Abstract
African American (AA) and Latino populations are impacted disproportionately by cancer incidence and mortality compared to the general US population. Contributing to these rates are multiple inheritable cancers that impact both men and women. Some of these diseases may be detected through genetic counseling and germline DNA testing; however, AA and Latinos are unaware and have limited knowledge and thus significantly underutilize these services and technologies. Research to detect influencing factors to testing uptake has also been slow due to multiple factors. The research team followed a community-based participatory research (CBPR) approach and worked with a Community Advisory Board composed of cancer survivors and co-survivors to design the exploratory study. Six focus groups were held with a pilot sample of African Americans and Latinos who self-reported to be at-risk for cancer (N = 53). The study was held over a 2-month period where attitudes, perceptions, and beliefs about cancer risk and preference regarding cancer-related genetic counseling and testing risk communication were explored. Themes that emerged included (1) the lack of knowledge about cancer-related genetic counseling and testing; (2) cancer is feared often; (3) cancer-related genetic testing was perceived as something that could help but was also perceived as unnecessary testing that exposed individuals to medical harm; and (4) benefits to test were perceived as favorable for medical personnel but not for the patient. Implications of the study provide a unique lens to explore how lived experiences among AA and Latinos may inform strategic risk communication about cancer-related genetic counseling and testing and help advance cancer health equity. Participants viewed cancer genetic testing as important cancer risk prevention strategies. Identification of perceptions of cancer risk and cancer-related genetic counseling and testing in collaboration with members of the community is needed to bolster communication efforts among these populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the era of precision medicine, advancements of cancer genetic and genomic technologies have grown exponentially, expanding healthcare (Patch & Middleton 2018) and informing community and public health efforts (Senier et al. 2019). While these technologies are accessible to some, awareness, knowledge of, and integration into clinical care are limited, particularly among racial/ethnic populations where health disparities persist and impede cancer health equity (Alcaraz et al. 2020). African American and Latino populations continue to experience disproportionate cancer incidence compared to most of the US population. The probability of an increased risk of dying from cancer also is higher among these populations (ACS 2019) and further illustrates deficits in cancer prevention and cancer care across the continuum. Contributing to these rates are multiple inheritable cancers that impact both men and women. For example, Latina women show an overall incidence of breast cancer lower than White women. However, breast cancer is often diagnosed at a later stage, and tumors are larger than in White women (DeSantis et al. 2019; Lynce et al. 2016). Among African American women, age-adjusted breast cancer mortality is nearly 40% higher (Jatoi et al. 2022), and there is higher breast cancer incidence before age 40, but incidence is lower between the ages 65 to 84. The likelihood of death from breast cancer however is higher among African American women at every age. African American and Latino men are also disproportionately impacted by cancer, having the highest mortality rate for prostate cancer compared to all other racial/ethnic groups (NCI 2021).
Approximately 10% of most cancers are attributable to inherited cancer syndromes and significantly elevated where the age at onset is even younger than in the general population (Ricker et al. 2018) (p. 85). Some of these inherited syndromes may be detected through genetic counseling and germline DNA testing prior to a cancer diagnosis; however, there is disproportionate genetic counseling and germline DNA testing among African Americans and Latinos (Canedo et al. 2019; Carroll et al. 2020; Singer et al. 2004) due to several barriers. Mistrust of medical personnel (Corbie-Smith et al. 2002; Singer et al. 2004), limited access to cancer risk assessment (Komenaka et al. 2016) (Ricker et al. 2006), low awareness ( Halbert et al. 2005; Hann et al. 2017; Singer et al. 2004), limited knowledge, and other patient-level, psycho-social factors (Olaya et al. 2009) contribute to low rates of genetic testing in African American and Latino populations. A growing body of research shows how risk perceptions about cancer-related genetic testing among racial/ethnic minorities (Chavez-Yenter et al. 2020; Peterson et al. 2018) may contribute to disproportionate counseling and testing approaches for prevention and early detection of inheritable cancers. Gaps in physician recommendations (McCarthy et al. 2016) could also explain disparities among racial/ethnic minority populations. Identification of individual-level and other structural/environmental barriers serves as a guide for health communication strategy and clinical practice and how to effectively communicate cancer risk among racial/ethnic minority (patient) populations. Available and accessible hereditary disease history information and thus the probability of inheritability of cancer and other risk factors through an inherited cancer syndrome risk assessment are additional pieces of information for informed decision-making between provider and patient (Timmermans 2020). Precision cancer prevention communication that is holistic rather than focused singularly on an oncological lens (Butler et al. 2022) provides an avenue to view multiple factors that may impact cancer prevention health equity.
