Abstract
Diabetes is a risk factor for greater severity of coronavirus disease 2019 (COVID-19). The stress hyperglycemia ratio (SHR) is an independent predictor of critical illness, and it is reported to have a stronger association than absolute hyperglycemia. The aim of this study was to assess the relationship of absolute hyperglycemia and SHR with the severity of COVID-19, since there are no studies investigating SHR in patients with COVID-19. We conducted a retrospective observational study on hospitalized patients with COVID-19 in the first months of the pandemic, regarding absolute hyperglycemia, SHR, and severity outcomes. Of the 374 patients, 28.1% had a previous diagnosis of type 2 diabetes. Absolute hyperglycemia (64.8% versus 22.7%; p < 0.01) and SHR [1.1 (IQR 0.9–1.3) versus 1.0 (IQR 0.9–1.2); p < 0.001] showed a statistically significant association with previous diabetes. Absolute hyperglycemia showed a significant association with clinical severity of COVID-19 (79.0% versus 62.7%; p < 0.001), need for oxygen therapy (74.8% versus 54.4%; p < 0.001), invasive mechanical ventilation (28.6% versus 11.6%; p < 0.001), and intensive care unit (30.3% versus 14.9%; p = 0.002), but not with mortality; by contrast, there was no statistically significant association between SHR and all these parameters. Our results are in agreement with the literature regarding the impact of absolute hyperglycemia on COVID-19 severity outcomes, while SHR was not a significant marker. We therefore suggest that SHR should not be evaluated in all patients admitted in the hospital for COVID-19, and we encourage the standard measures at admission of blood glucose and HbA1c levels.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
SHR is an independent predictor of critical illness, and it is reported to have a stronger association than absolute hyperglycemia. |
There are no studies investigating SHR in patients with COVID-19. |
The aim of this study was to assess the relationship of absolute hyperglycemia and SHR with the severity of COVID-19. |
Absolute hyperglycemia showed a significant association with clinical severity of COVID-19, while SHR was not a significant marker. |
SHR should not be evaluated in all patients admitted to the hospital for COVID-19. |
Introduction
The infection caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was first described in December 2019 in Wuhan, China, as a series of pneumonia reports of unknown cause, but a wide range of clinical, laboratory, and radiologic presentations are possible [1]. Only 3 months later, in March 2020, the World Health Organization declared coronavirus disease 2019 (COVID-19) a global pandemic. Almost 1 year later, this disease was responsible for more than 110,000,000 confirmed cases and 2,000,000 deaths [2].
Studies have not clearly shown that diabetes increases the susceptibility to COVID-19, while it seems to be associated with more clinically severe forms of the disease [3]; indeed, the presence of diabetes in patients hospitalized for COVID-19 has been consistently shown to be associated to worst outcomes, namely a higher proportion of intensive care unit (ICU) admissions and deaths [4]. In a retrospective study performed in Wuhan, COVID-19 in-patients with diabetes who did not survive had higher levels of blood glucose during hospitalization [5]. Indeed, like in other viral infections, hyperglycemia can be related to more adverse outcomes in patients with COVID-19, independently of previous diabetes diagnosis [6]. Another Chinese retrospective observational study showed that at-admission hyperglycemia in patients without a history of diabetes had a higher risk of a composite outcome (ICU admission, mechanical ventilation, and death) compared with normoglycemic patients without known diabetes [7]. In the CORONADO study, at-admission hyperglycemia, but not glycated hemoglobin (HbA1c), was found to be associated with the primary composite outcome (death and tracheal intubation for mechanical ventilation within the first 7 days after hospital admission) [8].
A transient phase of hyperglycemia may develop in response to acute illness, which may occur regardless of the previous diagnosis of diabetes, associated with worst clinical outcome in different clinical contexts [9]. This variation in the glycemic level is called stress hyperglycemia and can be quantified by the stress hyperglycemia ratio (SHR). SHR is calculated as the quotient of at-admission blood glucose divided by estimated average blood glucose, which is derived from the HbA1c level. An observational study involving 2290 patients hospitalized for acute illness showed that SHR above 1.14 was a better biomarker of critical illness (in-hospital death and admission to the ICU) than absolute hyperglycemia [10]. Yet, there are no studies investigating SHR in patients with COVID-19.
