Abstract
Introduction
Using pooled data from the REALI European database, we evaluated the impact of previous basal insulin (BI) type on real-life effectiveness and safety of switching to insulin glargine 300 U/ml (Gla-300) in people with suboptimally controlled type 2 diabetes.
Methods
Patient-level data were pooled from 11 prospective, open-label, 24-week studies. Participants were classified according to the type of prior BI. Of the 4463 participants, 1282 (28.7%) were pre-treated with neutral protamine Hagedorn (NPH) insulin and 2899 (65.0%) with BI analogues (BIAs), and 282 (6.3%) had undetermined prior BI.
Results
There were no meaningful differences in baseline characteristics between subgroups, except for a higher prevalence of diabetic neuropathy in the NPH subgroup (21.6% versus 7.8% with BIAs). Mean ± standard deviation haemoglobin A1c (HbA1c) decreased from 8.73 ± 1.15% and 8.35 ± 0.95% at baseline to 7.71 ± 1.09% and 7.82 ± 1.06% at week 24 in the NPH and BIA subgroups, respectively. Least squares (LS) mean change in HbA1c was − 0.85% (95% confidence interval − 0.94 to − 0.77) in NPH subgroup and − 0.70% (− 0.77 to − 0.64) in BIA subgroup, with a LS mean absolute difference between subgroups of 0.16 (0.06–0.26; p = 0.002). Gla-300 mean daily dose was slightly increased at week 24 by 0.07 U/kg/day (approximately 6 U/day) in both subgroups. Incidences of symptomatic and severe hypoglycaemia were low, without body weight change.
Conclusions
Irrespective of previous BI therapy (NPH insulin or BIAs), switching to Gla-300 improved glycaemic control without weight gain and with low symptomatic and severe hypoglycaemia incidences. However, a slightly greater glucose-lowering effectiveness was observed in people pre-treated with NPH insulin.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Switching basal insulin (BI) in people with type 2 diabetes mellitus (T2DM) is motivated by several factors including suboptimal glucose control, unacceptable frequency of hypoglycaemia, fear of weight gain, titration difficulties, or low treatment adherence |
By using the REALI database to pool patient-level data from 11 prospective studies reflecting routine clinical practice in different European countries, we sought to expand knowledge regarding the real-life effectiveness and safety of switching to Gla-300 in people with T2DM uncontrolled on NPH insulin or on BI analogues |
What was learned from the study? |
Gla-300 can improve glycaemic control without weight gain and with a low hypoglycaemia incidence, regardless of the nature of prior BI therapy |
People with suboptimally controlled T2DM who switch to Gla-300 from NPH insulin show slightly greater haemoglobin A1c reduction than those who switch from BI analogues |
Introduction
Based on clinical practice guidelines, people with type 2 diabetes mellitus (T2DM) who are unable to reach target haemoglobin A1c (HbA1c) levels with oral antidiabetic drugs (OADs) may be initiated on basal insulin (BI) therapy [1, 2]. BI options include neutral protamine Hagedorn (NPH) insulin, first-generation BI analogues (BIAs), namely insulin detemir and insulin glargine 100 U/ml (Gla-100), and second-generation BIAs namely insulin glargine 300 U/ml (Gla-300) and insulin degludec [1]. Long-acting BIAs (i.e., insulin detemir, Gla-100, Gla-300, and insulin degludec) may however be preferred over the intermediate-acting NPH insulin, since they show comparable glycaemic control with a reduced risk of hypoglycaemia [1, 2].
Gla-300 has several advantages when compared with NPH insulin and first-generation BIAs. These include a more prolonged half-life and a smoother pharmacokinetic/pharmacodynamic profile, coupled with low fluctuation and high reproducibility, resulting in evenly distributed glucose-lowering activity beyond 24 h [3, 4]. This extended and more stable coverage of Gla-300 may translate into reduced treatment burden and improved adherence, which could in turn improve treatment outcomes [5, 6].
