Abstract
Introduction
This study aimed to assess treatment satisfaction and self-reported health status in insulin-naïve patients with type 2 diabetes mellitus (T2DM) who started insulin glargine basal-supported oral therapy (BOT) with glycated hemoglobin (HbA1c) value of ≥6.5%, using data from Add-on Lantus® to Oral Hypoglycemic Agents 2 (ALOHA2) study, a 24-week single-arm, observational study of Japanese patients with T2DM, conducted as drug use surveillance in Japan.
Methods
Treatment satisfaction was measured using the Diabetes Treatment Satisfaction Questionnaire status version (DTSQs) and change version (DTSQc) and self-reported health status using EuroQol 5 Dimension (EQ-5D). The results were compared between the groups stratified by HbA1c level at the final evaluation point: target-achieved (<7.0%) and target-not-achieved groups (≥7.0%).
Results
In 1251 patients (336 in the target-achieved group), scores of DTSQs, DTSQc, and EQ-5D indicated significant improvement from baseline to the final evaluation point (both P < 0.01). The mean change in DTSQs scale score, DTSQs item score, and EQ-5D index score, and mean DTSQc scale score were significantly improved in the target-achieved group compared with the target-not-achieved group (P < 0.05 for all). DTSQs scale score and HbA1c level showed the same pattern of chronological change. Data analysis in patients stratified by DTSQs score showed better glycemic control in the high satisfaction group.
Conclusion
Following insulin glargine BOT introduction, treatment satisfaction and health status were improved from patients’ perspectives despite the need for daily injections. Based on the possible association between HbA1c 7.0% level achievement, treatment satisfaction, and health status, better glycemic control may be a key to successful treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A goal of diabetes treatment is to prevent diabetes complications and maintain as good quality of life (QOL) as those without diabetes, beginning from the fundamental step to achieve and maintain good glycemic control [1]. Although diligent life-long self-management is required due to the progressive nature of diabetes [2, 3], better glycemic control is associated with treatment satisfaction [4] and with better physical and psychological health [5]. Therefore, assessing treatment satisfaction and one’s perception, i.e., health status and QOL, using patient-reported outcome (PRO) measures as important outcomes and also as factors influencing disease and treatment outcomes is an important part of diabetes management [6].
Basal-supported oral therapy (BOT) in which long-acting insulin injection is added to ongoing treatment with oral antidiabetic drugs (OADs) has been widely adopted for patients with type 2 diabetes mellitus (T2DM) whose blood glucose control using OADs is insufficient [7]. The simple and less frequent administration is expected to lower a barrier to initiation derived from anticipated or actual physical and psychological burden of insulin treatment, and make the management easier, which can consequently encourage healthcare providers to initiate insulin treatment at early treatment stage. Insulin glargine, one of the long-acting insulin analogs most commonly used in BOT, can supplement endogenous basal insulin effectively to reduce glycemic levels for approximately 24 h by once-daily injection with smaller risk of hypoglycemia [8–11].
In Japan, Add-on Lantus® to Oral Hypoglycemic Agents 2 (ALOHA2) study, a 24-week, prospective, open-label multicenter, single-arm, observational study showed that insulin glargine BOT significantly improved blood glucose level in patients with T2DM, suggesting physiological efficacy and safety [12]. Although explored in other countries [13, 14], glargine BOT’s influence on treatment satisfaction and health status lacks data in Japanese patients, warranting the investigation specifically in a Japanese population. Anxiety and fear of insulin are known to hinder the introduction of insulin therapy [15]. Investigating the influence of glargine BOT on treatment satisfaction and health status may give patients and their medical practitioners an incentive to introduce insulin without undue delay. In the present analysis, using a subset of data from the ALOHA2, we explored treatment satisfaction and self-reported health status in patients starting insulin glargine BOT.
Methods
Study Design and Patients
The ALOHA2 study, a sequel of the ALOHA study [16–19], was conducted between 2012 and 2013 in 619 hospitals and clinics across Japan [12]. Participating patients were observed in a clinical setting. Patients with T2DM were included if they: were aged 20 or older, were being treated with OAD therapy, had glycated hemoglobin (HbA1c) ≥6.5% during 4 weeks prior to the study, and were to start BOT with insulin glargine. For data analysis, in the case of HbA1c levels in Japan Diabetes Society and the International Federation of Clinical Chemistry values, they were converted into the National Glycohemoglobin Standardization Program values [20].
