Abstract
Introduction
The objective of this analysis was to estimate the costs associated with using flash glucose monitoring with optional alarms as a replacement for either traditional continuous glucose monitoring (CGM) or routine self-monitoring of blood glucose (SMBG) in adults with diabetes and impaired awareness of hypoglycaemia (IAH) who use intensified insulin therapy, from a Swedish payer perspective, applying assumptions to simulate hypothetical scenarios.
Methods
A simple two-state cohort Markov model was used to calculate the cost per patient treated over a 3-year period, capturing the risk of severe hypoglycaemic events requiring medical assistance and non-adherence using quarterly Markov cycles. The costs considered were those for glucose monitoring and resource use to treat severe hypoglycaemic events. Cost inputs were sourced from Swedish price lists, manufacturer data and resource use reported in the control arm of the HypoDE study. Targeted literature searches were run in PubMed to source the clinical inputs. Uncertainty in the model was considered through one-way sensitivity analysis and scenario analysis.
Results
Over 3 years, flash monitoring with optional alarms resulted in potential cost-savings of Swedish krona (SEK) 7708 and SEK 69,908 per patient when compared to routine SMBG or CGM respectively. Sensitivity and scenario analyses were largely supportive of this conclusion with respect to SMBG, and large cost-savings were consistent across all sensitivity and scenario analyses with respect to CGM.
Conclusion
Utilizing flash monitoring with optional alarms is potentially a cost-saving treatment strategy compared to routine SMBG or traditional CGM in adults with diabetes using intensive insulin and IAH from a Swedish payer perspective. Future studies in the IAH population will help to assess more precisely the relative cost impact of flash glucose monitoring with optional alarms compared with SMBG and traditional CGM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
The aim of this study was to assess the costs of glucose monitoring in Swedish adults with diabetes and impaired awareness of hypoglycaemia (IAH) who use intensive insulin therapy, based on flash monitoring with optional alarms as a replacement for either traditional continuous glucose monitoring (CGM) or routine self-monitoring of blood glucose (SMBG). |
Assumptions were applied to simulate a hypothetical scenario. |
What was learned from the study? |
Over 3 years, flash monitoring with optional alarms resulted in potential cost-savings of Swedish krona (SEK) 7708 and of SEK 69,908 per patient when compared with routine SMBG or traditional CGM, respectively. |
From a Swedish payer perspective, utilizing flash monitoring with optional alarms is potentially a cost-saving treatment strategy compared with routine SMBG or traditional CGM in adults with diabetes and IAH on intensive insulin regimes. |
Digital Features
This article is published with digital features, including a summary slide, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.14762142.
Introduction
Impaired awareness of hypoglycaemia (IAH) refers to the absence or diminished ability to perceive the onset of hypoglycaemia amongst diabetes patients [1]. IAH caused by recurrent, untreated and non-severe hypoglycaemic events results in patients being less aware and less able to respond to onset hypoglycaemia, putting them at higher risk of suffering severe hypoglycaemic events [1]. Prevalence estimates of IAH range between 20 and 32% in adults with insulin-treated type 1 diabetes mellitus (T1DM) [1,2,3] and 10% in adults with insulin-treated type 2 diabetes mellitus (T2DM) [4] and increases with age and duration of diabetes [3].
People with IAH are disproportionally high healthcare users due to a sixfold increase in the risk of severe hypoglycaemia [5]. In addition to the high cost burden, hypoglycaemia is associated with worse quality of life, increased anxiety and reduced productivity [6,7,8]. Maintaining glucose levels within a recommended range reduces the risk of developing hypoglycaemia associated with an intensified insulin regimen. The Tandvårds-Läkemedelförmånsverket (TLV), a national health authority in Sweden, recommends that adults with insulin-treated diabetes test at least four and up to ten times per day [9]; however, it also recognises that adherence is poor as finger-prick testing can be both time consuming, painful and inconvenient.