Cancer risk and prevention in the context of cancer-related genetic testing risk communication is an area of clinical health communication where the inclusion of risk messaging may guide strategy for genetic testing. The present study acknowledges previous research but applies a novel community-engaged approach and to our knowledge is one of the first to inform the development of a risk communication model designed to strengthen genetic counseling and testing efforts and advance cancer health equity information among racial/ethnic minority populations. Drawing from robust literature and identifying psycho-social factors among the pilot sample, we reveal areas that will be critical for a clinical risk communication model to address cancer screening disparities.
Communicating cancer risk with cancer-related genetic testing among racial/ethnic minority populations
Identification of risk factors for disease is a critical component for calculating and assessing risk (Lautenbach et al. 2013). Those risks are partially determined by modifiable (e.g., lifestyle) and non-modifiable (e.g., genetics) factors. Communicating risk for genetic variations and other health conditions to the public presents multiple challenges including limited awareness and knowledge about basic genetic and genomic concepts among patients and clinicians; minimal understanding of the influence of family health history among those at risk; misinformation or distortion of information through mass media and direct advertising; and overall gaps in communication or cancer risk on multiple levels (Parrott et al. 2015).
Risk communication at an individual level enables those at a predicted increased risk of developing cancer to make informed decisions. Understanding risk perception about cancer and how these perceptions influence genetic counseling and testing among diverse populations could help guide effective clinical and public health communication strategies to address testing disparities. Judgment of risk acceptability also impacts how individuals make decisions about their health and actively seek care. The level of risk and how they evaluate and interpret the risk are influenced by multiple factors (i.e., fairness, benefits, alternatives, control, voluntariness) and will determine acceptance (Covelo 1991). Tailored approaches which include absolute risk or risk that is relevant compared to non-tailored approaches are more effective (Lautenbach et al. 2013; Kreuter et al. 2003). These approaches have the potential to increase salience of information and to positively impact attitudes, perceptions, and beliefs about the value of cancer-related genetic counseling and testing. Furthermore, culturally inclusive approaches maximize opportunities for equitable knowledge gathering, health information sharing, and dissemination.
Identification of attitudes, perceptions, and beliefs among racial/ethnic populations is critical for culturally appropriate cancer communication (Kinney et al. 2010; McQueen et al. 2011). Lack of culturally appropriate cancer-related genetic testing information (Peterson et al. 2018) and counseling risk communication strategies among minority and underserved populations (Jones et al. 2016; McCarthy et al. 2016; Smith et al. 2016) are contributors to disparities among these populations (Chavez-Yenter et al. 2020; Pagán et al. 2009). Furthermore, barriers such as genetic counselor bias, lack of diversity within the profession (Price et al. 2020), mistrust for medical personnel, access to health care, and education (Halbert et al. 2005) contribute to these disparities. Observational research shows gaps exist among racial/ethnic populations and attitudes, perceptions, and beliefs that hinder testing (Peterson et al. 2018), but more can be gained through engagement of and with community members from these populations; contribution to equitable cancer education and clinical communication models is also plausible. Mounting evidence demonstrates added value aspects of conducting research in partnership with non-research–trained stakeholders (Domecq et al. 2014), and much of the literature points to the importance of establishing trustworthy, bi-directional communications to achieve outcomes (Roche et al. 2020; Harrison et al. 2019).