In the EDITION phase III clinical trial programme performed in a large population with a broad clinical spectrum of T2DM, patients who switched to Gla-300 from another BI, either Gla-100 or NPH insulin, demonstrated comparable glycaemic control with consistently fewer hypoglycaemic events at any time of the day and nocturnally compared with those who switched to Gla-100 [7]. Real-world evidence concerning switching to Gla-300 has also been encouraging, with real-life prospective studies from different countries across Europe showing that a direct switch to Gla-300 from other BIs resulted in improved glycaemic control and a reduced risk of hypoglycaemia without weight gain [8,9,10,11,12,13]. However, there are very limited prospective real-world data evaluating the switch from NPH insulin to Gla-300, with only one published study from Poland prospectively assessing the effectiveness of switching from NPH insulin to Gla-300 in a total of 469 people with T2DM [8]. Hence, by using the REALI database to pool patient-level data from 11 observational/low-interventional, prospective studies reflecting routine clinical practice in different European countries, we sought to expand knowledge regarding the real-life effectiveness and safety of switching to Gla-300 in people with T2DM suboptimally controlled on a non-Gla-300 BI regimen.
Methods
Study Design and Participants
This REALI analysis included pooled data from 11 multicentre, prospective, open-label studies of a minimum duration of 24 weeks conducted between June 2015 and April 2019 in Germany, Austria, Switzerland, the Netherlands, Spain, France, the Czech Republic, Greece, Poland, Denmark, Slovenia, Slovakia, Croatia, the UK, Belgium, Serbia, Bulgaria, and Hungary [9,10,11,12,13,14,15,16,17,18,19]. The methodology of the REALI project and previous analyses from the REALI database have been presented elsewhere [20,21,22].
Patients included in this analysis were adults with T2DM inadequately controlled (HbA1c ≥ 7.0%) on previous BI therapy (± prandial and/or premixed insulin) with or without OADs who switched to Gla-300 therapy. In the pooled studies, patients were switched to Gla-300 upon the treating physician-investigator's decision because of suboptimal glucose control, titration difficulties, frequent hypoglycaemic episodes, or fear of hypoglycaemia. Gla-300 treatment was applied according to its approved label [23]. Gla-300 was administered subcutaneously once daily, at the same time of the day ± 3 h if needed.
All pooled studies were conducted according to the principles of the Declaration of Helsinki and the Good Clinical Practice guidelines and were approved by the relevant institutional review boards/ethics committees. All participants gave written informed consent. Before data pooling, all patient information was de-identified. Consequently, no ethical approval was required for this pooled analysis.
Assessments
Data were collected at baseline, 12 weeks, and 24 weeks. At baseline, recorded data included demographics, body weight and/or body mass index (BMI), T2DM duration, diabetic complications and cardiovascular comorbidities, previous antidiabetic therapy (OADs and insulins), and glycaemic parameters. At follow-up visits, current glycaemic variables, body weight, Gla-300 daily dose, and hypoglycaemic events were recorded.
Efficacy outcomes evaluated in the pooled analysis were the changes in HbA1c and fasting plasma glucose (FPG) from baseline to week 12 and week 24 of Gla-300 treatment as well as the proportion of patients achieving HbA1c targets of < 7.0% (< 53 mmol/mol), < 7.5% (< 58.5 mmol/mol), and < 8.0% (< 63.9 mmol/mol) at week 24.
Safety outcomes included hypoglycaemia incidence and annualised rate (events per patient-year), calculated for symptomatic and severe hypoglycaemic events occurring at any time of the day (24 h) and during the night (00:00–05:59 h). Symptomatic hypoglycaemia was defined as any event with clinical symptoms with or without documented blood glucose measurement. Severe hypoglycaemia was defined as any event requiring assistance from another person to actively administer carbohydrates, glucagon, or take other corrective actions. Other hypoglycaemic events (e.g., asymptomatic hypoglycaemia, symptomatic confirmed hypoglycaemia, daytime hypoglycaemia) were not reported across all individual studies and were hence not included in the REALI analysis. Likewise, hypoglycaemia during the 4-week period before Gla-300 initiation was not reported in most of the individual studies.
