Abstract
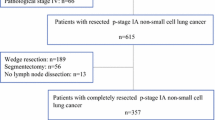
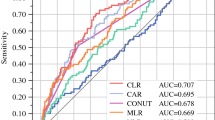
Tumor markers are indicators that can be used not only for cancer diagnosis but also for determining prognosis. Unfortunately, there is currently no tumor marker that reliably predicts the prognosis of lung cancer. In this study, we investigated the prognostic impact of the platelet-to-lymphocyte ratio (PLR) and Glasgow Prognostic Score (GPS), known as inflammation markers in peripheral blood, in patients who underwent resection for early-stage non-small cell lung cancer (NSCLC). We retrospectively analyzed the medical records of a total of 3300 patients who underwent surgery for NSCLC between 2010 and 2020. Among these patients, 250 met the inclusion criteria of lobectomy, pT1-T2N0 stage, and histology of adenocarcinoma or squamous cell carcinoma. Preoperative albumin, C-reactive protein (CRP), preoperative PLR, and postoperative 5th-day PLR values were determined from patient’s peripheral blood data. The impact of these values on postoperative recurrence and survival was investigated. GPS was calculated based on preoperative CRP and albumin values, and patients were divided into 3 groups: 0 (mild), 1 (moderate), and 2 (severe). The relationship between preoperative GPS and survival was analysed. Among the included patients, 155 (62%) had adenocarcinoma and 95 (38%) had squamous cell carcinoma. A total of 185 (74%) patients had pT1 tumors, while 65 (26%) had pT2 tumors. During the postoperative follow-up period, local recurrence was observed in 28 (11.2%) patients and distant metastasis in 51 (20.4%) patients. The overall mortality rate was 19.6%. The 5-year survival rates for pT1 and pT2 tumors were 80.4% and 72.5%, respectively. Significant associations were found between preoperative PLR, postoperative PLR, and recurrence (p = 0.005 and p = 0.011). The expected overall survival (OS) was 103.4 months in the mild GPS group, 91.8 months in the moderate GPS group, and 50 months in the severe GPS group. The relationship between GPS groups and OS was statistically significant (p = 0.005). Preoperative analysis of PLR and GPS may provide prognostic value in NSCLC patients who undergo surgical resection. Our study provides a rationale for further investigation of peripheral blood immune markers for prognostic purposes.

Similar content being viewed by others
Availability of data and materials
All data generated or analysed during this study are included in this published article [and its supplementary information files].
References
Greenberg PD, Mechanism of tumor immunology. In: Parslow TG, Stites DP, Terr Al, Imboden JB, editors. Medical Immunology. 10 th ed. New York: McGraw Hill, 2001. p.568-577
Coussens LM, Werb Z (2002) Inflammation, and cancer. Nature 420:860–867
Nikiteas NI, Tzanakis N, Gazouli M, Rallis G, Daniilidis K, ve ark Theodoropoulos G (2005) Serum IL-6, TNFalpha and CRP levels in Greek colorectal cancer patients: prognostic implications. World J Gastroenterol 11:1639–1643
Gockel I, Direksen K, Messow CM, Junginger T (2006) Significance of preoperative C-reactive protein as a parameter of the perioperative course and long-term prognosis in squamous cell carcinoma and adenocarcinoma of the oesophagus. World J Gastroenterol 12:3746–3750
Shiels MS, Pfeiffer RM, Hildesheim A, Engels EA, ve ark Kemp TJ, Park JH (2013) Circulating inflammation markers and prospective risk for lung cancer. J Natl Cancer Inst 105:1871–1880
Grivennikov SI, Greten FR, Karin M (2010) Immunity, inflammation, and cancer. Cell 19(140):883–899
Nøst TH et al (2021) Systemic inflammation markers and cancer incidence in the UK Biobank. Eur J Epidemiol 36(8):841–848
Osugi J et al (2016) Prognostic impact of the high sensitivity modified Glasgow prognostic score in patients with resectable non-small cell lung cancer. J Cancer Rese Ther 12(2):945–951
Wang E et al (2021) Prognostic significance of platelet lymphocyte ratio in patients with melanoma: a meta-analysis. Medicine 100(38):e27223
Chandrasekaran D et al (2022) Preoperative neutrophil–lymphocyte ratio/platelet–lymphocyte ratio: a potential and economical marker for renal cell carcinoma. J Cancer Res Ther 18(6):1635–1639
Eberst G et al (2022) Prognostic value of CD4+ T lymphopenia in non-small cell lung cancer. BMC Cancer 22(1):529
Venkatesulu BP et al (2022) A systematic review and meta-analysis of the impact of radiation-related lymphopenia on outcomes in pancreatic cancer. Future Oncol 18(15):1885–1895
Paul M, Pamela SO (2020) The roles of CD8+ T cell subsets in antitumor immunity. Trends Cell Biol 30(9):695–704
Zikos TA, Donnenberg AD, Landreneau RJ, Luketich JD (2011) Donnenberg VS Lung T-cell subset composition at the time of surgical resection is a prognostic indicator in non-small cell lung cancer. Cancer Immunol Immunother 60:819–827
Park J et al (2023) Microenvironment-driven metabolic adaptations guiding CD8+ T cell anti-tumor immunity. Immunity 56(1):32–42
Han J et al (2022) Role of CD4+ T, CD8+ T cells, and CD4+ T/CD8+ T cell ratio in gastric cancer and its clinical significance. Appl Bionics Biomech. https://doi.org/10.1155/2022/1094607
Garcia P et al (2023) CD8+ T-cell density ıs an ındependent predictor of survival and response to adjuvant chemotherapy in stage III colon cancer. Appl Immunohistochem Mol Morphol 31(2):69–76