Therefore, in the present study we aimed to assess the impact of absolute at-admission hyperglycemia on clinical severity of hospitalized patients with COVID-19 in the first months of the pandemic before the availability of the vaccines, which favorably impacted the clinical outcome of such patients. We also examined the association between SHR and the same clinical outcomes of COVID-19 in all patients for whom it was possible to calculate this biomarker.
Methods
Study Design and Participants
This is a retrospective observational study of patients hospitalized with COVID-19, in a medical ward of Curry Cabral Hospital (Centro Hospitalar Universitário Lisboa Central—CHULC), in the first 8 months of the COVID-19 pandemic in Portugal (from 1 March to 31 October 2020). In this study were included all patients admitted to the hospital with SARS-CoV-2 detection in a laboratory test by real-time polymerase chain reaction, regardless the cause of admission. This population was characterized for demographic features, previous diagnosis of diabetes, blood glucose level at admission, HbA1c assessed during hospital stay, and clinical outcomes for COVID-19 severity—need for oxygen therapy, invasive mechanical ventilation (IMV), admission to ICU, and mortality. The medical care provided to each patient was selected according to the clinical context, considering the clinical judgment and protocols provided by the National General-Directorate of Health [11].
Data Collection
Demographic and clinical data were collected from the electronic clinical records. The demographic data collected were age, gender, and ethnicity of the patient. The main clinical data collected were the presence of a previous diagnosis of diabetes mellitus. The analytical data collected were blood glucose level at admission (obtained by collecting venous or arterial blood in the emergency department or in the first 24 h of admission to the ward) and HbA1c any time during hospital stay. The clinical outcomes evaluated were: clinical severity of COVID-19, need for oxygen therapy, need for IMV, admission to ICU, and mortality. These data were evaluated in a single moment and placed directly into a digital file, protected by password and only available to the medical team that was responsible for the patients.
This study was performed in accordance with the 1964 Declaration of Helsinki and its later amendments. This study has a retrospective and observational nature that had no impact on the diagnosis or treatment of those involved. The article was approved for publication by the Health Ethics Committee of Centro Hospitalar Universitário Lisboa Central (CES 1226/2022). Patient consent was waived since the data were pseudo-anonymized, collected from an electronic record consultation, with an observational and retrospective character, and subsequently destroyed. The need for informed consent was waived by the Health Ethics Committee of Centro Hospitalar Universitário Lisboa Central (CES 1226/2022).
Definitions
Previous diagnosis of diabetes was considered when mentioned in the patient’s personal medical history or if the patient was under antidiabetic medication prior to hospitalization. The HbA1c level was not considered for a previous diagnosis of diabetes, even when higher than 6.5%; this cluster of patients was considered to have new-onset diabetes. Absolute hyperglycemia at hospital admission was defined as any blood glucose level greater than 140 mg/dL in the emergency department or within the first 24 h after hospital admission, according to the American Diabetes Association guidelines [12] and the joint recommendations of the Portuguese Society of Diabetology and the Portuguese Society of Internal Medicine [13]. The determination of the clinical severity of COVID-19 for each patient was based on national clinical guidelines [11] and clinical judgment. A mild COVID-19 illness was considered to be one with mild symptoms (fever lasting fewer than 3 days and with adequate response to antipyretics, cough, sore throat, headache, muscle pain, nausea, vomiting or diarrhea without dehydration, loss of taste and smell) without respiratory distress or radiological evidence of pneumonia. A moderate COVID-19 disease was considered to be one with clinical or radiological evidence of pneumonia dependent on clinical judgment with peripheral oxygen saturation ≥ 90% on room air and without hemodynamic instability; serious COVID-19 illness was defined as evidence of pneumonia with at least one criterion of tachypnea greater than 30 cycles per minute, breathing difficulty, peripheral oxygen saturation < 90% on room air, and hemodynamic instability (systolic pressure < 90 mmHg or heart rate > 125 bpm); critical illness was defined as acute respiratory distress syndrome with PaO2/FiO2 < 100 or septic shock.