Traditional continuous glucose monitoring (CGM) is currently funded under the Swedish national health service, and adults with IAH are prioritised for reimbursement [10]. CGM automatically tracks glucose in interstitial fluid and is typically used in combination with occasional self-monitoring of blood glucose (SMBG). A useful feature of CGM devices is the inclusion of alarms to notify patients when their glucose is outside of a pre-defined range. These alarms facilitate improved glycaemic control by allowing patients or their caregivers to monitor and respond to changes. Two recent randomised controlled trials (RCTs) [11, 12] compared CGM to routine SMBG in patients with IAH; both trials reported significant differences in the number of patients experiencing severe hypoglycaemic events, with the results in favour of CGM. While CGM has been demonstrated to be effective in improving glycaemic control [13,14,15], patient adherence is variable. Of 1662 participants reporting CGM use at time of enrolment into the T1DM Exchange Registry, 675 (41%) reported discontinuing CGM use at the 1-year data collection. Alarm fatigue has been reported is one of the main contributors to non-adherence [16, 17].
The FreeStyle Libre™ 2 system (Abbott Diabetes Care, Witney, UK) is the same as the original flash glucose monitoring system, the FreeStyle Libre™ system, with the exception that it features optional real-time glucose alarms. Both systems continuously measure glucose levels in patients’ interstitial fluid and wirelessly transfer data by scanning from a sensor to a handheld reader (or smartphone). In addition, the FreeStyle Libre™ 2 system is continuously transferring the data from the sensor to the reading device, which allows alarms to be issued automatically by the minute. The systems are factory calibrated and do not require calibration using SMBG.
The clinical benefits of flash glucose monitoring in comparison to routine SMBG have been demonstrated in two RCTs in people with T1DM [18] and T2DM [19], using an intensified insulin regimen. In real-world studies, flash monitoring has shown reductions from baseline in haemoglobin A1c (HbA1c) [20] and hypoglycaemia [21]. The economic case for flash glucose monitoring has also been demonstrated in published economic analyses [22,23,24,25]. A key differentiator of the newer model of flash glucose monitoring is that the optional alarms empower patients by providing a choice about how they want to use the alarms. The efficacy of flash monitoring with optional alarms for people with diabetes and IAH who are using an intensified insulin regimen is expected to be similar to that of CGM. This assumption is appropriate because both technologies are similar, to the extent that in some countries, such as Germany, flash monitoring with optional alarms is listed by payers as a CGM device. In addition, the US Food and Drug Administration (FDA) defines flash monitoring with optional alarms in the same category as CGM [26]. Although there are differences between the alarm features for flash monitoring with optional alarms and CGM, there is no reliable evidence to demonstrate improved clinical outcomes based on alarms, which is also consistent with the assumption of a similar efficacy of these systems.
The objective of this analysis was to estimate the potential costs associated with using flash glucose monitoring with optional alarms compared with either traditional CGM or routine SMBG. In the absence of direct evidence for flash monitoring with optional alarms, a set of clinical and resource-based assumptions are applied. The analysis focused on adults with diabetes and IAH who use an intensified insulin regimen, from a Swedish payer perspective.
This study involves a cost analysis and did not involve any studies with human or animal subjects performed by any of the authors; hence there was no requirement to seek ethics committee approval.
Methods
Base Case Scenario
The analysis calculates the cost per patient treated over a 3-year period, applying a set of clinical and resource use assumptions to simulate a hypothetical base case scenario. Flash monitoring with optional alarms was compared to two alternatives: routine SMBG or traditional CGM, based on the DexCom G6 CGM system (DexCom Inc., San Diego, CA, USA). Costs were estimated from a Swedish national health service payer perspective and are reported in 2018 Swedish krona (SEK). The costs considered in the model include glucose monitoring costs and resource use to treat severe hypoglycaemic events.
