkinetic Mov (N Y). 2014;4:266.
Modestin J, Wehrli MV, Stephan PL, Agarwalla P. Evolution of neuroleptic-induced extrapyramidal syndromes under long-term neuroleptic treatment. Schizophr Res. 2008;100:97–107.
Fernandez HH, Krupp B, Friedman JH. The course of tardive dyskinesia and parkinsonism in psychiatric inpatients: 14-year follow-up. Neurology. 2001;56:805–7.
Bhidayasiri R, Jitkritsadakul O, Friedman JH, Fahn S. Updating the recommendations for treatment of tardive syndromes: a systematic review of new evidence and practical treatment algorithm. J Neurol Sci. 2018. https://doi.org/10.1016/j.jns.2018.02.010.
Lawal HO, Krantz DE. SLC18: vesicular neurotransmitter transporters for monoamines and acetylcholine. Mol Aspects Med. 2013;34:360–72.
Jankovic J. Progress in Parkinson disease and other movement disorders. Nat Rev Neurol. 2017;13:76–8.
Benarroch EE. Monoamine transporters: structure, regulation, and clinical implications. Neurology. 2013;81:761–8.
Jankovic J. Dopamine depleters in the treatment of hyperkinetic movement disorders. Expert Opin Pharmacother. 2016;17:2461–70.
LeWitt PA. Tardive dyskinesia caused by tetrabenazine. Clin Neuropharmacol. 2013;36:92–3.
Caroff SN, Davis VG, Miller DD, Davis SM, Rosenheck RA, McEvoy JP, et al. Treatment outcomes of patients with tardive dyskinesia and chronic schizophrenia. J Clin Psychiatry. 2011;72:295–303.
Stahl SM. Mechanism of action of vesicular monoamine transporter 2 (VMAT2) inhibitors in tardive dyskinesia: reducing dopamine leads to less “go” and more “stop” from the motor striatum for robust therapeutic effects. CNS Spectr. 2017;23:1–6.
Lundbeck. Xenazine (tetrabenazine), Highlights of Prescribing Information. [cited 2018 Jan 4]; Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/021894s010lbl.pdf.
Austedo (deutetrabenazine) Tablets, Medical Review(s). [cited 2018 Jan 4]; Available from: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2017/208082Orig1s000TOC.cfm.
Grigoriadis DE, Smith E, Hoare SRJ, Madan A, Bozigian H. Pharmacologic characterization of valbenazine (NBI-98854) and its metabolites. J Pharmacol Exp Ther. 2017;361:454–61.
Mehanna R, Hunter C, Davidson A, Jimenez-Shahed J, Jankovic J. Analysis of CYP2D6 genotype and response to tetrabenazine. Mov Disord. 2013;28:210–5.
Teva Pharmaceuticals. Austedo (deutetrabenazine), Highlights of Prescribing Information. [cited 2018 Jan 4]; Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/208082s000lbl.pdf.
Neurocrine Biosciences. Ingrezza (valbenazine), Highlights of Prescribing Information. [cited 2018 Jan 4]; Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/209241lbl.pdf.
Ondo WG, Hanna PA, Jankovic J. Tetrabenazine treatment for tardive dyskinesia: assessment by randomized videotape protocol. Am J Psychiatry. 1999;156:1279–81.
Kazamatsuri H, Chien C, Cole JO. Treatment of tardive dyskinesia. I. Clinical efficacy of a dopamine-depleting agent, tetrabenazine. Arch Gen Psychiatry. 1972;27:95–9.
Kenney C, Hunter C, Jankovic J. Long-term tolerability of tetrabenazine in the treatment of hyperkinetic movement disorders. Mov Disord. 2007;22:193–7.
Jankovic J, Beach J. Long-term effects of tetrabenazine in hyperkinetic movement disorders. Neurology. 1997;48:358–62.
Kenney C, Hunter C, Mejia N, Jankovic J. Is history of depression a contraindication to treatment with tetrabenazine? Clin Neuropharmacol. 2006;29:259–64.
Gant TG. Using deuterium in drug discovery: leaving the label in the drug. J Med Chem. 2014;57:3595–611.
Stamler D, Bradbury M, Brown F. The pharmacokinetics and safety of deuterated-tetrabenazine. Neurology. 2013;80:P07.210.
Fernandez HH, Factor SA, Hauser RA, Jimenez-Shahed J, Ondo WG, Jarskog LF, et al. Randomized controlled trial of deutetrabenazine for tardive dyskinesia. Neurology. 2017;88:2003–10.
Anderson KE, Stamler D, Davis MD, Factor SA, Hauser RA, Isojärvi J, et al. Deutetrabenazine for treatment of involuntary movements in patients with tardive dyskinesia (AIM-TD): a double-blind, randomised, placebo-controlled, phase 3 trial. Lancet Psychiatry. 2017;4:595–604.