Summary Results of the ALOHA2 Study
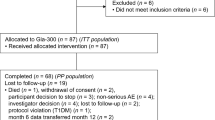
Of the 2630 patients enrolled, 2602 and 1629 patients comprised the safety and efficacy analysis set, respectively (Fig. 1). Of patients included in the safety analysis set, 140 patients (5.38%) reported hypoglycemic events, including 11 patients (0.42%) with severe hypoglycemic events (0.019 event/patient-year). As to efficacy, HbA1c, FPG, and 2 h PPG levels significantly improved from baseline to the final evaluation point (9.6% to 7.9%; 203.0 to 148.6 mg/dL; and 267.0 to 192.5 mg/dL, respectively).
Patient flow. CRF case report form, HbA1c glycated hemoglobin, OAD orally administered antidiabetic agent, PRO patient-reported outcome. a patients who had ever been administered insulin glargine. b patients who had not been treated with insulin previously and started insulin glargine basal-supported oral therapy during the observational period. c patients whose PRO instrument data were evaluable
PRO Instruments
Patients’ satisfaction and self-reported health status were measured using validated Japanese versions of three questionnaires: Diabetes Treatment Satisfaction Questionnaire status version (DTSQs) and change version (DTSQc) [21] and EuroQol 5 Dimension (EQ-5D) in the original 3-level format [22]. DTSQs and EQ-5D were administered at baseline, week 10 and week 24 or the last visit (final evaluation point) and DTSQc at the final evaluation point.
DTSQ simply and comprehensively assesses satisfaction specifically with diabetes treatment [23]. DTSQs captures the current status and DTSQc the change in treatment satisfaction [23, 24]. The instruments contain 8 questions: (1) satisfaction with current treatment, (2) perceived frequency of hyperglycemia, (3) perceived frequency of hypoglycemia, (4) convenience of the treatment, (5) flexibility of the treatment, (6) understanding of diabetes mellitus, (7) willingness to recommend the treatment to others, and (8) satisfaction to continue the treatment. Each item scores from 0 to 6 and −3 to 3 in the DTSQs and DTSQc, respectively. Treatment satisfaction was evaluated based on the combined score of 6 treatment satisfaction items: item 1, and 4–8. Scale scores range from 0 to 36 and −18 to 18 in DTSQs and DTSQc, respectively. A higher score indicates greater satisfaction or greater improvement in satisfaction. Perceived frequency of hyperglycemia and hypoglycemia (item 2 and 3, respectively) were assessed independently; a lower score indicates fewer perceived episodes of hyperglycemia, hypoglycemia, or a reduction in the number of such episodes.
EQ-5D is a universally used tool to describe respondent’s perceived health status [25]. The instrument includes the descriptive system and the visual analogue scale (EQ-VAS). The descriptive system consists of 5 dimensions: mobility, self-care, pain/discomfort, usual activities, and anxiety/depression, with three response levels: no problem, some problems, and extreme problems. The index score derived from the conversion of the total responses ranges from −0.11 to 1.00 in the Japanese population with the score of 1 denoting “full health” and 0 “death” [22]. EQ-VAS records respondent’s general health ranging from 0 (worst imaginable health state) to 100 (best possible health state).
Statistical Analysis
Of the efficacy analysis set insulin-naïve patients (n = 1629), patients with data on PRO instruments and HbA1c level at the final evaluation point available were analyzed. The patients were stratified according to the HbA1c level at the final evaluation point: <7.0% as target-achieved group, recommended level of glycemic control [1, 2, 26]; ≥7.0% as target-not-achieved group. Missing data were substituted by the data of the final evaluation point, using the last observation carried forward method. Data were compared between groups. Demographic and clinical characteristics were summarized descriptively and compared using Wilcoxon’s rank-sum test for continuous variables and Fisher’s exact test for nominal variables. The PRO score at baseline and the final evaluation point was compared using Wilcoxon signed-rank test (change in the DTSQc score was calculated based on the assumed baseline score of zero, indicating no change). The scores and their changes from baseline of each PRO instrument at the final evaluation point were compared using the Wilcoxon rank-sum test.
To explore possible factors that may influence treatment satisfaction, patients were stratified by tertiles of DTSQs satisfaction score change from baseline to the final evaluation point: high, middle, and low satisfaction groups. Factors were compared between the three groups using the Fisher’s exact test for nominal and Kruskal–Wallis test for continuous variables.
All statistical tests were conducted at a two-tailed significance level of 0.05 using SAS System software (version 9.2 or higher, SAS Institute, Cary, NC, 2006).
