Abstract
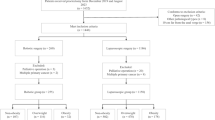
The aim of this pooled analysis was to evaluate the impact of robotic total mesorectal excision (TME) on pathology metrics in Male Overweight patients with Low rectal cancer (MOL). This was a multicenter retrospective pooled analysis of data. Two groups were defined: MOL (Male, Overweight, Low rectal cancer) and non-MOL. Overweight was defined as BMI ≥ 25 kg/m2. Low rectal cancer was defined as cancer within 6 cm from the anal verge. The primary endpoints of this study were histopathological metrics, namely circumferential resection margin (CRM) (mm), CRM involvement rate (%), and the quality of TME. Circumferential resection margin (CRM) was involved if < 1 mm. 836 (106 MOL and 730 non-MOL) patients that underwent robotic TME by six surgeons over 3 years were compared. No significant differences in demographics and perioperative variables were found, except for operating time, distal margin, and number of lymph nodes harvested. CRM involvement rate did not significantly differ (7.5% vs. 5.5%, p = 0.395). Mean CRM was statistically significantly narrower in MOL patients (6.6 vs. 7.7 mm, p = 0.04). Quality of TME did not differ. Distance of tumor from the anal verge was the only independent predictor of CRM involvement. Robotic TME may provide optimal pathology metrics in overweight males with low rectal cancer. Although CRM was a few millimeters narrower in MOL, the values were within the range of uninvolved margins making the difference statistically significant, but not clinically. Being MOL was not a risk factor for involvement of circumferential resection margin.




Similar content being viewed by others
Data availability
Data of this study are not available for dissemination. Data can be made available to the editor on reasonable request.
References
Heald RJ (1988) The “Holy Plane” of rectal surgery. J Roy Soc Med 81(9):503–508
Chapuis P, Bokey L, Fahrer M, Sinclair G, Bogduk N (2002) Mobilization of the rectum: anatomic concepts and the bookshelf revisited. Dis Colon Rectum 45(1):1–8 (discussion 8-9)
Nagtegaal ID, van de Velde CJH, van der Worp E, Kapiteijn E, Quirke P, van Krieken JHJM et al (2002) Macroscopic evaluation of rectal cancer resection specimen: clinical significance of the pathologist in quality control. J Clin Oncol 20(7):1729–1734
Quirke P, Steele R, Monson J, Grieve R, Khanna S, Couture J et al (2009) Effect of the plane of surgery achieved on local recurrence in patients with operable rectal cancer: a prospective study using data from the MRC CR07 and NCIC-CTG CO16 randomised clinical trial. Lancet 373(9666):821–828
Birbeck KF, Macklin CP, Tiffin NJ, Parsons W, Dixon MF, Mapstone NP et al (2002) Rates of circumferential resection margin involvement vary between surgeons and predict outcomes in rectal cancer surgery. Ann Surg 235(4):449–457
Oh SY, Kim YB, Paek OJ, Suh KW (2011) Does total mesorectal excision require a learning curve? Analysis from the database of a single surgeon’s experience. World J Surg 35(5):1130–1136
Bendl R, Bergamaschi R (2016) Transanal TME: a bum rap? Colorectal Dis 18(1):7–8
Veldkamp R, Kuhry E, Hop WCJ, Jeekel J, Kazemier G, Bonjer HJ et al (2005) Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol 6(7):477–484
Colon Cancer Laparoscopic or Open Resection Study Group, Buunen M, Veldkamp R, Hop WCJ, Kuhry E, Jeekel J et al (2009) Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol 10(1):44–52
van der Pas MH, Haglind E, Cuesta MA, Fürst A, Lacy AM, Hop WC et al (2013) Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol 14(3):210–218