The research team followed a community-based participatory approach (CBPR) which rests on a continuous establishing a trusting relationship between the researcher and patient partner(s). In this study, CBPR was the platform chosen to explore attitudes, perceptions, and beliefs toward cancer and cancer-related genetic counseling and testing among a pilot sample of African Americans and Latinos. Additionally, participants shared their views on cancer-related genetic counseling and testing (i.e., genetic susceptibility testing) risk communication as a cancer risk prevention strategy.
Methods
Study design
Data were collected through a CBPR process that included forming a specific study community advisory board (CAB) from other existing African American and Latino CABs. The CAB guided the research focus and informed the research design and consisted of two African American cancer survivors and one Latina cancer co-survivor (an individual who lends support beginning at diagnosis through treatment). The research team included a genetic counselor, a precision medicine scientist, two social scientists, the director of a Latino center for health, and one physician scientist. Focus groups were conducted to collect data on participants’ experiences with cancer and cancer-related genetic counseling and testing and their perceptions about cancer-related genetic counseling and testing risk communication. The Theory of Planned Behavior (Ajzen 1991) guided focus group discussions where the constructs (attitude, subjective norms, perceived behavioral control) were used to explore participants’ attitudes, perceptions, and beliefs about cancer and cancer-related genetic counseling and testing. The team used Covelo’s risk perception model (Covelo 1991) to guide the discussion about communicating risk for cancer and genetic susceptibility testing. These constructs guided the analysis and exploration of how participants’ lived experiences shaped their perceptions about cancer risk based on inherited factors and their likelihood to explore genetic counseling and testing. The team also used a previous pilot study’s findings as a guide for the present study (Lumpkins et al. 2020). The University of Kansas Medical Center Institutional Review Board (IRB #00142461) approved the study.
Study population
The study team recruited focus group participants in 2019 using existing community networks. Individuals eligible to participate in the study self-identified as either African American and/or Latino, were able to communicate in English, were at least 18 years old, self-identified as a cancer survivor or cancer co-survivor, identified as being either high or moderate risk for cancer, or had a family history of cancer.
Engagement with CAB
The CAB met monthly with the research team between October 2018 and March of 2019 to discuss the research design. CAB members reviewed a moderator’s guide from a previous study conducted with African American faith populations (Lumpkins et al. 2020) and developed a guide for the study with African American and Latino populations. Members also agreed and finalized the study’s focus group recruitment strategy, focus group procedures, and survey. The semi-structured guide included the following four domains of interest (see Table 1): (1) experiences with cancer and genetic testing for cancer risk; (2) Cancer-related genetic counseling and testing; (3) Cancer-related genetic counseling and testing risk communication; and (4) Barriers to screening.
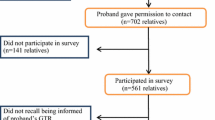
Recruitment
A purposive sampling technique was used to recruit from within African American and Latino networks in the Kansas City metropolitan area with the support of the CAB; JUNTOS Center for Advancing Latino Health (JUNTOS), a community-academic partnership to improve Latino health; and Faith Works Connecting for a Health Community (FWCFHC), a consortium created to address cancer disparities among African American faith communities. This process included posting recruitment flyers on the JUNTOS social media page and community-based locations and flyers handed out to FWCFHC consortium members during meetings and announcements given by church pastors and health ministry leaders during worship service and other church activities. Recruitment occurred from January to March 2019. Three research assistants reflecting the study population called or emailed individuals to determine eligibility, answered questions, and enrolled participants in specific focus group sessions (N = 6).
Focus group procedures
The study team held focus groups between March and May of 2019 at the University of Kansas Medical Center campus with easily accessible parking and public transportation access for participants. Participants were given a written, informed consent document prior to the start of the focus group. A study staff member also engaged in conversation and answered questions. Prior to the start of the focus group, participants completed a survey about cancer screening, genetic counseling, and genetic testing intention and completion. Study staff that included a moderator, co-moderator, and note-taker assigned participants in a circular seating arrangement. Three African American and 3 Latino focus groups were held between 70 and 90 min and included 4 to 13 participants in each group. Participants received a $25 gift card as an honorarium. The research team recorded all but one of the focus groups and subsequently transcribed recorded discussions for data analysis. One African American focus group discussion recording was missing from the analysis because of audio recording failure; however, the team included focus group notes in the analyses. The principal investigator, co-investigator from JUNTOS, translational scientist, and physician scientist reviewed each transcript for analysis.