Compliance with Ethics Guidelines
This study was conducted as a special drug use surveillance in compliance with the pharmaceutical affairs law and the ministerial ordinance of “Good Post-Marketing Study Practice” in Japan, and conducted after a contract with each medical institution participating in the survey. Informed consent was obtained from all patients included in the study. All treatment decisions were made by each attending physician. Physicians and healthcare medical staff were blinded to the patients’ response to questionnaires.
Results
Patient Characteristics
Of the 1251 patients included in this analysis (Fig. 1), 336 patients (26.9%) achieved the target HbA1c level of <7.0%. Their baseline characteristics are summarized by target-achieved and target-not-achieved groups in Table 1. The disease seemed to have progressed less in the target-achieved than in the target-not-achieved group prior to baseline (i.e., a shorter duration of diabetes, fewer concomitant OAD, and lower percentage of patients with diabetic nephropathy (P < 0.05 for all).
Mean HbA1c level significantly decreased in both groups at the final evaluation point from baseline (paired t test, P < 0.0001) with significantly greater reduction in the target-achieved group (P < 0.0001) (Fig. 2). From baseline, both groups illustrated a similar trend of reduction (more than 1%) to week 12 and slight reduction (about 0.5%) in the target-achieved group and sideway shift with slight increase (less than 0.1%) in the target-not-achieved group onwards to the final evaluation point.
HbA1c level from baseline to the final evaluation point by the target-achieved and target-not-achieved group. ***P < 0.0001 (mean change target-achieved group vs target-not-achieved), Wilcoxon rank-sum test. HbA1c glycated hemoglobin. a Patients whose data both at baseline and the final evaluation point available were included in the inter-group comparison. Change from baseline to the final evaluation point (target-achieved vs target-not-achieved group, mean ± standard deviation): −2.98 ± 2.21 vs −1.15 ± 1.60%. b Final evaluation point: week 24 or the final visit in case of discontinuation
Although data from patients who answered the questionnaire were analyzed, data from those who did not answer did not show significantly poorer glycemic control or higher incidence of treatment-related adverse events in this particular group of patients (P > 0.05) (data not shown).
DTSQ
The mean DTSQs treatment satisfaction scale score significantly improved from baseline to the final evaluation point in overall patients (baseline vs final evaluation point: 21.8 vs 25.6, P < 0.0001) and also in the target-achieved and target-not-achieved group (P < 0.0001 for both) (Fig. 3a). The mean change from baseline to the final evaluation point was significantly greater in the target-achieved group (mean ± standard deviation: 5.3 ± 8.0 and 3.2 ± 7.6, P = 0.001). Over the study period, the treatment satisfaction scale score increased in both groups from baseline to week 10, and continued to increase slightly thereafter in the target-achieved group and almost leveled off in the target-not-achieved group, similar to the change in HbA1c level (Fig. 3a). Mean score of each item significantly improved from baseline to the final evaluation point (P < 0.0001 for all) with significantly greater improvement in the target-achieved group (P < 0.05 for all) (Fig. 3b).
DTSQ treatment satisfaction score by the target-achieved and target-not-achieved groups. a–c DTSQs treatment satisfaction score by the target-achieved and target-not-achieved groups. d–f DTSQc treatment satisfaction score at the final evaluation point by the target-achieved and target-not-achieved groups. DTSQ Diabetes Treatment Satisfaction Questionnaire, DTSQs Diabetes Treatment Satisfaction Questionnaire status version, DTSQc Diabetes Treatment Satisfaction Questionnaire change version. *<0.05, **<0.01, ***<0.001, ns not significant, (mean change target-achieved vs target-not-achieved group), Wilcoxon rank-sum test. a Patients whose data both at baseline and the final evaluation point available were included in the inter-group comparison. Change from baseline to the final evaluation point [target-achieved vs target-not-achieved group, mean ± standard deviation (SD)]: 5.3 ± 8.0 vs 3.2 ± 7.6 (total satisfaction scale score), mean ± SD vs mean ± SD (item score). b Final evaluation point: week 24 or the final visit in case of discontinuation
The mean DTSQs score of perceived frequency of hyperglycemia significantly improved from baseline to the final evaluation point in both groups (P < 0.0001 for both) (Fig. 3c) with significantly greater improvement in the target-achieved group (P = 0.0014). Mean score shift over time followed the same pattern as the treatment satisfaction scale score and the HbA1c level. Mean hypoglycemia scores increased in both groups from baseline to the final evaluation point with small changes in actual values (1.2 to 1.4 and 1.0 to 1.4) without significant inter-group difference in the change (P = 0.6706) (Fig. 3c).
