Abstract
Since 2010, several guidelines and consensus papers have been proposed to support surgeons in the decision-making process (Cuccurullo et al. in Hernia 17(5):557–566, 2013; Silecchia et al. in Surg Endosc 29:2463–2484, 2015; Bittner et al. in Surg Endosc 33(11):3511–3549, 2015) with the conclusion that laparoscopic repair (LR) has gained popularity in the treatment of IH.
To date, however, it is not yet clear as to the uptake of LR for IH on national basis. Only dated studies encompassing of all types of incisional hernia repairs are available in literature (Bisgaard et al. in Br J Surg 96:1452–1457, 2009). The aim of our study is to present a snapshot of Italian data for LR of ventral hernias, over a 6 years period, including volume of LR, procedural features and major postoperative outcomes. Data were extracted from the Italian Hospital Information System (HIS) that collects clinical and administrative information regarding each hospital admission of every patient discharged from any hospital in Italy. Using Hospital Discharge records regional Databases (HDD), all laparoscopic ventral hernia procedures carried out in public and private hospitals between 2015 and 2020, in patients over 18 years and resident in Italy, were collected based on diagnosis and procedure codes. The National Agency for Regional Health Services (AgeNaS) oversees the management and analysis of data. All hospital admissions that occurred between 2015 and 2020 were analyzed.
A total of 154,546 incisional hernia repairs were performed in Italy from 2015 to 2020. Of these, 20,789 (13.45%) were minimally invasive repairs. The number of procedures performed increased significantly over time, constituting 11.96 and 15.24% of all procedures performed in 2015 and 2020 respectively. However, considering the whole period, the mean annual change was—5.58% (CI − 28.6% to 17.44%; p < 0.0001).
Urgent minimally invasive repairs were performed in 1968 cases (1.27%). The absolute rate of laparoscopically treated patients needing an urgent surgical procedure increased overtime (from 7.36% in 2015 to 13.418% in 2020). The mean annual change registered over the whole period was 7.42%. 92% (CI − 0.03 to 14.09%; p < 0.0001). However, when considering the period from 2015 to 2019, the mean annual change was 10.42% (CI 6.35 to 14.49%; p < 0.0001). To our knowledge this is the first nationwide Italian report presenting the national workload of surgical units and the main perioperative features of minimally invasive surgery for ventral hernia repairs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Following abdominal surgery, incisional hernias (IH) are associated with 20% of procedures, with a global lifetime risk of 5% [1]. The healthcare system costs for the treatment of ventral hernias are high and these costs are expected to continue to rise [2]. There are a number of approaches to incisional hernia repair, in addition to traditional open methods, including, several endoscopic, laparoscopic and hybrid procedures.
Since 2010, several guidelines and consensus papers have been proposed to support surgeons in the decision-making process [3,4,5] with the conclusion that laparoscopic repair (LR) has gained popularity in the treatment of IH.
To date, however, it is not yet clear as to the uptake of LR for IH on national basis. Only dated studies encompassing of all types of incisional hernia repairs are available in literature [6].
The aim of our study is to present a snapshot of Italian data for LR of ventral hernias, over a six years period, including volume of LR, procedural features and major postoperative outcomes.
Materials and methods
Data extraction
Data were extracted from the Italian Hospital Information System (HIS) that collects clinical and administrative information regarding each hospital admission of every patient discharged from any hospital in Italy. Using Hospital Discharge records regional Databases (HDD), all laparoscopic ventral hernia procedures carried out in public and private hospitals between 2015 and 2020, in patients over 18 years and resident in Italy, were collected based on diagnosis and procedure codes.
The National Agency for Regional Health Services (AgeNaS) oversees the management and analysis of data. All hospital admissions that occurred between 2015 and 2020 were analyzed. Subsequently, information on every admission with a diagnosis of incisional hernia as either primary or secondary [ICD-9-CM code 5512x, 5522x, 5532x,] were extracted. The presence of intestinal obstruction at the time of the operation was also registered [ICD-9-CM code 5518, 5528, 5529].
