Abstract
The treatment landscape for patients affected by gastric and colorectal cancer (G&CRC) has significantly broadened over the past decade. Molecular diagnostic methods have improved with a precision oncology-driven approach to the development of treatment options tailored to specific molecular targets, including the human epidermal growth factor 2 (HER2). While scientific evidence on the role of HER2 in G&CRC has improved, there has been a lag in general understanding and applications of testing for HER2+ G&CRC and resulting targeting treatment in the wider oncology community. To better understand and address the root causes of this gap, a needs assessment deployed among 85 oncology care providers was conducted and informed the development of an accredited online educational program entitled “GetSMART.” The program consisted of four modules developed and narrated by experts in gastrointestinal oncology. The educational content and assessment metrics were guided by a confidence-based assessment (CBA) model and the Moore, Green, and Gallis outcomes framework. Assessment methods consisted of quantitative pre- and post-activity tests, an evaluation embedded within the education (n = 163), and semi-structured interviews (n = 5) post-activity completion. Findings indicated that “GetSMART” enhanced participants’ knowledge, confidence, and intent to change practice in relation to their (1) identification of HER2 aberrations, (2) selection of appropriate treatments for HER2+ G&CRC, and (3) ability to engage patients in shared decision-making and management of adverse events. “GetSMART” can therefore be a valuable educational resource for oncology HCPs caring for patients affected by HER2+ metastatic G&CRC, offering strategies to ensure an optimal team and patient-centered approach to the care being delivered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric and colorectal cancers (G&CRC) are among the most incident and lethal cancers in the world [1]. When human epidermal growth factor 2 (HER2) is amplified or overexpressed, as is the case for about 20% of gastric cancers and 6% of colorectal cancers, there is an increased activation of cellular proliferation and differentiation pathways, tumor progression, metastasis, and resistance to treatment, which substantially affects the prognosis of patients with these cancers [2,3,4]. Increased HER2 signaling has been most widely associated with breast carcinomas, but a number of studies have shown similarly increased expression drives subsets of G&CRC.
Approaches to achieving accurate diagnosis and effective treatment for G&CRC have changed significantly over the past two decades, from the common use of immunohistochemistry (IHC) to the incorporation of fluorescence in situ hybridization (FISH), and also assessment of alterations using next-generation sequencing (NGS) [5]. For metastatic cases, improved molecular diagnostic methods accompanied by precision oncology-driven clinical trial designs have improved patients’ outcomes while more effectively tailoring treatment for individual patients [5]. The molecular testing of HER2, among other biomarkers, is strongly recommended in routine clinical practice to inform treatment decisions [6,7,8,9]. Despite increased evidence supporting routine evaluation and screening cases of HER2 amplification and respective use of targeted therapy in G&CRC, advances in this field have not been as readily recognized and adopted by healthcare professionals (HCPs) and the wider community [10].
An accredited online educational program entitled “GetSMART,” informed by a pre-intervention assessment survey, was deployed and evaluated to help address current educational gaps and needs of HCPs in the community. The program aimed to enhance learners’ knowledge and competencies in assessing and applying the molecular testing of G&CRC, including HER2 amplification and overexpression, prior to making an informed treatment decision with patients. The intended outcome was to help HCPs confidently offer an appropriate and balanced recommendation for the optimal treatment path of a patient with HER2+ mG&CRC. Critical components of the HCP’s communication with their patients would highlight the value of HER2 testing, the importance of accurate diagnosis and treatment selection, and communicate and address the need to skillfully monitor and manage adverse events (AEs) in the interest of optimizing safe and effective patient care. This paper presents the evaluation of the program, which aimed to assess the impact of “GetSMART” in terms of its educational outcomes and intent to change practice among learners when caring for patients with metastatic HER2+ G&CRC.