The mean DTSQc treatment satisfaction scale score at the final evaluation point was 9.4 in overall patients. The score in the target-achieved and target-not-achieved group was 10.9 and 8.8, respectively, indicating significant improvement from baseline (P < 0.0001). The scale and each of the item scores were significantly greater in the target-achieved group indicating a greater improvement in satisfaction with the change in treatment (scale: P < 0.0001; item scores: P < 0.001 for all) (Fig. 3d, e). Mean hyperglycemia and hypoglycemia scores at the final evaluation point were significantly lower in the target-achieved than target-not-achieved group indicating a greater reduction in the perceived frequency of hyperglycemia and hypoglycemia in the target-achieved group (hyperglycemia: −0.9 and 0.0, respectively, P < 0.0001; hypoglycemia: −0.7 and −0.4, respectively, P = 0.0041) (Fig. 3f).
Of the data at baseline and final evaluation point analyzed to explore possible factors associated with treatment satisfaction by high, middle, and low satisfaction groups, the proportion of the patients with diabetic nephropathy and those with renal dysfunction were significantly smaller in the high satisfaction and larger in low satisfaction group (P < 0.05 for all) (Table 2). HbA1c and FPG levels were not significantly different at baseline between groups, although they were at the final evaluation point (highest in the low and lowest in the high satisfaction group, P < 0.05 for all). More patients in the low satisfaction group (8.6%) than the others (middle and high satisfaction groups: 5.3 and 4.7%, respectively) reported hypoglycemic events as treatment-related adverse events, but without significant inter-group difference (P = 0.1613).
EQ-5D
Overall patients reported relatively good health status (i.e., 75.9–94.8% of patients responded “No problem” in each item). The mean index score significantly increased from 0.893 at baseline to 0.911 at the final evaluation point (P = 0.0011) in the whole sample and also increased in both target-achieved and target-not-achieved groups (from 0.872 to 0.917 and 0.891 to 0.908, P = 0.0012 and 0.0185, respectively). Mean change of EQ-5D index score from baseline to the final evaluation point was significantly greater in the target-achieved than in the target-not-achieved group (0.037 and 0.011, respectively, P = 0.0185) (Fig. 4a). In all dimensions in both groups, except self-care in the target archived group, the proportion of patients who answered that they had no problem increased from baseline to the final evaluation point (Table 3). Greatest mean change, about 10%, was observed in the anxiety/depression dimension in the target-achieved group among all the dimensions in the groups. At the final evaluation point, no patient in either the target-achieved or the target-not-achieved group answered that they had “extreme problems” in the anxiety/depression dimension.
EQ-5D score from baseline to the final evaluation point by the target-achieved and target-not-achieved group. EQ-5D EuroQol 5 dimension, VAS visual analogue scale *<0.05, **<0.01, ***<0.001, ns not significant, (mean change target-achieved vs target-not-achieved group), Wilcoxon rank-sum test. a Final evaluation point: week 24 or the final visit in case of discontinuation. b Patients whose data both at baseline and the final evaluation point available were included in the inter-group comparison. Change from baseline to the final evaluation point (target-achieved vs target-not-achieved group, mean ± standard deviation): 0.037 ± 0.153 vs 0.011 ± 0.142 (index score), 13.69 ± 20.31 vs 5.71 ± 20.53 (VAS score )
The mean EQ-VAS score significantly increased from baseline to the final evaluation point (61.19–69.46, P < 0.0001) across all samples and also increased in both groups (from 58.65 to 73.51 and from 62.10 to 68.01 in the target-achieved and target-not-achieved group, respectively, P < 0.0001 for both). Mean change in score was significantly greater in the target-achieved group (P < 0.0001), starting from the lower score at baseline (Fig. 4b).
Discussion
In this sub-analysis using data from the ALOHA2 study, we explored treatment satisfaction and self-reported health status in patients with T2DM in whom the oral treatment failed and glargine BOT started. Improvement in treatment satisfaction was reflected in both DTSQs and DTSQc. Further significant improvement in EQ-5D index score (range −0.11 to 1.0) from a mean baseline score of more than 0.8, representing good health status, in both groups suggests that health further improved after starting glargine BOT even in the patients originally regarding themselves in a good health state. The results showed that treatment satisfaction and self-reported health status were not compromised but rather all improved following introduction of glargine BOT, representing the effectiveness of the treatment from patients’ perspectives.