General data
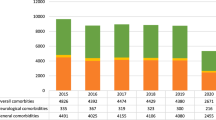
Gender, age and preexisting comorbidities were considered. As for the latter they were divided into general comorbidities [ICD-9-CM code atrial fibrillation (42,731), diabetes (2500×); anticoagulant therapy (2865 × and V5861) respiratory failure (49,120), renal failure (5859×) and obesity (278.0×).
Complication rate was also collected, either as primary diagnosis or among the first five secondary diagnosis [ICD-9-CM code bleeding (99,811), haematoma (99,812), serohematoma (99,813); infection (9960×–9965×), wound (998.59 e 9989×), bowel (99,687)] additionally, the presence of colostomy or ileostomy [ICD-9-CM V44.3 V44.2] was registered.
Procedural data
In this study, the discrimination between laparoscopic or open incisional hernia repair was defined as the presence or the absence of the ICD-9-CM code 54.21 as secondary diagnosis while robotic-assisted procedure was classified with the ICD-9-CM code 0039. The conversion to open surgery from minimally invasive surgery has a separate ICD-9-CM codification (6411). The association with other surgical procedures was also considered.
Based on HIS data and patient discharge records, the analysis included total hospital stay (primary plus readmission within 30 days), readmission rate, early mortality (within the first admission and < 30 days from the operation), late mortality (> 30-day mortality) and 30-day morbidity.
Statistical analysis
Data were processed using the MedCalc statistical package (version 12.5). Qualitative variables were summarized by frequency and percentage, while non-normally distributed quantitative variables were described by the median and standard deviation (SD).
Statistical analysis was performed using Student’s t test and the Cochran Armitage test for trend as appropriate. A two-tailed p value < 0.05 was considered statistically significant. The sample size was the Italian population, reported by region, according to the average yearly population for the period 2015–2020, reported by the Italian National Institute of Statistics (ISTAT) (Supplemental Table S1).
Results
A total of 154,546 incisional hernia repairs were performed in Italy from 2015 to 2020. Of these, 20,789 (13.45%) were minimally invasive repairs.
The number of procedures performed increased significantly over time, constituting 11.96 and 15.24% of all procedures performed in 2015 and 2020 respectively. However, considering the whole period, the mean annual change was − 5.58% (CI − 28.6 to 17.44%; p < 0.0001).
Specifically, a negative trend was observed between 2016 and 2017 (– 2.65%), and between 2019 and 2020 was − 51, 60%. However, if considering the period between 2015 and 2019 the mean annual change was 5.92% (CI − 0.03 to 11.87%; p < 0.0001) Fig. 1.
A significant increase was also registered in the number of ventral hernias performed robotically, with a mean annual change of 9.37% (CI − 10.22 to 28.96%; p < 0.0001) between 2015 and 2020 and of 36.71% (CI 28.15 to 45.27%; p < 0.0001) when considering only the first five years.
The gender ratio was about 44% for male patients for the entire period without significant fluctuation overtime and the mean age of treated patients ranged from 61 ± 13 in 2015 to 63 ± 13 in 2020.
Procedural data
Urgent minimally invasive repairs were performed in 1968 cases (1.27%). The absolute rate of laparoscopically treated patients needing an urgent surgical procedure increased overtime (from 7.36% in 2015 to 13.418% in 2020). The mean annual change registered over the whole period was 7.42% 0.92% (CI: − 0.03 to 14.09%; p < 0.0001). However, when considering the period from 2015 to 2019 the mean annual change was 10.42% (CI 6.35 to 14.49%; p < 0.0001) Fig. 2.
A total of 7714 (37.11%) incisional hernia repairs were associated with other surgical procedures during this period. The most performed concurrent procedure was minimally invasive adhesiolysis, here, a slight increase was observed from 2015 to 2020 (mean annual change = 6.75%; CI 5.1 to 8.34%; p = 0.445), while the mean annual change for the whole period was − 4.64% (CI − 27.55 to 18.27%; p = 0.542) (Fig. 3).
Type of admission and hospital stay
The number of patients treated as elective admissions ranged from 2640 in 2020 to 3991 in 2019 as absolute numbers and from 95.21% to 97.43% as relative values to overall procedures in 2019 and 2017 respectively. The mean annual change was -5.81 (CI − 28.37 to 16.75%; p < 0.0001), however, a positive mean annual change was observed if considering only the first five years (mean annual change = 5.53%; CI 10.51 to 0.55%; p = 0.003).
