Abstract
Introduction
VERTIS CV is the cardiovascular outcome trial for the sodium–glucose cotransporter 2 (SGLT2) inhibitor ertugliflozin. A sub-study was conducted to assess the efficacy and safety of ertugliflozin in patients with type 2 diabetes mellitus (T2DM) inadequately glycemic-controlled on metformin and a sulfonylurea (SU).
Methods
Patients with T2DM, established atherosclerotic cardiovascular disease (ASCVD), and an HbA1c of 7.0–10.5% on stable metformin (≥ 1500 mg/day) and moderate to high SU doses were randomly assigned to once-daily ertugliflozin (5 or 15 mg) or placebo. The primary sub-study objectives were to assess the effect of ertugliflozin on HbA1c compared with placebo and to evaluate safety following 18 weeks of treatment. Key secondary endpoints included changes in fasting plasma glucose (FPG), body weight (BW), blood pressure (BP), and the proportion of patients achieving HbA1c < 7%.
Results
Of the 8246 patients enrolled in VERTIS CV, 330 were eligible for this sub-study (ertugliflozin 5 mg, n = 100; ertugliflozin 15 mg, n = 113; placebo, n = 117). This subgroup had a mean (SD) age of 63.2 (8.4) years and T2DM duration of 11.4 (7.4) years. At week 18, ertugliflozin 5 mg and 15 mg were each associated with significantly greater least squares (LS) mean reductions from baseline in HbA1c relative to placebo (placebo-adjusted LS mean [95% CI] − 0.66% [− 0.89, − 0.43] and − 0.75% [− 0.98, − 0.53], respectively, p < 0.001 for each dose vs placebo). Ertugliflozin significantly reduced FPG and BW compared with placebo (p < 0.001), but not systolic BP. Adverse events were reported in 48.0%, 54.9%, and 47.0% of patients in the ertugliflozin 5 mg and 15 mg, and placebo groups. The incidences of symptomatic hypoglycemia were 11.0% (5 mg), 12.4% (15 mg), and 7.7% (placebo), and of severe hypoglycemia 2.0% (5 mg), 1.8% (15 mg), and 0.9% (placebo).
Conclusions
In patients with T2DM and ASCVD, ertugliflozin added to metformin and SU improved glycemic control, reduced BW, and was generally well tolerated.
Trial Registration
VERTIS CV ClinicalTrials.gov identifier, NCT01986881.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Metformin and sulfonylureas (SUs) remain a commonly used combination for the treatment of type 2 diabetes mellitus (T2DM). If additional glycemic control is required and a decision is made to add a third oral agent to that regimen, the glycemic efficacy and extra-glycemic effects of sodium–glucose cotransporter 2 (SGLT2) inhibitors, including their associated effects on reduction in body weight and blood pressure and cardiorenal benefits, make them a potentially attractive choice. |
VERTIS CV was the cardiovascular outcome study for the SGLT2 inhibitor ertugliflozin, conducted in patients with T2DM and established atherosclerotic cardiovascular disease. As part of VERTIS CV, a sub-study was conducted to assess the efficacy and safety of ertugliflozin (5 mg and 15 mg) as add-on therapy to metformin (≥1500 mg/day) and a SU. |
What was learned from the study? |
Ertugliflozin as add-on therapy to metformin and SU resulted in significantly greater reductions in HbA1c, fasting plasma glucose, and body weight than placebo. |
Ertugliflozin was generally well tolerated with a safety profile consistent with the SGLT2 inhibitor drug class. |
Ertugliflozin is a suitable candidate add-on therapy in patients with T2DM who are inadequately controlled with metformin and SU. |
Digital Features
This article is published with digital features, including a summary slide, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.13950776.
Introduction
Type 2 diabetes mellitus (T2DM) is a progressive disease, and with disease progression, metformin and sulfonylureas (SUs) remain a commonly used combination therapy because of their glycemic efficacy, low cost, and complementary mechanisms of actions [1, 2]. The major pharmacologic actions of metformin are to decrease hepatic glucose production, decrease intestinal absorption of glucose, and improve insulin sensitivity [3, 4]; whereas, SUs are insulin secretagogues [5]. While SUs are effective in reducing glycated hemoglobin (HbA1c) when used with metformin, they are associated with weight gain and a higher incidence of hypoglycemia than other antihyperglycemic agents (AHAs) [6, 7]. When additional glycemic control is needed and a decision is made to add a third oral AHA to the existing metformin + SU regimen, sodium–glucose transporter 2 (SGLT2) inhibitors may be an attractive option.
SGLT2 inhibitors represent a class of AHAs that decrease renal glucose reabsorption from the proximal tubule of the kidney, thereby enhancing urinary glucose excretion and reducing plasma glucose and HbA1c [8]. Unlike SUs, SGLT2 inhibitors act independently of beta cell function and insulin sensitivity, are not associated with hypoglycemia when used as monotherapy, and are associated with weight loss [9,10,11,12]. SGLT2 inhibitors have also been demonstrated to have cardiovascular (CV) and renal benefits [13,14,15,16,17,18,19]. Because of their cardiorenal benefits, recent society guidances and consensus statements are recommending the use of SGLT2 inhibitors earlier in the treatment algorithms for patients with T2DM with established or at an increased risk of CV disease and in those with chronic kidney disease [20, 21].