Gao Y et al (2017) Prognostic value of programmed death-1, programmed death-ligand 1, programmed death-ligand 2 expression, and CD8 (+) T cell density in primary tumors and metastatic lymph nodes from patients with stage T1–4N+ M0 gastric adenocarcinoma. Cancer Commun 36(1):1–14
Platini H et al (2022) Neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio as prognostic markers for advanced non-small-cell lung cancer treated with immunotherapy: a systematic review and meta-analysis. Medicina 58(8):1069
Cheng H et al (2022) Preoperative neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio are correlated with tumor–node–metastasis stages in patients with non-small cell lung cancer. J Cancer Res Ther 18(6):1666–1673
Jensen LS, Andersen AJ, Christiansen PM, Hokland P, Juhl CO, Madsen G, Mortensen J, Møller-Nielsen C, Hanberg-Sørensen HM (1992) Postoperative infection and natural killer cell function following blood transfusion in patients undergoing elective colorectal surgery. Br J Surg 79:513–516
Houbiers JGA, Brand A, van de Watering LMG, Hermans J, Verwey PJM, Bijnen AB, Pahlplatz P, Eeftinck Schattenkerk M, Wobbes TH, de Vries JE, Klementschitsch P, van de Maas AHM, van de Velde CJH (1994) Randomised controlled trial comparing transfusion of leukocyte-depleted or buffy-coat-depleted blood in surgery for colorectal cancer. Lancet 344:573–578
Pêgo-Fernandes PM et al (2021) The role of the surgeon in treating patients with lung cancer. An updating article. Sao Paulo Med J 139:293–300
Hoy H, Lynch T, Beck M (2019) Surgical treatment of lung cancer. Critical Care Nursing Clin 31(3):303–313
Mun M et al (2018) Video-assisted thoracoscopic surgery lobectomy for non-small cell lung cancer. General Thorac Cardiovasc Surg 66:626–631
Mandaliya H et al (2019) Prognostic biomarkers in stage IV non-small cell lung cancer (NSCLC): neutrophil to lymphocyte ratio (NLR), lymphocyte to monocyte ratio (LMR), platelet to lymphocyte ratio (PLR) and advanced lung cancer inflammation index (ALI). Transl Lung Cancer Res 8(6):886
Liu J et al (2019) Systemic immune-inflammation index, neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio can predict clinical outcomes in patients with metastatic non-small-cell lung cancer treated with nivolumab. J Clin Lab Anal 33(8):e22964
Drpa G et al (2020) Neutrophil-to-lymphocyte ratio can predict outcome in extensive-stage small cell lung cancer. Radiol Oncol 54(4):437–446
Ma A et al (2022) The clinical relevance of neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in chronic obstructive pulmonary disease with lung cancer. Front Oncol 12:902955
Kang J et al (2019) Neutrophil-to-lymphocyte ratio and risk of lung cancer mortality in a low-risk population: a cohort study. Int J Cancer 145(12):3267–3275
Evkan Öztürk A et al (2021) İleri evre akciğer kanserinde; Yaygın Kanser İnflamasyon İndeksi (ALI), serum nötrofil/lenfosit oranı (NLR), trombosit/lenfosit oranının (PLR) prognostik değeri. İzmir Göğüs Hastanesi Dergisi 35(3):134–139
Dirican N et al (2016) Hematolojik parametrelerin küçük hücreli akciğer kanserli hastalarda prognoz üzerine etkileri. Cukurova Med J 41(2):333–341
Lohinai Z et al (2019) Neutrophil–lymphocyte ratio is prognostic in early stage resected small-cell lung cancer. PeerJ 7:e7232
Wang J., Huawei L., Xu R. et al. The MLR, NLR, PLR and D-dimer are associated with clinical outcome in lung cancer patients treated with surgery. BMC Pulm Med. 2022. 22(1):104. 1–7
Duran AO et al (2017) Evre 1–2 opere küçük hücreli dışı akciğer kanseri hastalarında nötrofil/lenfosit ve platelet/lenfosit oranlarının prognoz ile ilişkisi: tek merkez deneyimi. Anadolu Kliniği Tıp Bilimleri Dergisi 22(3):149–156
Zhang Y, Chen S, Chen H et al (2023) A comprehensive analysis glasgow prognostic score (GPS)/ the modified Glasgow Prognostic Score (mGPS) on immüne checkpoint inhibitor efficacy among patients with advenced cancer. Cancer Med 12:38–48
Bilgin B et al (2019) Albümin globulin oraninin küçük hücreli akciğer kanserinde prognostik önemi. Ankara Med J 19(4):729–735
Kumbasar U (2018) Prognostic significance of the Glasgow prognostic score in patients undergoing pulmonary metastasectomy.". Uhod-Uluslararası Hematolojı-Onkolojı Dergısı. https://doi.org/10.4999/uhod.182921
Funding
There is no specific funding related to this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics committee of our hospital (2022/57-65) approved the protocol for the current study. All patients gave written informed consent for surgical treatment and were aware that all information could be used anonymously for scientific purposes only.
Conflict of interest
The authors declare that they have no competing interests.
Informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. Informed consent was obtained from all participants.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Agaoglu Sanli, B., Gulmez, B., Yazgan, S. et al. The effect of platelet-to-lymphocyte ratıo (PLR) and glasgow prognostıc score (GPS) on recurrence, and survıval ın patıents undergoıng lobectomy for early-stage non-small cell lung cancer (NSCLC). Updates Surg 76, 631–639 (2024). https://doi.org/10.1007/s13304-023-01669-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-023-01669-3