Abstract
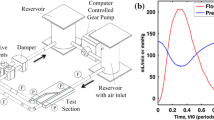
The coronary arterial tree experiences large displacements due to the contraction and expansion of the cardiac muscle and may influence coronary haemodynamics and stent placement. The accurate measurement of catheter trackability forces within physiological relevant test systems is required for optimum catheter design. The effects of cardiac motion on coronary flowrates, pressure drops, and stent delivery has not been previously experimentally assessed. A cardiac simulator was designed and manufactured which replicates physiological coronary flowrates and cardiac motion within a patient-specific geometry. A motorized delivery system delivered a commercially available coronary stent system and monitored the trackability forces along three phantom patient-specific thin walled compliant coronary vessels supported by a dynamic cardiac phantom model. Pressure drop variation is more sensitive to cardiac motion than outlet flowrates. Maximum pressure drops varied from 7 to 49 mmHg for a stenosis % area reduction of 56 to 90%. There was a strong positive linear correlation of cumulative trackability force with the cumulative curvature. The maximum trackability forces and curvature ranged from 0.24 to 0.87 N and 0.06 to 0.22 mm−1 respectively for all three vessels. There were maximum and average percentage differences in trackability forces of (23–49%) and (1.9–5.2%) respectively when comparing a static pressure case with the inclusion of pulsatile flow and cardiac motion. Cardiac motion with pulsatile flow significantly altered (p value <0.001) the trackability forces along the delivery pathways with high local percentage variations and pressure drop measurements.










Similar content being viewed by others
References
Alfonso, F., C. Macaya, J. Goicolea, R. Hernandez, J. Segovia, J. Zamorano, et al. Determinants of coronary compliance in patients with coronary artery disease: an intravascular ultrasound study. J. Am. Coll. Cardiol. 23(4):879–884, 1994.
Balcon, R. Recommendations on stent manufacture, implantation and utilisation. Eur. Heart J. 18(10):1536–1547, 1997.
Bogaert, J., and F. E. Rademakers. Regional nonuniformity of normal adult human left ventricle. Am. J. Physiol. Heart Circ. Physiol. 280:H610–H620, 2001.
Caldwell, R. A., J. E. Woodell, S. P. Ho, S. W. Shalaby, T. Boland, E. M. Langan, et al. In vitro evaluation of phosphonylated low-density polyethylene for vascular applications. J. Biomed. Mater. Res. 62(4):514–524, 2002.
Capron, L., and P. Bruneval. Influence of applied stress on mitotic response of arteries to injury with a balloon catheter: quantitative study in rat thoracic aorta. Cardiovasc. Res. 23(11):941–948, 1989.
Chen, S. Y., and J. D. Carroll. Kinematic and deformation analysis of 4-D coronary arterial trees reconstructed from cine angiograms. IEEE Trans. Med. Imaging 21(6):710–721, 2003.
Davies, J. E., Z. I. Whinnett, D. P. Francis, C. H. Manisty, J. Aguado-Sierra, et al. Evidence of a dominant backward-propagating “suction” wave responsible for diastolic coronary filling in humans attenuated in left ventricular hypertrophy. Circulation 113:1768–1778, 2006.
Dunn, A. C., and T. D. Zaveri. Macroscopic friction coefficient measurements on living endothelial cells. Tribol. Lett. 27(2):233–238, 2007.
Ene, F., P. Delassus, and L. Morris. The influence of computational assumptions on analysing abdominal aortic aneurysm haemodynamics. Proc. Inst. Mech. Eng. H 228(8):768–780, 2014.
Ethier, C. R., and A. C. Simmons. Introduction to Biomechanics. From Cells to Organisms. New York: Cambridge University Press, 2007.
Fedel, M., F. Tessarolo, P. Ferrari, C. Lösche, N. Ghassemieh, G. M. Guarrera, et al. Functional properties and performance of new and reprocessed coronary angioplasty balloon catheters. J. Biomed. Mater. Res. 78B(2):364–372, 2006.
Gielen, H., O. Daniels, and H. van Lier. Natural history of congenital pulmonary valvar stenosis: an echo and Doppler cardiographic study. Cardiol. Young 1999(9):129–135, 1999.
Johnston, K., P. Sharma, and J. Oshinski. Coronary artery flow measurement using navigator echo gated phase contrast magnetic resonance velocity mapping at 3.0T. J. Biomech. 41:508–602, 2008.
Kamangar, S., G. Kalimuthu, I. A. Badruddin, A. Badarudin, N. J. Ahmed, and T. M. Khan. Numerical investigation of the effects of stenosis geometry on the coronary diagnostic parameters. Sci. World J. 2014:354946, 2014.
Kinney, T. B., M. Fan, A. K. Chin, J. C. Finn, W. G. Hayden, and T. J. Fogarty. Shear force in angioplasty. Am. J. Roentgenol. 144(1):115–122, 1985.
Kolandavel, M. K., E. T. Fruend, S. Ringgaard, and P. G. Walker. The effects of time varying curvature on species transport in coronary arteries. Ann. Biomed. Eng. 34(12):1820–1832, 2006.