Ertugliflozin is a selective SGLT2 inhibitor that has been evaluated as both monotherapy and in combination with other AHAs in the phase 3 VERTIS (eValuation of ERTugliflozin effIcacy and Safety) clinical program [22,23,24,25,26,27,28,29]. Data from the VERTIS suite of studies have shown that ertugliflozin (5 mg and 15 mg) results in clinically meaningful reductions in HbA1c, is associated with reductions in body weight and blood pressure, and is generally well tolerated with a safety profile consistent with other SGLT2 inhibitors [22,23,24,25,26,27,28,29]. However, the addition of ertugliflozin as third-line therapy on a background of metformin and SU has not been previously studied. The VERTIS CV trial was conducted to evaluate the effects of ertugliflozin on CV and renal outcomes in patients with T2DM and established atherosclerotic CV disease (ASCVD) [19, 30]. The VERTIS CV trial included sub-studies to assess the efficacy of ertugliflozin in combination with other AHAs on glycemic and metabolic endpoints. The results reported here describe the efficacy and safety in patients who were inadequately controlled with metformin and a SU.
Methods
Objectives
The primary objectives of the present sub-study were to assess the effects of 18 weeks of treatment with ertugliflozin (5 mg and 15 mg) on HbA1c compared with placebo, and to evaluate the safety and tolerability of ertugliflozin. As secondary objectives, the effects of ertugliflozin on fasting plasma glucose (FPG), body weight, proportion of patients with HbA1c < 7%, and systolic and diastolic blood pressure (SBP and DBP, respectively) were also assessed.
Study Design
VERTIS CV was a multicenter, randomized, double-blind, placebo-controlled, parallel-group, event-driven study that was initiated in 2013. The main study was enrolled in two sequential cohorts (cohort 1 and cohort 2). On the basis of evolving information about the SGLT2 inhibitor class, the study population was expanded by a protocol amendment in 2016 to enable the assessment of VERTIS CV cardiorenal endpoints. The metformin + SU sub-study included patients from cohort 1 who were on metformin + SU at baseline.
The metformin + SU sub-study was conducted during the first 18 weeks of the double-blind treatment period in patients with T2DM and ASCVD who had inadequate glycemic control with metformin and SU at moderate to high doses. A computer-generated code based on the method of random permuted blocks was used to randomly assign patients 1:1:1 to receive once-daily, orally administered 5 mg or 15 mg ertugliflozin or matching placebo. To maintain double-blinding, placebo tablets matched the ertugliflozin 5 mg and 10 mg tablets, and patients were instructed to take two tablets daily of ertugliflozin/placebo.
Doses of all background AHAs were to remain constant during the 18-week treatment period. However, patients were to receive glycemic rescue therapy if FPG increased to > 270 mg/dL (15.0 mmol/L) between randomization and week 6, > 240 mg/dL (13.3 mmol/L) during weeks 6–12, or > 200 mg/dL (11.1 mmol/L) during weeks 12–18. Participants who received glycemic rescue therapy remained in the study and continued to receive blinded study medication (ertugliflozin or matching placebo) for the duration of the study. In addition, investigators were permitted to reduce or discontinue the background AHAs (metformin and/or SU) in response to a clinically significant hypoglycemic event, and to adjust medications for CV disease (e.g., for hypertension, dyslipidemia) as needed. Patients were counseled according to local dietary and lifestyle guidelines and asked to adhere to these guidelines throughout the study.
The protocol and informed consent documents were approved by the institutional review board or independent ethics committee at each participating site (Table S1). The study was conducted in accordance with the ethical principles of the Declaration of Helsinki and in compliance with all International Council for Harmonisation Good Clinical Practice Guidelines. All participants signed informed consent forms (that were witnessed) before any screening procedures were conducted.
Patient Sample
Women and men aged ≥ 40 years were eligible for the main VERTIS CV trial if they had a diagnosis of T2DM according to the American Diabetes Association guidelines, an HbA1c of 7.0–10.5% (53–91 mmol/mol) at screening, a body mass index (BMI) ≥ 18.0 kg/m2, and a history or evidence of coronary artery disease, ischemic cerebrovascular disease, or peripheral arterial disease. Protocol-specified definitions of these conditions have been published previously [30]. Patients taking blood pressure or lipid-lowering medications were required to be on a stable dose for ≥ 4 weeks prior to randomization. Patients who met the aforementioned criteria were included in the present sub-study if they had been receiving metformin (≥ 1500 mg/day) and SU (gliclazide [immediate- or modified-release], glimepiride, glipizide, glyburide [micronized and non-micronized], acetohexamide, tolbutamide, or tolazamide) at stable doses above a prespecified minimum for at least 8 weeks prior to screening and randomization. Individuals were excluded if they had a history of type 1 diabetes or ketoacidosis, screening FPG or fingerstick glucose measurement > 270 mg/dL (15 mmol/L), unstable weight (≥ 5% change in body weight in previous 6 months), or estimated glomerular filtration rate (eGFR) < 55 mL/min/1.73 m2 or a screening serum creatinine ≥ 1.3 mg/dL (115 μmol/L) in men or ≥ 1.2 mg/dL (110 μmol/L) in women.