Law CK, Stevenson ARL, Solomon M, Hague W, Wilson K, Simes JR et al (2022) Healthcare costs of laparoscopic versus open surgery for rectal cancer patients in the first 12 months: a secondary endpoint analysis of the Australasian laparoscopic cancer of the rectum trial (ALaCaRT). Ann Surg Oncol 29(3):1923–1934
Kang SB, Park JW, Jeong SY, Nam BH, Choi HS, Kim DW et al (2010) Open versus laparoscopic surgery for mid or low rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): short-term outcomes of an open-label randomised controlled trial. Lancet Oncol 11(7):637–645
Fleshman J, Branda M, Sargent DJ, Boller AM, George V, Abbas M et al (2015) Effect of laparoscopic-assisted resection vs open resection of stage II or III rectal cancer on pathologic outcomes: the ACOSOG Z6051 randomized clinical trial. JAMA 314(13):1346–1355
Mak TWC, Lee JFY, Futaba K, Hon SSF, Ngo DKY, Ng SSM (2014) Robotic surgery for rectal cancer: a systematic review of current practice. World J Gastrointest Oncol 6(6):184–193
Ackerman SJ, Daniel S, Baik R, Liu E, Mehendale S, Tackett S et al (2018) Comparison of complication and conversion rates between robotic-assisted and laparoscopic rectal resection for rectal cancer: which patients and providers could benefit most from robotic-assisted surgery? J Med Econ 21(3):254–261
Chen B, Zhang Y, Zhao S, Yang T, Wu Q, Jin C et al (2016) The impact of general/visceral obesity on completion of mesorectum and perioperative outcomes of laparoscopic TME for rectal cancer: a STARD-compliant article. Medicine (Baltimore) 95(36):e4462
Crolla RMPH, Coffey JC, Consten EJC (2022) The mesentery in robot-assisted total mesorectal excision. Clin Colon Rectal Surg 35(4):298–305
Ahmed J, Cao H, Panteleimonitis S, Khan J, Parvaiz A (2017) Robotic vs laparoscopic rectal surgery in high-risk patients. Colorectal Dis 19(12):1092–1099
de Jesus JP, Valadão M, de Castro Araujo RO, Cesar D, Linhares E, Iglesias AC (2016) The circumferential resection margins status: a comparison of robotic, laparoscopic and open total mesorectal excision for mid and low rectal cancer. Eur J Surg Oncol 42(6):808–812
Achilli P, Radtke TS, Lovely JK, Behm KT, Mathis KL, Kelley SR et al (2021) Preoperative predictive risk to cancer quality in robotic rectal cancer surgery. Eur J Surg Oncol 47(2):317–322
Barnajian M, Pettet D, Kazi E, Foppa C, Bergamaschi R (2014) Quality of total mesorectal excision and depth of circumferential resection margin in rectal cancer: a matched comparison of the first 20 robotic cases. Colorectal Dis 16(8):603–609
D’Annibale A, Pernazza G, Monsellato I, Pende V, Lucandri G, Mazzocchi P et al (2013) Total mesorectal excision: a comparison of oncological and functional outcomes between robotic and laparoscopic surgery for rectal cancer. Surg Endosc 27(6):1887–1895
Aselmann H, Kersebaum JN, Bernsmeier A, Beckmann JH, Möller T, Egberts JH et al (2018) Robotic-assisted total mesorectal excision (TME) for rectal cancer results in a significantly higher quality of TME specimen compared to the laparoscopic approach-report of a single-center experience. Int J Colorectal Dis 33(11):1575–1581
Park JS, Lee SM, Choi GS, Park SY, Kim HJ, Song SH et al (2023) Comparison of laparoscopic versus robot-assisted surgery for rectal cancers: the COLRAR randomized controlled trial. Ann Surg. https://doi.org/10.1097/SLA.0000000000005788
Sun XY, Xu L, Lu JY, Zhang GN (2019) Robotic versus conventional laparoscopic surgery for rectal cancer: systematic review and meta-analysis. Minim Invasive Ther Allied Technol 28(3):135–142
Kim MJ, Park SC, Park JW, Chang HJ, Kim DY, Nam BH et al (2018) Robot-assisted versus laparoscopic surgery for rectal cancer: a phase II open label prospective randomized controlled trial. Ann Surg 267(2):243–251