Kousera, C. A., S. Nijjer, R. Torii, R. Petraco, S. Sen, N. Foin, A. D. Hughes, D. P. P. Francis, X. J. Xu, and J. E. Davies. Patient-specific coronary stenoses can be modelled using a combination of OCT and flow velocities to accurately predict hyperemic pressure gradients. IEEE Trans. Biomed. Eng. 61:1902–1913, 2014.
Lee, R. T., A. J. Grodzinsky, E. H. Frank, R. D. Kamm, and F. J. Schoen. Structure-dependent dynamic mechanical behavior of fibrous caps from human atherosclerotic plaques. Circulation 83:1764–1770, 1991.
Leung, J. H., A. R. Wright, N. Cheshire, et al. Fluid structure interaction of patient specific abdominal aorta aneurysms: a comparison with solid stress models. BioMed. Eng. OnLine 5:33, 2006.
Malve, M., A. Garcia, J. Ohayon, and M. A. Martinez. Unsteady blood flow and mass transfer of a human left coronary artery bifurcation FSI vs CFD. Int. Commun. Heat Mass Transf. 39:745–751, 2012.
Mamada, K., H. Kosukegawa, V. Fridrici, P. Kapsa, and M. Ohta. Friction properties of PVA-H/steel ball contact under water lubrication conditions. Tribol. Int. 44(7):757–763, 2011.
McDaniel, M. C., E. M. Galbraith, A. M. Jeroudi, O. R. Kashlan, P. Eshtehardi, et al. Localization of culprit lesions in coronary arteries of patients with ST-segment elevation myocardial infarctions: relation to bifurcations and curvatures. Am. Heart J. 161:508–515, 2011.
Meng, S., H. Stefan, H. Geyer, F. da Luciano, M. P. Viana, and W. J. Weninger. Objective characterization of the course of the parasellar internal carotid artery using mathematical tools. Surg. Radiol. Anat. 30(6):519–526, 2008.
Morris, L., P. Delassus, A. Callanan, M. Walsh, F. Wallis, P. Grace, and T. McGloughlin. 3-D numerical simulation of blood flow through models of the human aorta. J. Biomech. Eng. 127(5):767–775, 2005.
Nichols, W. W., and M. F. Rourke. McDonald’s Blood Flow in Arteries (5th ed.). Boca Raton: Taylor & Francis, 2005.
O’Flynn, P., G. O’Sullivan, and A. Pandit. Methods for three-dimensional geometric characterization of the arterial vasculature. Ann. Biomed. Eng. 35(8):1368–1381, 2007.
O’Flynn, P., G. O’Sullivan, and A. Pandit. Geometric variability of the abdominal aorta and its major peripheral branches. Ann. Biomed. Eng. 38(3):824–840, 2010.
Pao, Y. C., J. T. Lu, and E. L. Ritman. Bending and twisting of an in vivo coronary artery at a bifurcation. J. Biomech. 25(3):287–295, 1992.
Papaharilaou, Y., J. A. Ekaterinaris, E. Manousaki, et al. A decoupled fluid structure approach for estimating wall stress in abdominal aortic aneurysms. J. Biomech. 40:367–377, 2007.
Perktold, K., and G. Rappitsch. Computer simulation of local blood flow and vessel mechanics in a compliant carotid artery bifurcation model. J. Biomech. 28:845–856, 1995.
Pivkin, I. V., P. D. Richardson, D. H. Laidlaw, and G. E. Karniadakis. Combined effects of pulsatile flow and dynamic curvature on wall shear stress in a coronary artery bifurcation model. J. Biomech. 38:1283–1290, 2005.
Prosi, E., K. Perktold, Z. Ding, and M. H. Friedman. Influence of curvature dynamics on pulsatile coronary artery flow in a realistic bifurcation model. J. Biomech. 37:1767–1775, 2004.
Rennie, A. C., P. L. Dickrell, and W. G. Sawyer. Friction coefficient of soft contact lenses: measurement and modelling. Tribol. Lett. 18(4):499–504, 2005.
Rieu, R., P. Barragan, V. Garitey, P. O. Roquebert, J. Fuseri, P. Commeau, et al. Assessment of the trackability, flexibility, and conformability of coronary stents: A comparative analysis. Catheter Cardiovasc. Interv. 59(4):496–503, 2003.
Samady, H., P. Eshtehardi, M. C. McDaniel, J. Suo, S. S. Dhawan, C. Maynard, L. H. Timmins, A. A. Quyyumi, and D. P. Giddens. Coronary artery wall shear stress is associated with progression and transformation of atherosclerotic plaque and arterial remodeling in patients with coronary artery disease. Circulation 124:779–788, 2011.
Schmidt, W., N. Grabow, P. Behrens, and K. P. Schmitz. Trackability, crossability, and pushability of coronary stent systems—an experimental approach. Biomed. Tech. (Berl.) 47(1):124–126, 2002.