Relative hyperglycemia was defined on the basis of SHR. SHR was calculated using blood glucose at admission and HbA1c according to this formula: \({\text{at admission blood glucose}} \div \left( {28.7 \times {\text{HbA}}1{\text{c}} - 46.7} \right)\) [10, 14]. Stress hyperglycemia was defined as an SHR greater than 1.14. This cutoff value has already been used in previous studies related to other clinical scenarios [15], since it has been shown to be associated with a higher risk of critical illness [10].
Outcome Measures
Patients in whom blood glucose was measured at admission were divided into two groups: patients with absolute hyperglycemia (blood glucose at admission > 140 mg/dL) and at-admission normoglycemic patients (blood glucose at admission ≤ 140 mg/dL). Patients in whom it was possible to calculate SHR (patients who had both glucose levels at admission and HbA1c measured) were divided into two groups: patients with stress hyperglycemia during hospitalization (SHR > 1.14) and patients without stress hyperglycemia (SHR ≤ 1.14). For each group, clinical outcomes of COVID-19 were assessed and compared between groups.
Statistical Analysis
Patients’ baseline characteristics were evaluated using descriptive statistics. Variables with non-normal distribution were analyzed nonparametrically by median and Mann–Whitney tests. Categorical variables were presented as numbers and percentage proportions. Continuous variables were analyzed parametrically by means and standard deviations. Differences in categorical variables were calculated with the χ2 method. Statistically significance was considered when p value < 0.05. Statistical analyses were performed with SPSS Software, version 23 (IBM Corporation, Armonk, NY, USA).
Results
From 1 March 2020 to 31 October 2020, 374 patients with COVID-19 were admitted to Functional Unit of Internal Medicine 7.2 of CHULC, in Lisbon, Portugal. Demographic and clinical variables of the patients involved in this study are presented in Table 1.
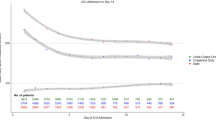
Most patients were male (n = 209 patients, 55.9%). The median age of hospitalized patients was 71.5 years (interquartile range 53.0–84.0 years). The mean age of the patients was 68.0 years, with a standard deviation of 19.3 years. Hospitalized women were older (median 79.0 years, IQR 60.5–88.0 years) than men (median 67.0, IQR 49.0–80.0 years). Most inpatients were Caucasian (n = 324 patients, 86.6%) and had no previous diagnosis of diabetes (n = 269 inpatients, 71.9%). A total of 105 patients (28.1%) had a prior diagnosis of diabetes. Of the 374 inpatients, blood glucose at hospital admission was not available for 14 patients. Considering the blood glucose value at admission, patients were categorized into two groups: a group (119 patients) with at-admission blood glucose > 140 mg/dL (at-admission hyperglycemia group) and another (241 patients) with blood glucose ≤ 140 mg/dL (at-admission normoglycemia group). Most patients with a previous diagnosis of diabetes had hyperglycemia at admission (n = 68 patients, 64.8%), while in patients without diagnosis of diabetes that percentage was lower (n = 61 patients, 22.7%). There was a significant association between the presence of a previous diagnosis of diabetes and the presence of absolute hyperglycemia at the initial clinical evaluation (p < 0.001). In patients with blood glucose measurement, the median blood glucose at admission was 121 mg/dL (IQR 97–165.3 mg/dL). HbA1c was measured in only 116 patients (31.0% of total) during hospitalization. The median HbA1c was 6.4% (IQR 5.7–7.8%) for all patients, 7.2% (IQR 6.2–8.3%) for those known for diabetes, and 5.9% (IQR 5.6–6.5%) for those without previous diagnosis. Once for estimation of SHR, it was necessary to have both at-admission blood glucose value as well as HbA1c measured during hospitalization. Data were available in 110 patients (29.4% of all). In those patients, SHR was significantly higher in the group with previous diabetes [1.1 (IQR 0.9–1.3) versus 1.0 (IQR 0.9–1.2); p < 0.001].
