Abstract
Introduction
Sodium-dependent glucose transporter-2 (SGLT2) inhibitors such as dapagliflozin induce weight loss, but the mechanism is thought to involve loss of both body fat and skeletal muscle mass. The decrease in skeletal muscle mass may lead to worsening of insulin resistance in type 2 diabetes patients. On the other hand, formula diet (FD) is a low-calorie food containing low carbohydrates, low fat, and sufficient protein, vitamins, and minerals to support a healthy and balanced diet, and is used for the treatment of obesity or diabetes. Therefore, we examine whether the protein supplementation is superior to the fat supplementation in metabolic improvement of the poorly controlled type 2 diabetes patients treated with SGLT2 inhibitor. We compare the therapeutic effects using two types of FD; a high protein FD and a high fat FD. Patients are prescribed dapagliflozin and replacement of one of three meals with FD. We compare high protein FD and high fat FD with respect to improvement of glycemic control while maintaining skeletal muscle mass.
Methods
We conduct a prospective, multicenter, double-blinded, randomized, controlled, investigator-initiated clinical trial. Patients who satisfy the eligibility criteria will be randomized to two groups (1:1) and prescribed 5 mg of dapagliflozin once daily together with a high protein FD or high fat FD (same number of calories) to replace one of three meals a day (one meal with FD only and two normal meals). The observation period for both groups is 24 weeks. The primary endpoint is the change in HbA1c.
Planned Outcomes
This study is ongoing and scheduled to complete in June 2019. The findings of this study will be disseminated through peer-reviewed publications and conference presentations.
Trial Registration
University Hospital Medical Information Network (UMIN) 000024580.
Funding
This study was carried out under contract with the specified nonprofit corporation Hokkaido Institute of Health Sciences, based on a grant from AstraZeneca Co., Ltd. and Ono Pharmaceutical Co., Ltd. for an investigator-initiated clinical trial. The authors funded the journals article processing charges.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
While diet and exercise therapy are certainly important for the treatment of diabetes, nutritionally balanced calorie restriction is essential. However, calorie restriction depends on individuals and is difficult to implement for diabetes patients, especially outpatients. Caloric restriction is also indispensable for the treatment of obesity, but severe calorie restriction in the form of starvation therapy with insufficient intake of protein, vitamins, and minerals is harmful, because muscular catabolism may develop.
For this reason, formula diet (FD) was developed as an extremely low-calorie food for treating severe obesity. An FD consists of low carbohydrate, low fat, and sufficient protein, vitamins, and minerals to support a healthy and balanced diet. The usefulness and safety of FD have been reported in many articles [1,2,3,4,5,6,7,8,9,10].
We previously reported the effect of FD in type 2 diabetes patients. Replacing one of three meals with FD reduced body weight, visceral fat mass, HbA1c, and systolic blood pressure, and increased HDL-cholesterol [11]. These data suggest that apart from calorie restriction, protein supplementation is preferable for patients with type 2 diabetes because of the effects of weight loss and visceral fat loss with possibly maintenance of the skeletal muscle mass.
In recent years, sodium-dependent glucose transporter-2 (SGLT2) inhibitors such as dapagliflozin have been widely used as antidiabetic drugs. These inhibitors have a novel glucose-lowering mechanism that does not depend on insulin secretion. The basic pharmacological effect of SGLT2 inhibitors is promotion of glucose excretion in urine. From the viewpoint of diet therapy, the use of SGLT2 inhibitors corresponds to a decrease of approximately 300 kcal per day due to accelerated urinary excretion of glucose, potentially achieving a condition resembling carbohydrate restriction [12]. In addition, administration of SGLT2 inhibitors increases gluconeogenesis in the liver with loss of glucose from the kidney. On the other hand, fat and muscle are catabolized and ketone bodies are elevated. Thus, the weight loss effect of SGLT2 inhibitors is thought to involve loss of both fat and muscle. In fact, it has been reported that not only fat but also skeletal muscle mass decreases when SGLT2 inhibitor tofogliflozin is administered to mice to which a high fat diet has been administered [13]. It has also been reported that both fat and lean mass decrease when dapagliflozin is administered to patients with type 2 diabetes who are on metformin [14, 15]. Although SGLT2 inhibitors are thought to improve insulin sensitivity [16, 17], there is also a possibility of worsening insulin sensitivity from the viewpoint of skeletal muscle reduction.