A possible reason for the improvement in treatment satisfaction and self-reported health status despite insulin introduction may be attributed to perceived low frequency of hypoglycemia in contrast to the often held negative impression of insulin [27, 28]. DTSQs hypoglycemia item score slightly deteriorated or did not change, although DTSQc equivalent did improve. This contradiction may be due in part to the floor effect with the DTSQs whereby many patients scored zero at baseline for perceived frequency of hypoglycemia and could not show an improvement, only a worsening. The DTSQc overcame this floor effect. A greater decrease in hypoglycemia frequency shown in DTSQc item 3 scores in the target-achieved group despite a similar proportion of patients who actually experienced one or more hypoglycemic events in the target-achieved and target-not-achieved groups (7.1% and 5.6%, respectively, P = 0.3465) (data not shown) may imply that better glycemic control achieved may have given the retrospective impression that the hypoglycemia frequency had decreased and so imply importance of achieving glycemic control. DTSQc’s higher responsiveness to change [24, 29] may support this inference. In addition to the improvement in HbA1c level, patients’ perceived low frequency of hypoglycemia may have defied the anxiety toward insulin therapy, perhaps leading to improved treatment satisfaction and perceived health status. Our current findings along with previous consistent study results [13, 14, 30] may underscore the effectiveness and safety of insulin glargine added to OADs from both clinical and patient perspectives.
The current analysis suggests associations of HbA1c with treatment satisfaction and health status as reported in previous studies [31–34]. Treatment satisfaction and health status were more likely to improve in the target-achieved than in the target-not-achieved group based on the greater improvement in PRO scores in the target-achieved group; the similar improving trend over time traced by changes in HbA1c level and DTSQs except hypoglycemia frequency; and significant difference in the HbA1c and FPG level at the final evaluation point despite the non-significant difference at baseline in the DTSQs tertile group analysis. Improvement in the DTSQ treatment satisfaction scale and item scores encompassing various impressions, e.g., convenience of the treatment, in the target-achieved group may allow an interpretation that better glycemic control may have further lightened various burdens as well as hypoglycemia. The findings suggest better glycemic state may enhance treatment satisfaction and health status, or vice versa. Moreover, considering these links suggested in combination with better glycemic control achieved by earlier introduction of additional insulin on OAD treatment reported in several studies [35, 36] including ALOHA sub-analysis [19] may provide another perspective. Earlier insulin initiation may help achieve better glycemic status further leading to better treatment satisfaction and health status. The present findings may add to the collective evidence for recommending early insulin initiation. In addition, the associations between complications and reduced treatment satisfaction and impaired glycemic control are indicated by the higher proportion of patients with diabetic nephropathy and renal dysfunction at baseline in the lower satisfaction groups, and also a significantly higher proportion of patients with complications at baseline in the target-not-achieved group. Having existing complications which are difficult to relieve may have prevented patients from feeling more satisfied with treatment.
The EQ-5D result suggests that anxiety and depression coexist in a certain proportion of patients with T2DM. Depression in patients with diabetes is twice as prevalent as in the counterparts without [37], although the association does not link to diabetes itself, but to complications [38–40]. Comorbidity of diabetes and depression may be associated with poor self-caring attitudes, treatment adherence, glycemic control, and eventually to onset or progression of vascular complications [41–45]. Greater improvement in the anxiety/depression dimension in those with better glycemic control may reinforce the relationships. Given a path to the goal of diabetes treatment intersected with various factors, e.g., glycemic control, complications, treatment satisfaction, and health status, comprehensive assessment encompassing subjective and objective parameters is important for successful diabetes management.
Some aspects may limit the interpretation of this sub-analysis. First, the design is single-arm observational and the aim itself does not lay in confirmation of superiority of insulin glargine BOT. Since the ALOHA2 study was conducted as post-marketing surveillance in a routine clinical setting after the drug was marketed, hypoglycemia was not strictly defined and counted unlike clinical trials. Therefore, hypoglycemia frequencies can be underestimated. Secondly, our analysis cannot fully explain associations found, since our results cannot suggest causality in the associations and our study may not have encompassed all the factors that may influence the relationships. Increased treatment satisfaction may also result in improved HbA1c leading to reduced anxiety. Consequently, treatment satisfaction or perceived health status could improve. Thirdly, findings associated with glargine BOT may not be generalizable to different insulin treatment modalities or analogs. Fourthly, although statistically significant, the change in the EQ-5D could not reach the minimal important difference in diabetes patients in the United Kingdom [46]. However, the originally perceived good health status may not have left sufficient room for further improvement. Finally, patients who participated in this study may be more proactive and the results may not generalize well.