The pooled analysis also evaluated changes in body weight and the daily dose of Gla-300 (expressed in both U/day and in U/kg/day) from baseline to weeks 12 and 24.
Statistical Analysis
To evaluate the impact of prior BI regimens on the effectiveness and safety of Gla-300, patients were classified into two subgroups: those treated with prior NPH insulin and those previously treated with BIAs (i.e., Gla-100, insulin detemir, insulin degludec).
The change in HbA1c from baseline to weeks 12 and 24 of Gla-300 treatment was evaluated using a mixed model for repeated measures (MMRM), with fixed categorical effects of study, visit, subgroup category, and subgroup category-by-visit interaction as well as continuous fixed covariates of baseline HbA1c, baseline HbA1c value-by-visit interaction, age, age value-by-visit interaction, BMI, and BMI value-by-visit interaction. Based on this MMRM, we estimated the least squares (LS) mean changes in HbA1c from baseline to week 24 in the two subgroups and the corresponding 95% confidence intervals (CIs). All other efficacy and safety endpoints as well as baseline characteristics were summarised descriptively, with categorical variables presented as counts and percentages and continuous variables as mean ± standard deviation (SD) or as median (quartile 1–quartile 3).
Effectiveness and safety analyses were performed on all included patients who received at least one Gla-300 dose. No imputation of missing data was performed. All statistical tests were two-sided, with a p value of < 0.05 considered statistically significant. All analyses were performed using SAS version 9.4 (SAS Institute Inc, Cary, NC, USA).
Results
Participants
A total of 4463 participants were included in this REALI pooled analysis, of whom 4372 (98.0%) received at least one Gla-300 dose and were hence part of the effectiveness and safety analyses. Of the 4463 included participants, 282 (6.3%) had undetermined prior BI type. Among the remaining 4181 participants, 1282 (28.7%) switched to Gla-300 from NPH insulin and 2899 (65.0%) from BIAs, namely Gla-100 (1947/2899; 67.2%), insulin detemir (615/2899; 21.2%), insulin degludec (316/2899; 10.9%), and other insulins (21/2899; 0.7%). Baseline characteristics were overall comparable between the two BI pre-treated subgroups (Table 1). The mean ± SD age of the 4463 participants was 64.1 ± 9.6 years, with slightly more male patients enrolled (53.5%). The mean ± SD BMI was 32.7 ± 5.7 kg/m2, with most participants (64.9%) having a baseline BMI ≥ 30 kg/m2. Median diabetes duration was 12.0 years, with most participants receiving at baseline biguanides (73.0%), followed by dipeptidyl peptidase-4 inhibitors (25.5%) and sulphonylureas (18.2%). The mean ± SD baseline HbA1c in the 4463 included participants was 8.46 ± 1.05%, while the mean ± SD baseline FPG was 175.6 ± 52.7 mg/dl.
Glycaemic Control
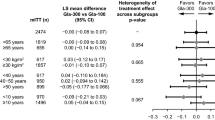
In the efficacy population (N = 4372), mean ± SD HbA1c decreased from 8.47 ± 1.05% at baseline to 7.78 ± 1.08% at week 24, corresponding to a LS mean change in HbA1c from baseline to week 24 of − 0.76% (95% CI − 0.81 to − 0.70). In the NPH and BIA subgroups, mean ± SD HbA1c decreased from 8.73 ± 1.15% and 8.35 ± 0.95% at baseline to 7.71 ± 1.09% and 7.82 ± 1.06% at week 24, respectively. Accordingly, the LS mean decrease in HbA1c from baseline was statistically significantly higher in patients previously treated with NPH insulin than in those previously treated with BIAs (Fig. 1) at both week 12 (p = 0.02) and week 24 (p = 0.002). At week 24, the LS mean decrease in HbA1c from baseline was 0.85% in the NPH insulin subgroup and 0.70% in the BIA subgroup, for a between-group difference of 0.16 (95% CI 0.06–0.26). Consistently, the proportion of patients achieving HbA1c targets of < 7.0%, < 7.5%, and < 8.0% at week 24 was numerically higher in patients previously treated with NPH insulin than in those previously treated with BIAs (Fig. 2).