Model Overview
A simple two-state cohort Markov model was built in Microsoft Excel® in Office 365® (Microsoft Corp., Redmond, WA, USA). It was constructed to account for risk of severe hypoglycaemic events requiring medical assistance and non-adherence over a 3-year time horizon using quarterly Markov cycles (Fig. 1).
In the flash monitoring with optional alarms and CGM arms, patients enter the first health state where they use flash monitoring with optional alarms or CGM respectively, with occasional SMBG. Patients may discontinue flash monitoring with optional alarms or CGM due to non-compliance and move to a state where they are on routine SMBG. In both states, patients may experience severe hypoglycaemic events for which they accrue the medical costs associated with the event. In the routine SMBG arm, the model consists of only one state in which the patient may experience severe hypoglycaemic events.
Model Inputs
The cost inputs, reported in Table 1, were sourced from Swedish price lists, manufacturer data and resource use reported in the control arm of the HypoDE study [12], an RCT that compared CGM to routine SMBG in a population predominantly of people with IAH. The unit cost for a physician visit was sourced from a prior Swedish cost-effectiveness study [24]. The cost of a severe hypoglycaemic event was calculated using inflated unit costs reported in Jonsson et al. [27] and the resource use reported in Heller et al. [28]. For the purposes of this study, a severe hypoglycaemic event is one that requires third party medical assistance (SHE2), including ambulance call outs, emergency room visits and/or hospital admissions. (Further details of the approach to calculating severe hypoglycaemic costs are provided in the Electronic Supplementary Material [ESM]).
The HypoDE study cohort, consisting of 149 patients with T1DM, was used as the reference for clinical outcomes. The rationale for using this study as the reference was that at entry 94% of the cohort had a hypoglycaemia unawareness score of ≥ 4 (Clarke questionnaire) and 62% had reported at least one severe hypoglycaemia event within the past 12 months. The mean age of the study cohort was 46.6 years, mean duration of diabetes was 21.3 years and 60% were male. Mean HbA1c at entry was 7.5%, and ≥ 90% were using insulin analogues for basal and prandial insulin requirements. The model cohort was not stratified by T1DM or T2DM status because evidence suggests the level of unmet need for people using MDI therapy who have IAH is likely to be significant regardless of whether they have T1DM or T2DM, including their need for effective glucose monitoring [4, 29].
Targeted literature searches were run in PubMed to source the clinical inputs referenced in Table 2. The baseline risk for severe hypoglycaemic events was also sourced from Heller et al. [28]. This rate was adjusted to account for a threefold higher rate of severe hypoglycaemia reported in real-world settings compared to clinical trials [30]. A further adjustment was applied to account for higher rates of severe hypoglycaemia amongst intensified insulin regimen users with IAH compared with those without IAH [5].
Efficacy data for both flash glucose monitoring with alarms and CGM was sourced from Heinemann et al. [12], using the rate ratio of all SHE2s. Treatment discontinuation was modelled using the proportion of patients (23.4%) who discontinued using CGM in a real-world study after 1 year [31]. No further discontinuation is assumed beyond year 1. In the base case the discontinuation rate is assumed to be the same for CGM and flash monitoring with alarms because no flash monitoring with alarms specific data are available. (Further details of the selection rationale and adjustments applied to all clinical inputs are provided in the ESM).
One-Way Sensitivity Analysis
One-way sensitivity analysis was conducted by varying all inputs individually within lower and upper bounds and ranking the results in order of impact. High and low values were selected using a 95% confidence interval where this was provided in the literature, or by varying the input by 50% or to extreme values where there was high uncertainty and to 25% where there was moderate uncertainty. The inputs for the analysis comparing flash glucose monitoring with alarms to routine SMBG and CGM are reported in Tables 3 and 4, respectively.
Scenario Analyses
The rate of severe hypoglycaemic events in IAH populations is uncertain as few studies have been conducted in IAH populations. Furthermore, clinical trials tend to underestimate the risk of severe hypoglycaemic events due to their strict inclusion criteria that might disproportionately exclude those at greatest risk. The rate of severe hypoglycaemic events applied in our model was calculated using data from an RCT [28] in a T1DM diabetes population and applying an adjustment for a real-world setting and an IAH population. To account for uncertainty between these adjustments, the IAH rate ratio, the combined adjustment for real-world setting and IAH population, was varied while keeping all other model inputs constant.