Conclusion
In the patients with T2DM whose OAD treatment failed to achieve adequate glycemic control, introduction of insulin glargine BOT does not detract from treatment satisfaction or health status but rather benefits patients from their own perspectives with a minimal risk for hypoglycemia despite the negative impressions often associated with insulin treatment. Improvement in both treatment satisfaction and health status and glycemic control were associated. HbA1c achievement may relieve various burdens. Based on the possible association, a key to successful treatment may be found in achievement of target glycemic level and early initiation of insulin glargine BOT.
References
Japan Diabetes Society. Chapter 3A: treatment objectives and control indicators. In: Japan Diabetes Society, editor. Treatment Guide for Diabetes 2014–2015. Tokyo: Bunkodo Co., Ltd.; 2014. p. 24–6 (in Japanese).
Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in Type 2 diabetes, 2015: a patient-centered approach: update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2015;38:140–9.
Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care. 2002;25:1159–71.
Cappelleri JC, Cefalu WT, Rosenstock J, Kourides IA, Gerber RA. Treatment satisfaction in type 2 diabetes: a comparison between an inhaled insulin regimen and a subcutaneous insulin regimen. Clin Ther. 2002;24:552–64.
Colman SS, Brod M, Potter LP, Buesching DP, Rowland CR. Cross-sectional 7-year follow-up of anxiety in primary care patients. Depress Anxiety. 2004;19:105–11.
Fisher EB, Thorpe CT, Devellis BM, Devellis RF. Healthy coping, negative emotions, and diabetes management: a systematic review and appraisal. Diabetes Educ 2007;33:1080–103 (discussion 1104–6).
Riddle MC, Rosenstock J, Gerich J, and on behalf of the Insulin Glargine 4002 Study Investigators. The treat-to-target trial: randomized addition of glargine or human NPH insulin to oral therapy of type 2 diabetic patients. Diabetes Care 2003;26:3080–6.
Fritsche A, Schweitzer MA, Häring HU. 4001 Study Group. Glimepiride combined with morning insulin glargine, bedtime neutral protamine hagedorn insulin, or bedtime insulin glargine in patients with type 2 diabetes. A randomized, controlled trial. Ann Intern Med. 2003;138:952–9.
Rosenstock J, Schwartz SL, Clark CM Jr, Park GD, Donley DW, Edwards MB. Basal insulin therapy in type 2 diabetes: 28-week comparison of insulin glargine (HOE901) and NPH insulin. Diabetes Care. 2001;24:631–6.
Dunn CJ, Plosker GL, Keating GM, McKeage K, Scott LJ. Insulin glargine: an updated review of its use in the management of diabetes mellitus. Drugs. 2003;63:1743–78.
Yki-Järvinen H, Dressler A, Ziemen M, HOE 901/300s Study Group. Less nocturnal hypoglycemia and better post-dinner glucose control with bedtime insulin glargine compared with bedtime NPH insulin during insulin combination therapy in type 2 diabetes. HOE 901/3002 Study Group. Diabetes Care. 2000;23:1130–6.
Kobayashi M, Tsukube S, Ikeda Y, Shuto Y. Safety and efficacy of combination therapy with insulin glargine and oral hypoglycaemic agents including DPP-4 inhibitors in Japanese T2DM patients: ALOHA 2 study, a post-marketing surveillance for Lantus. J Diabetes Mellit. 2014;4:273–89.
Secnik Boye K, Matza LS, et al. Patient-reported outcomes in a trial of exenatide and insulin glargine for the treatment of type 2 diabetes. Health Qual Life Outcomes 2006;4:80.
Vinik AI, Zhang Q. Adding insulin glargine versus rosiglitazone: health-related quality-of-life impact in type 2 diabetes. Diabetes Care. 2007;30:795–800.
Bradley-Gibride J, Bradley C. Partially randomized preference trial design. In: Salkind Neil J, editor. Encyclopedia of research design. Vol. 2. Thousand Oaks: Sage Publications USA; 2010.
Kadowaki T, Ohtani T, Odawara M. Potential formula for the calculation of starting and incremental insulin glargine doses: ALOHA subanalysis. PLoS One. 2012;7:e41358.
Odawara M, Ohtani T, Kadowaki T. Dosing of insulin glargine to achieve the treatment target in Japanese type 2 diabetes on a basal supported oral therapy regimen in real life: ALOHA study subanalysis. Diabetes Technol Ther. 2012;14:635–43.
Odawara M, Kadowaki T, Naito Y. Incidence and predictors of hypoglycemia in Japanese patients with type 2 diabetes treated by insulin glargine and oral antidiabetic drugs in real-life: ALOHA post-marketing surveillance study sub-analysis. Diabetol Metab Syndr. 2014;15(6):20.