Scotti, C. M., and E. A. Finol. Compliant biomechanics of abdominal aortic aneurysms: a fluid-structure interaction study. Comput. Struct. 85:1097–1113, 2007.
Scotti, C. M., A. D. Shkolnik, S. C. Muluk, et al. Fluid-structure interaction in abdominal aortic aneurysms: effects of asymmetry and wall thickness. BioMed. Eng. OnLine 4:64, 2005.
Shaw, J. A., B. A. Kingwell, A. S. Walton, J. D. Cameron, P. Pillay, C. D. Gatzka, et al. Determinants of coronary artery compliance in subjects with and without angiographic coronary artery disease. J. Am. Coll. Cardiol. 39(10):1637–1643, 2002.
Sinusas, A. J., X. Papademetris, R. T. Constable, D. P. Dione, M. D. Slade, P. Shi, and J. S. Duncan. Quantification of 3-D regional myocardial deformation: shape-based analysis of magnetic resonance images. Am. J. Physiol. Heart Circ. Physiol. 281:H698–H714, 2001.
Steinman, D. A., Y. Hoi, P. Fahy, L. Morris, et al. Variability of CFD solutions for pressure and flow in a giant aneurysm: the SBC2012 CFD challenge. J. Biomech. Eng. 135(2):021016, 2013. doi:10.1115/1.4023382.
Szabadits, P., Z. Puskas, and J. Dobranszky. Flexibility and trackability of laser cut coronary stent systems. Acta Bioeng. Biomech. 11(3):11–18, 2009.
Takashima, K., R. Shimomura, T. Kitou, H. Terada, K. Yoshinaka, and K. Ikeuchi. Contact and friction between catheter and blood vessel. Tribol. Int. 40(2):319–328, 2007.
Vavuranakis, M., I. Stamatopoulos, T. G. Papaioannou, S. Nikolopoulos, K. Toutouzas, and C. Stefanadis. Alterations of pressure waveforms along the coronary arteries and the effect of microcirculatory vasodilation. Int. J. Cardiol. 117:254–259, 2007.
Weydahl, E. S., and J. E. Moore. Dynamic curvature strongly affects wall shear rates in a coronary artery bifurcation model. J. Biomech. 34:1189–1196, 2001.
Whittaker, D. R., J. Dwyer, and M. F. Fillinger. Prediction of altered endograft path during endovascular abdominal aortic aneurysm repair with the gore excluder. J. Vasc. Surg. 41(4):575–583, 2005.
Wijesinghe, L. D., D. J. A. Scott, and D. Kessel. Analysis of renal artery geometry may assist in the design of new stents for endovascular aortic aneurysm repair. Br. J. Surg. 84(6):797–799, 1997.
Williams, M. J. A., R. A. H. Stewart, C. J. S. Low, and G. T. Wilkins. Assessment of the mechanical properties of coronary arteries using intravascular ultrasound: an in vivo study. Int. J. Card. Imaging 15(4):287–294, 1999.
Wood, N. B., S. Z. Zhao, A. Zambanini, M. Jackson, W. Gedroyc, S. A. Thom, A. D. Hughes, and X. Y. Xu. Curvature and tortuosity of the superficial femoral artery: a possible risk factor for peripheral arterial disease. J. Appl. Physiol. 101(5):1412–1418, 2006.
Yin, C. P. F., Y. R. K. Strumpf, P. H. Chew, and S. L. Zeger. Quantification of the mechanical properties of noncontracting canine myocardium under simultaneous biaxial loading. J. Biomech. 20(6):577–589, 1987.
Zeng, D., Z. Ding, M. H. Friedman, and C. R. Ethier. Effects of cardiac motion on right coronary artery hemodynamics. Ann. Biomed. Eng. 31:420–429, 2003.
Zhao, S. Z., X. Y. Xu, A. D. Hughes, et al. Blood flow and vessel mechanics in a physiologically realistic model of a human carotid arterial bifurcation. J. Biomech. 33:975–984, 2000.
Zheng, S., and Y. Qi. Motion estimation of 3D coronary vessel skeletons from X-ray angiographic sequences. Comput. Med. Imaging Graph. 35(5):353–364, 2011.
Zoarski, G. H., J. M. Mathis, and J. R. Hebel. Performance characteristics of microcatheter systems in a standardized tortuous pathway. Am. J. Neuroradiol. 19(8):1571–1576, 1998.
Acknowledgments
The authors would like to acknowledge Strands I and III funding from the Department of Education in Ireland and IRCSET funding from the Irish Research Council.
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Studies
No human or animal studies were carried out by the authors for this article.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Ajit P. Yoganathan oversaw the review of this article.
Rights and permissions
About this article
Cite this article
Morris, L., Fahy, P., Stefanov, F. et al. The Effects That Cardiac Motion has on Coronary Hemodynamics and Catheter Trackability Forces for the Treatment of Coronary Artery Disease: An In Vitro Assessment. Cardiovasc Eng Tech 6, 430–449 (2015). https://doi.org/10.1007/s13239-015-0241-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13239-015-0241-y