Abstract
Background
The aim of this study was to evaluate whether the visceral fat area (VFA) has an impact on the histopathology specimen metrics of male patients undergoing robotic total mesorectal resection (rTME) for distal rectal cancer.
Methods
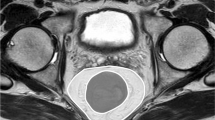
Prospectively collected data of patients undergoing rTME for resectable rectal cancer by five surgeons during a period of three years were extracted from the REgistry of Robotic SURgery for RECTal cancer (RESURRECT). VFA was measured in all patients at preoperative computed tomography. Distal rectal cancer was defined as <6cm from the anal verge. The histopathology metrics included circumferential resection margin (CRM) (in mm) and its involvement rate (if <1mm), distal resection margin (DRM), and quality of TME (complete, nearly-complete, incomplete).
Results
Of 839 patients who underwent rTME, 500 with distal rectal cancer were included. One hundred and six (21.2%) males with VFA>100cm2 were compared to 394 (78.8%) males or females with VFA≤100cm2. The mean CRM of males with VFA>100cm2 was not significantly different from its counterpart (6.6 ± 4.8 mm versus 7.1 ± 9.5mm; p=0.752). CRM involvement rates were 7.6% in both groups (p=1.000). The DRM was not significantly different: 1.8±1.9cm versus 1.8±2.6cm; p=0.996. The quality of TME did not significantly differ: complete TME 87.3% vs. 83.7%; nearly complete TME 8.9% vs. 12.8%; incomplete TME 3.8% vs. 3.6%. Complications and clinical outcomes did not significantly differ.
Conclusion
This study did not find evidence to support that increased VFA would result in suboptimal histopathology specimen metrics when performing rTME in males with distal rectal cancer.




Similar content being viewed by others
References
Laurent C, Nobili S, Rullier A, Vendrely V, Saric J, Rullier E (2006) Efforts to improve local control in rectal cancer compromise survival by the potential morbidity of optimal mesorectal excision. J Am Coll Surg 203:684–691. https://doi.org/10.1016/j.jamcollsurg.2006.07.021
Birbeck KF, Macklin CP, Tiffin NJ, Parsons W, Dixon MF, Mapstone NP et al (2002) Rates of circumferential resection margin involvement vary between surgeons and predict outcomes in rectal cancer surgery. Ann Surg 235:449–457. https://doi.org/10.1097/00000658-200204000-00001
Ballian N, Yamane B, Leverson G, Harms B, Heise CP, Foley EF et al (2010) Body mass index does not affect postoperative morbidity and oncologic outcomes of total mesorectal excision for rectal adenocarcinoma. Ann Surg Oncol 17:1606–1613. https://doi.org/10.1245/s10434-010-0908-4
Son IT, Kim DW, Choe EK, Kim YH, Lee KH, Ahn S et al (2019) Oncologic evaluation of obesity as a factor in patients with rectal cancer undergoing laparoscopic surgery: a propensity-matched analysis using body mass index. Ann Surg Treat Res 96:86–94. https://doi.org/10.4174/astr.2019.96.2.86
Ballian N, Lubner MG, Munoz A, Harms BA, Heise CP, Foley EF et al (2012) Visceral obesity is associated with outcomes of total mesorectal excision for rectal adenocarcinoma. J Surg Oncol 105:365–370. https://doi.org/10.1002/jso.22031
Kang J, Baek SE, Kim T, Hur H, Min BS, Lim JS et al (2012) Impact of fat obesity on laparoscopic total mesorectal excision: more reliable indicator than body mass index. Int J Colorectal Dis 27:497–505. https://doi.org/10.1007/s00384-011-1333-2
Kartheuser AH, Leonard DF, Penninckx F, Paterson HM, Brandt D, Remue C et al (2013) Waist circumference and waist/hip ratio are better predictive risk factors for mortality and morbidity after colorectal surgery than body mass index and body surface area. Ann Surg 258:722–730. https://doi.org/10.1097/SLA.0b013e3182a6605a
Fleshman J, Branda M, Sargent DJ, Boller AM, George V, Abbas M et al (2015) Effect of laparoscopic-assisted resection vs open resection of stage II or III rectal cancer on pathologic outcomes: the ACOSOG Z6051 randomized clinical trial. JAMA 314:1346–1355. https://doi.org/10.1001/jama.2015.10529
Tou S, Bergamaschi R (2016) Laparoscopic rectal cancer resection: inferior to open or not? Colorectal Dis 18:233. https://doi.org/10.1111/codi.13270
Zhou CJ, Cheng YF, Xie LZ, Hu WL, Chen B, Xu L et al (2020) Metabolic syndrome, as defined based on parameters including visceral fat area, predicts complications after surgery for rectal cancer. Obes Surg 30:319–326. https://doi.org/10.1007/s11695-019-04163-1
