Abstract
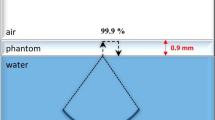
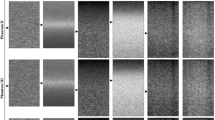
Diagnostic ultrasound (US) scanners are generally evaluated using proprietary quality assurance (QA) phantoms, but their prohibitively high cost may prevent organizations to perform the necessary tests. This study aimed to develop a low-cost gel wax phantom with targets to determine the lateral and axial resolution and diameter of a hyperechoic target in an US scanner. The acoustic property (AP) of gel wax, which includes the speed of sound (cus), acoustic impedance (Z), and attenuation coefficient (µ), were determined for multiple transducers operating at 2.25, 5, 10, 15, and 30 MHz. These results were compared to the AP of soft tissue. Two polytetrafluoroethylene (PTFE) rectangular frames with holes separated by 5, 10, and 20 mm were constructed. Nylon filaments and stainless-steel disc (SS disc) (diameter = 16.8 mm) were threaded through the frames and suitably placed in gel wax to obtain orthogonal targets in the phantom. The target dimensions obtained from computerized tomography (CT) and US images of the phantom were compared for phantom validation. The average cus=1431.4 m/s, mass density ρ = 0.87 g/cm3, Z = 1.24 MRayls, and µ ranged from 0.7 to 0.98 dB/cm/MHz for gel wax at 22 °C. The US image measurement exhibited a maximum error in determining the diameter of the SS disc, resulting in a value of 18 mm instead of its actual value of 16.8 mm. The phantom volume decreased by 1.8% in 62 weeks. The present phantom is affordable, stable, customizable, and can be used to evaluate diagnostic US scanners across multiple centers.






Similar content being viewed by others
References
Goodsitt MM, Carson PL, Witt S, Hykes DL, Kofler JM (1998) Real-time B-mode ultrasound quality control test procedures: report of AAPM ultrasound task group No. 1. Med Phys 25:1385–1406. https://doi.org/10.1118/1.598404
Kofler JM. Quality assurance of ultrasound imagers: procedures, expectations, and philosophies. AAPM 43rd Annu Meet Am. 2001:1–37.
Sipilä O, Mannila V, Vartiainen E (2011) Quality assurance in diagnostic ultrasound. Eur J Radiol 80:519–525. https://doi.org/10.1016/j.ejrad.2010.11.015
Weigang B, Moore GW, Gessert J, Phillips WH, Schafer M (2003) The methods and effects of transducer degradation on image quality and the clinical efficacy of diagnostic sonography. J Diagn Med Sonogr 19:3–13. https://doi.org/10.1177/8756479302239545
Earle M, Portu GD, Devos E (2016) Agar ultrasound phantoms for low-cost training without refrigeration. Afr J Emerg Med 6:18–23. https://doi.org/10.1016/j.afjem.2015.09.003
Kendall JL, Faragher JP (2007) Ultrasound-guided central venous access: a homemade phantom for simulation. Can J Emerg Med 9:371–373. https://doi.org/10.1017/S1481803500015335
Bude R 0, Adler RS (1995) An Easily Made, Low-Cost, Tissue-Like Ultrasound Phantom Material. vol. 23.
Madsen EL, Frank GR, Dong F (1998) Liquid or solid ultrasonically tissue-mimicking materials with very low scatter. Ultrasound Med Biol 24:535–542. https://doi.org/10.1016/S0301-5629(98)00013-1
Oudry J, Bastard C, Miette V, Willinger R, Sandrin L (2009) Copolymer-in-oil phantom materials for elastography. Ultrasound Med Biol 35:1185–1197. https://doi.org/10.1016/j.ultrasmedbio.2009.01.012
Jones CJM, Munro PRT (2018) Stability of gel wax based optical scattering phantoms. Biomed Opt Express 9:3495. https://doi.org/10.1364/boe.9.003495
Vieira SL, Pavan TZ, Junior JE, Carneiro AAO (2013) Paraffin-gel tissue-mimicking material for Ultrasound-guided needle biopsy Phantom. Ultrasound Med Biol 39:2477–2484. https://doi.org/10.1016/j.ultrasmedbio.2013.06.008
Maneas E, Xia W, Nikitichev DI, Daher B, Manimaran M, Wong RYJ et al (2018) Anatomically realistic ultrasound phantoms using gel wax with 3D printed moulds. Phys Med Biol. https://doi.org/10.1088/1361-6560/aa9e2c
Daly R, Planas JH, Ann M (2017) Adapting Gel Wax into an ultrasound-guided pericardiocentesis model at low cost. West J Emerg Med 114:114–116. https://doi.org/10.5811/westjem.2016.10.31506
Browne JE, Ramnarine KV, Watson AJ, Hoskins PR (2003) Mimicking Test Phantoms 29:1053–1060. https://doi.org/10.1016/S0301-5629(03)00053-X.