Sub-Study Endpoints and Assessments
The primary efficacy endpoint was change in HbA1c from baseline at week 18. Secondary endpoints included changes from baseline at week 18 in FPG, body weight, SBP, and DBP, as well as the proportion of patients with HbA1c < 7.0% (53 mmol/mol) at week 18. The proportion of patients who received glycemic rescue therapy was also assessed. Efficacy measurements were conducted at baseline and weeks 6, 12, and 18. All clinical laboratory assessments, including HbA1c and FPG, were performed at a central laboratory. Body weight was measured in duplicate using a standardized, digital scale. Sitting blood pressure was measured in triplicate using an automated, oscillometric blood pressure measuring device.
Treatment safety and tolerability were evaluated according to the reporting of assessments that included adverse events (AEs), serious AEs (SAEs), deaths, and discontinuations due to AEs. Prespecified AEs of special interest included genital mycotic infection (GMI) by gender, urinary tract infection (UTI), symptomatic hypoglycemia (event with clinical symptoms reported by the investigator as hypoglycemia), and hypovolemia. Other AEs of interest included documented hypoglycemia (episodes with a glucose level ≤ 70 mg/dL [3.9 mmol/L] with or without symptoms) and severe hypoglycemia (episodes that required second party assistance). To monitor safety during the study, AEs were reviewed contemporaneously by study team members, by formal review of aggregate and trends by the study team monthly, and unblinded interim safety data were periodically provided to an external data monitoring committee.
Statistical Methods
To ensure sufficient power to demonstrate superiority of ertugliflozin over placebo in reducing HbA1c during the 18-week treatment period, the sub-study was planned to enroll at least 260 patients (ca. 86 per treatment arm). This sample size was calculated to provide approximately 96% power to detect a treatment difference of 0.6% using a two-sided 0.05 alpha level of significance, assuming a standard deviation (SD) of 1.0% and a 10% rate of loss to follow-up. With the actual sample size of 330, the power was > 99%. The statistical analyses were conducted using SAS v9.3 (Cary, NC, USA).
Analysis of Efficacy Endpoints
The primary and secondary efficacy endpoints were tested using the null hypothesis of no difference between ertugliflozin and placebo, and controlling for the type I error rate using a fixed testing sequence. Separate hypotheses were set for each efficacy endpoint—one for the 15 mg dose and one for the 5 mg dose, which was tested only if the hypothesis for the 15 mg dose reached statistical significance (p < 0.05). Endpoints were tested in the following order, HbA1c, FPG, body weight, proportion of patients with HbA1c < 7.0%, SBP, DBP; testing was advanced to the next endpoint in the sequence until the first p value was ≥ 0.05. Efficacy endpoints were analyzed using the full analysis set (FAS), which comprised all randomized patients who received at least one dose of study medication and had at least one measurement of the analysis endpoint. Efficacy data obtained after the initiation of glycemic rescue therapy were censored (i.e., treated as missing) to avoid the confounding effects of these treatments (referred to as excluding rescue approach).
Between-group changes from baseline at week 18 were evaluated using a constrained longitudinal data analysis (cLDA) model that accounted for treatment, visit (categorical), treatment by visit interaction, and baseline eGFR (continuous). The cLDA model assumes a common mean across treatment groups at baseline and a different mean for each treatment at each of the post-baseline time points. Logistic regression analysis was used to evaluate the proportion of patients with HbA1c < 7.0% at week 18. The statistical model included terms for treatment (categorical), baseline HbA1c (continuous), and baseline eGFR (continuous). For missing data at week 18, the analysis utilized multiple imputation based on cLDA modeling. The proportion of patients requiring glycemic rescue therapy up to week 18 was analyzed by treatment using log-rank tests comparing the time-to-event distribution of each dose of ertugliflozin versus placebo.
Analysis of Safety Endpoints
Safety data were analyzed using the all subjects as treated (ASaT) population which comprised all randomized patients who received at least one dose of study medication. Two sets of data were considered—data pertaining to the treatment period and data pertaining to the all post-randomization follow-up period. The treatment period dataset included all data from randomization through week 18. For patients who discontinued study medication prior to week 18, the treatment period dataset included all data from randomization to 14 days after the final dose of study medication for AEs and 2 days after the final dose of study medication for laboratory endpoints and electrocardiograms. The all post-randomization follow-up period dataset included all available data after randomization, with week 18 as the upper limit on the follow-up window for the sub-study. Analyses of SAEs included all post-randomization follow-up data through week 18.
The AEs of UTI, GMI, symptomatic hypoglycemia, and hypovolemia were analyzed according to incidence, risk difference, 95% confidence interval (CI), and p values (not adjusted for multiplicity). With the exception of hypoglycemia, the safety analyses included data obtained after the initiation of rescue therapy (referred to as including rescue approach). For other AEs of interest, 95% CIs were calculated.