The number of procedures managed as day case procedures ranged from 80 in 2020 to 199 in 2019 as absolute numbers and from 2.38 to 4.75% as rates of overall procedures in 2017 and 2019 respectively. Overall, the mean annual change was − 5.27 (CI − 46.69 to 39.15%; p < 0.0001), however, a positive mean annual change was observed if considering only the first five years (8.22%; CI − 37.87 to 54.31%; p = 0.003).
Mean hospital stay was 5 days in 2015, 2018 and 2020. In 2016, 2017, 2019 it was 4 days.
Conversion, complications and readmission
Overall, a total of 271 (1.3%) conversions, 193 (0.93%) complications and 58 (0.28%) readmissions within 30 days were registered. Conversion rate significantly increased over the considered period with a mean annual change of 10.10% (CI − 4.64 to 24.84%; p < 0.0001) from 2015 to 2020 and of 13.12% 5.27 (CI − 4.31 to 30.55%; p = 0.0322). Complications ranged from 26 in 2016 to 40 in 2017 as absolute numbers and from 0.87 to 1.19% as rate of overall procedures in 2017 and 2019 respectively (mean annual change = − 3.5%; CI − 25.92 to 18.92%; p = 0.911). Readmissions ranged from 6 in 2020 to 15 in 2019, (mean annual change = − 20.44%; CI −93.84 to 52.96%; p = 0.487 from 2015 to 2020; mean annual change = 11.95%; CI − 35.62 to 59.52%; p = 0.184 from 2015 to 2019) Fig. 4.
Mortality rate
A total of 60 (0.28%) deaths were registered (mean annual change = 1.07%; CI − 37.64 to 39.78%; p = 0.142 from 2015 to 2020; mean annual change = − 7.58%; CI − 52.5 to 37.34; p = 0.887 from 2015 to 2019).
Thirty-two (53.33%) deaths occurred within 30 days from the operations and 28 after 30 days (46.67%). The mean annual change for early mortality was − 38.94% and − 40.34% with and without considering 2020 respectively (CI − 115.73 to 37.85%; p = 0.655 and CI − 139.42 to 58.78%; p = 0.943, respectively). The mean annual change for late mortality was -5.09% and -20% with and without considering 2020 respectively (CI − 87.13 to 76.95%; p = 0.008 and CI − 64.92 to 24.92%; p = 0.744, respectively).
Regional data
The number of elective procedures performed laparoscopically steadily increased across Italy, however, in six regions, the difference was not significant considering both the whole period and the first five years without analyzing 2020 data (Valle d’Aosta, Trentino, Friuli Venezia Giulia, Toscana, Umbria Abruzzo Molise and Campania). The minimum annual intervention rate was observed in Calabria (AIR = 1) while the maximum was registered in Valle d’Aosta (19 in 2018). Table 1
Considering urgent procedures, an increase in the adoption of laparoscopy was observed, however, in 9 regions, this increase was not significant considering both the whole period and the first five years excluding the 2020 data (Valle d’Aosta, Trentino, Veneto, Liguria, Umbria, Abruzzo, Molise, Basilicata, Calabria). Many regions showed the same annual intervention rate (AIR = 0) while the maximum was registered in Trentino [3]. Table 2 summarizes the distribution of urgent procedures in the index period.
Discussion
The indications and limitations for laparoscopic ventral hernia repair are well established by different guidelines [3,4,5], some of which were published before 2015.
In Italy, between 2015 and 2019 more than 26,000 patients underwent surgery for ventral hernia repair. The number of laparoscopic ventral hernia procedures in this period reached over 3000 patients annually, with a significant increase in its adoption from 2015 to 2019 (Table 3).
However, even if this positive trend is confirmed in the future, thanks to the dissemination of several interesting new techniques [5] the indications for minimally invasive ventral hernia repair are likely to expand; indeed, in 2019 and 2020 the laparoscopic approach stood at 15% of the total number of ventral repairs (Table 4).
As COVID-19 spread in 2020, Italy, along with the rest of the world, faced an unexpected new healthcare emergency which significantly affected surgical activity. [7].