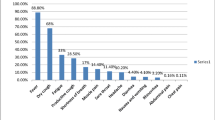
Most patients hospitalized for COVID-19 needed oxygen therapy at any time during hospitalization (n = 225, 60.2%). Table 2 presents clinical outcomes of patients depending on their glycemic status at admission.
Of patients with normoglycemia at admission, 54.4% (n = 131) needed oxygen supplementation during hospitalization, corresponding to 35.0% of patients admitted to hospital. Considering the total number of patients hospitalized for COVID-19, of those with hyperglycemia at admission, 23.8% (n = 89) needed supplemental oxygen during hospitalization. In patients with high blood glucose levels at admission, 74.8% needed supportive oxygen therapy (versus 25.2% who always remained without oxygen supply). This study showed a statistically significant association between absolute hyperglycemia at admission and need for oxygen therapy during COVID-19 hospitalization (74.8% versus 54.4%; p < 0.001). Most patients (n = 310, 82.9%) admitted to this ward did not undergo IMV. In patients hospitalized with COVID-19 who were ventilated, 53.1% had hyperglycemia at admission (n = 34, 9.1% of the total hospitalized). Absolute hyperglycemia at admission presented a statistically significant association with the use of IMV (28.6% versus 11.6%; p < 0.001). Considering the entire sample, 19.8% (n = 74) were admitted to the ICU. Most patients hospitalized with COVID-19 were normoglycemic at admission and did not need to be admitted to the ICU (n = 205, 54.8%). There was a statistically significant association between hyperglycemia at admission and ICU admission (30.3% versus 14.9%; p = 0.002). The mortality of patients hospitalized with COVID-19 in the considered period was 17.9%, with no significant difference between patients with or without absolute hyperglycemia: 20.2% (24 in 119) versus 17.4% (42 in 241), respectively. Considering all the patients hospitalized with COVID-19, 13.9% (n = 52) were asymptomatic, 19.8% (n = 74) presented with mild disease, 9.4% (n = 35) with moderate disease, 39.3% (n = 147) with severe illness, and 17.6% (n = 66) with critical illness. In this study, we found that the presence of absolute hyperglycemia at admission was a statistically significant factor for the severity of SARS-CoV-2 infection—moderate to critical disease versus asymptomatic to mild disease (79.0% versus 62.7%, respectively; p < 0.001). Compared with those with normoglycemia, the group with absolute hyperglycemia at admission presented lower percentage of patients with the asymptomatic, mild, and moderate forms of the disease and higher percentage of patients with the severe and critical forms.
Table 3 depicts the clinical outcomes between patients with and without stress hyperglycemia. Among the group of 110 patients where SHR was calculated, 37 patients (33.6%) presented values consistent with stress hyperglycemia (SHR > 1.14). There was no statistically significant difference between patients with and without stress hyperglycemia for any of the clinical outcomes considered.
Discussion
This study showed that at-admission absolute hyperglycemia in hospitalized patients with COVID-19 was statistically associated with a greater need for oxygen therapy, need for IMV, ICU admission, and greater clinical severity of COVID-19. However, absolute hyperglycemia at admission did not show a statistically significant association with mortality in these patients. Stress hyperglycemia (defined by SHR ≥ 1.14) in hospitalized patients with SARS-CoV-2 infection was not associated with worst clinical outcomes.
These results are in line with what has been described in other studies, but also extend such previous observations. The prevalence of diabetes in these 374 patients admitted with COVID-19 was 28.1%. This prevalence is higher than the estimated prevalence of diabetes in Portugal in the adult population (13.6% among adults aged 20–79 years) [16]. However, when considering older people, the prevalence of diabetes reaches 30% among Portuguese males, which is similar to the result obtained in the study [16]. This does not mean that diabetes increases the risk of acquiring COVID-19, but that it can be associated with more severe forms of the disease. A Chinese study showed a prevalence of diabetes in patients with COVID-19 similar to the prevalence of diabetes in China, but the prevalence of diabetes was much greater in patients with severe COVID-19 [5, 17]. Many contributions from different geographical areas have consistently shown that the prevalence of diabetes in patients with COVID-19 is not superior to that of the general population (reviewed in [18]); by contrast, the presence of diabetes has been associated with the most severe forms of COVID-19 worldwide [19]. Early studies from other European countries, such as Italy and Romania, performed in the first months of the pandemic, exactly like the present study, have also shown that the presence of diabetes was one of the key factors associated with COVID-19 mortality, together with hypertension, obesity, and chronic kidney disease [20, 21], explaining the high excess mortality early reported in Italy, the first European country seriously hit by COVID-19 [22].