Percentage changes from baseline in high-density lipoprotein cholesterol (HDL-C) and low-density lipoprotein cholesterol (LDL-C) were analyzed using the cLDA method described for HbA1c. Mean changes from baseline for other reported clinical laboratory tests (serum magnesium, phosphate, and uric acid, and hematocrit and hemoglobin) were summarized descriptively.
Results
Patient Disposition and Baseline Characteristics
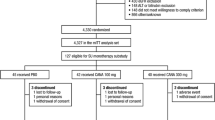
A total of 330 patients were randomized to receive ertugliflozin (5 mg, n = 100; 15 mg, n = 113) or placebo (n = 117) and 313 (94.8%) patients completed study treatment (5 mg, n = 96; 15 mg, n = 108; placebo, n = 109) (Fig. 1). Patient withdrawal was the most common reason for treatment discontinuation (Fig. 1). Study discontinuation rates were low; one patient in the placebo group withdrew from the study and one patient in the 15 mg group died, with all others remaining in the study to completion.
Treatment groups were generally similar with regard to patient demographics and other baseline characteristics (Table 1). Overall, the majority of patients were male (74.8%), had a mean (SD) age of 63.2 (8.4) years and BMI of 31.7 (5.2) kg/m2, and were notably European (58.8%). Patients had been diagnosed with T2DM a mean (SD) of 11.4 (7.4) years prior to entering the study. Baseline HbA1c and FPG values were similar across treatment groups. A higher percentage of patients treated with ertugliflozin (9.0% [5 mg] and 10.6% [15 mg]) than placebo (2.6%) had eGFR values between 30 and < 60 mL/min/1.73 m2. Medications with evidence of CV benefit in this secondary prevention population were highly utilized, including renin–angiotensin–aldosterone system inhibitors (80.3%), lipid-modifying agents (78.8%), aspirin (69.1%; in the analgesics category), beta-blockers (68.5%), diuretics (35.5%), and antithrombotic agents (34.2%).
At randomization, all patients were taking metformin ≥ 1500 mg daily; the median (range) dose at baseline was 2000 (1500–3000) mg/day (mean [SD], 2077.5 mg/day [410.3]) (Table 2). The most commonly prescribed SUs (median dose [range]) at randomization were gliclazide (90 mg/day [60.0–320.0]), glimepiride (4.0 mg/day [4.0–8.0]), glipizide (15.0 mg/day [10.0–40.0]), and glyburide (glibenclamide) (10.0 mg/day [7.0–20.0]) (Table 2).
Efficacy
Treatment with ertugliflozin resulted in a progressive decrease in HbA1c levels over 18 weeks (Fig. 2). Ertugliflozin 5 mg and 15 mg were each associated with a significantly greater least squares (LS) mean reduction from baseline in HbA1c relative to placebo at week 18 (p < 0.001 for both comparisons; Table 3, Fig. 3a). Additionally, greater proportions of patients in the ertugliflozin groups achieved HbA1c < 7.0% by week 18 compared with placebo (Fig. 3b). Accordingly, patients in the ertugliflozin treatment groups had significantly higher odds ratios of achieving HbA1c < 7.0% than those who received placebo (5 mg: 6.0 [95% CI 2.9, 12.5]; 15 mg: 4.1 [95% CI 2.0, 8.4]). In a subgroup analysis, both doses of ertugliflozin reduced HbA1c relative to placebo irrespective of baseline HbA1c, age, gender, or race (Fig. 4).
Primary and secondary efficacy outcomes. a LS mean change from baseline in HbA1c at week 18; b Proportion of patients with HbA1c < 7% at week 18; c LS mean change from baseline in FPG at week 18; d LS mean change from baseline in body weight at week 18; e LS mean change from baseline in systolic BP at week 18; f LS mean change from baseline in diastolic BP at week 18. BP blood pressure, CI confidence interval, FPG fasting plasma glucose, HbA1c glycated hemoglobin, LS least squares
Estimate of placebo-adjusted change from baseline in HbA1c at week 18 by subgroup category (FAS population, excluding rescue approach). Point estimate and 95% CIs are shown. The median age (65 years) and median HbA1c (8.1%) were derived from the overall patient population of the main study. Values in parentheses are n’s for placebo, ertugliflozin 5 mg and 15 mg groups, respectively. CI confidence interval, FAS full analysis set, HbA1c glycated hemoglobin, LS least squares
At week 18, LS mean reductions from baseline in FPG (Fig. 3c) and body weight (Fig. 3d) were significantly greater for the ertugliflozin 5 mg and 15 mg groups compared with placebo (p < 0.001 for all comparisons). The placebo-adjusted LS mean (95% CI) change in body weight was − 1.6 kg (− 2.3, − 0.8) and − 1.9 kg (− 2.7, − 1.2) for ertugliflozin 5 mg and 15 mg, respectively. LS mean reductions from baseline SBP (Fig. 3e) and to a lesser extent DBP (Fig. 3f) at week 18 were observed with ertugliflozin 5 mg and 15 mg compared with placebo, but the effect on SBP with ertugliflozin 15 mg was not significant, hence further hypothesis testing of remaining secondary endpoints (blood pressure assessments) was stopped. Glycemic rescue therapy was required by fewer patients in the ertugliflozin 5 mg (7.0%) and 15 mg (2.7%) groups through week 18 relative to the placebo group (10.3%).