Elective surgery was particularly affected by the pandemic, with numbers of elective procedures for benign conditions, dramatically reduced [8].
In 2020, the number of ventral repairs, both open and minimally invasive, almost halved if compared to 2019. Naturally, this trend affected observations that could be made regarding the adoption of minimally invasive repair in Italy over the index period, therefore, we opted to split the statistical analysis, by considering the whole period as well as omitting the 2020 data.
Nevertheless, an interesting observation is that, despite the dramatic drop in the number of performed procedures in 2020, [9, 10] the rate of minimally invasive procedures across the total number of procedures performed remained unchanged from 2019 to 2020, with minimally invasive procedures accounted for almost 15% of all ventral hernia repairs performed in these two years.
The impact of Sars-Cov-2 on elective surgical activity is more evident when analyzing data related to urgent procedures: the decrease in absolute numbers observed in 2020 was also noted in the number of urgent ventral hernia repairs, however, urgent procedures in 2020 represented the 13.14% of the whole number of ventral hernia repairs performed in 2020, in contrast to 2019 when urgent procedures represented the 9.26% of the total procedures.
In the literature, urgent repair is not a contraindication to laparoscopy, however, laparoscopy is generally contraindicated in the presence of diffuse peritonitis or marked bowel distension [11,12,13,14,15] in addition to the general advise against the use of pneumoperitoneum in cases of hemodynamic instability or severe lung and heart disease [15, 16]. Our study confirms that laparoscopic ventral hernia repair is safe, with a complication rate of 0.93% and a percentage of readmission within 30 days of 0.4%. There is sufficient data presented in literature based on several meta-analyses and randomized controlled trials to support laparoscopic mesh repair for IH as a low risk procedure [17,18,19,20]. Most laparoscopic IH repairs require an elective admission with a mean hospital stay of 4–5 days. Type of hospital admission and length of stay are strongly influenced by mesh size, patient age and comorbidities. Complex defects and incarcerated hernias are also predictive factors associated with longer hospitalization [21].
Regional data showed a high variability among the Italian regions in the adoption of the laparoscopic approach when dealing with incisional hernias. This might be explained by the fact that the adoption of the laparoscopic approach is mostly based on the performing surgeons’ preferences and training and on the actual resources of the hospitals. In our opinion, this observation may highlight the urgency for standardization for this procedure and its indications as well as for the publication of proper guidelines.
Conclusions
To our knowledge, this is the first nationwide Italian report presenting the national workload of surgical units and the main perioperative features of minimally invasive surgery for ventral hernia repairs.
The definition of ventral hernia encompasses several hernia types, differing in size of the fascial defect and number and complexity of the previous surgical procedures. The coding system is not able to discriminate accurately the nature of all ventral hernias, therefore, the results of the present work, particularly where open repair is compared, could be influenced by bias. Still, there was a steady increase in the adoption of the laparoscopic approach in both emergent and elective settings in the index period. The high variability observed among the Italian regions.
Data availability
Data will be available if requested.