Materials and Methods
Program Description
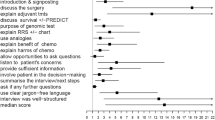
The educational content of “GetSMART” was informed by (phase 1) a needs assessment survey administered to 85 HCPs caring for patients with HER2+ mG&CRC. Supplementary information A summarizes the methods and results of this survey in alignment with the final learning objectives of the program. The program was comprised of four interactive online modules relevant to the following areas of care: identification of HER2 aberrations, selection of appropriate treatment for HER2+ G&CRC, and patient engagement in shared decision-making (SDM) and management of AEs. Each module engaged learners in approximately 20–30 min of didactic content, in addition to case scenarios and questions aimed to elicit both discussion and reflection. The content was developed and presented by clinical experts (co-authors EL, JM, AC, and TY) to help learners apply their knowledge in practice and consider changes in their approach to patient care. Relevant educational resources on the various topics were presented as reinforcement materials and made available to learners for download. Learners could obtain CME credit after correctly responding to 75% of the case-based questions. The program was launched in January 2021 and made available to learners through April 2022.
Evaluation Approach
A mixed-methods study design was used to evaluate (phase 2) the impact of the educational program. Methods included a (1) pre-post analysis of learners’ responses to matched assessment questions included in the educational activity; (2) descriptive analysis of learners’ responses to a formal evaluation immediately post-activity; and (3) qualitative interviews (20–30 min) with learners, at least 10 days after they had completed the activity. The evaluation was guided by the Moore, Green, and Gallis outcomes framework for planning and assessing continuing medical education (CME). The activity covered levels 1 (participation) to 5 (performance-self-reported) [11] and also included a confidence-based assessment (CBA) model to measure knowledge mastery [12]. To better understand the immediate impact of “GetSMART,” a comparison between pre- and (first attempt) post-activity assessment was decided.
Participants
The potential learners of “GetSMART” were targeted via an international outreach campaign, targeting members of oncology teams (e.g., physicians, registered nurses, and advanced practice providers). For the evaluation, participants consisted of those learners who took part in all four modules of the activity, provided consent for including their data in the analysis, and/or agreed to participate in the interview.
Data Collection
Data collection tools were developed in line with the guiding evaluation frameworks [11, 12], the learning objectives of the program, and the four targeted areas of care. Upon registration, learners were invited to provide their country, profession, specialty, and years of practice. Before and after completing modules, learners responded to knowledge-based multiple-choice questions and rated their confidence in response (1 = I’m guessing, 2 = I think, 3 = I’m sure). They were also asked to rate their perceived confidence (1 = not at all confident, 3 = neutral, 5 = very confident) and frequency (1 = never, 3 = sometimes, 5 = always) in performing specific behaviors at baseline and post-activity. A formal evaluation questionnaire was presented to learners immediately after completion of all four modules to collect learners’ perceptions of the program and intent to change specific elements in their individual and interprofessional practice. Learners were allowed to skip questions if they did not wish to respond. Interviews were conducted post-activity over a secure conference line (Zoom Video Communications Inc., 2022) by an expert moderator from AXDEV Group Inc. Questions were open-ended to elicit insights and reflections gained by learners, in addition to the anticipated impact on clinical practice, and remaining challenges and barriers to overcome. Interviews were recorded and transcribed.
Analysis and Integration of Methods
The responses to open-ended questions and transcripts of interviews were coded and thematically analyzed in NVivo Version 12 (QSR International Pty Ltd., 2021) using an inductive reasoning approach that allowed the exploration of emerging trends and patterns [13] by a trained researcher at AXDEV Group Inc. Data derived from the quantitative assessment questions of learners were matched across data collection points (i.e., pre- and post-activity) and imported into SPSS Statistics (Version 27.0, IBM Corp., Armonk, NY, USA). Knowledge-based responses were dichotomized based on correctness and confidence in participants’ responses [12]. Participants who provided a correct response and were “sure” about it were classified as having achieved “mastery.” Confidence ratings of “5 = very confident” and “4 = somewhat confident” were grouped as “confident.” Frequency ratings of “5 = always” and “4 = often” were grouped as “always or often.” McNemar statistical tests were performed to measure the direction, magnitude, and significance of change between matched, dichotomized pre- and post-activity responses [14]. Descriptive analysis was performed on post-activity evaluation responses. Missing values were excluded. Quantitative and qualitative findings were linked to their respective learning objective and integrated based on their complementary nature to obtain a full understanding of the impact of “GetSMART” [15].