Citrome L. Deutetrabenazine for tardive dyskinesia: a systematic review of the efficacy and safety profile for this newly approved novel medication-What is the number needed to treat, number needed to harm and likelihood to be helped or harmed? Int J Clin Pract. 2017;71:e13030.
ClinicalTrials.gov. Reducing involuntary movements in tardive dyskinesia. NCT02198794. [Internet]. Auspex Pharm. Inc. 2017 [cited 2017 Nov 6]. Available from: https://clinicaltrials.gov/ct2/show/NCT02198794.
Anderson K, Stamler D, Davis M, Factor S, Hauser R, Isojärvi J, et al. Long-term safety of deutetrabenazine for the treatment of tardive dyskinesia: results from an open-label, long-term study [abstract]. Mov Disord. 2017;32 (suppl 2). [Internet]. [cited 2018 Jan 4]. Available from: http://www.mdsabstracts.org/abstract/long-term-safety-of-deutetrabenazine-for-the-treatment-of-tardive-dyskinesia-results-from-an-open-label-long-term-study/.
Frank S, Stamler D, Kayson E, Claassen DO, Colcher A, Davis C, et al. Safety of converting from tetrabenazine to deutetrabenazine for the treatment of chorea. JAMA Neurol. 2017;74:977–82.
Bashir H, Jankovic J. Treatment options for chorea. Expert Rev Neurother. 2018;18:51–63.
Jankovic J, Jimenez-Shahed J, Budman C, Coffey B, Murphy T, Shprecher D, et al. Deutetrabenazine in tics associated with tourette syndrome. Tremor Other Hyperkinetic Mov (N Y). 2016;6:422.
Müller T. Valbenazine for the treatment of tardive dyskinesia. Expert Rev Neurother. 2017;17:1135–44.
Caroff SN, Aggarwal S, Yonan C. Treatment of tardive dyskinesia with tetrabenazine or valbenazine: a systematic review. J Comp Eff Res. 2017;6:422.
O’Brien CF, Jimenez R, Hauser RA, Factor SA, Burke J, Mandri D, et al. NBI-98854, a selective monoamine transport inhibitor for the treatment of tardive dyskinesia: A randomized, double-blind, placebo-controlled study. Mov Disord. 2015;30:1681–7.
Hauser RA, Factor SA, Marder SR, Knesevich MA, Ramirez PM, Jimenez R, et al. KINECT 3: a phase 3 randomized, double-blind, placebo-controlled trial of valbenazine for tardive dyskinesia. Am J Psychiatry. 2017;174:476–84.
Citrome L. Valbenazine for tardive dyskinesia: A systematic review of the efficacy and safety profile for this newly approved novel medication-What is the number needed to treat, number needed to harm and likelihood to be helped or harmed? Int J Clin Pract. 2017;71:e12964.
Thai-Cuarto D, O’Brien CF, Jimenez R, Liang GS, Burke J. Cardiovascular profile of valbenazine: analysis of pooled data from three randomized, double-blind, placebo-controlled trials. Drug Saf. 2017. https://doi.org/10.1007/s40264-017-0623-1.
Factor SA, Remington G, Comella CL, Correll CU, Burke J, Jimenez R, et al. The effects of valbenazine in participants with tardive dyskinesia: results of the 1-year KINECT 3 extension study. J Clin Psychiatry. 2017;78:1344–50.
Angus S, Sugars J, Boltezar R, Koskewich S, Schneider NM. A controlled trial of amantadine hydrochloride and neuroleptics in the treatment of tardive dyskinesia. J Clin Psychopharmacol. 1997;17:88–91.
Pappa S, Tsouli S, Apostolou G, Mavreas V, Konitsiotis S. Effects of amantadine on tardive dyskinesia: a randomized, double-blind, placebo-controlled study. Clin Neuropharmacol. 2010;33:271–5.
Thaker GK, Nguyen JA, Strauss ME, Jacobson R, Kaup BA, Tamminga CA. Clonazepam treatment of tardive dyskinesia: a practical GABAmimetic strategy. Am J Psychiatry. 1990;147:445–51.
Zheng W, Xiang Y-Q, Ng C, Ungvari G, Chiu H, Xiang Y-T. Extract of Ginkgo biloba for tardive dyskinesia: meta-analysis of randomized controlled trials. Pharmacopsychiatry. 2016;49:107–11.
Zhang W-F, Tan Y-L, Zhang X-Y, Chan RCK, Wu H-R, Zhou D-F. Extract of Ginkgo biloba treatment for tardive dyskinesia in schizophrenia: a randomized, double-blind, placebo-controlled trial. J Clin Psychiatry. 2011;72:615–21.
Zhang XY, Zhang W-F, Zhou D-F, Chen DC, Xiu MH, Wu H-R, et al. Brain-derived neurotrophic factor levels and its Val66Met gene polymorphism predict tardive dyskinesia treatment response to Ginkgo biloba. Biol Psychiatry. 2012;72:700–6.
