Abstract
Introduction
Pars plana vitrectomy (PPV) is considered to be an essential and effective surgical approach for the management of complications of diabetic retinopathy. Given the high rate of accelerated cataract progression after PPV, PPV combined with cataract surgery appears to be an attractive treatment option for patients with diabetes. However, this combined surgical approach remains controversial in terms of effectiveness and safety. We have therefore conducted a meta-analysis to evaluate the treatment outcome of PPV with or without cataract surgery.
Methods
A systematic search of three electronic databases (PubMed, Web of Science, and the Cochrane Library) was performed to identify relevant articles, using the key words “pars plana vitrectomy,” “cataract,” and “diabetic retinopathy.” Main outcome measures included the final visual acuity and postoperative complications. The incidence of postoperative complications was pooled using odds ratio (OR) with 95% confidence intervals in a random effect model.
Results
Ultimately, one randomized controlled trial (RCT) and four high-quality retrospective studies met the inclusion criteria and were included in the meta-analysis. In four of these studies, final visual acuity did not vary significantly between patients undergoing PPV alone and those undergoing PPV combined with cataract surgery (combined surgery). Only one study reported better visual improvement in the combined treatment group. Our analysis also showed that most phakic eyes after PPV had cataract progression with varying degrees. In addition, patients receiving PPV alone had a lower risk of neovascular glaucoma (OR 0.36; P < 0.05), iris synechias to anterior capsule (OR 0.36; P < 0.05), and iris rubeosis (OR 0.26; P < 0.05) compared with those receiving combined surgery.
Conclusion
Overall, our findings show that PPV combined with cataract surgery achieved good outcomes without a substantial increased risk to visual acuity or most complications. Given the high rates of cataract progression after PPV, combined surgery may be the more appropriate treatment for patients with diabetes and coexistent visually significant cataract.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Introduction
Diabetic retinopathy is the most common microvascular complication of diabetes and is also the leading cause of blindness in patients with diabetes [1]. Pars plana vitrectomy (PPV) has been the most widely performed ophthalmic procedure since its inception in the early 1970s and is considered to be an essential and effective procedure for the management of complications of diabetic retinopathy [2].
Cataract is also believed to be a major cause of blindness globally [3]. A higher incidence of senile cataract is commonly observed in patients with diabetes [4] and, additionally, accelerated cataract progression is the most common complication in phakic eyes receiving vitrectomy [5, 6]. Hence, the management of the lens in diabetic eyes undergoing vitrectomy has long been a source of controversy. Consequently, there is interest in determining the effectiveness and safety of PPV combined with cataract surgery (combined surgery) for the management of diabetic retinopathy in patients with diabetes.
Initially, many concerns were voiced about a higher risk for the progression of diabetic retinopathy following cataract extraction, with the lens being regarded as a protective barrier to reduce the risk of anterior segment neovascularization [7,8,9]. Hence, many surgeons attempt to spare the lens during vitrectomy. However, additional surgical challenges for cataract surgery appear after vitrectomy owing to the deep anterior chambers, zonular dehiscence, and increased inflammation of the affected eye [10,11,12]. Moreover, there have been remarkable advances in surgical techniques, instrumentation, and experience, and recent studies have shown good surgical and functional outcomes in patients receiving PPV combined with cataract surgery [13,14,15]. In this context, combined surgery may be a more advisable option for patients with diabetes.
To date, it has not been well established whether PPV combined with cataract surgery would contribute to better clinical outcomes compared with PPV alone. Thus, we conducted a meta-analysis to evaluate the treatment outcome of PPV with or without cataract surgery.
Methods
Search Strategy
The review is reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [16]. We conducted a systematic search of the websites PubMed, Web of Science, and the Cochrane Library to identify relevant available articles published up to April 2019. The search terms used were “pars plana vitrectomy,” “cataract,” and “diabetic retinopathy.” The language was restricted to English. We also reviewed reference lists from retrieved articles in an attempt to identify other potentially relevant studies.
Inclusion Criteria
The inclusion criteria were: (1) randomized controlled trials (RCTs) or high-quality comparative studies; (2) studies that compared the therapeutic effects of PPV alone versus PPV combined with cataract surgery in patients with diabetes; and (3) all studies that contained adequate informative data, such as postoperative complications and final visual acuity. A noncomparative, single-arm study that was identified during the systematic search was not included in the meta-analysis, nor were case reports, abstracts, reviews, and reports with incomplete data. If different publications based on the same study subjects were available, the most recent one was included.