Therefore, we examine whether the protein supplementation is superior to the fat supplementation in metabolic improvement of the poorly controlled type 2 diabetes patients treated with SGLT2 inhibitor. The mechanistic assumption is that protein supplementation prevents skeletal muscle loss by promoting only fat burning and improves basal metabolism and insulin resistance through retaining skeletal muscle mass. To prove this hypothesis, we compare the therapeutic effects using two types of FD, a high protein FD and a high fat FD.
Objectives
We aim to evaluate the effects of concomitant use of FD with an SGLT2 inhibitor (dapagliflozin) on body composition and metabolic improvement as well as safety in patients with type 2 diabetes mellitus (Diet-Dapper study). We prescribe 5 mg daily of dapagliflozin, which is the initial dose for the treatment of type 2 diabetes in Japan, and FD (to replace one of three meals in a day) to patients with poorly controlled type 2 diabetes. Then we compare the effects of high protein FD and high fat FD with respect to improving glycemic control and insulin resistance while maintaining skeletal muscle mass.
Methods
Study Design
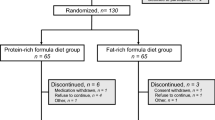
The study design is a prospective, multicenter, double-blinded, randomized, controlled, investigator-initiated clinical trial. Subjects are randomized to two groups: high protein FD (group A) and high fat FD (group B). The two FD have the same number of calories (182 kcal) and are started simultaneously with dapagliflozin. In group A, patients take 5 mg of dapagliflozin orally once daily and replace one meal with a high protein FD while taking two normal meals a day. In group B, patients take dapagliflozin 5 mg orally once daily and replace one meal with a high fat FD while taking two normal meals a day. The observation period for both groups is 24 weeks. Patients are recruited from seven facilities participating in this study. Eligible patients who provide written informed consent are randomized to group A or group B at a ratio of 1: 1 by a computer program located at the registration center, using a minimization method balancing age (≤ 65 or > 65 years), HbA1c level (≤ 8.0 or > 8.0%), and waist circumference (men, ≤ 85 or > 85 cm; women, ≤ 80 or > 80 cm) at the time of screening (Fig. 1).
Sample Size Calculation
The primary endpoint of this study is the change in HbA1c. Shirai et al. [11] reported a change in HbA1c of − 0.6 ± 1.1% using a high protein FD. According to a domestic phase III clinical trial of dapagliflozin, the change in HbA1c after 24-week treatment with dapagliflozin is − 0.4% ± 0.7%. Although there is no report on high fat FD, the protein/fat/carbohydrate (P/F/C) ratio per day in group B is not so different from conventional Japanese food. We thus estimate that dapagliflozin treatment will result in the same level of change in group B. Assuming that an additive effect is obtained in group A using a high protein FD and dapagliflozin, the change in HbA1c at 24 week is estimated to be − 1.0%. In group B using a high fat FD and dapagliflozin, the change in HbA1c will be similar to that of the domestic phase III clinical trial of dapagliflozin and is estimated to be − 0.6%. The standard deviation of the change in HbA1c is presumed to be 0.8%, which is the range in general clinical studies. At a significance level (α) of 0.05 and a detection power [100(1 − β)] of 80%, the number of cases per group necessary to detect a significant difference in change in HbA1c between the two groups is calculated to be 64 cases. Assuming 5% deviant and omission samples, the target number of cases for each group is 68 cases, with a total of 138 participants in this study.