A second scenario analysis considers the impact if adherence to flash glucose monitoring with optional alarms is higher than adherence to CGM. In the base case a conservative assumption was applied, assuming that adherence was equal; however, flash monitoring with optional alarms is potentially more engaging for users than CGM as the notification feature is more flexible.
Results
Base Case
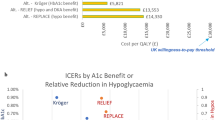
The base case results over a 3-year time horizon are shown in Fig. 2. Over 3 years, a patient using flash glucose monitoring with optional alarms is expected to realise cost-savings of SEK 7708 when compared to a patient using routine SMBG and SEK 69,908 when compared to a patient using CGM.
In comparison to CGM, the savings accrued by using flash monitoring with optional alarms are largely due to differences in the sensor cost, the fact that there is no need for a transmitter and a lower reader cost (Fig. 2; Table 5). In contrast, the cost-savings when compared to routine SMBG are due to severe hypoglycaemic events avoided because the aggregate cost of treating severe hypoglycaemic events is around 50% lower.
Sensitivity Analysis
The results of the one-way sensitivity analysis comparing flash glucose monitoring with optional alarms with routine SMBG are illustrated in a tornado plot in Fig. 3, which ranks the parameters in order of effect. The model is most sensitive to the severe hypoglycaemic event parameters. Changing the intervention incidence rate ratio, the rate ratio to account for IAH or the base line severe hypoglycaemic event rate to their respective upper and lower bounds can cause the model results to shift over the cost-saving threshold or become even more cost saving than the base case.
The results of the one-way sensitivity analysis projecting the cost saving of flash glucose monitoring with optional alarms compared to CGM after 3 years are illustrated in Fig. 4. The analysis is seen to be most sensitive to the unit cost of the CGM sensor and the intervention rate ratio for flash glucose monitoring with optional alarms respectively. However, in all scenarios the cost per patient using flash monitoring with optional alarms is substantially lower than that with CGM.
Scenario Analyses
The results of the scenario analysis on varying the IAH rate ratio are reported in Table 6. These results show that flash glucose monitoring with optional alarms is cost-saving compared to SMBG when the IAH severe hypoglycaemic event rate ratio is > 12.72. Flash monitoring with optional alarms is cost-neutral when the IAH ratio is 12.72. The cost-savings compared to CGM do not change when this rate is varied as the effect of CGM on severe hypoglycaemic events is the same for both flash monitoring with optional alarms and CGM.
The results of the scenario analysis varying adherence to flash glucose monitoring with optional alarms are reported in Table 7. These results show that the model is not particularly sensitive to this input. Flash monitoring with optional alarms is cost-saving compared to CGM or routine SMGB in all variations of adherence to flash monitoring with alarms considered. The relationship between this variable and difference in cost is not linear because higher adherence is associated with both higher consumable costs as well as cost-savings from severe hypoglycaemic events avoided.
Discussion
The base case analysis presented here suggests that the higher acquisition cost of flash glucose monitoring with optional alarms compared to routine SMBG is offset by cost-savings from avoiding severe hypoglycaemic events. In addition to costs avoided, reducing the risk of severe hypoglycaemic events has additional health benefits not captured in the model; these include avoiding detriments to patient’s quality of life associated with severe hypoglycaemic events [33] and reducing risk of further complications or death [34]. The sensitivity and scenario analyses found some uncertainty regarding this conclusion, where the result was particularly sensitive to varying the severe hypoglycaemic event parameters, most notably the intervention rate ratio. Nonetheless, the IN CONTROL trial [11] showed a similar reduction as the Hypo-DE study in the rate of severe hypoglycaemia in a population of people with IAH. Applying the intervention rate ratio observed in the Hypo-DE study in our base case analysis is therefore considered to be reliable.