Mast TD (2000) Empirical relationships between acoustic parameters in human soft tissues. Acoust Res Lett Online 1:37–42. https://doi.org/10.1121/1.1336896
Phani D, Varadarajulu RK, Thomas A, Paramu R, Singh MS, Shaiju VS et al (2020) Acoustic and ultrasonographic characterization of polychloroprene, beeswax, and carbomer-gel to mimic soft-tissue for diagnostic ultrasound. Phys Eng Sci Med 43:1171–1181. https://doi.org/10.1007/s13246-020-00919-7
Bushberg JT, Boone JM (2011) The essential physics of medical imaging. Lippincott Williams and Wilkins, United States
Bigelow TA (2008) Ultrasound attenuation estimation using backscattered echoes from multiple sources. J Acoust Soc Am 124:1367–1373. https://doi.org/10.1121/1.2949519
Maruvada S, Shung KK, Wang S-H (2000) High-frequency backscatter and attenuation measurements of selected bovine tissues between 10 and 30 MHz. Ultrasound Med Biol 26:1043–1049. https://doi.org/10.1016/S0301-5629(00)00227-1
White R, Kopchok G, Zalewski M, Ayres B, Wilson E, De Virgilio C et al (1996) Comparison of the deployment and healing of thin-walled expanded PTFE stented grafts and covered stents. Ann Vasc Surg 10:336–346. https://doi.org/10.1007/BF02286777
Vatnitsky SM, International Atomic Energy Agency (2008) Commissioning of radiotherapy treatment planning systems: testing for typical external beam treatment techniques : report of the Coordinated Research Project on Development of Procedures for Quality Assurance of Dosimetry Calculations in Radiotherapy. International Atomic Energy Agency
Cabrelli LC, Pelissari PI, Deana AM, Carneiro AA, Pavan TZ (2016) Stable phantom materials for ultrasound and optical imaging. Phys Med Biol 62:432
Drever L, Hilts M (2007) Daily quality assurance phantom for ultrasound image guided radiation therapy. J Appl Clin Med Phys 8:126–136. https://doi.org/10.1120/jacmp.v8i3.2467
Najafi M, Afsham N, Abolmaesumi P, Rohling R (2014) A closed-form differential formulation for ultrasound spatial calibration: multi-wedge phantom. Ultrasound Med Biol 40:2231–2243. https://doi.org/10.1016/j.ultrasmedbio.2014.03.006
Dendy PP, Heaton B (2011) Physics for Diagnostic Radiology, 3rd edn. CRC Press
Wong EY, Thorne ML, Nikolov HN, Poepping TL, Holdsworth DW (2008) Doppler ultrasound compatible plastic material for use in rigid flow models. Ultrasound Med Biol 34:1846–1856. https://doi.org/10.1016/j.ultrasmedbio.2008.01.002
De Carvalho IM, Basto RLQ, Infantosi AFC, Von Krüger MA, Pereira WCA (2010) Breast ultrasound imaging phantom to mimic malign lesion characteristics. Phys Procedia 3:421–426. https://doi.org/10.1016/j.phpro.2010.01.055
Taylor Z, Jonveaux L, Caskey C (2017) Development of a Portable and Inexpensive Ultrasound Imaging Device for Use in the Developing World. URL Httpswww Semanticscholar OrgpaperDevelopment—Portable–Inexpensive-Imaging-Taylor-Jonveaux4a45c73373a1e1168f7a276d977d65cebc29e0eb
Khalitov RS, Gurbatov SN, Demin IY (2016) The use of the Verasonics ultrasound system to measure shear wave velocities in CIRS phantoms. Phys Wave Phenom 24:73–76. https://doi.org/10.3103/S1541308X16010143
Ali A, Logeswaran R (2007) A visual probe localization and calibration system for cost-effective computer-aided 3D ultrasound. Comput Biol Med 37:1141–1147. https://doi.org/10.1016/j.compbiomed.2006.10.003
Soehl M, Walsh R, Rankin A, Lasso A, Fichtinger G (2014) Tracked ultrasound calibration studies with a phantom made of LEGO bricks. Med. Imaging 2014 Image-Guid. Proced. Robot. Interv. Model., vol. 9036, SPIE; p. 90362R-90362R. https://doi.org/10.1117/12.2044121
Poon TC, Rohling RN (2005) Comparison of calibration methods for spatial tracking of a 3-D ultrasound probe. Ultrasound Med Biol 31:1095–1108. https://doi.org/10.1016/j.ultrasmedbio.2005.04.003
Luan H, Qi F, Xue Z, Chen L, Shen D (2008) Multimodality image registration by maximization of quantitative-qualitative measure of mutual information. Pattern Recognit 41:285–298. https://doi.org/10.1016/j.patcog.2007.04.002
Pagoulatos N, Haynor DR, Kim Y (2001) A fast calibration method for 3-D tracking of ultrasound images using a spatial localizer. Ultrasound Med Biol 27:1219–1229. https://doi.org/10.1016/S0301-5629(01)00431-8
Acknowledgements
The authors are grateful to Ramesh Babu V, Precision Fabrication Facility, Biomedical Technology Wing, Sree Chitra Tirunal Institute for Medical Sciences and Technology Trivandrum, Kerala, INDIA, for fabricating the polytetrafluoroethylene frames used in this study. We thank Jyoti R Seth, Advanced Rheology Facility, Indian Institute of Technology Bombay Powai, Mumbai, INDIA, for providing the information on polyethylene gels and gel waxes.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Phantom preparation and data collection were performed by DP, AP, SP, GZ, and SVS. Analysis was performed by VM, RKV, RP, MSS and RKN. The first draft of the manuscript was written by DP, and all authors commented on previous versions. The final manuscript was read and approved by all authors.
Corresponding author
Ethics declarations
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This article does not contain any studies performed on human participants or animals.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Phani, D., Varadarajulu, R.K., Paramanick, A. et al. Development and validation of a gel wax phantom to evaluate geometric accuracy and measurement of a hyperechoic target diameter in diagnostic ultrasound imaging. Phys Eng Sci Med 47, 261–272 (2024). https://doi.org/10.1007/s13246-023-01362-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13246-023-01362-0