Data Extraction
For each study, the following data were independently extracted by two reviewers: name of the first author, year of publication, location of the study, study design, origin of the study, number of eyes, mean age, lens status, and indications for surgery. Data on treatment outcomes in terms of postoperative complications and final visual acuity were also extracted. Any disagreement was resolved through discussion by the two reviewers.
Qualitative Assessment
The quality of the one RCT identified as relevant to the study was assessed according to the Cochrane Collaboration’s tool [17]. We carefully assessed the following characteristics for biases: random sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective reporting (reporting bias), and other factors that contribute to biases. In addition, the modified Newcastle–Ottawa Scale (NOS) was used to perform the quality assessment of retrospective studies [18]; this scale consists of three parts, namely, patient selection, outcome assessment, and comparability.
Statistical Analyses
Statistical analyses were performed using the Cochrane Review Manager (RevMan, version 5.2) software. An odds ratio (OR) with corresponding 95% confidence interval (CI) was used to evaluate the incidence of postoperative complications in a random effects model, and P < 0.05 was considered to be statistically significant. The between-study heterogeneity was tested using the Chi-square test and the I2 statistic, whereby I2 > 50% was taken to indicate substantial heterogeneity among studies. Sensitivity analyses were also conducted, and the influence of a single study on the pooled effect was examined by removing one study at a time, which is referred to as the leave-one-study-out method.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not involve any new studies of human or animal subjects performed by any of the authors.
Results
Search Outcomes
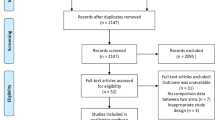
The selection process for the inclusion of studies in this meta-analysis is summarized in Fig. 1. A total of 535 studies that were potentially relevant were identified by the electronic search of the three databases. After excluding duplicate studies, we retrieved 502 articles, of which we screened the titles and abstracts, consequently identifying 14 studies for further assessment and a full-text review. Among these 14 articles, three were excluded due to providing insufficient data and six were excluded because they did not directly compare PPV without cataract surgery to PPV combined with cataract surgery. Ultimately, five studies [19,20,21,22,23] met the inclusion criteria and were included in the meta-analysis.
Characteristics of the Studies
Among the five studies included in the meta-analysis, one was conducted in Taiwan, two were conducted in Korea, and two were conducted in the USA. Of these, one was an RCT, one was a prospective study, and three were retrospective studies. In total, data from 747 eyes were available for the meta-analysis. A total of 325 and 422 eyes underwent PPV alone and PPV combined with cataract surgery, respectively. Detailed characteristics of the included studies are shown in Table 1.
Visual Outcomes
Compared with visual acuity at baseline, postoperative visual acuity improved in both the PPV group and PPV combined with cataract group in all studies. In four of the studies, no statistically significant final vision improvement was observed between the two groups. Only one study showed that more eyes in the combined group achieved a better vision improvement, compared with those in the PPV alone group [23].
Cataract Progression
Among the five studies included in this meta-analysis, three articles reported cataract progression within the PPV group. One study reported that 64% of phakic eyes had cataract progression, of which 39% required subsequent cataract surgery within the 4-year follow-up period [22]. In another study, of the 21 phakic eyes, 13 remained clear, six had minor opacities, and the remaining two had major cataracts [21]. In addition, Tseng et al.’s study reported that 20 of 26 eyes whose lens were clear at baseline developed nuclear or posterior subcapsular cataracts after PPV, and almost all eyes with cataracts in the PPV alone group showed the progression of cataract after surgery [23].
Complications
All studies examined the occurrence of any adverse events (change in intraocular pressure, anterior segment complications, and posterior segment complications) within the PPV alone group and PPV combined with cataract surgery group (Fig. 2). Three studies [21,22,23] reported the occurrence of neovascular glaucoma (NVG), and the pooled estimate showed a lower risk in the PPV alone group than in the PPV combined with cataract surgery group (OR 0.36, 95% CI 0.13–0.97; P < 0.05). One study [21] also provided data on the rates of iris rubeosis, with the authors reporting that the risk of this condition was significantly lower in the PPV alone group than in the PPV combined with cataract surgery group (OR 0.26, 95% CI 0.08–0.88; P < 0.05). The complication of iris synechias to anterior capsule was reported in only one study [20], with the incidence being lower in the PPV alone group than in the PPV combined with cataract surgery group (OR 0.17, 95% CI 0.03–0.85; P < 0.05). In addition, there were no significant differences between the two groups in terms of the risk of other complications (P > 0.05).