FD and Calorie Intake
Sunny Health Co., Ltd. is the manufacturer and distributor of the FD. The number of calories of a normal meal (conventional Japanese food) is calculated by 35 kcal/kg × standard body weight (kg). We assume that the standard body weight is equivalent to a body mass index (BMI) of 22 kg/m2. For example, if the patient’s standard body weight is 60 kg, a 35 kcal/kg meal would be 2100 kcal per day, which is equivalent to 700 kcal per meal. Therefore, if the subject takes FD (182 kcal) once a day and a normal meal of 700 kcal twice a day, the total calorie will be 1582 kcal per day, which is equivalent to 26.4 kcal/kg.
The protein components of FD consist of egg white, casein, and soybean protein. The P/F/C ratio is approximately 42:12:46 for the high protein FD (group A) and 2:55:43 for the high fat FD (group B). When the subject’s standard body weight is 60 kg, the overall P/F/C balance is 21:24:56 for group A and 16/28/56 for group B.
Since the height and standard body weight of each subject differ, the P/F/C ratio also differs among subjects, but the errors are acceptable. For example, when the height of the subject is 140 cm vs. 190 cm, the P/F/C balance in the high protein FD group is 22:23:55 vs. 20:24:56, and that in the high fat FD is 16:29:55 vs. 17:27:56.
The FD is reconstituted in a 600-ml dedicated shaker. A package of the FD together and 350–400 ml of water are shaken well before consumption. On weeks 0 and 12, subjects receive instructions on how to use the formula diet and nutritional guidance about calorie intake from a nutritionist at each facility. In the absence of a nutritionist, the instructions are given by nurses.
When a low carbohydrate diet is given to a patient using SGLT2 inhibitors, the onset of diabetic ketoacidosis (DKA) is a concern. In this study, we use FD which is a low-calorie diet itself, but the use of FD is limited to one pack per day. For the remaining two meals, nutritional guidance targeting 35 kcal/kg is given, and considering on a per day basis, both groups will take about 25 kcal/kg. Also, carbohydrates are taken at about 56% according to P/F/C ratio. A low carbohydrate diet of less than 50 g per day is considered to be a ketogenic diet [18]. The daily calorie intake of participants in this study is determined by the height of the individual, but even a person with a height of 140 cm has about 160 g of carbohydrates intake per day. Therefore, we consider that diet therapy in this study is not an intense carbohydrate-restricted diet even considering urine glucose excreted by treatment with dapagliflozin. Also, blood and urinary ketone bodies are monitored during the observation period.
Eligibility Criteria
Inclusion Criteria
Eligible patients are type 2 diabetes patients who satisfy all of the following selection criteria: (1) aged between 20 and 75 years when providing consent; (2) HbA1c in the range of 7.0% to 8.5%; (3) BMI > 22 kg/m2, (4) estimated glomerular filtration rate (eGFR) > 50 ml/min/1.73 m2; (5) patients who have adequate understanding of the study contents upon receiving detailed explanations based on the written consent form, and give written informed consent of their own free will.
Exclusion Criteria
Patients who meet any of the following exclusion criteria will be excluded from this study: (1) type 1 diabetes; (2) use of SGLT2 inhibitors within the previous 3 months; (3) hypersensitivity to the drug component; (4) severe ketosis, diabetic coma or pre-coma; (5) treated with insulin; (6) determined by the investigator as inappropriate to participate in the study; (7) eGFR less than 45 ml/min/1.73 m2; (8) planning to become pregnant; (9) pregnant, possibly pregnant, or breast-feeding; (10) severe infectious disease, severe trauma, preoperative or postoperative patient; (11) allergy to the ingredients of the FD (soybeans, eggs, yeasts, and milk).
Study Setting
This study is conducted at Toho University Sakura Medical Center and six other hospitals or clinics. Participating facilities are listed in https://upload.umin.ac.jp/cgi-open-bin/ctr/ctr_view.cgi?recptno=R000028290. This study was registered in the University Hospital Medical Information Network (UMIN) Clinical Trials Registry (UMIN000024580) on March 1, 2017. The trial is ongoing and is scheduled to be completed in June 2019.