Most hospitalized patients needed oxygen therapy during hospitalization. This observation is in line with the fact that one of the reasons for hospitalization is the need for supplemental oxygen supply. This became even more evident after support networks for patients with COVID-19 were created in Portugal to receive infected people without the need for hospital medical care, whose only reason for hospitalization was the inability to maintain social distance at home. The study showed that there was more at-admission hyperglycemia in patients who needed supplemental oxygen than in the group of patients who did not. Similar findings were found regarding IMV support and ICU admission. Admission hyperglycemia has been shown to be a predictor of greater severity of COVID-19, especially with an impact on the rapid worsening of respiratory function [23]. Regarding mortality, there was no statistically significant difference between the percentage of patients with absolute hyperglycemia at admission in the group of patients who survived compared with the group of patients who did not survive. This finding is different from what was found in studies carried out in other countries. In the USA, a retrospective observational study showed a particularly high mortality rate among individuals with uncontrolled hyperglycemia in the absence of diabetes (individuals with two or more blood glucose levels above 180 mg/dL with HbA1c below 6.5%) compared with patients with diabetes (defined as HbA1c greater than 6.5%) [24]. This may reflect the role of stress hyperglycemia, an acute and transient event, in patients with usually adequate glycemic control, represented by a normal level of HbA1c.
Stress hyperglycemia has been shown to be associated with adverse clinical events in different hospital settings. In patients without diabetes and normoglycemic before surgery, a blood glucose greater than 180 mg/dL after the surgical procedure led to a threefold increase in complications and sixfold increase in mortality, but the association with perioperative complications and deaths was present even with blood glucose levels between 140 and 180 mg/dL [25]. SHR is a parameter developed to quantify stress hyperglycemia that adjusts absolute hyperglycemia to the value of HbA1c [10]. To our knowledge, this is the first study that uses SHR to quantify stress hyperglycemia in patients hospitalized for COVID-19 and assesses that index in terms of clinical outcomes. However, SHR has been used to assess adverse outcomes in respiratory patients. In 2017, a study attempted to link stress hyperglycemia with acute exacerbation of chronic obstructive pulmonary disease. That study showed that glycemic variables adjusted to HbA1c, which included SHR, were not independent risk factors for the development of acute respiratory failure [26]. Furthermore, SHR did not show a statistically significant association with the development of acute respiratory failure. However other glycemic parameters derived from HbA1c were shown to have a superior discriminative power in relation to absolute hyperglycemia in predicting the development of acute respiratory failure [26]. In our study, the value of SHR was limited by the small number of patients in which HbA1c was assessed. This assay was performed in less than half of the patients. Thus, patients with an SHR value greater than 1.14 with adverse clinical outcomes may have been missed. We believe that this study highlights the importance of evaluating HbA1c in hospitalized patients, not only because it allows the calculation of SHR but also because it allows for a better characterization of the hospitalized population, whether or not a known diagnosis of diabetes is present.
The mechanisms responsible for glycemic decompensation in individuals with SARS-CoV-2 infection have been elucidated. Both hyperglycemia/diabetes and SARS-CoV-2 infection correspond to pro-inflammatory and pro-coagulant states capable of negatively influencing the patient’s clinical course [27, 28]. Similar to SARS-CoV, SARS-CoV-2 enters cells through a receptor widely spread in multiple cells, namely in endocrine pancreatic beta cells, which may cause direct damage to them, contributing to the worsening of blood glucose in these patients or even new-onset diabetes [6, 27, 29]. Several cases have been reported of individuals without previous diagnosis of diabetes who develop new-onset diabetes with an acute hyperglycemic crisis such as diabetic ketoacidosis during the acute or recovery phase of SARS-CoV-2 infection. That points to a potential direct cytotoxic effect and insulin secretion impairment of this virus [30, 31].