Sensitivity Analysis
In this meta-analysis, statistical heterogeneity was found in terms of ocular hypertension (P = 0.007, I2 = 71%) and vitreous hemorrhage (VH) (P = 0.07, I2 = 63%). For the occurrence of ocular hypertension, the sensitivity analysis found that Blankenship’s study [21] was the likely source of heterogeneity. After excluding Blankenship’s study [21], the pooled OR was 0.88 (95% CI 0.40–1.94), with no evidence of heterogeneity (P = 0.18, I2 = 39%). The sensitivity analysis also found that the heterogeneity of VH was dependent on the inclusion of Tseng et al.’s study [23]. When this study was excluded from the meta-analysis, the pooled OR was 0.94 (95% CI 0.34–2.61), with no evidence of heterogeneity (P = 0.99, I2 = 0%). In addition, the results of the leave-one-out analysis showed that none of exclusions altered the results of the previous analyses, indicating the good reliability and stability of the results of this meta-analysis.
Discussion
In the present study we investigated the effect of combining cataract surgery with PPV on patients’ visual outcome. We found that patients receiving PPV combined with cataract surgery had similar visual outcomes as those receiving PPV alone, without any higher incidence of most postoperative complications. In addition, accelerated cataract development was observed in most phakic eyes receiving PPV. Hence, for patients with diabetes with significant cataract, PPV combined with cataract surgery would be a safe procedure and may achieve more satisfactory results.
Vitrectomy is highly successful in achieving visual rehabilitation in patients with diabetic retinopathy [24, 25]. In our meta-analysis, similar vision improvement was observed in both the PPV alone and PPV combined with cataract surgery groups. Only one study reported a better visual outcome in the combined group, compared with the PPV alone group [23]. It should be noted that in this study, there were more cases with more significant cataract in the PPV combined with cataract surgery group, and this tendency may give more room for better vision improvement owing to the lens extraction. In addition, one study reported that the final visual outcomes did not differ substantially by different primary indications [22].
Cataract formation remains the most common complication of PPV in phakic eyes [26]. Similar to previous reports, our study showed that most of the phakic eyes in the PPV along group had cataract progression to some degree after vitreoretinal surgery. Possible reasons for cataract formation after PPV include altered lens permeability after gel removal, intraoperative oxidation of lens proteins, and altered metabolic characterization of aqueous humor [27, 28].
Postoperative hypotony is considered to be a common occurrence after vitrectomy [29, 30]. It is also believed that combined cataract and PPV treatment has a higher risk of hypotony since the removal of vitreous is usually more complete. In our study, there was no significant difference in the incidence of hypotony between the PPV alone group and the PPV combined with cataract surgery group. It has been proposed that combined surgery might lead to an increase in ciliary body thickness and a decrease in the angle opening, which would transiently increase the intraocular pressure (IOP) [20]. However, although combined surgery is associated with a higher risk of IOP elevation, the rate of the IOP spike has been found not be differ between patients receiving PPV alone and those receiving PPV combined with cataract surgery. Therefore, combined surgery may be safe in terms of maintenance of a stable postoperative IOP.
The initial rationale for lens-sparing diabetic vitrectomy was the apparent lower rate of anterior segment neovascularization. Early studies found that the incidence of iris rubeosis was higher in eyes undergoing PPV combined with cataract surgery than in those undergoing PPV alone [5, 7]. However, the advent of posterior segment visualization and the development of more refined surgical techniques, especially intraoperative laser photocoagulation, have played a major role in reducing this severe complication. In recent studies, the incidence of postoperative iris neovascularization was found to be relatively rare and did not differ between the vitrectomy alone group and the PPV combined with cataract surgery group [31, 32].
NVG is one of the most severe postoperative complications of PPV. Our study showed that the incidence of NVG was higher in the PPV combined with cataract surgery group than in the PPV alone group. It has been reported that the post-PPV aphakia is an independent risk factor for NVG [15, 33]. The lens is regarded as a protective barrier that reduces the diffusion of angiogenic factors from the posterior segment. Preoperative neovascularization of the angle, inadequate panretinal photocoagulation (PRP), and severe postoperative inflammation are also considered to be potential risk factors [34, 35]. Overall, for PPV combined with cataract surgery, it is recommended that surgeons be cautious in their evaluation of the retina and provide adequate PRP if there is an indication of active proliferative diabetic retinopathy or neovascularization, and patients should be regularly followed up for development of NVG.
Over the years, the anatomic and visual outcomes and postoperative complication rates have been generally unaffected by the lens status of the eye as a result of remarkable advances in surgical techniques, instrumentation, and experience. Given the accelerated cataract formation associated with vitrectomy, as well as the additional anesthetic risk for future cataract surgery, combined surgery may be more appropriate for patients with diabetes. Nevertheless, when considering the combined surgery approach, surgeons should pay attention to possible postoperative inflammation and complications which may arise due to the longer surgical time. With these findings in mind, the vitreoretinal surgeon should feel comfortable optimizing treatment strategy.