Blinding
This study is conducted with a double-blind design, and blinding is maintained throughout the study for all research stakeholders except the allocation officer through the following procedures. The investigator fills in the necessary information of a potential subject in the case registration card using subject identification number and transmits by facsimile to the research support organization (Ibec Corporation, Osaka, Japan). The allocation officer of the research support organization confirms eligibility of the potential subject. When eligibility is confirmed, the allocation officer randomizes the subject according to an allocation table consisting of the serial number, the test food group identification number in random order, and the test food allocation code. The allocation officer replies by facsimile to the investigators regarding the results of eligibility and randomization. The allocation officer ensures that the appearance of the test food, the packaging, and the indications on the label of the two FD are indistinguishable. The allocation officer keeps the allocation table sealed until the key is opened, and does not disclose it to other related persons involved in the study except during emergency. When unused test food is collected before key opening, the food is collected in a sealed state to maintain blindness.
Intervention
After registration and randomization, dapagliflozin 5 mg is taken orally once daily for 24 weeks. In principle, a daily dose of 5 mg is taken, but if HbA1c exceeds 8.5%, the dose may be increased to 10 mg at the investigator’s discretion. At the same time, the subjects take a high protein or high fat FD to replace one of the three meals a day.
The schedule of study visits and data collection is summarized in Table 1.
Treatment Compliance
The investigators confirm the status of compliance to medication and test food intake at each visit and instruct the subjects to bring empty packages of the test food and unused test food at the next visit.
Concomitant Medication
In principle, treatments for diabetes, hypertension, dyslipidemia, and hyperuricemia are not changed from the time of obtaining consent to the completion of study, to avoid effects on the efficacy and safety assessments of this study. However, changes are permitted when the glucose level improves markedly owing to sufficient weight loss or when the onset of hypoglycemic attacks is a concern. If it is judged that adding a new antidiabetic drug is necessary because of insufficient therapeutic effect, the trial will be discontinued at that time. If treatment is changed, the contents of change and the reason and timing are described in the case report form.
Outcomes
The primary endpoint is the change in HbA1c from the start of treatment to 24 weeks after initiation of treatment, and is compared between the two groups. Secondary endpoints are the rates of change in (1) body weight and BMI; (2) blood pressure and heart rate; (3) waist circumference; (4) fasting blood glucose level and insulin level for the calculation of homeostatic model assessment (HOMA)-β and HOMA-R; (5) serum lipid levels (total cholesterol, LDL-cholesterol calculated using the Friedewald equation, fasting triglyceride, HDL-cholesterol); (6) ketone fraction (venous blood); (7) lipid-related parameters [pre-heparin lipoprotein lipase (LPL) protein, lipoprotein fraction (polyacrylamide gel electrophoresis), remnant-like lipoprotein cholesterol, apoprotein (Apo A1, A2, B, C2, C3, E)]; (8) high sensitivity C-reactive protein (hs-CRP); (9) urinary albumin quantification; (10) ankle brachial index (ABI) and cardio-ankle vascular index (CAVI) as a marker of arterial stiffness (only when measurement is possible), (11) body composition (only when measurement is possible). Insulin, ketone fraction, lipid-related parameters, and hs-CRP will be measured at a central laboratory (LSI Medience Corporation, Tokyo, Japan). ABI and CAVI are measured using the VaSera series (FUKUDA DENSHI, Tokyo, Japan). Body composition is evaluated by the InBody series (Biospace, Tokyo, Japan) that performs multifrequency bioelectrical impedance analysis. Serious adverse events (AEs) will be documented and reported per regulatory requirements.
CAVI
A novel arterial stiffness diagnostic parameter called CAVI has been developed in Japan, which essentially reflects the stiffness of the aorta, femoral artery, and tibial artery [19]. This stiffness parameter has been reported to be less affected by blood pressure at the time of measurement and adequately reproducible for clinical use [20, 21]. CAVI is also known to be associated with traditional parameters of vascular structure and function, such as intima–media thickness (IMT), pulse wave velocity (PWV), and central augmentation index [22]. Furthermore, no special technique is required for the measurement of CAVI. CAVI has been associated with a number of risk factors for cardiovascular disease (CVD) and the severity of CVD [23,24,25,26,27]. An increase in number of risk factors for metabolic syndrome also correlates positively with increased CAVI, probably as a result of insulin resistance [28].