References
Bikhchandani J, Fitzgibbons RJ Jr (2013) Repair of giant ventral hernias. Adv Surg 47:1–27
Bower C, Roth JS (2013) Economics of abdominal wall reconstruction. Surg Clin North Am 93:1241–1253
Cuccurullo D, Piccoli M, Agresta F, Magnone S, Corcione F, Stancanelli V, Melotti G (2013) Laparoscopic ventral incisional hernia repair: evidence-based guidelines of the first Italian consensus conference. Hernia 17(5):557–566
Silecchia G, Campanile FC, Sanchez L (2015) Laparoscopic ventral/incisional hernia repair: updated guidelines from the EAES and EHS endorsed consensus development conference. Surg Endosc 29:2463–2484
Bittner R, Bain K, Bansal VK (2019) Update of guidelines for laparoscopic treatment of ventral and incisionale hernia abdominal wall hernias (International endohernia society (IEHS)): part B. Surg Endosc 33(11):3511–3549
Bisgaard T, Kehlet H, Bay-Nielsen MB (2009) Nationwide study of early outcomes after incisional hernia repair. Br J Surg 96:1452–1457
Bracale U, Podda M, Castiglioni S, Peltrini R, Sartori A, Arezzo A, Corcione F, Agresta F, CLOUD-19 Collaborative Group (2021) Changes in surgical behaviors during the Covid-19 pandemic. The SICE CLOUD19 Study. Updates Surg 73(2):731–744
COVIDSurg Collaborative (2020) Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg 107(11):1440–1449
Arezzo A, Francis N, Mintz Y, Adamina M, Antoniou SA, Bouvy N, Copaescu C, de Manzini N, Di Lorenzo N, Morales-Conde S, Müller-Stich BP, Nickel F, Popa D, Tait D, Thomas C, Nimmo S, Paraskevis D, Pietrabissa A, EAES Group of Experts for Recovery Amid COVID-19 Pandemic (2021) EAES recommendations for recovery plan in minimally invasive surgery amid COVID-19 pandemic. Surg Endosc 35(1):1–17
Botteri E, Podda M, Sartori A (2020) The COVID-19 pandemic should not take us back to the prelaparoscopic era. J Trauma Acute Care Surg 89(2):273–274
Grafen FC, Neuhaus V, Schob O, Turina M (2010) Management of acute small bowel obstruction from intestinal adhesions: indications for laparoscopic surgery in a community teaching hospital. Langenbecks Arch Surg 395(1):57–63
Landau O, Kyzer S (2004) Emergent laparoscopic repair of incarcerated incisional and ventral hernia. Surg Endosc 18:1374–1376
Franklin ME, Gonzalez JJ, Miter DB, Glass JL, Paulson D (2004) Laparoscopic diagnosis and treatment of intestinal obstruction. Surg Endosc 18:26–30
Szomstein S, Lo Menzo E, Simpfendorfer C, Zundel N, Rosenthal R (2006) Laparoscopic lysis of adhesions. World J Surg 30:535–540
Olmi S, Cesana G, Eba L, Croce E (2009) Emergency laparoscopic treatment of acute incarcerated incisional hernia. Hernia 3:605–608
Bessa SS, Abdel-Razek AH (2013) Results of prosthetic mesh repair in the emergency management of the acutely incarcerated and/or strangulated ventral hernias: a seven years study. Hernia 17(1):59–65
Sauerland S, Walgenbach M, Habermalz B, Seiler CM, Miserez M (2011) Laparoscopic versus open surgical techniques for ventral or incisional hernia repair. Cochrane Database Syst Rev 16(3):CD007781
Eker HH, Hansson BM, Buunen M, Janssen IM, Pierik RE, Hop WC, Bonjer HJ, Jeekel J, Lange JF (2013) Laparoscopic vs. open incisional hernia repair: a randomized clinical trial. JAMA Surg 148:259–263
Forbes SS, Eskicioglu C, McLeod RS, Okrainec A (2009) Metaanalysis of randomized controlled trials comparing open and laparoscopic ventral and incisional hernia repair with mesh. Br J Surg 96:851–858
Moreau PE, Helmy N, Vons C (2012) Laparoscopic treatment of incisional hernia. State of the art in 2012. J Vasc Surg 149(5 Suppl):e40–e48
Kurian A, Gallagher S, Cheeyandira A, Josloff R (2010) Predictors of in-hospital length of stay after laparoscopic ventral hernia repair: results of multivariate logistic regression analysis. Surg Endosc 24:2789–2792
Acknowledgements
Authors would like to thank AgeNas (Agenzia nazionale per i servizi sanitari regionali) for supporting consultation and analysis of databases.
Funding
Open access funding provided by Università Politecnica delle Marche within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
AS, AB and MO conceived the study; AS, AB, MO, EB and FS designed and performed the research; MO analyzed the data; AS, AB, MO, EB, SW wrote the paper; MG, and SMC supervised the paper; all authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interests to disclose.
Research involving human participants
Data were collected anonymously from a national public database, no consent was needed for this study.
Informed consent
For this type of study formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Botteri, E., Ortenzi, M., Williams, S. et al. Nationwide analysis of inpatient laparoscopic ventral hernia repair in Italy from 2015 to 2020. Updates Surg 75, 1661–1670 (2023). https://doi.org/10.1007/s13304-023-01460-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-023-01460-4