Results
Sample Size
Among the 284 learners who completed all four modules of the “GetSMART” program and its post-activity evaluation, 163 provided consent to have their data analyzed for reporting, of which 121 reported on their profession and specialty: 50% were registered nurses (RN), 18% physician assistants (PA), 14% medical doctors (MD), 6% pharmacists (PharmD), and 5% other. Specialties included oncology (32%), hematology/oncology (29%), general practice/internal medicine (11%), and other (28%). Of those who reported their country (n = 101), 92% were from the USA. The remaining participants opted out of the research study. Five qualitative interviews were completed with the following professions represented: RN specialized in oncology (n = 2), MD specialized in hematology/oncology (n = 1), MD specialized in gastroenterology (n = 1), and PharmD (n = 1), all from the USA.
Main Findings
Pre-activity assessment questions of the learners who completed “GetSMART” confirmed that a majority had knowledge gaps when starting the activity (mean = 69% of learners not having selected accurate responses). Confidence pertaining to each of the learning objectives of “GetSMART” was low (mean = 71% of learners with a gap). The highest percentage of learners at baseline who demonstrated knowledge accuracy was 63%, specifically regarding the appropriateness of HER2 testing according to the NCCN guidelines for colorectal cancer. However, only 8% demonstrated knowledge mastery of this topic. An average of 59% of learners reported “never,” “seldom,” or “sometimes,” considering molecular testing results in the selection of treatment options for advanced G&CRC and 51% engaging patients with metastatic G&CRC in SDM.
Post-activity, “GetSMART” showed a significant impact (two-sided p < 0.05 for McNemar test) on the increased percentage of participants with a successful educational outcome (level 3 – knowledge, level 4 – confidence, and level 5 – performance) for many of the learning objectives (Tables 1, 2, and 3). The greatest gains were found for the percentage of learners post-activity with knowledge accuracy regarding the proportion of gastric cancers that are HER2-positive (+19%, p = 0.002, Table 1); knowledge mastery of AEs that should be monitored for patients receiving a HER2-targeted therapy (+21%, p < 0.001, Table 3); confidence identifying treatment for patients with advanced G&CRC based on molecular testing results (+35%, p < 0.001, Table 2); confidence anticipating and managing side effects related to HER2-targeted therapies (+16%, p < 0.001, Table 3); and intent to consider “always” or “often” HER2-targeted therapy as an option for patients with mG&CRC (+23%, p < 0.001, Table 2).
Evaluation-based responses showed that 82% of learners agreed that as a result of participating in “GetSMART,” they were better able to fulfill each of the learning objectives outlined in Tables 1, 2, and 3 (outcome level 4 – competency). In addition, 84% agreed that they were better able to recognize the barriers that prevent the acceptance or adoption of new clinical evidence into practice behaviors. A majority of learners (69%) projected a “moderate” or “major” impact on their performance (outcome level 5 – performance).
Reflections shared by participants who responded to open-ended questions of the evaluation and completed interviews emphasized the importance of leveraging a team-based approach to care when promptly ordering molecular test results, educating patients regarding the value of testing, and supporting an informed treatment decision. For example, an MD specialized in hematology/oncology mentioned: “My Nurse Navigator, I basically empowered her […] that she automatically gets those tests sent off right away […] To make sure that nothing has slipped through the cracks. Before I had to order it specifically, and now, it’s getting automatically done.” While an RN specialized in oncology reported in her evaluation to committing to the following as a result of attending the activity: “Check to see if HER2 testing has been ordered on any new metastatic gastric patient that I meet for intake.”