Body Composition Measurement
Body fat is measured by bioelectrical impedance analysis (BIA) using Inbody. The BIA method is noninvasive and easy to measure and is more convenient and effective when measuring multiple times. The BIA method measures the resistance (impedance) of a body by applying a weak and noninvasive current to the body. Since the muscle contains water that readily conducts electricity, the impedance decreases as the amount of muscle increases, and conversely the impedance increases as fat increases. Impedance in the body is measured and the impedance index is calculated by an established formula [29]. Body water content is calculated from this impedance index, and lean body mass is determined on the basis of the fact that approximately 73% of the fat-free mass is body water. Further, the body fat mass is obtained by subtracting the fat-free mass from the body weight.
Data Management, Monitoring, Safety, and Auditing
The investigators will maintain the records of individual patients as source data, which include a log of informed consent forms, medical history, laboratory data, and other records, as appropriate. All entries in the case report forms (CRFs) should be backed up by the relevant source data. CRFs must be completed in a timely manner.
All data will be collected by the data management center. There will be no direct communication between investigators and data managers. Clinical data entry, coding, data management and reporting will be performed by the research support organization, with reading and visual check, and a data clarification form (DCF) is issued if there is inconsistency.
Monitoring and auditing of this research will be conducted by Clinical Research Office Corporation (Kanagawa, Japan). Monitors will ensure that the investigational team complies with the study protocol, that data and AEs are accurately recorded in the CRFs, that severe AEs are forwarded to the trial coordinator and the investigational drug provider, and that those meeting reporting criteria are forwarded to the institutional review board (IRB).
When AEs occur, the investigators immediately take appropriate measures and describe the AEs in the medical record and CRFs without inconsistency. For investigation of adverse events, the investigators conduct follow-up until the subjects recover to the state before initiation of treatment and confirm the outcomes. If the follow-up cannot be performed for any reason, this should be described in the CRFs and the investigation will be terminated.
In the case that identification of the test food is necessary to avert an emergency, the investigator (or the subinvestigator if the investigator is absent) at the study site requests unblinding of the allocation code by the test food allocation manager, through the principal investigator, and receives the result of disclosure for that case. Disclosure of information after emergency code opening is determined elsewhere.
Audit personnel are independent of those that perform monitoring and quality control. The person in charge of auditing conducts audits for quality assurance in accordance with the audit procedures prepared prior to implementation of audit.
Statistical Analysis
Analyses of primary and secondary endpoints are performed using full analysis set (FAS) and per protocol set (PPS). As a rule, analyses are carried out under the condition of a 95% confidence interval (CI). A medical statistician prepares a statistical analysis plan and specifies details of the statistical methods including data handling. The statistical analysis plan is prepared before data fixation.
Subject to patient consent regarding use of the analytical data, the statistician checks the data of individual patients for any deviation from the protocol and the degree of deviation, as well as any dropout from the study and the timing of dropout. The statistician then defines the following three sets to be analyzed. The FAS contains cases that satisfy the following: (i) diagnosed as type 2 diabetes, (ii) randomized and received test treatment at least once, (iii) has data on efficacy after starting the study. The PPS contains cases showing no violations of selection criteria, exclusion criteria violation, and concomitant drug, with compliance not less than 75% and not more than 120%. The safety analysis set contains cases that are enrolled in the study and have started and received a part or all the test treatments.