Kadowaki T, Ohtani T, Odawara M. Baseline predictive factors for glycemic control in Japanese type 2 diabetes patients treated with insulin glargine plus oral antidiabetic drugs: ALOHA study subanalysis. Diabetol Int. 2013;4:16–22.
Kashiwagi A, Kasuga M, Araki E, et al. Committee on the standardization of diabetes mellitus related laboratory testing of Japan Diabetes Society. International clinical harmonization of glycated hemoglobin in Japan: From Japan Diabetes Society to National Glycohemoglobin Standardization Program values. J Diabetes Investig. 2012;3:39–40.
Ishii H, Bradley C, Riazi A, Barendse S, Yamamoto T. The Japanese Version of the Diabetes Treatment Satisfaction Questionnaire (DTSQ): translation and clinical evaluation. J Clin Exp Med. 2000;192:809–14 (in Japanese).
Tsuchiya A, Ikeda S, Ikegami N, et al. Estimating an EQ-5D population value set: the case of Japan. Health Econ. 2002;11:341–53.
Bradley C, Lewis KS. Measures of psychological well-being and treatment satisfaction developed from the responses of people with tablet-treated diabetes. Diabet Med. 1990;7:445–51.
Bradley C, Plowright R, Stewart J, Valentine J, Witthaus E. The Diabetes Treatment Satisfaction Questionnaire change version (DTSQc) evaluated in insulin glargine trials shows greater responsiveness to improvements than the original DTSQ. Health Qual Life Outcomes. 2007;5:57.
EuroQol Group. EuroQol—a new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199–208.
Nathan DM, Buse JB, Davidson MB, et al. European Association for Study of Diabetes. Medical management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2009;32:193–203.
Polonsky WH, Fisher L, Guzman S, Villa-Caballero L, Edelman SV. Psychological insulin resistance in patients with type 2 diabetes: the scope of the problem. Diabetes Care. 2005;28:2543–5.
Meece J. Dispelling myths and removing barriers about insulin in type 2 diabetes. Diabetes Educ. 2006;32:9S–18S.
Bradley C. Diabetes treatment satisfaction questionnaire. Change version for use alongside status version provides appropriate solution where ceiling effects occur. Diabetes Care. 1999;22:530–2.
Garg SK, Admane K, Freemantle N, et al. Patient-led versus physician-led titration of insulin glargine in uncontrolled patients with type 2 diabetes: a randomized multinational-ATLAS Study. Endocr Pract. 2015;21:143–57.
Hajos TR, Pouwer F, de Grooth R, et al. The longitudinal association between glycaemic control and health-related quality of life following insulin therapy optimisation in type 2 diabetes patients. A prospective observational study in secondary care. Qual Life Res. 2012;21:1359–65.
Marra G, DIAB. & TE.S Project Study Group. The DIAB. & TE.S Project: how patients perceive diabetes and diabetes therapy. Acta Biomed 2004;75:164–70.
Kelley K, Dempsey C. An evaluation of an insulin transfer programme delivered in a group setting. J Clin Nurs. 2007;16:152–8.
Tahrani AA, Digwood S, Lee C, Moulilk P. Evaluation of glargine group-start sessions in patients with type 2 diabetes as a strategy to deliver the service. Int J Clin Pract. 2007;61:329–35.
UK Prospective Diabetes Study Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet 1998;352:837–53 (Erratum in: Lancet 1999;354:602).
Niswender K. Early and aggressive initiation of insulin therapy for type 2 diabetes: what is the evidence? Clin Diabetes. 2009;27:60–8.
Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care. 2001;24:1069–78.
UK Prospective Diabetes Study Group. Quality of life in type 2 diabetic patients is affected by complications but not by intensive policies to improve blood glucose or blood pressure control (UKPDS 37). UK Prospective Diabetes Study Group. Diabetes Care. 1999;22:1125–36.
Wexler DJ, Grant RW, Wittenberg E, et al. Correlates of health-related quality of life in type 2 diabetes. Diabetologia. 2006;49:489–97.
Wändell PE. Quality of life of patients with diabetes mellitus. An overview of research in primary health care in the Nordic countries. Scand J Prim Health Care. 2005;23:68–74.
Schram MT, Baan CA, Pouwer F. Depression and quality of life in patients with diabetes: a systematic review from the European depression in diabetes (EDID) research consortium. Curr Diabetes Rev. 2009;5:112–9.