Safety
Overall AE Summary
AEs, SAEs, and discontinuations due to an AE occurred at similar rates across treatment groups (Table 4). The number of patients who discontinued treatment because of an AE was low (n = 5); two were in the placebo group (abdominal distension, upper respiratory tract infection) and three were in the ertugliflozin 15 mg group (genital fungal infection, depression, dysuria). Incidences of SAEs were similar across treatment groups; none were considered related to study drug. One AE resulting in death (due to multiple organ failure associated with a hemorrhagic stroke) was reported in the sub-study in the ertugliflozin 15 mg group.
Prespecified and Other AEs of Interest
Symptomatic hypoglycemic events (excluding rescue therapy use) were numerically higher in the ertugliflozin groups, occurring among 7.7%, 11.0%, and 12.4% of patients who received placebo, ertugliflozin 5 mg, and ertugliflozin 15 mg, respectively (estimate of difference [95% CI] 3.3% [− 4.6, 11.9] and 4.7% [− 3.2, 13.0] for ertugliflozin 5 mg and 15 mg, respectively) (Table 4). The incidence of documented hypoglycemia (symptomatic and asymptomatic) was higher in the ertugliflozin 15 mg group (26.5%) than the placebo group (14.5%) (estimate of difference [95% CI] 12.0% [1.6, 22.5]) but not in the ertugliflozin 5 mg group (20.0%; estimate of difference [95% CI] 5.5% [− 4.6, 16.0]) (Table 4). Severe hypoglycemia episodes were infrequent across treatment groups (Table 4). The incidence of UTI was low and similar across treatment groups (Table 4). No serious UTI AEs were reported for any patients; all were mild to moderate in intensity and only one led to discontinuation of study medication. GMI was experienced by significantly higher proportions of male patients who received ertugliflozin 5 mg and 15 mg (4.2% and 4.8%, respectively) compared with placebo (0.0%; p ≤ 0.05 for both comparisons) and by a numerically, but not significantly, higher proportion of female patients who received ertugliflozin 15 mg compared with placebo (10.3% vs 3.8%; p = 0.36) (Table 4). No serious GMI AEs were reported for any patients and only one led to discontinuation of study medication. One patient in the ertugliflozin 15 mg group experienced an AE associated with hypovolemia (orthostatic hypotension) compared with none in the other groups (Table 4).
Laboratory Assessments
At week 18, increases in the LS mean percentage change from baseline in LDL-C and HDL-C were observed in the ertugliflozin 15 mg group relative to the placebo group (Table S2). Small mean increases from baseline in serum magnesium (< 0.2 mEq/L) and serum phosphate (< 0.2 mg/dL) and small mean decreases in serum uric acid (< 0.4 mg/dL) were observed at week 18 in both ertugliflozin groups (Table S3). Small increases from baseline in hematocrit (≤ 2.6%) and hemoglobin (≤ 0.6 g/dL) were observed at week 18 in both ertugliflozin groups (Table S3).
Discussion
In this sub-study of the VERTIS CV trial, patients with T2DM and established ASCVD on a background regimen of metformin and SU achieved greater reductions in HbA1c with once-daily ertugliflozin 5 mg and 15 mg than with placebo. Additionally, ertugliflozin was associated with greater improvements in FPG and body weight, and higher proportions of patients achieved HbA1c < 7%, compared with placebo. Glycemic rescue medication was required by a higher percentage of placebo patients relative to ertugliflozin, further supporting the glycemic efficacy of ertugliflozin. The changes in HbA1c were consistent across all subgroups analyzed, including baseline HbA1c, age, gender, and race. The glycemic efficacy observed with ertugliflozin in this sub-study is comparable with that observed in studies of other SGLT2 inhibitors where those agents were added on to a background of metformin and SU dual therapy [31,32,33].
Weight loss is an important consideration in the treatment of T2DM [20]. In the context of the weight gain typically seen with SU therapy [7, 24], the reductions in body weight observed in the present sub-study represent an additional benefit to patients on metformin and SU combination therapy. In VERTIS CV, the reduction in body weight observed with ertugliflozin, compared with placebo, in the overall population was remarkably stable over the multi-year duration of the study [19].
SGLT2 inhibitors, including ertugliflozin, have been shown to be associated with modest reductions in blood pressure, particularly systolic blood pressure [7, 10, 34, 35]. The lack of a significant reduction in systolic blood pressure with ertugliflozin, compared with placebo, in the present sub-study is inconsistent with other ertugliflozin studies, including the main VERTIS CV trial, where changes in blood pressure were observed to be comparable in magnitude to those observed with the drug class. In the main VERTIS CV trial, in the overall population, the changes from baseline in systolic blood pressure at week 18 in the ertugliflozin groups relative to placebo were greater than observed in this sub-study (LS mean change 0.05 mmHg [placebo], − 2.42 mmHg [ertugliflozin 5 mg], − 2.76 mmHg [ertugliflozin 15 mg]).