Analysis
Three social science researchers and one physician scientist followed an open coding and constant comparison method (Denzin and Lincoln 2011) to identify themes. Coders met between October 2019 and May 2020 to analyze the collected data. The coders first individually analyzed transcripts and subsequently came together to discuss and form a consensus for overarching categories and phrases, words, and a preliminary identification of codes and themes. A score sheet was subsequently created to quantify how phrases appeared and fit within these categories during each focus group discussion. After coders completed this step, the research assistant compiled the data, and the coders subsequently met as a team one final time to discuss the categories and emerging themes across all focus groups. From this analysis, coders identified five themes.
Results
Focus group discussions were guided by a semi-structured interview guide (Table 1) and mirrored survey results that illuminated social determinants of health that impede cancer health equity (Alcaraz et al. 2020). Key themes that emerged about cancer-related genetic counseling and testing and communication of testing technology among racial/ethnic minority communities (Table 2) also yielded identifiable factors (individual and structural) that hinder equitable precision cancer prevention (Butler et al. 2022) among the study sample (Table 3). Participants were primarily female (92%), had at least a high school education (76%), and had not seen a genetic counselor (87%) even when self-reporting as high or at moderate risk for cancer (Table 4). Coders identified five overarching themes through their analysis. First, participants had limited knowledge about cancer-related genetic counseling and testing. They also shared a fear of cancer, believing that cancer is (often) fatal. Another theme that emerged from focus group discussions included the perception of risk associated with cancer-related counseling and testing; this perception was a barrier to participating in cancer-related genetic counseling and testing. Participants also saw the benefit to participate in counseling and testing as a benefit for others. Finally, participants believed it was important to culturally tailor this type of information.
Themes
Knowledge gap about cancer-related genetic counseling and testing
There was an overall knowledge gap for cancer-related genetic counseling and testing among both African American and Latino focus group members. Participants drew from their experiences as cancer survivors, cancer co- survivors, and those who self-identified as at risk for cancer.
“I think that it is good reason for genetic testing because I hear women say she had breast cancer and then her momma had it and her sister had it, I think when it’s hitting family like that I think that genetic testing would be good because they would benefit from it because they would be aware before they even end up with the symptoms…” (African American participant, 4–16-19).
“I wonder why it was a question at all if genetic testing should be available because if there is a way to just be knowledgeable about what is going on with your body, anybody, I would think that would just be automatic, instead of just being offered now.” (African American participant, 3–30-19).
“I’m 43 and I have never been offered a genetic test and it’s, you know, I have been sitting here thinking about I have been going to the same person or the same clinic for 10 years and never once have they said maybe we should do this or maybe we should do that.” (Latino participant, 4–17-19).
Cancer is feared and (often) fatal
Participants responded that their experiences with cancer were associated with finality of life, i.e., “it (cancer) was a death sentence.” This observation is consistent with an existing body of literature that reports perceived cancer fatalism reduces an individual’s desire to pursue cancer prevention screening (Powe and Finnie 2003). Among racial/ethnic populations, fear also presents and perpetuates barriers to cancer treatment, therapies, and throughout the cancer continuum (Dettenborn et al. 2004).
“Cancer, it scares me; yes, it just scares me. I lost my sister to cancer and a close friend; my feeling is just they are automatically dead.” (African American participant, 4–16-2019).
“Limited time. You have an expiration date.” (Latino participant, 4–17-2019).
“Fear, a lot of times when people are diagnosed with cancer, fear creates a lot of things in their mind, in my opinion, you can’t do anything about it.” (African American participant, 3–30-19).
“When you hear about cancer, we are scared and now I remember years ago in Mexico, everybody went talking about cancer and thinking we will die, maybe one month, two month and it’s very sad.” (Latino participant, 5–9-19).