The comparison with CGM suggests that flash monitoring with optional alarms dominates CGM because the acquisition costs are substantially lower and both treatment strategies may provide similar efficacy. This conclusion, namely that cost-savings are associated with switching from CGM to flash monitoring with optional alarms, was consistent across the sensitivity and scenario analyses.
Glucose monitoring is particularly important in people with diabetes and IAH who are using an intensified insulin regimen due to the increased risk of severe hypoglycaemic events. Managing complications with diabetes imposes a high cost burden on healthcare services in Sweden, with the cost of treating hypoglycaemia projected to be SEK 34 million in 2020 [35]. We believe the conclusions of this analysis will be transferable to many countries in Europe and outside Europe that have relatively similar cost structures to Sweden. The precise results for the population with IAH will differ from country to country and will depend especially on the local cost of treating severe hypoglycaemia.
A limitation of this analysis is the lack of direct data on the use of flash glucose monitoring with optional alarms in the IAH population, compared with CGM or SMBG. In the absence of real-world data, this analysis assumes that similar to CGMs, [11, 12], flash monitoring with optional alarms improves glycaemic control in IAH populations and that patients with IAH, irrespective of whether they have T1DM or T2DM, are sixfold more likely to be admitted for severe hypoglycaemia compared to those with normal glycaemic awareness. These assumptions draw on results reported in prior studies in IAH populations where a UK-based survey reported a sixfold increase in the risk of severe hypoglycaemia compared to those with normal awareness [1] and an Australian study reported rates of severe hypoglycaemia over a 6-month period of 1.4 ± 3.9 in an IAH population compared to 0.3 ± 1.0 in those with normal awareness [3]. Nonetheless, further real-world studies are required to verify the assumptions applied in this hypothetical scenario.
Two RCTs in populations using an intensified insulin regimen [18, 19] demonstrate high scanning rates linked to flash glucose monitoring, and real-world evidence confirms that frequent glucose checks with high rates of scanning are maintained when used as regular, daily diabetes management [21]. This observation is expected to be transferrable to an IAH population. Frequent testing is recommended in clinical guidelines [9] for effective diabetes management because real-world studies [36] demonstrate that frequent testing is associated with more effective management of both HbA1c levels and reduced risk of hypoglycaemia with intensified insulin regimen use. This benefit is expected to be particularly pertinent to IAH populations who are using an intensified insulin regimen given their higher susceptibility to hypoglycaemia.
A further benefit of flash monitoring with optional alarms over routine SMBG is the additional information captured, making this monitoring strategy more compliant with current international consensus for good practice. Each scan provides more information than a single glucose reading from an SMBG test, and flash monitoring with optional alarms can provide a summary ambulatory glucose profile (AGP) and a complete 24-h glucose record. A recent international consensus statement endorsed by European Association for the Study of Diabetes (EASD), American Diabetes Association (ADA), American Association of Clinical Endocrinologists (AACE), American Association of Diabetes Educators (AADE) and International Society for Pediatric and Adolescent Diabetes (ISPAD) [37] recognizes the importance of time in glucose ranges (TIR) as “appropriate and useful as clinical targets and outcome measurements”. The flash monitoring system with optional alarms provides TIR in the AGP report, in contrast with SMBG which does not easily facilitate capturing this metric.
An economic evaluation has been reported [38] based on people with T1DM and IAH for a population in North West London, comparing CGM with SMBG. This evaluation assumed a clinical benefit from CGM based on a concurrent reduction in severe hypoglycaemia (59%) and a reduction in HbA1c (0.6%) compared with SMBG. However, these effects were not observed in the same study, and it is unclear whether differences of this magnitude would be observed together in a single population. The acquisition cost of flash glucose monitoring with optional alarms is less than that of CGM; accordingly, we believe the budget impact of flash glucose monitoring with optional alarms will be less than that of CGM. We also believe the model described here is more reliable than the one for North West London because it is based on clinical outcomes from a single study.