The remaining barriers or challenges that were noted by learners in their interviews were related to (a) patients resisting or refusing molecular testing due to low socioeconomic status and/or ability to afford medication; (b) complexities of obtaining financial reimbursement for certain molecular tests and targeted therapies by insurance companies; and (c) a need to ensure organizational processes are available to strengthen interprofessional collaboration when selecting treatment decisions and managing AEs. For example, an interviewed pharmacist mentioned: “the nurses may not be as comfortable talking to patients about medications and explaining how to take it, or what reactions they might have […] We [pharmacists] can always be involved in the medication counseling part of it, regardless of what treatment it is.” In comparison, an MD specializing in gastroenterology shared: “two opinions are always better than one opinion. And if I miss something, somebody else will remind me about it. The program has stressed the importance of collaboration.”
Discussion
“GetSMART” informed HCPs, mostly located in the USA, involved in the care of patients affected by G&CRC. The program employed a survey to identify the gaps that were most crucial to address, informing the development and refinement of the program’s learning objectives and educational content. It engaged a range of professions, including mostly registered nurses, who play a central role in patient communication, coordination, and education, and can influence diagnostic and treatment decisions during tumor board discussions. The baseline assessment embedded within “GetSMART” confirmed the findings of the survey, appropriately addressing identified knowledge and confidence gaps related to the (1) identification of HER2 aberrations, (2) selection of appropriate treatments for HER2+ G&CRC, and (3) patient engagement in SDM and management of AEs.
In line with the Moore, Green, and Gallis (2009) framework [11], this mixed-methods evaluation assessed changes in educational outcomes at multiple levels: knowledge, competencies, and performance, which aim to improve patient outcomes (i.e., higher-level outcomes). The results obtained from the evaluation of “GetSMART” showed a remaining need to enhance clinicians’ knowledge in relation to precision-medicine and team-based care affecting patients with G&CRC due to HER2+ status, which suggests that current interventions focusing on knowledge acquisition are appropriate. Indeed, changes in skill, performance, and patient outcomes are possible after a thorough understanding of the foundational evidence in the field is established (i.e., clinicians’ knowledge is current and reflective of scientific advancements). After this initial step of performance improvement is achieved, there is an opportunity to incorporate additional strategies into performance improvement efforts, such as guided action plans with audit feedback.
The interprofessional nature of oncology care and the need to engage learners from multiple disciplines in interventions, such as “GetSMART,” is especially worth highlighting. While this concept equally applies to therapeutic areas outside of oncology, we should remind ourselves that patients affected by an illness as severe as cancer need to rapidly grasp the state of their health to be able to properly engage in a treatment and management plan most suitable to their needs, preferences, and socioeconomic circumstances (e.g., access to insurance coverage or ability to pay for the cost of molecular tests and targeted therapies). Consistent messaging from all professionals and specialists involved in the care of affected patients, who offer them evidence-based recommendations in line with their expected roles and responsibilities, is critical to ensure patients are knowledgeable of the best diagnostic and therapeutic options available to them. As demonstrated by the results of this study, patients facing high out-of-pocket costs may be reluctant to undergo molecular tests, even if recommended by their HCP. Hence, the involvement of social workers and nurses in diagnostic and treatment decisions affected by patients’ insurance coverage and/or other types of financial assistance programs (e.g., Medicare and Medicaid) is necessary. Future interventions should consider developing activities aimed at facilitating communication and collaboration among professionals and specialists involved in HER2+ G&CRC, especially at the metastatic stage. This could be achieved through a revision of organizational processes by clinical leaders and facilitated multidisciplinary team discussions related to points during which communication and collaboration between all professions and specialties can be enhanced. A limitation of this study was the smaller participation rate of gastroenterologists and oncologists, groups that are vital and most likely to influence diagnostic testing, therapeutic decision-making, and communications with this patient population. Additional efforts should be made to effectively inform this group of HCPs pertaining to available educational activities, such as “GetSMART” and future activities alike.