Our meta-analysis has a number of limitations. First, very few trials have been published on this issue—with only one RCT identified—which may have affected the results to some extent. Hence, further well-designed studies with large samples are needed to substantiate the present results. Second, some studies included in the meta-analysis were relatively dated, and the relatively old-fashioned surgical methods and strategies reported in these studies may have increased the risk of postoperative complications—although the sensitivity analysis pointed to a good reliability and stability of the results of this meta-analysis. Third, the results evaluating NVG and VH showed large heterogeneity.
Conclusion
In conclusion, this meta-analysis compared the therapeutic effect of PPV with or without cataract surgery. Our study showed that there was no significant difference between the two treatment groups in terms of final visual improvement and most postoperative complications. Given the high rates of cataract progression and the additional challenge of cataract surgery after vitrectomy, the PPV combined with cataract surgery approach may be safe and more appropriate for patients with significant cataract and coexisting vitreoretinal diseases. Large randomized and prospective studies are required to refine our conclusions and evaluate the long-term effect of the PPV combined with cataract surgery approach in patients with diabetes.
References
Heng LZ, Comyn O, Peto T, et al. Diabetic retinopathy: pathogenesis, clinical grading, management and future developments. Diabet Med. 2013;30(6):640–50.
Smiddy WE, Flynn HW Jr. Vitrectomy in the management of diabetic retinopathy. Surv Ophthalmol. 1999;43(6):491–507.
Livingston PM, Carson CA, Taylor HR. The epidemiology of cataract: a review of the literature. Ophthalmic Epidemiol. 1995;2(3):151–64.
Cherfan GM, Michels RG, de Bustros S, Enger C, Glaser BM. Nuclear sclerotic cataract after vitrectomy for idiopathic epiretinal membranes causing macular pucker. Am J Ophthalmol. 1991;111(4):434–8.
Schachat AP, Oyakawa RT, Michels RG, Rice TA. Complications of vitreous surgery for diabetic retinopathy. II. Postoperative complications. Ophthalmology. 1983;90(5):522–30.
Melberg NS, Thomas MA. Nuclear sclerotic cataract after vitrectomy in patients younger than 50 years of age. Ophthalmology. 1995;102(10):1466–71.
Blankenship G, Cortez R, Machemer R. The lens and pars plana vitrectomy for diabetic retinopathy complications. Arch Ophthalmol. 1979;97(7):1263–7.
Thompson JT, Glaser BM. Effect of lensectomy on the movement of tracers from vitreous to aqueous. Arch Ophthalmol. 1984;102(7):1077–8.
Thompson JT, Glaser BM. Role of lensectomy and posterior capsule in movement of tracers from vitreous to aqueous. Arch Ophthalmol. 1985;103(3):420–1.
Biro Z, Kovacs B. Results of cataract surgery in previously vitrectomized eyes. J Cataract Refract Surg. 2002;28(6):1003–6.
Meyers SM, Klein R, Chandra S, Myers FL. Unplanned extracapsular cataract extraction in postvitrectomy eyes. Am J Ophthalmol. 1978;86(5):624–6.
Steel DH. Cataract surgery after diabetic vitrectomy. Acta Ophthalmol. 2015;93(2):e168.
Goto A, Inatani M, Inoue T, et al. Frequency and risk factors for neovascular glaucoma after vitrectomy in eyes with proliferative diabetic retinopathy. J Glaucoma. 2013;22(7):572–6.
Azzolini C, Brancato R, Camesasca FI, Codenotti M. Influence of silicone oil on iris microangiopathy in diabetic vitrectomized eyes. Ophthalmology. 1993;100(8):1152–8 (Discussion 8–9).
Lahey JM, Francis RR, Kearney JJ. Combining phacoemulsification with pars plana vitrectomy in patients with proliferative diabetic retinopathy: a series of 223 cases. Ophthalmology. 2003;110(7):1335–9.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Higgins JP, Altman DG, Gotzsche PC, et al. The cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5.
Lee JY, Jeong HS, Lee DY, Sohn HJ, Nam DH. Early postoperative intraocular pressure stability after combined 23-gauge sutureless vitrectomy and cataract surgery in patients with proliferative diabetic retinopathy. Retina. 2012;32(9):1767–74.
Park SP, Ahn JK, Lee GH. Morphologic changes in the anterior segment after phacovitrectomy for proliferative diabetic retinopathy. J Cataract Refract Surg. 2009;35(5):868–73.