Conclusion
This assumption-based cost analysis estimates the difference in cost per patient per year over 3 years, comparing flash glucose monitoring with optional alarms to routine SMBG and traditional CGM in T1/T2DM populations with IAH, from a Swedish payer perspective. In the scenarios hypothesised, flash monitoring with optional alarms was found to be cost-saving compared to both alternative strategies. After 3 years, flash monitoring with optional alarms is expected to result in cost-savings of SEK 7708 and of SEK 69,908 when compared to routine SMBG or traditional CGM respectively.
Future studies in the IAH population will help to assess more precisely the relative cost impact of flash glucose monitoring with optional alarms compared with SMBG and traditional CGM.
References
Geddes J, Schopman JE, Zammitt NN, Frier BM. Prevalence of impaired awareness of hypoglycaemia in adults with type 1 diabetes. Diabet Med. 2008;25(4):501–4.
Choudhary P, Geddes J, Freeman JV, Emery CJ, Heller SR, Frier BM. Frequency of biochemical hypoglycaemia in adults with type 1 diabetes with and without impaired awareness of hypoglycaemia: no identifiable differences using continuous glucose monitoring. Diabet Med. 2010;27(6):666–72.
Hendrieckx C, Hagger V, Jenkins A, Skinner TC, Pouwer F, Speight J. Severe hypoglycemia, impaired awareness of hypoglycemia, and self-monitoring in adults with type 1 diabetes: results from Diabetes MILES—Australia. J Diabet Complic. 2017;31(3):577–82.
Schopman JE, Geddes J, Frier BM. Prevalence of impaired awareness of hypoglycaemia and frequency of hypoglycaemia in insulin-treated type 2 diabetes. Diabetes Res Clin Pract. 2010;87(1):64–8.
Gold AE, Macleod KM, Frier BM. Frequency of severe hypoglycemia in patients with type I diabetes with impaired awareness of hypoglycemia. Diabetes Care. 1994;17(7):697–703.
Wild D, von Maltzahn R, Brohan E, et al. A critical review of the literature on fear of hypoglycemia in diabetes: implications for diabetes management and patient education. Patient Educ Couns. 2007;68(1):10–5.
Anderbro T, Gonder-Frederick L, Bolinder J, et al. Fear of hypoglycemia: relationship to hypoglycemic risk and psychological factors. Acta Diabetol. 2015;52(3):581–9.
Brod M, Christensen T, Thomsen TL, Bushnell DM. The impact of non-severe hypoglycemic events on work productivity and diabetes management. Value in Health. 2011;14(5):665–71.
The Dental and Pharmaceutical Benefits Agency (Tandvårds-Läkemedelförmånsverket). TLV Health technology assessment report in support of county council decision-making: FreeStyle Libre; 2017. https://www.tlv.se/download/18.3322d85a162195ccf87a8293/1521729251535/bes171117_underlag_freedstyle_libre_eng.pdf. Accessed 24 June 2021.
The Dental and Pharmaceutical Benefits Agency (Tandvårds-Läkemedelförmånsverket). Underlag för beslut i landstingen MiniMed 670G; 2018. https://www.tlv.se/medicinteknik/halsoekonomiska-bedomningar/avslutade-bedomningar/arkiv/2018-10-05-halsoekonomisk-utvardering-av-minimed-670g.html. Accessed 24 June 2021
van Beers CA, DeVries JH, Kleijer SJ, et al. Continuous glucose monitoring for patients with type 1 diabetes and impaired awareness of hypoglycaemia (IN CONTROL): a randomised, open-label, crossover trial. Lancet Diabetes Endocrinol. 2016;4(11):893–902.