Summary statistics of the background data are calculated for the test groups. Nominal variables are expressed as frequency or percentage of each category. Summary statistics (number of cases, mean, standard deviation, minimum, median, and maximum) are calculated for continuous variables. Patient characteristics are compared using a χ2 test or Fisher’s exact test for categorical variables, and Student’s t test or Wilcoxon rank sum test for continuous variables. In the analyses of primary and secondary outcomes, summary statistics (number of cases, mean, standard deviation, minimum, median, and maximum) are calculated for the measured values, the amount of change, and the rate of change for each evaluation item. The amount of change and the rate of change are compared using one-sample t test for intragroup comparison and two-sample t test for intergroup comparison. The correlation between HbA1c and each variable is then evaluated using Pearson’s moment correlation coefficient or Spearman’s rank correlation coefficient.
Strengths and Limitations
This study is the first double-blind randomized controlled trial to assess the efficacy of formula diet in patients with type 2 diabetes using the SGLT2 inhibitor dapagliflozin. The design of this study aims to provide evidence for the importance of protein supplementation when using SGLT2 inhibitors for the treatment of type 2 diabetes, from the viewpoint of insulin resistance improvement and skeletal muscle maintenance. Noninvasive tests such as CAVI as a marker of vascular elasticity and bioelectrical impedance analysis for evaluation of body composition are used.
There are some limitations in this study. In order to verify whether FD provides adjunct benefit in patients treated with SGLT2 inhibitor, the study needs to randomize patients to (1) no treatment; (2) FD alone; (3) dapagliflozin alone; (4) dapagliflozin and FD. However, the current protocol has only two groups: dapagliflozin and high protein FD or dapagliflozin and high fat FD because of the limited numbers of type 2 diabetes subjects and the limited funding for our research. Other potential limitations of the trial include a study population of mostly Japanese and a short follow-up period.
Ethics and Dissemination
Research Ethics Approval and Protocol Amendments
The trial was approved by the IRB at each of the participating institutions and will be conducted in accordance with the Declaration of Helsinki. The IRBs are as follows: Toho University Sakura Medical Center Ethics Committee (ID number: S16101), Shin-Oyama City Hospital Center Ethics Committee. Other facilities were judged at the centralized IRB. Substantial amendments of the study protocol must be approved by the IRBs.
Informed Consent
The investigator provides each potential subject with an informed consent form/information sheet that has been approved by the IRB, explains the contents of the study in detail both in writing and orally, and obtains the subject’s written consent of his/her own free will. When efficacy and safety information that may potentially affect the subject’s consent is obtained or when the protocol is changed, the investigator will promptly inform the subject and confirm the intention of the subject on whether to participate in the study. At the same time, the investigator will revise the informed consent form/information sheet with prior approval by the IRB of each study facility, and obtain informed consent again from the subject.
Confidentiality
Subject ID numbers unrelated to the subjects’ personal information are assigned at the time of case registration, and are used when handling samples and information related to the study to maintain anonymity of the materials. For anonymization, an anonymized table is prepared, and the investigator supervises to ensure that the anonymized table is stored securely.
Dissemination
The findings of this study will be disseminated through peer-reviewed publications and conference presentations.
Change history
12 February 2020
In the original article, the 6th sentence of the section ���FD and calorie intake��� is incorrect. The correct sentence is ���The protein component of FD consists of whey protein, casein, and soy protein���.
12 February 2020
In the original article, the 6th sentence of the section ���FD and calorie intake��� is incorrect. The correct sentence is ���The protein component of FD consists of whey protein, casein, and soy protein���.
References
Bistrian BR. Clinical use of a protein-sparing modified fast. JAMA. 1978;240(21):2299–302.
Saito Y, Ishikawa Y, Shinomiya M, Shirai K, Yoshida S. Effects of protein-sparing modified fasting on obese Japanese patients. J Clin Biochem Nutr. 1987;2(1):91–100.
Heymsfield SB, van Mierlo CA, van der Knaap HC, Heo M, Frier HI. Weight management using a meal replacement strategy: meta and pooling analysis from six studies. Int J Obes Relat Metab Disord. 2003;27(5):537–49.