Desmarais JE, Beauclair L, Annable L, Bélanger M-C, Kolivakis TT, Margolese HC. Effects of discontinuing anticholinergic treatment on movement disorders, cognition and psychopathology in patients with schizophrenia. Ther Adv Psychopharmacol. 2014;4:257–67.
Vinogradov S, Fisher M, Warm H, Holland C, Kirshner MA, Pollock BG. The cognitive cost of anticholinergic burden: Decreased response to cognitive training in schizophrenia. Am J Psychiatry. 2009;166:1055–62.
Aquino CCH, Lang AE. Tardive dyskinesia syndromes: current concepts. Parkinsonism Relat Disord. 2014;20:S113–7.
Waln O, Jankovic J. Zolpidem improves tardive dyskinesia and akathisia. Mov Disord. 2013;28:1748–9.
Jankovic J. An update on new and unique uses of botulinum toxin in movement disorders. Toxicon. 2017. https://doi.org/10.1016/j.toxicon.2017.09.003.
Tan EK, Jankovic J. Tardive and idiopathic oromandibular dystonia: a clinical comparison. J Neurol Neurosurg Psychiatry. 2000;68:186–90.
Morigaki R, Mure H, Kaji R, Nagahiro S, Goto S. Therapeutic perspective on tardive syndrome with special reference to deep brain stimulation. Front Psychiatry. 2016;7:207.
Sun B, Chen S, Zhan S, Le W, Krahl SE. Subthalamic nucleus stimulation for primary dystonia and tardive dystonia. Acta Neurochir Suppl. 2007;97:207–14.
Meng D-W, Liu H-G, Yang A-C, Zhang K, Zhang J-G. Long-term effects of subthalamic nucleus deep brain stimulation in tardive dystonia. Chin Med J (Engl). 2016;129:1257–8.
Yasui-Furukori N, Nakamura K, Katagai H, Kaneko S. The effects of electroconvulsive therapy on tardive dystonia or dyskinesia induced by psychotropic medication: a retrospective study. Neuropsychiatr Dis. Treat. 2014;10:1209–12.
Peng L-Y, Lee Y, Lin P-Y. Electroconvulsive therapy for a patient with persistent tardive dyskinesia. J ECT. 2013;29:e52–4.
Manteghi A, Hojjat SK, Javanbakht A. Remission of tardive dystonia with electroconvulsive therapy. J Clin Psychopharmacol. 2009;29:314–5.
Funding
No sources of funding were used to conduct this study or prepare this manuscript.
Author information
Authors and Affiliations
Contributions
NN contributed to the conception, design, organization, and execution of the study and the writing of the first and subsequent drafts. JJ contributed to the conception, design, organization, and execution of the study, to review and critique, and to writing of the second and subsequent drafts.
Corresponding author
Ethics declarations
Conflict of interest
Nicki Niemann has no conflicts of interest that are directly relevant to the content of this study. Dr. Jankovic has received research and/or training grants from Adamas Pharmaceuticals, Inc.; Allergan, Inc.; Biotie Therapies; CHDI Foundation; Civitas/Acorda Therapeutics; Dystonia Coalition; Dystonia Medical Research Foundation; F. Hoffmann-La Roche Ltd; Huntington Study Group; Kyowa Haako Kirin Pharma, Inc.; Medtronic Neuromodulation; Merz Pharmaceuticals; Michael J. Fox Foundation for Parkinson Research; National Institutes of Health; Neurocrine Biosciences; NeuroDerm Ltd; Parkinson’s Foundation; Nuvelution; Parkinson Study Group; Pfizer Inc.; Prothena Biosciences Inc.; Psyadon Pharmaceuticals, Inc.; Revance Therapeutics, Inc.; Sangamo BioSciences, Inc.; St. Jude Medical; and Teva Pharmaceutical Industries Ltd. Dr. Jankovic has served as a consultant or as an advisory committee member for Adamas Pharmaceuticals, Inc.; Allergan, Inc.; Merz Pharmaceuticals; Pfizer Inc.; Prothena Biosciences; Revance Therapeutics, Inc.; and Teva Pharmaceutical Industries Ltd. Dr. Jankovic has also received royalties or other payments from Cambridge; Elsevier; Future Science Group; Hodder Arnold; Medlink: Neurology; Lippincott Williams and Wilkins; and Wiley-Blackwell.
Additional information
The original version of this article was revised: Due to Figure 1 update.
Rights and permissions
About this article
Cite this article
Niemann, N., Jankovic, J. Treatment of Tardive Dyskinesia: A General Overview with Focus on the Vesicular Monoamine Transporter 2 Inhibitors. Drugs 78, 525–541 (2018). https://doi.org/10.1007/s40265-018-0874-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-018-0874-x