Observed mean haemoglobin A1c (HbA1c) and least squares (LS) mean change (95% confidence interval [CI]) in HbA1c from baseline to weeks 12 and 24 according to previous basal insulin. N = number of patients with available data at each time point. BIA basal insulin analogue, NPH neutral protamine Hagedorn
In line with changes in HbA1c, patients previously treated with NPH insulin showed a greater mean ± SD decrease in FPG from baseline to week 24 than those previously treated with BIAs (change of − 46.4 ± 64.4 mg/dl versus − 22.5 ± 77.9 mg/dl). In both subgroups, the reduction in FPG happened mainly in the first 12 weeks of Gla-300 treatment (Fig. 3). In the overall efficacy population (N = 4372), the observed mean ± SD FPG decreased from 176.3 ± 52.5 mg/dl at baseline to 146.2 ± 60.5 mg/dl at week 24, corresponding to an observed mean ± SD change of − 29.8 ± 74.0 mg/dl.
Hypoglycaemia, Gla-300 Dose, and Body Weight
During the 24-week Gla-300 treatment period, 555/4372 (12.7%) patients experienced at least one hypoglycaemic episode. Incidences and event rates for symptomatic and severe hypoglycaemia occurring at any time of the day and during the night were low in both subgroups (Table 2). The observed daily dose of Gla-300 slightly increased from baseline to week 24 by an overall mean change of 0.07 U/kg/day (approximately 6 U/day) in both subgroups, with the greatest dose increase during the initial 12 weeks of Gla-300 treatment (Table 3). Body weight remained stable throughout the 24-week Gla-300 treatment period (Table 3).
Discussion
Switching BI in people with T2DM is motivated by several factors including suboptimal glucose control, unacceptable frequency of hypoglycaemia, fear of weight gain, titration difficulties, or low treatment adherence resulting from a complex regimen and heavy injection burden [5, 11]. In this REALI pooled analysis conducted in a large and clinically diverse population with T2DM, switching to Gla-300 from another BI (i.e., NPH insulin, Gla-100, insulin detemir, insulin degludec) was associated with a clinically meaningful and continuous decrease in HbA1c, especially in those switching from NPH insulin. These results are encouraging, particularly since patients previously treated with NPH insulin had higher levels of baseline HbA1c and FPG compared to those previously treated with BIAs, which may be related to a greater number and/or severity of hypoglycaemia episodes usually seen with NPH insulin compared to insulin glargine/detemir therapy, curbing the titration process [24].
The glycaemic improvement in the REALI analysis was achieved without any weight gain and with a low incidence of symptomatic and severe hypoglycaemia. Our results support the findings from randomised controlled trials (RCTs) and from other real-world studies not included in this REALI analysis conducted in people with inadequately controlled T2DM, in which switching to Gla-300 from other BIs was associated with an improved glycaemic control regardless of the nature or duration of prior BI therapy, a reduced incidence of hypoglycaemia, and a neutral or positive effect on body weight [6, 25,26,27]. The low incidence of symptomatic and severe hypoglycaemia after switching to Gla-300 from previous BIs can be attributed to the flat and stable pharmacokinetic/pharmacodynamic profile of Gla-300 and its 24-h duration of action that help to reduce the magnitude and frequency of blood glucose fluctuations [28].
Fear of hypoglycaemia is known to reduce patients’ adherence to insulin regimens and decrease their quality of life, as it can promote compensatory behaviours to avoid hypoglycaemia, such as decreased or omitted insulin doses, resulting in poor glycaemic control and an increased risk of serious health consequences [29]. Hence, the reported low incidence of hypoglycaemia associated with Gla-300 is important to give people with T2DM the confidence to initiate and optimise their BI therapy and to better control their disease in the long term. The reduction of hypoglycaemia incidence by switching to Gla-300 from another BI regimen has also been found to have a positive economic impact by reducing healthcare utilisation such as inpatient hospitalisation rates and emergency department visits [26].