Allison DB, Gadbury G, Schwartz LG, et al. A novel soy-based meal replacement formula for weight loss among obese individuals: a randomized controlled clinical trial. Eur J Clin Nutr. 2003;57(4):514–22.
Vazquez C, Montagna C, Alcaraz F, et al. Meal replacement with a low-calorie diet formula in weight loss maintenance after weight loss induction with diet alone. Eur J Clin Nutr. 2009;63(10):1226–32.
Kempf K, Schloot NC, Gartner B, Keil R, Schadewaldt P, Martin S. Meal replacement reduces insulin requirement, HbA1c and weight long-term in type 2 diabetes patients with > 100 U insulin per day. J Hum Nutr Diet. 2014;27(Suppl 2):21–7.
Moldovan CP, Weldon AJ, Daher NS, et al. Effects of a meal replacement system alone or in combination with phentermine on weight loss and food cravings. Obesity (Silver Spring). 2016;24(11):2344–50.
Christensen P, Henriksen M, Bartels EM, et al. Long-term weight-loss maintenance in obese patients with knee osteoarthritis: a randomized trial. Am J Clin Nutr. 2017;106(3):755–63.
Leslie WS, Taylor R, Harris L, Lean ME. Weight losses with low-energy formula diets in obese patients with and without type 2 diabetes: systematic review and meta-analysis. Int J Obes (Lond). 2017;41(1):96–101.
Kempf K, Rohling M, Niedermeier K, Gartner B, Martin S. Individualized meal replacement therapy improves clinically relevant long-term glycemic control in poorly controlled type 2 diabetes patients. Nutrients. 2018;10(8):1022.
Shirai K, Saiki A, Oikawa S, et al. The effects of partial use of formula diet on weight reduction and metabolic variables in obese type 2 diabetic patients–multicenter trial. Obes Res Clin Pract. 2013;7(1):e43–54.
List JF, Woo V, Morales E, Tang W, Fiedorek FT. Sodium-glucose cotransport inhibition with dapagliflozin in type 2 diabetes. Diabetes Care. 2009;32(4):650–7.
Obata A, Kubota N, Kubota T, et al. Tofogliflozin improves insulin resistance in skeletal muscle and accelerates lipolysis in adipose tissue in male mice. Endocrinology. 2016;157(3):1029–42.
Bolinder J, Ljunggren O, Kullberg J, et al. Effects of dapagliflozin on body weight, total fat mass, and regional adipose tissue distribution in patients with type 2 diabetes mellitus with inadequate glycemic control on metformin. J Clin Endocrinol Metab. 2012;97(3):1020–31.
Bolinder J, Ljunggren O, Johansson L, et al. Dapagliflozin maintains glycaemic control while reducing weight and body fat mass over 2 years in patients with type 2 diabetes mellitus inadequately controlled on metformin. Diabetes Obes Metab. 2014;16(2):159–69.
Merovci A, Solis-Herrera C, Daniele G, et al. Dapagliflozin improves muscle insulin sensitivity but enhances endogenous glucose production. J Clin Invest. 2014;124(2):509–14.
Ferrannini E, Muscelli E, Frascerra S, et al. Metabolic response to sodium-glucose cotransporter 2 inhibition in type 2 diabetic patients. J Clin Invest. 2014;124(2):499–508.
Westman EC, Feinman RD, Mavropoulos JC, et al. Low-carbohydrate nutrition and metabolism. Am J Clin Nutr. 2007;86(2):276–84.
Shirai K, Utino J, Otsuka K, Takata M. A novel blood pressure-independent arterial wall stiffness parameter; cardio-ankle vascular index (CAVI). J Atheroscler Thromb. 2006;13(2):101–7.
Matsui Y, Kario K, Ishikawa J, Eguchi K, Hoshide S, Shimada K. Reproducibility of arterial stiffness indices (pulse wave velocity and augmentation index) simultaneously assessed by automated pulse wave analysis and their associated risk factors in essential hypertensive patients. Hypertens Res. 2004;27(11):851–7.