Given the potential deleterious effect of hyperglycemia on the clinical course of patients hospitalized with COVID-19, it makes sense to optimize the glycemic control of these patients, even in those without a known history of diabetes. An Italian study showed that hyperglycemic patients treated with insulin infusion during hospitalization for moderate COVID-19 had a lower risk of severe disease than those who did not receive this treatment [32]. In patients with at-admission hyperglycemia in this study population, the median at-admission blood glucose was 191 mg/dL with an interquartile range of 159–227.5 mg/dL. These patients would meet criteria for glycemic control with insulin therapy according to some reports [33]. Maybe the results observed would be different if an internal protocol of hyperglycemia management in patients with COVID-19 had been developed. Other authors have investigated the effects of novel antidiabetic therapies on glycemic control in patients with type 2 diabetes and COVID-19, showing that most of these novel agents have a beneficial effects on COVID-19 outcomes [34], such as glucagon-like peptide 1 receptor agonists, for which a molecular mechanism of direct interaction with SARS-CoV-2 activity has been postulated [35].
We also wish to clearly state that present study has some limitations, as the vast majority of the investigations were performed on patients with COVID-19 during the first months of the pandemic. This is a retrospective and observational study, which makes it dependent on the information obtained through the analysis of the patients’ clinical records. The study does not consider the conditions under which the at-admission blood glucose was assessed, namely whether the sample collection was performed in a fasted state or whether it corresponded to an occasional measurement. It was also not possible to determine whether the patient was undergoing fluid therapy with glucose supply at the time of sample collection, which could have influenced the results. The diagnosis of previous diabetes was based on the patients’ clinical history and self-report of this diagnosis, which may have led to under-detection for those cases. The patients’ concomitant comorbidities, often present along with diabetes such as arterial hypertension or cardiovascular disease, seem to influence the clinical course of COVID-19 [6] and were not considered in this study. Data may be missing, namely the concomitant measurement of blood glucose at admission and glycated hemoglobin that allows the calculation of SHR. To make this clear, it was decided not to exclude any patient from the presentation of the results. The sample in which this was possible to calculate is small, and care must be taken when extrapolating the results to other realities. Despite its limitations, our study reinforces the impact that lack of glycemic control may have on the clinical severity of COVID-19.
Conclusions
Our results are in accordance with the literature regarding the impact of absolute hyperglycemia on severity outcomes. In addition, we are reporting novel data that SHR is not a marker of severity for clinical outcomes in those patients. All the learnings on diabetes and COVID-19 pandemic are of particular importance, since insights from recent experience are essential to guide future management [36]. We therefore suggest that SHR should not be evaluated in all patients admitted in the hospital for COVID-19, and we encourage the standard measurement at-admission of blood glucose and HbA1c levels.
References
Guan WJ, Ni ZY, Hou Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2019;382:1708–20. https://doi.org/10.1056/NEJMoa2002032.
WHO Coronavirus Disease (COVID-19) Dashboard. Available online: http://covid19.who.int/coronavirus/world_dashboard. Accessed 19 Feb 2021.
Ceriello A, Stoian AP, Rizzo M. COVID-19 and diabetes management: what should be considered? Diabetes Res Clin Pract. 2020;163: 108151.
Stoian AP, Kempler P, Stulnig T, et al. Diabetes and COVID-19: what 2 years of the pandemic has taught us. Metab Syndr Relat Disord. 2021. https://doi.org/10.1089/met.2021.0133 (Online ahead of print).
Shi Q, Zhang X, Jiang F, et al. Clinical characteristics and risk factors for mortality of COVID-19 patients with diabetes in Wuhan, China: a two-center, retrospective study. Diabetes Care. 2020;43:1382–91.
Apicella M, Campopiano MC, Mantuano M, Mazoni L, Coppelli A, Del Prato S. COVID-19 in people with diabetes: understanding the reasons for worse outcomes [published correction appears in Lancet Diabetes Endocrinol. 2020 Oct;8(10):e5] [published correction appears in Lancet Diabetes Endocrinol. 2020 Nov;8(11):e6]. Lancet Diabetes Endocrinol. 2020;2020(8):782–92.