Insulin titration is another challenging issue in routine clinical practice. In the EDITION 1 and EDITION 2 RCTs, people with T2DM who switched from Gla-100 or NPH insulin to Gla-300 showed a mean dose increase of 0.28–0.36 U/kg/day from baseline to week 24 of Gla-300 therapy, with the greatest Gla-300 dose increase during the initial 12 weeks of treatment (of 0.25–0.31 U/kg/day) [6]. In the present REALI analysis, the dose of Gla-300 also increased until week 12 of treatment and then stabilised. However, in REALI, mean Gla-300 dose increased from baseline to weeks 12 and 24 of treatment by only 0.07 U/kg/day at both time points, suggesting that changes in insulin dosing in routine clinical practice are smaller than those seen in RCTs. Due to its stable pharmacokinetic/pharmacodynamic profile as well as its longer duration of action lasting up to 24 h, Gla-300 requires overall less frequent titration than other BIs to reach steady state over the dosing period [30]. Nevertheless, the small increase in the mean daily dose of Gla-300 that was reported in REALI suggests that more efforts regarding timely and efficient BI titration are needed in routine clinical practice, with a well-defined and easy BI treatment algorithm as well as continuous patient education and empowerment [11, 12, 16, 27].
There are limitations to the current pooled analysis, such as the relatively short treatment duration and the presence of a potential reporting bias, which is inherent to observational studies. There is usually underreporting of hypoglycaemic events in real-world studies, which may lead to underestimation of absolute rates of hypoglycaemia. This underestimation is also possible in RCTs, in which patient-reported hypoglycaemic episodes are compared with glucometer records [31]. However, in the present analysis, the direction of changes in hypoglycaemia risk throughout the 24-week Gla-300 treatment period as well as between-group comparisons seems to be maintained, thereby lending confidence to the data reported herein. Of note, symptomatic and severe hypoglycaemias occurring at any time of the day (24 h) and during the night were the only types of hypoglycaemic events that were consistently reported across the individual pooled studies [9,10,11,12,13,14,15,16,17,18,19]. Other hypoglycaemic events (e.g., asymptomatic hypoglycaemia, symptomatic confirmed hypoglycaemia, daytime hypoglycaemia) were not reported across all individual studies and were hence not included in the REALI analysis. Likewise, assessment of hypoglycaemia during the 4-week period before Gla-300 initiation was not reported in most individual studies. In addition, this REALI analysis did not pool data on Gla-300-related adverse events/serious adverse events other than hypoglycaemia, since the individual studies did not identify new adverse events or safety signals during Gla-300 treatment. All reported adverse events in the individual studies [9,10,11,12,13,14,15,16,17,18,19] were consistent with Gla-300’s established safety profile. Furthermore, although there is a diverse representation of countries across Europe in REALI, bias may exist in some data given the inclusion of different countries with different healthcare systems and practices, which may impact T2DM management, particularly the choice of BI for insulin initiation as well as BI titration. For example, in some European countries (e.g., Serbia, Norway, Sweden, Hungary), NPH insulin is recommended by local guidelines as the first-line insulin over BIAs. Another limitation of this pooled analysis is the lack of a comparator arm versus Gla-300 inherent to the design of the individual studies [9,10,11,12,13,14,15,16,17,18,19].
This pooled analysis is nevertheless strengthened by its large sample size as well as the prospective nature of the evaluated studies increasing the reliability of data when compared to retrospective real-world data analyses. Additional strengths include the application of standardised endpoint definitions to reduce study-specific differences, the adoption of a MMRM analysis with adjustments for baseline factors, and the relatively high external validity of the included studies as a result of the lack of strict inclusion and exclusion criteria. Overall, this REALI analysis offers valuable insight regarding the effectiveness and safety of Gla-300 administered in routine clinical practice among people with T2DM suboptimally controlled on NPH insulin or other BIAs.