Heinemann L, Freckmann G, Ehrmann D, et al. Real-time continuous glucose monitoring in adults with type 1 diabetes and impaired hypoglycaemia awareness or severe hypoglycaemia treated with multiple daily insulin injections (HypoDE): a multicentre, randomised controlled trial. Lancet. 2018;391(10128):1367–77.
Beck RW, Riddlesworth TD, Ruedy K, et al. Continuous glucose monitoring versus usual care in patients with type 2 diabetes receiving multiple daily insulin injections: a randomized trial. Ann Intern Med. 2017;167(6):365–74.
Beck RW, Riddlesworth T, Ruedy K, et al. Effect of continuous glucose monitoring on glycemic control in adults with type 1 diabetes using insulin injections: the DIAMOND randomized clinical trial. JAMA. 2017;317(4):371–8.
Lind M, Polonsky W, Hirsch IB, Heise T, Bolinder J, Dahlqvist S, et al. Continuous glucose monitoring vs conventional therapy for glycemic control in adults with type 1 diabetes treated with multiple daily insulin injections: the GOLD randomized clinical trial. JAMA. 2017;317(4):379–87.
Roberts R, Walsh J, Heinemann L. Help! Someone is beeping. J Diabetes Sci Technol. 2014;8(4):627–9.
Shivers JP, Mackowiak L, Anhalt H, Zisser H. “Turn it off!”: diabetes device alarm fatigue considerations for the present and the future. J Diabetes Sci Technol. 2013;7(3):789–94.
Bolinder J, Antuna R, Geelhoed-Duijvestijn P, Kröger J, Weitgasser R. Novel glucose-sensing technology and hypoglycaemia in type 1 diabetes: a multicentre, non-masked, randomised controlled trial. Lancet. 2016;388(10057):2254–63.
Haak T, Hanaire H, Ajjan R, Hermanns N, Riveline J-P, Rayman G. Flash glucose-sensing technology as a replacement for blood glucose monitoring for the management of insulin-treated type 2 diabetes: a multicenter, open-label randomized controlled trial. Diabetes Ther. 2017;8(1):55–73.
Evans M, Welsh Z, Ells S, Seibold A. The impact of flash glucose monitoring on glycaemic control as measured by HbA1c: a meta-analysis of clinical trials and real-world observational studies. Diabetes Ther. 2019;11(1):1–13.
Dunn TC, Xu Y, Hayter G, Ajjan RA. Real-world flash glucose monitoring patterns and associations between self-monitoring frequency and glycaemic measures: a European analysis of over 60 million glucose tests. Diabetes Res Clin Pract. 2018;137:37–46.
Hellmund R, Weitgasser R, Blissett D. Cost calculation for a flash glucose monitoring system for UK adults with type 1 diabetes mellitus receiving intensive insulin treatment. Diabetes Res Clin Pract. 2018;138:193–200.
Hellmund R, Weitgasser R, Blissett D. Cost calculation for a flash glucose monitoring system for adults with type 2 diabetes mellitus using intensive insulin–a UK perspective. Eur Endocrinol. 2018;14(2):86.
Bilir SP, Hellmund R, Wehler E, Li H, Munakata J, Lamotte M. The cost-effectiveness of a flash glucose monitoring system for management of patients with type 2 diabetes receiving intensive insulin treatment in Sweden. Eur Endocrinol. 2018;14(2):80.
Bilir SP, Hellmund R, Wehler B, Li H, Munakata J, Lamotte M. Cost-effectiveness analysis of a flash glucose monitoring system for patients with type 1 diabetes receiving intensive insulin treatment in Sweden. Eur Endocrinol. 2018;14(2):73.
US Food and Drug Administration. Premarket notification: integrated continuous glucose monitoring system, factory calibrated, not for use with automated insulin delivery systems. https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpmn/pmn.cfm?ID=K193371. Accessed 24 June 2021
Jönsson L, Bolinder B, Lundkvist J. Cost of hypoglycemia in patients with type 2 diabetes in Sweden. Value Health. 2006;9(3):193–8.