The safety findings in this sub-study were consistent with those of previous VERTIS phase 3 studies, in which ertugliflozin was generally well tolerated. GMI is a recognized adverse event with SGLT2 inhibitor therapy [36, 37]. In the present sub-study, a significantly higher AE rate in male GMI was observed in both ertugliflozin groups compared with the placebo group. UTIs were reported at similar rates across treatment groups and no serious UTIs were reported; however, in the main study, more non-serious UTIs were seen in the ertugliflozin groups than in the placebo group [19]. Changes from baseline in laboratory parameters including lipids, hematocrit and hemoglobin, and analytes (magnesium, phosphate, uric acid) observed in this sub-study were consistent with the findings in other VERTIS program studies [38]. The increases in hemoglobin and hematocrit and decreases in uric acid may be important mediators of the beneficial effects of SGLT2 inhibitors on heart failure, CV death, and kidney events [39,40,41].
The pattern of hypoglycemia observed in this sub-study and similar studies with other SGLT2 inhibitors suggests that the addition of SGLT2 inhibitors to a background of metformin and SU (a dual combination therapy associated with hypoglycemia because of the SU component) may be associated with an increased risk of hypoglycemia. In this sub-study a numerically higher incidence of symptomatic hypoglycemia occurred in the ertugliflozin groups compared with the placebo group and a significantly higher incidence of documented hypoglycemia occurred in the ertugliflozin 15 mg group compared with the placebo group. The limited number of severe hypoglycemia events that occurred in this sub-study limits conclusions that can be drawn about severe hypoglycemia. In a 24-week study where empagliflozin 10 mg or 25 mg was added on to a background of metformin and SU, confirmed hypoglycemic AEs were reported more frequently in the empagliflozin 10 mg (n = 36; 16.1%) and empagliflozin 25 mg (n = 25; 11.5%) groups compared with the placebo group (n = 19; 8.4%); none of the events required assistance [31]. In a 24-week study where dapagliflozin 10 mg or placebo was added on to a background of metformin and SU, the incidence of hypoglycemia was significantly higher in the dapagliflozin group compared with the placebo group (12.8% vs 3.7%; p = 0.024); no major episodes were reported [33]. In a 52-week study where canagliflozin 100 mg and 300 mg or placebo was added on to a background of metformin and SU, a significantly increased incidence of documented hypoglycemia was observed with canagliflozin groups compared with the placebo group; differences (95% CI) vs placebo were 15.8% (5.6, 26.0) and 18.6% (8.3, 28.9) for canagliflozin 100 mg and 300 mg, respectively, with one episode of severe hypoglycemia in each treatment group [32].
Limitations
A potential criticism is that the duration of the study was restricted to 18 weeks; however, this represents sufficient time to observe the effects of ertugliflozin on background metformin and SU as evidenced by the plateau in HbA1c. Long-term evaluation was limited by modification allowed to background AHAs after that time. Although patients who participated in the sub-study were not specifically followed as a separate analyzed cohort beyond 18 weeks, the long-term effect of ertugliflozin on glycemic control was observed in the overall VERTIS CV population [19]. Although these results are in a population with T2DM and established ASCVD, the efficacy observed in the present sub-study is consistent with previous ertugliflozin studies where patients were not selected for ASCVD [22,23,24,25,26,27,28,29], and therefore is likely generalizable to patients with T2DM without prevalent ASCVD.
Conclusions
In patients with T2DM and established ASCVD with inadequate glycemic control on metformin and a SU, the addition of ertugliflozin treatment (both 5 mg and 15 mg) versus placebo for 18 weeks resulted in clinically meaningful reductions from baseline in HbA1c and FPG, and a greater proportion of patients achieving HbA1c < 7.0%. Ertugliflozin also reduced body weight relative to placebo, but did not provide statistically significant improvements in blood pressure. Ertugliflozin was generally well tolerated and exhibited a safety profile consistent with previous studies of ertugliflozin and the SGLT2 inhibitor class.
References
Montvida O, Shaw J, Atherton JJ, Stringer F, Paul SK. Long-term trends in antidiabetes drug usage in the US: real-world evidence in patients newly diagnosed with type 2 diabetes. Diabetes Care. 2018;41:69–78.
Sanchez-Rangel E, Inzucchi SE. Metformin: clinical use in type 2 diabetes. Diabetologia. 2017;60:1586–93.
Foretz M, Guigas B, Viollet B. Understanding the glucoregulatory mechanisms of metformin in type 2 diabetes mellitus. Nat Rev Endocrinol. 2019;15:569–89.
Foretz M, Guigas B, Bertrand L, Pollak M, Viollet B. Metformin: from mechanisms of action to therapies. Cell Metab. 2014;20:953–66.
Proks P, Reimann F, Green N, Gribble F, Ashcroft F. Sulfonylurea stimulation of insulin secretion. Diabetes. 2002;51(Suppl 3):S368–76.
Mishriky BM, Cummings DM, Tanenberg RJ. The efficacy and safety of DPP4 inhibitors compared to sulfonylureas as add-on therapy to metformin in patients with type 2 diabetes: a systematic review and meta-analysis. Diabetes Res Clin Pract. 2015;109:378–88.