Conclusions
Irrespective of previous BI therapy, switching to Gla-300 was associated with improved glycaemic control without weight gain and with a low incidence of symptomatic and severe hypoglycaemia in people with T2DM suboptimally controlled on BI with or without OADs. However, a slightly greater glucose-lowering effectiveness was observed in people pre-treated with NPH insulin.
References
Davies MJ, D’Alessio DA, Fradkin J, Management of hyperglycemia in type 2 diabetes, et al. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2018;41(12):2669–701.
Garber AJ, Handelsman Y, Grunberger G, et al. Consensus statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the comprehensive type 2 diabetes management algorithm—2020 executive summary. Endocr Pract. 2020;26(1):107–39.
Becker RH, Dahmen R, Bergmann K, Lehmann A, Jax T, Heise T. New insulin glargine 300 units ml-1 provides a more even activity profile and prolonged glycemic control at steady state compared with insulin glargine 100 units ml-1. Diabetes Care. 2015;38(4):637–43.
Becker RH, Nowotny I, Teichert L, Bergmann K, Kapitza C. Low within- and between-day variability in exposure to new insulin glargine 300 U/ml. Diabetes Obes Metab. 2015;17(3):261–7.
Anderson SL, Trujillo JM, Anderson JE, Tanenberg RJ. Switching basal insulins in type 2 diabetes: practical recommendations for health care providers. Postgrad Med. 2018;130(2):229–38.
Roussel R, d’Emden MC, Fisher M, et al. Glycaemic control and hypoglycaemia in people with type 2 diabetes switching from twice-daily basal insulin to once-daily insulin glargine 300 U/ml or insulin glargine 100 U/ml (EDITION 1 and EDITION 2 subgroup analysis). Diabetes Obes Metab. 2018;20(2):448–52.
Ritzel R, Roussel R, Bolli GB, et al. Patient-level meta-analysis of the EDITION 1, 2 and 3 studies: glycaemic control and hypoglycaemia with new insulin glargine 300 U/ml versus glargine 100 U/ml in people with type 2 diabetes. Diabetes Obes Metab. 2015;17(9):859–67.
Wolnik B, Wiza D, Szczepanik T, Syta A, Klupa T. Switching from neutral protamine Hagedorn insulin to insulin glargine 300 U/ml improves glycaemic control and reduces hypoglycaemia risk: results of a multicentre, prospective, observational study. J Diabetes Res. 2020;2020:8751348.
Hidvégi T, Balogh Z, Vass V, Kovács G, Stella P. Insulin glargine 300 U/ml and insulin glulisine treatment in patients with type 2 diabetes: a non-interventional study of effectiveness in routine clinical practice. Diabetes Ther. 2020;11(2):467–78.
Prázný M, Flekac M, Jelínek P, Mašková J. Insulin glargine 300 units/ml effectiveness in patients with T2DM uncontrolled by basal insulin in real-life settings in the Czech Republic. J Diabetes Mellit. 2020;10:109–23.
Gourdy P, Bahloul A, Boultif Z, Gouet D, Guerci B. Efficacy and safety of switching patients inadequately controlled on basal insulin to insulin glargine 300 U/ml: the TRANSITION 2 study. Diabetes Ther. 2020;11(1):147–59.
Kamenov Z, Pehlivanova V, Kuneva T, et al. Real-world effectiveness and safety of insulin glargine 300 U/ml in patients with T2D uncontrolled on NPH or premixed insulins as part of routine clinical practice in Bulgaria: ToUPGRADE study. Diabetes Ther. 2021;12(3):913–30.
Seufert J, Wiesli P, Fritsche A, et al. Switching the basal insulin to insulin glargine 300 U/ml in people with type 2 diabetes under basal insulin supported oral therapy: observational trial on effectiveness and safety. Diabetes Obes Metab. 2022;24(1):72–81.