Jayne D, Pigazzi A, Marshall H, Croft J, Corrigan N, Copeland J et al (2017) Effect of Robotic-Assisted vs Conventional laparoscopic surgery on risk of conversion to open laparotomy among patients undergoing resection for rectal cancer: the ROLARR randomized clinical trial. JAMA 318(16):1569–1580
Felsenreich DM, Gachabayov M, Bergamaschi R, RESURRECT Study Group (2023) Does the mesorectal fat area impact the histopathology metrics of the specimen in males undergoing TME for distal rectal cancer? Updates Surg. 75(3):581–588
Sylla P (2023) Multicenter Phase II Study of Transanal Total Mesorectal Excision (taTME) With Laparoscopic Assistance for Rectal Cancer [Internet]. clinicaltrials.gov [cited 2023 Jun 6]. Report No.: NCT03144765. Available from: https://clinicaltrials.gov/ct2/show/NCT03144765
Acknowledgements
RESURRECT Study Group: Seon-Hahn Kim, Colorectal Division, Department of Surgery, Korea University Anam Hospital, Korea University College of Medicine, Seoul, South Korea; Guglielmo Niccolo Piozzi, Colorectal Division, Department of Surgery, Korea University Anam Hospital, Korea University College of Medicine, Seoul, South Korea; Rosa Jimenez-Rodriguez, Section of Colorectal Surgery, Hospital Universitario Virgen del Rocio, Sevilla, Spain; Li-Jen Kuo, Division of Colorectal Surgery, Department of Surgery, Taipei Medical University Hospital, Taipei, Taiwan; Tomohiro Yamaguchi, Division of Colon and Rectal Surgery, Shizuoka Cancer Center Hospital, Shizuoka, Japan; Fabio Cianchi, Department of Surgery and Translational Medicine, Careggi Hospital, University of Florence, Florence, Italy; Oktar Asoglu, Department of Surgery, Bosphorus Clinical Research Academy, Istanbul, Turkey; Vusal Aliyev, Department of Surgery, Istanbul Florence Nightingale Hospital, Istanbul, Turkey; Dejan Ignjatovic, Department of Surgery, Akershus University Hospital, Lørenskog, Norway; Yosef Nasseri, Department of Surgery, Cedar Sinai Medical Center, Los Angeles, CA, USA; Moshe Barnajian, Department of Surgery, Cedar Sinai Medical Center, Los Angeles, CA, USA; Dorin E. Popa, Linköping University Hospital, Linköping, Sweden; Mirkhalig Javadov, Department of Surgery, Medicana International Atasehir Istanbul, Turkey
Funding
This research received no external funding.
Author information
Authors and Affiliations
Consortia
Contributions
Conceptualization, MG and RB; methodology, MG and RB; software, MG and RB; validation, MG, HL, AK, and RB; formal analysis, MG; investigation, MG and HL; resources, AK; data curation, MG and RB; writing—original draft preparation, MG and HL; writing—review and editing, MG, HL, AK, and RB; visualization, MG, HL, AK, and RB; supervision, RB; project administration, RB; funding acquisition, none.
Corresponding author
Ethics declarations
Conflict of interest
All authors disclose financial or non-financial interests that are directly or indirectly related to the work submitted for publication.
Research involving human participants and/or animals
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by Western Institutional Review Board (reference number: 1-1329396-1).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Please see Acknowledgements for coauthors in the RESURRECT Study Group.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gachabayov, M., Lee, H., Kajmolli, A. et al. Impact of robotic total mesorectal excision upon pathology metrics in overweight males with low rectal cancer: a pooled analysis of 836 cases. Updates Surg 76, 505–512 (2024). https://doi.org/10.1007/s13304-023-01733-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-023-01733-y