Yambe T, Yoshizawa M, Saijo Y, et al. Brachio-ankle pulse wave velocity and cardio-ankle vascular index (CAVI). Biomed Pharmacother. 2004;58(Suppl 1):S95–8.
Gomez-Sanchez L, Garcia-Ortiz L, Patino-Alonso MC, et al. The association between the cardio-ankle vascular index and other parameters of vascular structure and function in Caucasian adults: MARK study. J Atheroscler Thromb. 2015;22(9):901–11.
Kubozono T, Miyata M, Ueyama K, et al. Clinical significance and reproducibility of new arterial distensibility index. Circ J. 2007;71(1):89–94.
Nakamura K, Tomaru T, Yamamura S, Miyashita Y, Shirai K, Noike H. Cardio-ankle vascular index is a candidate predictor of coronary atherosclerosis. Circ J. 2008;72(4):598–604.
Noike H, Nakamura K, Sugiyama Y, et al. Changes in cardio-ankle vascular index in smoking cessation. J Atheroscler Thromb. 2010;17(5):517–25.
Suzuki J, Kurosu T, Kon T, Tomaru T. Impact of cardiovascular risk factors on progression of arteriosclerosis in younger patients: evaluation by carotid duplex ultrasonography and cardio-ankle vascular index(CAVI). J Atheroscler Thromb. 2014;21(6):554–62.
Dobsak P, Soska V, Sochor O, et al. Increased cardio-ankle vascular index in hyperlipidemic patients without diabetes or hypertension. J Atheroscler Thromb. 2015;22(3):272–83.
Satoh N, Shimatsu A, Kato Y, et al. Evaluation of the cardio-ankle vascular index, a new indicator of arterial stiffness independent of blood pressure, in obesity and metabolic syndrome. Hypertens Res. 2008;31(10):1921–30.
Malbrain ML, Huygh J, Dabrowski W, De Waele JJ, Staelens A, Wauters J. The use of bio-electrical impedance analysis (BIA) to guide fluid management, resuscitation and deresuscitation in critically ill patients: a bench-to-bedside review. Anaesthesiol Intensive Ther. 2014;46(5):381–91.
Acknowledgements
We would like to thank all the staff members in our departments and the participating institutions who contributed to this study.
Funding
This study was carried out under contract with the specified nonprofit corporation Hokkaido Institute of Health Sciences, based on a grant from AstraZeneca Co., Ltd. and Ono Pharmaceutical Co., Ltd. for investigator-initiated clinical trial. AstraZeneca Co., Ltd. and Ono Pharmaceutical Co., Ltd., which are manufacturers and distributors of the drug used in this research, are not involved in the planning, data management, analysis, and publication of results of this research and do not fund the journal’s article processing charges. The formula diet was purchased from Sunny Health Co., Ltd. using research funds, and there is no provision from Sunny Health Co., Ltd. including materials and labor for this research. The authors funded the journals article processing charges. All authors had full access to all of the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analysis.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Ichiro Tatsuno received lecture fees from Takeda Pharmaceutical Co., Ltd., and received research grants from Takeda Pharmaceutical Co., Ltd. and Mochida Pharmaceutical Pharma Co., Ltd. Yasuhiro Watanabe, Nobuichi Kuribayash, Daigaku Uchida, Daisuke Suzuki, Mitsutoshi Kato, Daiji Nagayama, Hiroshi Ohashi, Masahiro Ohira and Atsuhito Saiki have nothing to disclose.
Compliance with Ethics Guidelines
The protocol was approved by the institutional review board of each participating institution. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study. Patients and the public are not involved in the present study.
Data Availability
The analyzed data sets are available from the corresponding author on reasonable request.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced Digital Features
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.7447970.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Watanabe, Y., Kuribayashi, N., Uchida, D. et al. Study Protocol for the Effects of Formula Diet with Dapagliflozin on Metabolic Improvement and Body Composition in Type 2 Diabetes Mellitus. Diabetes Ther 10, 311–321 (2019). https://doi.org/10.1007/s13300-018-0555-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-018-0555-5