Zhang Y, Li H, Zhang J, et al. The clinical characteristics and outcomes of patients with diabetes and secondary hyperglycaemia with coronavirus disease 2019: a single-centre, retrospective, observational study in Wuhan. Diabetes Obes Metab. 2020;22:1443–54.
Cariou B, Hadjadj S, Wargny M, et al. Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: the CORONADO study [published correction appears in Diabetologia. 2020 Jul 2;:]. Diabetologia. 2020;63:1500–15.
Dungan KM, Braithwaite SS, Preiser JC. Stress hyperglycaemia. Lancet. 2009;373:1798–807.
Roberts GW, Quinn SJ, Valentine N, et al. Relative hyperglycemia, a marker of critical illness: introducing the stress hyperglycemia ratio. J Clin Endocrinol Metab. 2015;100:4490–7.
Direção-Geral da Saúde. COVID-19: Abordagem do Doente com Suspeita ou Confirmação de COVID-19. Norma nº 004/2020 de 23/03/2020 atualizada a 14/10/2020. 2020.
American Diabetes Association. 15. Diabetes care in the hospital: standards of medical care in diabetes-2020. Diabetes Care. 2020;43(Suppl 1):S193–202.
Godinho C, Jordão A, Dias A, Lopes A, Duarte A, Carvalho D et al. Recomendações Conjuntas da Sociedade Portuguesa de Diabetologia SPD)/Sociedade Portuguesa de Medicina Interna (SPMI) sobre a Abordagem e Tratamento da Hiperglicemia em Internamento (não Crítico). Supl Rev Soc Med Interna. 2015; 22.
Nathan DM, Kuenen J, Borg R, Zheng H, Schoenfeld D, Heine RJ, Group, A1c-Derived Average Glucose Study. Translating the A1C assay into estimated average glucose values. Diabetes Care. 2008;31:1473–8.
Di Luzio R, Dusi R, Mazzotti A, Petroni ML, Marchesini G, Bianchi G. Stress hyperglycemia and complications following traumatic injuries in individuals with/without diabetes: the case of orthopedic surgery. Diabetes Metab Syndr Obes. 2020;13:9–17.
Sociedade Portuguesa de Diabetologia. Diabetes: Factos e Números - O ano de 2016, 2017 e 2018 - Relatório Anual do Observatório Nacional de Diabetes. 2019.
Guan WJ, Liang WH, Zhao Y, et al. Comorbidity and its impact on 1590 patients with Covid-19 in China: a nationwide analysis. Eur Respir J. 2020; 55.
Pugliese G, Vitale M, Resi V, Orsi E. Is diabetes mellitus a risk factor for COronaVIrus Disease 19 (COVID-19)? Acta Diabetol. 2020;57:1275–85.
Al Mahmeed W, Al-Rasadi K, Banerjee Y, CArdiometabolic Panel of International experts on Syndemic COvid-19 (CAPISCO), et al. Promoting a syndemic approach for cardiometabolic disease management during COVID-19: the CAPISCO International Expert Panel. Front Cardiovasc Med. 2021;8:787761.
Grasselli G, Zangrillo A, Zanella A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323:1574–81.
Pantea Stoian A, Pricop-Jeckstadt M, Pana A, et al. Death by SARS-CoV 2: a Romanian COVID-19 multi-centre comorbidity study. Sci Rep. 2020;10:21613.
Rizzo M, Foresti L, Montano N. Comparison of reported deaths from COVID-19 and increase in total mortality in Italy. JAMA Intern Med. 2020;180:1250–2.
Fadini GP, Morieri ML, Boscari F, et al. Newly-diagnosed diabetes and admission hyperglycemia predict COVID-19 severity by aggravating respiratory deterioration. Diabetes Res Clin Pract. 2020;168:108374.
Bode B, Garrett V, Messler J, et al. Glycemic characteristics and clinical outcomes of COVID-19 patients hospitalized in the United States [published correction appears in J Diabetes Sci Technol. 2020 Jun 10;:1932296820932678]. Diabetes Sci Technol. 2020;14:813–21.