Mearns ES, Sobieraj DM, White CM, et al. Comparative efficacy and safety of antidiabetic drug regimens added to metformin monotherapy in patients with type 2 diabetes: a network meta-analysis. PLoS One. 2015;10:e0125879.
Ferrannini E, Solini A. SGLT2 inhibition in diabetes mellitus: rationale and clinical prospects. Nat Rev Endocrinol. 2012;8:495–502.
Zhang YJ, Han SL, Sun XF, et al. Efficacy and safety of empagliflozin for type 2 diabetes mellitus: meta-analysis of randomized controlled trials. Medicine (Baltimore). 2018;97:e12843.
Hu J, Deng A, Zhao Y. Ertugliflozin as a monotherapy for the treatment of type 2 diabetes. Expert Opin Pharmacother. 2018;19:1841–7.
Dhillon S. Dapagliflozin: a review in type 2 diabetes. Drugs. 2019;79:1135–46.
Parveen R, Agarwal NB, Kaushal N, Mali G, Raisuddin S. Efficacy and safety of canagliflozin in type 2 diabetes mellitus: systematic review of randomized controlled trials. Expert Opin Pharmacother. 2016;17:105–15.
Neal B, Perkovic V, Mahaffey KW, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017;377:644–57.
Wiviott SD, Raz I, Bonaca MP, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2019;380:347–57.
Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373:2117–28.
McMurray JJV, Solomon SD, Inzucchi SE, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019;381:1995–2008.
Wanner C, Inzucchi SE, Lachin JM, et al. Empagliflozin and progression of kidney disease in type 2 diabetes. N Engl J Med. 2016;375:323–34.
Perkovic V, Jardine MJ, Neal B, et al. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med. 2019;380:2295–306.
Cannon CP, Pratley R, Dagogo-Jack S, et al. Cardiovascular outcomes with ertugliflozin in type 2 diabetes. N Engl J Med. 2020;383:1425–35.
American Diabetes Association. 9. Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes-2020. Diabetes Care. 2020;43:S98-s110.
Cosentino F, Grant PJ, Aboyans V, et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J. 2020;41:255–323.
Dagogo-Jack S, Liu J, Eldor R, et al. Efficacy and safety of the addition of ertugliflozin in patients with type 2 diabetes mellitus inadequately controlled with metformin and sitagliptin: the VERTIS SITA2 placebo-controlled randomized study. Diabetes Obes Metab. 2018;20:530–40.
Grunberger G, Camp S, Johnson J, et al. Ertugliflozin in patients with stage 3 chronic kidney disease and type 2 diabetes mellitus: the VERTIS RENAL randomized study. Diabetes Ther. 2018;9:49–66.
Hollander P, Liu J, Hill J, et al. Ertugliflozin compared with glimepiride in patients with type 2 diabetes mellitus inadequately controlled on metformin: the VERTIS SU randomized study. Diabetes Ther. 2018;9:193–207.
Pratley RE, Eldor R, Raji A, et al. Ertugliflozin plus sitagliptin versus either individual agent over 52 weeks in patients with type 2 diabetes mellitus inadequately controlled with metformin: the VERTIS FACTORIAL randomized trial. Diabetes Obes Metab. 2018;20:1111–20.
Rosenstock J, Frias J, Pall D, et al. Effect of ertugliflozin on glucose control, body weight, blood pressure and bone density in type 2 diabetes mellitus inadequately controlled on metformin monotherapy (VERTIS MET). Diabetes Obes Metab. 2018;20:520–9.
Terra SG, Focht K, Davies M, et al. Phase III, efficacy and safety study of ertugliflozin monotherapy in people with type 2 diabetes mellitus inadequately controlled with diet and exercise alone. Diabetes Obes Metab. 2017;19:721–8.
Miller S, Krumins T, Zhou H, et al. Ertugliflozin and sitagliptin co-initiation in patients with type 2 diabetes: the VERTIS SITA randomized study. Diabetes Ther. 2018;9:253–68.
Ji L, Liu Y, Miao H, et al. Safety and efficacy of ertugliflozin in Asian patients with type 2 diabetes mellitus inadequately controlled with metformin monotherapy: VERTIS Asia. Diabetes Obes Metab. 2019;21:1474–82.
Cannon CP, McGuire DK, Pratley R, et al. Design and baseline characteristics of the eValuation of ERTugliflozin effIcacy and Safety CardioVascular outcomes trial (VERTIS-CV). Am Heart J. 2018;206:11–23.
Haring HU, Merker L, Seewaldt-Becker E, et al. Empagliflozin as add-on to metformin plus sulfonylurea in patients with type 2 diabetes: a 24-week, randomized, double-blind, placebo-controlled trial. Diabetes Care. 2013;36:3396–404.
Wilding JP, Charpentier G, Hollander P, et al. Efficacy and safety of canagliflozin in patients with type 2 diabetes mellitus inadequately controlled with metformin and sulphonylurea: a randomised trial. Int J Clin Pract. 2013;67:1267–82.
Matthaei S, Bowering K, Rohwedder K, Grohl A, Parikh S. Dapagliflozin improves glycemic control and reduces body weight as add-on therapy to metformin plus sulfonylurea: a 24-week randomized, double-blind clinical trial. Diabetes Care. 2015;38:365–72.