Yu H, Joh YG, Son GM, Kim HS, Jo HJ, Kim HY (2016) Distribution and impact of the visceral fat area in patients with colorectal cancer. Ann Coloproctol 32:20–26. https://doi.org/10.3393/ac.2016.32.1.20
Heus C, Bakker N, Verduin WM, Doodeman HJ, Houdijk APJ (2019) Impact of body composition on surgical outcome in rectal cancer patients, a retrospective cohort study. World J Surg 43:1370–1376. https://doi.org/10.1007/s00268-019-04925-z
Clark W, Siegel EM, Chen YA, Zhao X, Parsons CM, Hernandez JM et al (2013) Quantitative measures of visceral adiposity and body mass index in predicting rectal cancer outcomes after neoadjuvant chemoradiation. J Am Coll Surg 216:1070–1081. https://doi.org/10.1016/j.jamcollsurg.2013.01.007
Bocca G, Mastoridis S, Yeung T, James DRC, Cunningham C (2022) Visceral-to-subcutaneous fat ratio exhibits strongest association with early post-operative outcomes in patients undergoing surgery for advanced rectal cancer. Int J Colorectal Dis 37:1893–1900. https://doi.org/10.1007/s00384-022-04221-8
Baastrup NN, Christensen JK, Jensen KK, Jorgensen LN (2020) Visceral obesity and short-term outcomes after laparoscopic rectal cancer resection. Surg Endosc 34:177–185. https://doi.org/10.1007/s00464-019-06748-4
Shiomi A, Kinugasa Y, Yamaguchi T, Kagawa H, Yamakawa Y (2016) Robot-assisted versus laparoscopic surgery for lower rectal cancer: the impact of visceral obesity on surgical outcomes. Int J Colorectal Dis 31:1701–1710. https://doi.org/10.1007/s00384-016-2653-z
Chen B, Zhang Y, Zhao S, Yang T, Wu Q, Jin C et al (2016) The impact of general/visceral obesity on completion of mesorectum and perioperative outcomes of laparoscopic TME for rectal cancer: A STARD-compliant article. Medicine (Baltimore) 95:e4462. https://doi.org/10.1097/MD.0000000000004462
Levic K, Bulut O, Schodt M, Bisgaard T (2017) Increased perirenal fat area is not associated with adverse outcomes after laparoscopic total mesorectal excision for rectal cancer. Langenbecks Arch Surg 402:1205–1211. https://doi.org/10.1007/s00423-017-1636-z
Gachabayov M, Kim SH, Jimenez-Rodriguez R, Kuo LJ, Cianchi F, Tulina I et al (2020) Impact of robotic learning curve on histopathology in rectal cancer: A pooled analysis. Surg Oncol 34:121–125. https://doi.org/10.1016/j.suronc.2020.04.011
Acknowledgments
** RESURRECT study group:
1) Seon-Hahn Kim, Colorectal Division, Department of Surgery, Korea University Anam Hospital, Korea University College of Medicine, Seoul, South Korea
2) Guglielmo Niccolo Piozzi, Colorectal Division, Department of Surgery, Korea University Anam Hospital, Korea University College of Medicine, Seoul, South Korea
3) Rosa Jimenez-Rodriguez, Section of Colorectal Surgery, Hospital Universitario Virgen del Rocio, Sevilla, Spain
4) Li-Jen Kuo, Division of Colorectal Surgery, Department of Surgery, Taipei Medical University Hospital, Taipei, Taiwan
5) Tomohiro Yamaguchi, Division of Colon and Rectal Surgery, Shizuoka Cancer Center Hospital, Shizuoka, Japan
6) Fabio Cianchi, Department of Surgery and Translational Medicine, Careggi Hospital, University of Florence, Florence, Italy
7) Oktar Asoglu, Bosphorus Clinical Research Academy, Istanbul, Turkey
8) Vusal Aliyev, Department of General Surgery, Istanbul Florence Nightingale Hospital, Istanbul, Turkey
9) Dejan Ignjatovic, Surgical Department, Akershus University Hospital, Lørenskog, Norway
10) Yosef Nasseri, Cedar Sinai Medical Center, Los Angeles, CA, USA
11) Moshe Barnajian, Cedar Sinai Medical Center, Los Angeles, CA, USA
12) Dorin E. Popa, Linköping University Hospital, Linköping, Sweden
Funding
None.
Author information
Authors and Affiliations
Consortia
Contributions
Study conception and design: MG, RB. Acquisition of data: RB, RESURRECT Study Group. Analysis and interpretation of data: MG, DMF, SU, RB. Drafting of the manuscript: MG, DMF, SU, RB. Critical revision of manuscript: MG, DMF, SU, RB, RESURRECT Study Group.
Corresponding author
Ethics declarations
Conflict of interest
Authors have no conflicts of interests
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gachabayov, M., Felsenreich, D., Bhatti, S. et al. Does the visceral fat area impact the histopathology specimen metrics after total mesorectal excision for distal rectal cancer?. Langenbecks Arch Surg 408, 257 (2023). https://doi.org/10.1007/s00423-023-02981-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-023-02981-7