Blankenship GW. The lens influence on diabetic vitrectomy results. Report of a prospective randomized study. Arch Ophthalmol. 1980;98(12):2196–8.
Silva PS, Diala PA, Hamam RN, et al. Visual outcomes from pars plana vitrectomy versus combined pars plana vitrectomy, phacoemulsification, and intraocular lens implantation in patients with diabetes. Retina. 2014;34(10):1960–8.
Tseng HY, Wu WC, Hsu SY. Comparison of vitrectomy alone and combined vitrectomy, phacoemulsification and intraocular lens implantation for proliferative diabetic retinopathy. Kaohsiung J Med Sci. 2007;23(7):339–43.
Chung TY, Chung H, Lee JH. Combined surgery and sequential surgery comprising phacoemulsification, pars plana vitrectomy, and intraocular lens implantation: comparison of clinical outcomes. J Cataract Refract Surg. 2002;28(11):2001–5.
Demetriades AM, Gottsch JD, Thomsen R, et al. Combined phacoemulsification, intraocular lens implantation, and vitrectomy for eyes with coexisting cataract and vitreoretinal pathology. Am J Ophthalmol. 2003;135(3):291–6.
Shousha MA, Yoo SH. Cataract surgery after pars plana vitrectomy. Curr Opin Ophthalmol. 2010;21(1):45–9.
Hsuan JD, Brown NA, Bron AJ, Patel CK, Rosen PH. Posterior subcapsular and nuclear cataract after vitrectomy. J Cataract Refract Surg. 2001;27(3):437–44.
Ji Y, Rong X, Lu Y. Metabolic characterization of human aqueous humor in the cataract progression after pars plana vitrectomy. BMC Ophthalmol. 2018;18(1):63.
Gupta OP, Weichel ED, Regillo CD, et al. Postoperative complications associated with 25-gauge pars plana vitrectomy. Ophthalmic Surg Lasers Imaging. 2007;38(4):270–5.
Hsu J, Chen E, Gupta O, Fineman MS, Garg SJ, Regillo CD. Hypotony after 25-gauge vitrectomy using oblique versus direct cannula insertions in fluid-filled eyes. Retina. 2008;28(7):937–40.
Kadonosono K, Matsumoto S, Uchio E, Sugita M, Akura J, Ohno S. Iris neovascularization after vitrectomy combined with phacoemulsification and intraocular lens implantation for proliferative diabetic retinopathy. Ophthalmic Surg Lasers. 2001;32(1):19–24.
Honjo M, Ogura Y. Surgical results of pars plana vitrectomy combined with phacoemulsification and intraocular lens implantation for complications of proliferative diabetic retinopathy. Ophthalmic Surg Lasers. 1998;29(2):99–105.
Rice TA, Michels RG, Maguire MG, Rice EF. The effect of lensectomy on the incidence of iris neovascularization and neovascular glaucoma after vitrectomy for diabetic retinopathy. Am J Ophthalmol. 1983;95(1):1–11.
Ho PC, Tolentino FI. Bacterial endophthalmitis after closed vitrectomy. Arch Ophthalmol. 1984;102(2):207–10.
Wand M, Madigan JC, Gaudio AR, Sorokanich S. Neovascular glaucoma following pars plana vitrectomy for complications of diabetic retinopathy. Ophthalmic Surg. 1990;21(2):113–8.
Acknowledgements
Funding
This study was supported by the National Key R&D Program of China (NO. 2018YFA 0107304, 2017YFA 0105000) and the Plan For Scientific Innovation Talent of Henan Province (NO.184200510005). The Rapid Service Fee was funded by the authors.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions
Kang Xiao, Yi-chen Dong, Xin-guang Xiao, Shen-zhi Liang, Jiong Wang, Cheng Qian, and Guang-ming Wan were responsible for the conception and design of this meta-analysis, the acquisition of data, and the analysis and interpretation of that data; for drafting the initial manuscript; and for revising it critically for important intellectual content. Kang Xiao and Yi-chen Dong wrote the final draft of the manuscript and are co-first authors. All authors approved the final manuscript.
Disclosures
Kang Xiao, Yi-chen Dong, Xin-guang Xiao, Shen-Zhi Liang, Jiong Wang, Cheng Qian, Guang-Ming Wan have nothing to disclose.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced Digital Features
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.8920589.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Xiao, K., Dong, YC., Xiao, XG. et al. Effect of Pars Plana Vitrectomy With or Without Cataract Surgery in Patients with Diabetes: A Systematic Review and Meta-Analysis. Diabetes Ther 10, 1859–1868 (2019). https://doi.org/10.1007/s13300-019-0672-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-019-0672-9