Mazidi M, Rezaie P, Gao HK, Kengne AP. Effect of sodium-glucose cotransport-2 inhibitors on blood pressure in people with type 2 diabetes mellitus: a systematic review and meta-analysis of 43 randomized control trials with 22,528 patients. J Am Heart Assoc. 2017;6:e004007.
Zaccardi F, Webb DR, Htike ZZ, Youssef D, Khunti K, Davies MJ. Efficacy and safety of sodium-glucose co-transporter-2 inhibitors in type 2 diabetes mellitus: systematic review and network meta-analysis. Diabetes Obes Metab. 2016;18:783–94.
Shi FH, Li H, Shen L, et al. Appraisal of non-cardiovascular safety for sodium-glucose co-transporter 2 inhibitors: a systematic review and meta-analysis of placebo-controlled randomized clinical trials. Front Pharmacol. 2019;10:1066.
Unnikrishnan AG, Kalra S, Purandare V, Vasnawala H. Genital infections with sodium glucose cotransporter-2 inhibitors: occurrence and management in patients with type 2 diabetes mellitus. Indian J Endocrinol Metab. 2018;22:837–42.
Gallo S, Charbonnel B, Goldman A, et al. Long-term efficacy and safety of ertugliflozin in patients with type 2 diabetes mellitus inadequately controlled with metformin monotherapy: 104-week VERTIS MET trial. Diabetes Obes Metab. 2019;21:1027–36.
Li J, Woodward M, Perkovic V, et al. Mediators of the effects of canagliflozin on heart failure in patients with type 2 diabetes. JACC Heart Fail. 2020;8:57–66.
Li J, Neal B, Perkovic V, et al. Mediators of the effects of canagliflozin on kidney protection in patients with type 2 diabetes. Kidney Int. 2020;98:769–77.
Inzucchi SE, Zinman B, Fitchett D, et al. How does empagliflozin reduce cardiovascular mortality? Insights from a mediation analysis of the EMPA-REG OUTCOME trial. Diabetes Care. 2018;41:356–63.
Acknowledgements
The authors wish to thank the investigators, staff, and participants of the VERTIS CV trial (protocol B1521021), as well as Susan Huyck, Philip Jones, and Jennifer Yu for their critical review of this paper.
Funding
This study was sponsored by Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA in collaboration with Pfizer Inc., New York, NY, USA. Journal rapid service fees were funded by Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA in collaboration with Pfizer Inc., New York, NY, USA.
Medical Writing and Editorial Assistance
Medical writing support was provided by Diane Hoffman, PhD, of Engage Scientific Solutions and was funded by Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA, in collaboration with Pfizer Inc., New York, NY, USA.
Authorship
All named authors met the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Alexandra G. Palmer, Robert Frederich, and David E. Lawrence are employees of Pfizer and own stock and/or stock options in Pfizer Inc., New York, NY, USA. Jie Liu and Ira Gantz are employees of Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA (MSD) and may own stock in Merck & Co., Inc., Kenilworth, NJ, USA. Matthew J. Budoff received grant support from MSD and Pfizer Inc related to the VERTIS CV trial, and has received speaker fees from Pfizer Inc. Timothy M.E. Davis has served on advisory boards for, and received research funding, speaker fees, and travel assistance to attend meetings from, MSD; he was a VERTIS CV local investigator; and has served on advisory boards for, and received speaker fees and travel assistance to attend meetings from, AstraZeneca, Boehringer Ingelheim, and Novo Nordisk. Giuseppe Derosa has nothing to disclose.
Compliance with Ethics Guidelines
The protocol and informed consent documents were approved by the institutional review board or independent ethics committee at each participating site. The study was conducted in accordance with the ethical principles of the Declaration of Helsinki and in compliance with all International Council for Harmonisation Good Clinical Practice Guidelines. All participants signed informed consent forms (that were witnessed) before any screening procedures were conducted.
Data Availability
Upon request, and subject to certain criteria, conditions, and exceptions (see https://www.pfizer.com/science/clinical-trials/trial-data-and-results for more information) Pfizer will provide access to individual de-identified participant data from Pfizer-sponsored global interventional clinical studies conducted for medicines, vaccines, and medical devices (1) for indications that have been approved in the USA and/or EU or (2) in programs that have been terminated (i.e., development for all indications has been discontinued). Pfizer will also consider requests for the protocol, data dictionary, and statistical analysis plan. Data may be requested from Pfizer trials 24 months after study completion. The de-identified participant data will be made available to researchers whose proposals meet the research criteria and other conditions, and for which an exception does not apply, via a secure portal. To gain access, data requestors must enter into a data access agreement with Pfizer.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Budoff, M.J., Davis, T.M.E., Palmer, A.G. et al. Efficacy and Safety of Ertugliflozin in Patients with Type 2 Diabetes Inadequately Controlled by Metformin and Sulfonylurea: A Sub-Study of VERTIS CV. Diabetes Ther 12, 1279–1297 (2021). https://doi.org/10.1007/s13300-021-01033-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-021-01033-x