Davis G, Fayfman M, Reyes-Umpierrez D, et al. Stress hyperglycemia in general surgery: why should we care? J Diabetes Complications. 2018;32:305–9.
Yang CJ, Liao WI, Tang ZC, et al. Glycated hemoglobin A1c-based adjusted glycemic variables in patients with diabetes presenting with acute exacerbation of chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2017;12:1923–32.
Hussain A, Bhowmik B, do Vale Moreira NC. COVID-19 and diabetes: Knowledge in progress. Diabetes Res Clin Pract. 2020; 162.
Anca PS, Toth PP, Kempler P, et al. Gender differences in the battle against COVID-19: impact of genetics, comorbidities, inflammation and lifestyle on differences in outcomes. Int J Clin Pract. 2021;75: e13666.
Agarwal S, Agarwal SK. Endocrine changes in SARS-CoV-2 patients and lessons from SARS-CoV. Postgrad Med J. 2020;96:412–6.
Eskandarani RM, Sawan S. Diabetic ketoacidosis on hospitalization with COVID-19 in a previously nondiabetic patient: a review of pathophysiology. Clin Med Insights Endocrinol Diabetes. 2020; 13.
Siddiqui RS, Zirkiyeva M, Saliaj M. Onset of ketosis-prone diabetes in the setting of COVID-19 infection. Cureus. 2020; 12.
Sardu C, D’Onofrio N, Balestrieri ML, et al. Outcomes in patients with hyperglycemia affected by COVID-19: can we do more on glycemic control? Diabetes Care. 2020;43:1408–15.
Bellido V, Pérez A. Inpatient hyperglycemia management and COVID-19. Diabetes Ther. 2021;12:121–32.
Popovic DS, Papanas N, Pantea Stoian A, et al. Use of novel antidiabetic agents in patients with type 2 diabetes and COVID-19: a critical review. Diabetes Ther. 2021;12:3037–54.
Banerjee Y, Pantea Stoian A, Silva-Nunes J, Sonmez A, Rizvi AA, Janez A, Rizzo M. The role of GLP-1 receptor agonists during COVID-19 pandemia: a hypothetical molecular mechanism. Expert Opin Drug Saf. 2021;20:1309–15.
Stoian AP, Banerjee Y, Rizvi AA, et al. Diabetes and the COVID-19 pandemic: how insights from recent experience might guide future management. Metab Syndr Relat Disord. 2020;18:173–5.
Acknowledgements
Funding
This research received no external funding.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Conceptualization, AM, IM and TS; Methodology, AM; Software, AM and TS; Formal analysis, AM and IM; Investigation, AM, IM and TS; Data curation, AM, IM and TS; Writing— original draft preparation, AM and IM; Writing—review and editing, TS, TR, CM, AP, MR and JSN; Visualization, AM and IM.
Disclosures
Teresa Rego is currently a medical doctor in Hospital Divino Espírito Santo, Ponta Delgada, Azores, Portugal. Alexandra A. Matias, Inês Manique, Teresa Sabino, Claudia Mihon, António Panarra, Manfredi Rizzo and José Silva-Nunes have nothing else to disclose.
Compliance with Ethics Guidelines
This study has a retrospective and observational nature which had no impact on the diagnosis or treatment of those involved. The article was approved for publication by the Health Ethics Committee of Centro Hospitalar Universitário Lisboa Central (CES 1226/2022). Patient consent was waived since the data were pseudo-anonymized, collected from an electronic record consultation, with an observational and retrospective character and subsequently destroyed. The need for informed consent was waived by the Health Ethics Committee of Centro Hospitalar Universitário Lisboa Central (CES 1226/2022).
Data Availability
The datasets generated during and/or analysed during the current study are not publicly available due to privacy restrictions.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Matias, A.A., Manique, I., Sabino, T. et al. Absolute Hyperglycemia versus Stress Hyperglycemia Ratio for the Prognosis of Hospitalized Patients with COVID-19 in the First Months of the Pandemic: A Retrospective Study. Diabetes Ther 14, 335–346 (2023). https://doi.org/10.1007/s13300-022-01347-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-022-01347-4