Pscherer S, Fritsche A, Anderten H, Pegelow K, Seufert J, Pfohl M. Switching to insulin glargine 300 U/ml (Gla-300) after failure of advanced insulin therapy (IT) with other basal insulins (BI) in patients (Pts) with type 2 diabetes (T2DM) improved glycemic control [Abstract]. Diabetes. 2018;67(Supplement 1):2288-PUB.
Wieringa TH, de Wit M, Twisk JW, Snoek FJ. Improved diabetes medication convenience and satisfaction in persons with type 2 diabetes after switching to insulin glargine 300 U/ml: results of the observational OPTIN-D study. BMJ Open Diabetes Res Care. 2018;6(1): e000548.
Russell-Jones D, Dauchy A, Delgado E, et al. Take control: a randomized trial evaluating the efficacy and safety of self-versus physician-managed titration of insulin glargine 300 U/ml in patients with uncontrolled type 2 diabetes. Diabetes Obes Metab. 2019;21(7):1615–24.
Perez A, Carrasco-Sánchez FJ, González C, et al. Efficacy and safety of insulin glargine 300 U/ml (Gla-300) during hospitalization and therapy intensification at discharge in patients with insufficiently controlled type 2 diabetes: results of the phase IV COBALTA trial. BMJ Open Diabetes Res Care. 2020;8(1): e001518.
Colin IM, Alexandre K, Bruhwyler J, Scheen A, Verhaegen A. Patient-reported outcomes with insulin glargine 300 U/ml in people with type 2 diabetes: the MAGE multicenter observational study. Diabetes Ther. 2020;11(8):1835–47.
Velojic-Golubovic M, Ciric V, Dimitrijevic M, et al. Clinical benefit of insulin glargine 300 U/ml among patients with type 2 diabetes mellitus previously uncontrolled on basal or premixed insulin in Serbia: a prospective, observational, single-arm, multicenter, real-world study. Diabetes Ther. 2021;12(7):2049–58.
Freemantle N, Bonadonna RC, Gourdy P, et al. Rationale and methodology for a European pooled analysis of postmarketing interventional and observational studies of insulin glargine 300 U/ml in diabetes: protocol of REALI project. BMJ Open. 2020;10(4): e033659.
Bonadonna RC, Mauricio D, Müller-Wieland D, et al. Impact of age on the effectiveness and safety of insulin glargine 300 U/ml: results from the REALI European pooled data analysis. Diabetes Ther. 2021;12(4):1073–97.
Gourdy P, Bonadonna RC, Freemantle N, et al. Does gender influence the effectiveness and safety of insulin glargine 300 U/ml in patients with uncontrolled type 2 diabetes? Results from the REALI European pooled analysis. Diabetes Ther. 2022;13(1):57–73.
European Medicines Agency. Toujeo: EPAR—Product Information. 2021. https://www.ema.europa.eu/en/documents/product-information/toujeo-epar-product-information_en.pdf. Accessed 26 Oct 2022.
Strandberg AY, Khanfir H, Mäkimattila S, Saukkonen T, Strandberg TE, Hoti F. Insulins NPH, glargine, and detemir, and risk of severe hypoglycemia among working-age adults. Ann Med. 2017;49(4):357–64.
Bonadonna RC, Renard E, Cheng A, et al. Switching to insulin glargine 300 U/ml: is duration of prior basal insulin therapy important? Diabetes Res Clin Pract. 2018;142:19–25.
Zhou FL, Ye F, Berhanu P, et al. Real-world evidence concerning clinical and economic outcomes of switching to insulin glargine 300 units/ml vs other basal insulins in patients with type 2 diabetes using basal insulin. Diabetes Obes Metab. 2018;20(5):1293–7.
Ragonese M, Larosa M, Angotti S, et al. Clinical outcomes of switching to insulin glargine 300 U/ml from other basal insulins in people with type 2 diabetes in Italy: a real-world study. Diabetes Ther. 2020;11(10):2283–98.