Heller S, Frier B, Hersløv M, Gundgaard J, Gough S. Severe hypoglycaemia in adults with insulin-treated diabetes: impact on healthcare resources. Diabet Med. 2016;33(4):471–7.
Martín-Timón I, del Cañizo-Gómez FJ. Mechanisms of hypoglycemia unawareness and implications in diabetic patients. World J Diabetes. 2015;6(7):912–26.
Elliott L, Fidler C, Ditchfield A, Stissing T. Hypoglycemia event rates: a comparison between real-world data and randomized controlled trial populations in insulin-treated diabetes. Diabetes Ther. 2016;7(1):45–60.
Battelino T, Liabat S, Veeze H, Castaneda J, Arrieta A, Cohen O. Routine use of continuous glucose monitoring in 10 501 people with diabetes mellitus. Diabet Med. 2015;32(12):1568–74.
Leese GP, Wang J, Broomhall J, et al. Frequency of severe hypoglycemia requiring emergency treatment in type 1 and type 2 diabetes: a population-based study of health service resource use. Diabetes Care. 2003;26(4):1176–80.
McQueen RB, Ellis SL, Maahs DM, et al. Association between glycated hemoglobin and health utility for type 1 diabetes. Patient-Centered Outcomes Research. 2014;7(2):197–205.
McCoy RG, Van Houten HK, Ziegenfuss JY, Shah ND, Wermers RA, Smith SA. Increased mortality of patients with diabetes reporting severe hypoglycemia. Diabetes Care. 2012;35(9):1897–901.
Lundqvist A, Andersson E, Steen Carlsson K. The cost of diabetes in 2020 and 2030—a model analysis comparing innovative glucose lowering treatments in second line following European and American guidelines compared to current standard of care. The Swedish Institute for Health Economics (IHE); 2016. https://ihe.se/en/publicering/costs-diabetes-2020-2030/. Accessed 24 June 2021.
Miller KM, Beck RW, Bergenstal RM, Goland RS, Haller MJ, McGill JB, et al. Evidence of a strong association between frequency of self-monitoring of blood glucose and hemoglobin A1c levels in T1D exchange clinic registry participants. Diabetes Care. 2013;36(7):2009–14.
Battelino T, Danne T, Bergenstal RM, et al. Clinical targets for continuous glucose monitoring data interpretation: recommendations from the international consensus on time in range. Diabetes Care. 2019;42(8):1593–603.
Chaugule S, Oliver N, Klinkenbijl B, Graham C. An economic evaluation of continuous glucose monitoring for people with type 1 diabetes and impaired awareness of hypoglycaemia within North West London Clinical Commissioning Groups in England. Eur Endocrinol. 2017;13:81–5.
Acknowledgements
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Deirdre Blissett is a paid consultant for Abbott Diabetes Care. Richard Hellmund is an employee of Abbott Diabetes Care and is a stockholder. Stig Attvall serves as a consultant for Abbott Diabetes Care.
Funding
This work, including the journal’s rapid service fee, was funded by Abbott Diabetes Care.
Author Contributions
DB created the spreadsheet tool and draft of the manuscript; SA validated the inputs to the model and reviewed the draft manuscript; RH proposed the inputs for the model and also reviewed the spreadsheet tool and draft manuscript.
Data Availability
All data generated or analyzed during this study are included in this published article or as supplementary information files.
Compliance with Ethics Guidelines
This study involves a cost analysis and it did not involve any studies with human or animal subjects performed by any of the authors, hence there was no requirement to seek ethics committee approval.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Blissett, D.B., Attvall, S. & Hellmund, R.A. Analysis Estimating the Potential Cost Impact of Utilizing Flash Glucose Monitoring with Optional Alarms in Swedish Adults with Diabetes with Impaired Awareness of Hypoglycaemia, Using Intensive Insulin. Diabetes Ther 12, 2179–2193 (2021). https://doi.org/10.1007/s13300-021-01099-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-021-01099-7