Katon W, von Korff M, Ciechanowski P, et al. Behavioral and clinical factors associated with depression among individuals with diabetes. Diabetes Care. 2004;27:914–20.
Ciechanowski PS, Katon WJ, Russo JE. Depression and diabetes: impact of depressive symptoms on adherence, function, and costs. Arch Intern Med. 2000;160:3278–85.
Lin EH, Katon W, von Korff M, et al. Relationship of depression and diabetes self-care, medication adherence, and preventive care. Diabetes Care. 2004;27:2154–60.
Lin EH, Rutter CM, Katon W, et al. Depression and advanced complications of diabetes: a prospective cohort study. Diabetes Care. 2010;33:264–9.
Mulhern B, Meadows K. Investigating the minimally important difference of the Diabetes Health Profile (DHP-18) and the EQ-5D and SF-6D in a UK diabetes mellitus population. Health. 2013;5:1045–54.
Acknowledgments
The authors are grateful to all physicians at the hospitals and clinics attending in the ALOHA 2 Study. The authors are also grateful to the developer of the DTSQs and DTSQc, Professor Clare Bradley, and Health Psychology Research Ltd. (http://www.healthpsychologyresearch.com), for granting us permission to use the instrument in our study. Statistical analysis was performed by EPS Corp. and editorial assistance in the preparation of this manuscript was provided by Clinical Study Support, Inc., and support for their assistance was funded by and under the contracts with Sanofi K.K., Tokyo, Japan. This study was conducted and sponsored, the article processing charges included, by Sanofi K.K. Sanofi K.K. had responsibility for the design, the statistical analysis plan, the drafting and approval of the manuscript. Each author made contribution to the paper in the following categories: design, study conduct, data collection and data analysis by Shoko Tsukube and Yukio Ikeda, interpretation of data analysis and manuscript writing by Shoko Tsukube, Yukio Ikeda, Takashi Kadowaki, and Masato Odawara. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript; take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published.
Access to Questionnaires: DTSQs and DTSQc visit http://www.healthpsychologyresearch.com. EQ-5D visit http://www.euroqol.org/.
Conflict of interest
Shoko Tsukube is an employee of Sanofi K.K., Tokyo, Japan. Yukio Ikeda is also an employee of Sanofi K.K., Tokyo, Japan. Takashi Kadowaki has served on advisory panels for Boehringer Ingelheim, Daiichi-Sankyo, Novo Nordisk, Taisho, Takeda and Tanabe-Mitsubishi; has served as a consultant for Boehringer Ingelheim and MSD; has received research support from Astra Zeneca, Chugai, Daiichi-Sankyo, MSD, Ono, Sanofi, Takeda and Tanabe-Mitsubishi; and has served on speakers’ bureaus for Astellas, Astra Zeneca, Boehringer Ingelheim, Daiichi-Sankyo, Dainippon-Sumitomo, Eli Lilly, Kowa, Kyowahakko Kirin, MSD, Novartis, Ono, Sanofi, Sanwa, Taisho, Takeda and Tanabe-Mitsubishi. Masato Odawara has served advisory panels for Astra Zeneca, Boehringer Ingelheim, Novo Nordisk, Sanofi, and Taisho; has received research support from Astellas, Astra Zeneca, Boehringer Ingelheim, Daiichi-Sankyo, Dainippon-Sumitomo, Eli Lilly, Kowa, Kyowahakko Kirin, MSD, Novartis, Ono, Sanofi, Taisho, Takeda and Tanabe-Mitsubishi; and has served on speakers’ bureaus for Astellas, Astra Zeneca, Boehringer Ingelheim, Daiichi-Sankyo, Dainippon-Sumitomo, Eli Lilly, Kowa, Kyowahakko Kirin, MSD, Novartis, Ono, Sanofi, Taisho, Takeda and Tanabe-Mitsubishi.
Compliance with ethics guidelines
This study was conducted as a special drug use surveillance complied with the pharmaceutical affairs law and the ministerial ordinance of “Good Post-Marketing Study Practice” in Japan, and conducted after a contract was signed with each medical institution participating in the survey. Informed consent was obtained from all patients for being included in the study. Ethical consideration including confidentiality had been given in a course of the study implementation.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Tsukube, S., Ikeda, Y., Kadowaki, T. et al. Improved Treatment Satisfaction and Self-reported Health Status after Introduction of Basal-Supported Oral Therapy Using Insulin Glargine in Patients with Type 2 Diabetes: Sub-Analysis of ALOHA2 Study. Diabetes Ther 6, 153–171 (2015). https://doi.org/10.1007/s13300-015-0111-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-015-0111-5