Abstract
Background
Many inflammatory and nutritional markers have been used to predict prognosis in lung cancer. The C-reactive protein (CRP)-to-lymphocyte ratio (CLR) is a useful prognostic factor in various cancers. However, the prognostic value of preoperative CLR in patients with non-small cell lung cancer (NSCLC) remains to be established. We examined the significance of the CLR compared with known markers.
Methods
A total of 1380 surgically resected NSCLC patients treated at two centers were recruited and divided into derivation and validation cohorts. After CLRs were calculated, patients were classified into high and low CLR groups based on the cutoff value determined by receiver operating characteristics curve analysis. Subsequently, we determined the statistical associations of the CLR with clinicopathological factors and prognosis and further analyzed its prognostic impact by propensity-score matching.
Results
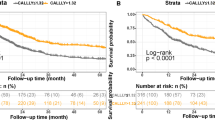
Of all the inflammatory markers examined, CLR yielded the highest area-under-the-curve value. The prognostic impact of CLR remained significant after propensity-score matching. Prognosis was significantly worse in the high-CLR group than in the low-CLR group (5-year, disease-free survival [DFS]: 58.1% vs. 81.9%, P < 0.001; 5-year overall survival [OS]: 72.1% vs. 91.2%, P < 0.001). The results were confirmed in the validation cohorts. Multivariable analysis also showed high CLR as an independent factor for both DFS and OS (DFS: hazard ratio [HR] 1.42, P = 0.027; OS: HR 1.95, P = 0.0037).
Conclusions
Preoperative CLR is a useful marker for predicting the prognosis of NSCLC patients who have undergone surgery.



Similar content being viewed by others
References
Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424.
Ruiz-Cordero R, Devine WP. Targeted therapy and checkpoint immunotherapy in lung cancer. Surg Pathol Clin. 2020;13:17–33.
Murata M. Inflammation and cancer. Environ Health Prevent Med. 2018;23:1–8.
Mandaliya H, Jones M, Oldmeadow C, et al. Prognostic biomarkers in stage IV non-small cell lung cancer (NSCLC): neutrophil to lymphocyte ratio (NLR), lymphocyte to monocyte ratio (LMR), platelet to lymphocyte ratio (PLR) and advanced lung cancer inflammation index (ALI). Trans Lung Cancer Res. 2019;8:886–94.
Ni XF, Wu J, Ji M, et al. Effect of C-reactive protein/albumin ratio on prognosis in advanced non–small-cell lung cancer. Asia-Pacific J Clin Oncol. 2018;14:402–9.
Yılmaz A, Tekin SB, Bilici M, et al. The significance of controlling nutritional status (CONUT) score as a novel prognostic parameter in small cell lung cancer. Lung. 2020;198:695–704.
Fan Z, Luo G, Gong Y, et al. Prognostic value of the c-reactive protein/lymphocyte ratio in pancreatic cancer. Ann Surg Oncol. 2020;27:4017–25. https://doi.org/10.1245/s10434-020-08301-3.
Ou W, Zhou C, Zhu X, et al. Prognostic significance of preoperative lymphocyte-to-C-reactive protein ratio in patients with nonmetastatic colorectal cancer. Oncol Targets Ther. 2021;14:337–46.
Iseda N, Itoh S, Yoshizumi T, et al. Lymphocyte-to-C-reactive protein ratio as a prognostic factor for hepatocellular carcinoma. Int J Clin Oncol. 2021;26:1890–900.
Goldstraw P, Crowley J, Chansky K, et al. The IASLC lung cancer staging project: proposals for the revision of the TNM stage groupings in the forthcoming (seventh) edition of the TNM classification of malignant tumours. J Thorac Oncol. 2007;2:706–14.
Travis WD, Brambilla E, Noguchi M, et al. International association for the study of lung cancer/american thoracic society/european respiratory society international multidisciplinary classification of lung adenocarcinoma. J Thorac Oncol. 2011;6(2):244–85.
Strzelak A, Ratajczak A, Adamiec A, et al. Tobacco smoke induces and alters immune responses in the lung triggering inflammation, allergy, asthma and other lung diseases: a mechanistic review. Int J Environ Res Public Health. 2018. https://doi.org/10.3390/ijerph15051033.
Shaw AC, Goldstein DR, Montgomery RR. Age-dependent dysregulation of innate immunity. Nat Rev Immunol. 2013;13:875–87.
Galdiero MR, Marone G, Mantovani A. Cancer inflammation and cytokines. Cold Spring Harbor Perspect Biol. 2018. https://doi.org/10.1101/cshperspect.a028662.
Alfaro C, Sanmamed MF, Rodríguez-Ruiz ME, et al. Interleukin-8 in cancer pathogenesis, treatment and follow-up. Cancer Treat Rev. 2017;60:24–31.
Slaats J, ten Oever J, van de Veerdonk FL, et al. IL-1β/IL-6/CRP and IL-18/ferritin: distinct inflammatory programs in infections. PLoS Path. 2016;12:1–13.
Nishimura S, Manabe I, Nagasaki M, et al. CD8+ effector T cells contribute to macrophage recruitment and adipose tissue inflammation in obesity. Nat Med. 2009;15:914–20.
Lu Y, Jiang J, Ren C. The clinicopathological and prognostic value of the pretreatment neutrophil-to-lymphocyte ratio in small cell lung cancer: a meta-analysis. PLoS ONE. 2020;15(4):e0230979.
Mandaliya H, Jones M, et al. Prognostic biomarkers in stage IV non-small cell lung cancer (NSCLC): neutrophil to lymphocyte ratio (NLR), lymphocyte to monocyte ratio (LMR), platelet to lymphocyte ratio (PLR) and advanced lung cancer inflammation index (ALI). Trans Lung Cancer Res. 2019;8(6):886–94.
Acknowledgment
The authors thank Sarah Ivins, PhD, and H. Nikki March, PhD, from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
10434_2023_13250_MOESM2_ESM.tiff
Supplemental Figure 1. Patient flowchart. KUH, Kyushu University Hospital; KCC, National Hospital Organization Kyushu Cancer Center; NSCLC, non-small cell lung cancer; pStage, pathological stage (TIFF 858 KB)
10434_2023_13250_MOESM3_ESM.tiff
Supplemental Figure 2. Kaplan–Meier curves showing survival of the internal cohort. (A) Disease-free survival and (B) overall survival of high and low CLR groups (TIFF 858 KB)
10434_2023_13250_MOESM4_ESM.tiff
Supplemental Figure 3. Kaplan–Meier curves showing survival of the external cohort. (A) Disease-free survival and (B) overall survival of high and low CLR groups (TIFF 858 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nagano, T., Kinoshita, F., Hashinokuchi, A. et al. Prognostic Impact of C-Reactive Protein-to-Lymphocyte Ratio in Non-small Cell Lung Cancer: A Propensity Score-Matching Analysis. Ann Surg Oncol 30, 3781–3788 (2023). https://doi.org/10.1245/s10434-023-13250-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-023-13250-8