Conclusion
“GetSMART” provided a foundation for addressing the pressing needs of HCPs involved in the care of patients affected by G&CRC due to HER2 aberrations. The intervention showed a positive impact on knowledge and confidence gains, in addition to anticipated performance in clinical practice that should enhance the health outcomes of patients affected by HER2+ G&CRC at the metastatic stage. The identification of HER2 aberrations in metastatic G&CRC and its appropriate treatment selection and management of AEs remains an ongoing challenge in oncology care that requires continued efforts to remain up-to-date regarding the value of testing. HCPs should be mindful of how to take steps to ensure an optimal team and patient-centered approach to care is being delivered to their patients.
Data Availability
Anonymized datasets used/analysed for this article can be made available upon reasonable request to the corresponding author.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424
Wang G, He Y, Sun Y, Wang W, Qian X, Yu X et al (2020) Prevalence, prognosis and predictive status of HER2 amplification in anti-EGFR-resistant metastatic colorectal cancer. Clin Translational Oncolog 22:813–822
Janjigian YY, Werner D, Pauligk C, Steinmetz K, Kelsen DP, Jäger E et al (2012) Prognosis of metastatic gastric and gastroesophageal junction cancer by HER2 status: a European and USA International collaborative analysis. Annals Oncol 23:2656–2662
Seo AN, Kwak Y, Kim DW, Kang SB, Choe G, Kim WH et al (2014) HER2 status in colorectal cancer: its clinical significance and the relationship between HER2 gene amplification and expression. PLoS One 9:e98528
Matsuoka T, Yashiro M (2020) Precision medicine for gastrointestinal cancer: recent progress and future perspective. World J Gastrointest Oncol 12:1–20
Lordick F, Carneiro F, Cascinu S, Fleitas T, Haustermans K, Piessen G et al (2022) Gastric cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up. Annals Oncolog 33:1005–1020
Benson AB, Venook AP, Al-Hawary MM, Arain MA, Chen Y-J, Ciombor KK et al (2020) NCCN guidelines insights: rectal cancer, version 6.2020: featured updates to the NCCN guidelines. J National Comprehen Cancer Netw 18:806–815
Ajani JA, D’Amico TA, Bentrem DJ, Chao J, Cooke D, Corvera C et al (2022) Gastric cancer, version 2.2022, NCCN clinical practice guidelines in oncology. J National Comprehensive Cancer Netw 20:167–192
Benson AB, Venook AP, Al-Hawary MM, Arain MA, Chen Y-J, Ciombor KK et al (2021) Colon cancer, version 2.2021, NCCN clinical practice guidelines in oncology. J National Comprehensive Cancer Netw 19:329–359
Hamilton N, Jacobs G, Augustyniak M, Fineberg S, Kaklamni V, McFadden P (2022) Informing the professional improvement of skills among oncology providers educating patients with HER2+ breast cancer, Presented at ONS 47th Annual Congress. Oncology Nursing Forum 49(2):E153–E154
Moore DE Jr, Green JS, Gallis HA (2009) Achieving desired results and improved outcomes: integrating planning and assessment throughout learning activities. J Continuing Educ Health Prof 29:1–15
Maqsood R, Ceravolo P (2018) “Corrective feedback and its implications on students’ confidence-based assessment,” In: International Conference on Technology Enhanced Assessment, pp. 55-72
Chapman A, Hadfield M, Chapman C (2015) Qualitative research in healthcare: an introduction to grounded theory using thematic analysis. J Royal College Phys Edinburgh 45:201–205
Adedokun OA, Burgess WD (2012) Analysis of paired dichotomous data: a gentle introduction to the McNemar test in SPSS. J MultiDisciplinary Eval 8:125–131
Bazeley P, Kemp L (2012) Mosaics, triangles, and DNA: metaphors for integrated analysis in mixed methods research. J Mixed Meth Res 6:55–72
Acknowledgements
The authors would like to acknowledge the support provided by Pam McFadden (Vice President, AXDEV Group Inc.) for supporting project administration, Patrice Lazure (Director of Research, AXDEV Group Inc.) for his guidance on the research components of this study, Randa Dalle (Project Manager, AXDEV Group Inc.) and Karen Mariano (Project Manager, Antidote Education Company) who supported coordination of tasks between collaborators and monitoring of data collection, and all the participants who took part in this study. An Independent Medical Education (IME) grant was provided by Daiichi-Sankyo to Antidote Education Company to support this initiative.