Bailey TS, Pettus J, Roussel R, et al. Morning administration of 0.4 U/kg/day insulin glargine 300 U/ml provides less fluctuating 24-h pharmacodynamics and more even pharmacokinetic profiles compared with insulin degludec 100 U/ml in type 1 diabetes. Diabetes Metab. 2018;44(1):15–21.
Fidler C, Elmelund Christensen T, Gillard S. Hypoglycemia: an overview of fear of hypoglycemia, quality-of-life, and impact on costs. J Med Econ. 2011;14(5):646–55.
Ghosh S, Ghosh R. Glargine-300: an updated literature review on randomized controlled trials and real-world studies. World J Diabetes. 2020;11(4):100–14.
Buzzetti R, Bonadonna RC, Giaccari A, et al. Underestimation of hypoglycaemia using patients’ diaries compared with downloaded glucometer data: an ITAS post hoc analysis. Diabetes Obes Metab. 2022;24(2):327–31.
Acknowledgements
Funding
This study was funded by Sanofi (Paris, France). The journal’s Rapid Service Fee was also funded by Sanofi (Paris, France).
Medical Writing, Editorial, and Other Assistance
We thank Thomas Rohban, MD, and Magalie El Hajj, PharmD, from Partner 4 Health (Paris, France) for providing medical writing support in accordance with Good Publication Practice (GPP3) guidelines (http://www.ismpp.org/gpp3), which was funded by Sanofi.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
All authors contributed to the project design and the analysis plan. Celine Mauquoi performed the statistical analysis of the data. All authors were involved in the interpretation of the data, writing and reviewing drafts of the manuscript, and approved the final version for submission.
Prior Presentation
Preliminary results were presented at the American Diabetes Association 82nd Scientific Sessions, New Orleans, Louisiana, June 3–7, 2022.
Disclosures
Dirk Müller-Wieland has acted as a consultant and has served on the speaker bureau for Amarin, Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Daiichi-Sankyo, Lilly, Merck Sharp & Dohme, Novo Nordisk, and Sanofi. Nick Freemantle has received research support and has acted as a consultant for Gedeon Richter, Abbott Singapore, Galderma, ALK, AstraZeneca, Ipsen, Vertex, Sanofi, Thea, Aimmune, Novartis, Novo Nordisk, Allergan, Alliance, and Merck Sharp & Dohme. Riccardo C. Bonadonna has served on the speaker bureau for Sanofi, Merck Sharp & Dohme, Bristol-Myers Squibb, AstraZeneca, and Janssen, and has served on the advisory panel for Merck Sharp & Dohme, Eli Lilly, Sanofi, and Johnson & Johnson. Celine Mauquoi is an IDDI employee and has acted as a biostatistics contractor for Sanofi. Gregory Bigot is an IVIDATA employee. Mireille Bonnemaire is an employee and stakeholder of Sanofi. Pierre Gourdy has received advisory board and speaker honoraria from Abbott, Amgen, AstraZeneca, Novo Nordisk, Boehringer Ingelheim, Eli Lilly, Merck Sharp & Dohme, Mundipharma, Organon, Sanofi, and Servier. Didac Mauricio has acted as a consultant and has served on the speaker bureau for Almirall, Eli Lilly, Esteve, Ferrer, Janssen, Menarini, Merck Sharp & Dohme, Novo Nordisk, and Sanofi.
Compliance with Ethics Guidelines
This analysis did not involve primary data collection by the authors, and all patient information was de-identified; consequently, separate ethical approval was not required. Protocols for all included studies were approved by the appropriate ethics committees, and the studies were conducted according to Good Clinical Practice guidelines and the Declaration of Helsinki. All patients provided written informed consent.
Data Availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Müller-Wieland, D., Freemantle, N., Bonadonna, R.C. et al. Glycaemic Control in People with Type 2 Diabetes Mellitus Switching from Basal Insulin to Insulin Glargine 300 U/ml (Gla-300): Results from the REALI Pooled Database. Diabetes Ther 14, 401–413 (2023). https://doi.org/10.1007/s13300-022-01356-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-022-01356-3