Author information
Authors and Affiliations
Contributions
Conceptualization: GJ and MF
Methodology: MA and GJ
Resources (i.e., development of education): EL, MF, JM, AC, and TY
Software: not applicable
Investigation: MA and GJ
Data curation: MA
Formal analysis: MA
Validation: EL, GJ JM, MF, AC, and TY
Writing – original draft: MA and GJ
Writing – review and editing: EL, JM, MF, AC, and TY
Visualization: MA
Supervision: GJ and MF
Project administration: MF
Funding acquisition: GJ and MF
Corresponding author
Ethics declarations
Ethics Approval
This study was conducted in accordance with the Declaration of Helsinki and national ethical standards (i.e., US Code of Federal Regulations 21 CFR Parts 50 and 56 and 45 CFR Part 46; the Tri-Council Policy Statement: Ethical Conduct for Research Involving Humans, TCPS). The research protocol and related documents were reviewed and approved by an Independent Review Board (IRB Veritas, Tracking Number: 2021-2550-8115-1, Study Number: GB-20-010).
Research Involving Human Participants and/or Animals
This study involved human participants.
Informed Consent
Only anonymized data from learners who agreed to opt-in via informed consent were included in this study.
Competing Interests
MA is an employee of AXDEV Group, Inc.; EL reports research grants from the American Cancer Society (RSG-22-022-01-CDP) and the Minnesota Ovarian Cancer Alliance; honorarium and travel expenses for a research talk at GlaxoSmithKline; honoraria and travel expenses for lab-based research talks and equipment for laboratory-based research, Novocure, Ltd.; compensation for scientific review of proposed printed content, Elsevier Publishing and Johns Hopkins Press; consultant, Nomocan Pharmaceuticals (no financial compensation); Scientific Advisory Board Member, Minnetronix, LLC, 2018–present (no financial compensation); consultant and speaker honorarium, Boston Scientific US, 2019; Institutional Principal Investigator for clinical trials sponsored by Celgene, Novocure, Intima Biosciences, and the National Cancer Institute, and University of Minnesota membership in the Caris Life Sciences Precision Oncology Alliance (no financial compensation). GJ is an employee of AXDEV Global Inc.; MF is an employee of Antidote Education Company. JM reports receipt of honorarium from Pfizer, AZ, Merck, Taiho, Bayer, Seagen, Caris, and Indivumed. AC reports involvement in adboards and or speaker for Amgen, Astra Zeneca, Astellas, Bayer, BMS, Merck Group, MSD, Ipsen, Lilly, Novartis, Roche, Pfizer, and Servier. TY reports research grants from Amgen, Chugai Pharmaceutical, Daiichi Sankyo, Eisai, FALCO Biosystems, Genomedia Inc., Molecular Health GmbH, MSD, Nippon Boehringer Ingelheim, Ono Pharmaceutical, Pfizer Japan, Roche Diagnostics, Sanofi K.K., Sysmex Corp., and Taiho Pharmaceutical; and honorarium from Bayer Yakuhin, Chugai Pharmaceutical, Merck Biopharma, MSD, Ono Pharmaceutical, Takeda Pharmaceutical, and Sumitomo Corp. EL, JM, AC, and TY received an honorarium from Antidote Education Company as part of this educational activity.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Augustyniak, M., Lou, E., Jacobs, G. et al. Learning Outcomes of “GetSMART,” Education for Diagnostics and Targeted Treatment for HER2+ Metastatic Gastric and Colorectal Cancers. J Canc Educ 39, 118–125 (2024). https://doi.org/10.1007/s13187-023-02384-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-023-02384-8