A sub-theme of spirituality informed perceptions about cancer and testing also emerged among African American focus groups.
“What he (the physician) said he would do; I don’t agree with it. He knows that I don’t agree with it. So, I already know I am going to talk to my spiritual healers, my people and see what they think I should do.” (African American participant, 4–16-2019).
“You have to believe that God loves you. You have to believe that there is somebody bigger than you and that allows you to wake up in the morning. If you don’t believe that, it’s easy to say a lot…if you don’t walk in that faith.” (African American participant, 4–16-2019).
Perceived risk of cancer and cancer-related genetic counseling and testing
Participants saw the discovery of cancer risk through medical practice and research as valuable for cancer prevention. They also saw it as an avenue to surreptitiously extrapolate data and information from vulnerable individuals and the potential to expose them to harmful practices that lead to cancer. Participants discussed how medical practice and research agendas may expose them to harmful practices that lead to cancer.
“My mom died in Mexico; it was 1996. The doctor said they would like to give a test just for (us) girls; we said no, we don’t want to be a guinea pig. I’m sorry, we didn’t know what kind of cancer my mom had but I don’t want to be a guinea pig for you, sorry no. And the four of us were like I won’t do it.” (Latino participant, 5–17-19).
“Don’t bull “stuff” things with me when it comes to medical. They can say it all they want to (genetic information) but I don’t know…so when you are bringing up other stuff, you are letting them know you are trying to dodge and weave the focus point of what we are doing.” (African American participant, 4–16-19).
“It’s the fear, because the misconception of what the test is going to be doing, you know they think that if you do the genetic testing, that it’s going to diagnose to whether or not you are going to have a cancer and that’s not it. You know what I mean, it’s the lack of education is going to be doing, what kind of information it is going to provide. So, I think it’s the misconception is what it is that’s what prevents people from doing it.” (African American participant, 4–16-19).
The overall sentiment was that the “test” had more to offer the scientific and medical establishments rather than provide direct value to the individual. These two racial/ethnic groups differed slightly where Latino participants expressed concern for being a target for research experiments.
“There was a huge resistance in my family to get the test done and it happens here, and it happens in Spain where the doctors are pushing it like a lot and to me it was painful to see my family and I include myself on it because I didn’t do it either, but you see the ones that were most to have it because this was more on my mother’s side not on my father’s side.” (Latino participant, 5-17-2019).
African American participants were especially wary of doctors and mistrustful of the process. They were disappointed about limited awareness and knowledge of this type of information and testing.
“I feel like the power of the many is in the hands of the few. And they don’t look like you, they are not at your level, they are the six people sitting at the head office who, hey I am friends with this head of the pharmaceutical company, we know the FDA thing.” (African American participant, 4–16-19).
Limited benefits to participate in cancer-related genetic counseling and testing
Participants discussed the benefits to cancer-related genetic counseling and testing and the direct tie to the benefits of others (medical personnel/researchers), however not for the receiver/patient. The team found that even if the genetic counseling and constitutional DNA testing was offered at no cost, the long-term benefits from the information provided was seen as only leading to additional complications and burdens for the participant. Individuals within the sample felt their limited awareness about the test minimized the rationale to participate in testing and negatively impacted how they felt others interpreted and could use the test for cancer prevention and risk. Participants were also concerned how this information would help them after the study along with the burden of additional costs associated with positive results from counseling and genetic testing (e.g., cost for further diagnostic testing, surgery, treatment).
“Open, being super honest about it. If you are going to explain what is going to happen and why it is done and what are the benefits not for yourself but for the community, like you are going to get like twenty bucks for this. We are not silly, we are not dumb, so it’s not about the money, like why is this important?” (Latino participant – May 9, 2019).
“I just want to make sure you are not going to take my information and sell it to someone else. I want to make sure when I give you my genetic, my genetic makeup, this is what my DNA looks like you are not going to, oh let’s just pull that one black lady that now everybody has got genes off of her body.” (African American participant – 3–30-2019).
A sub-theme among Latino groups was also the fear of their immigration status.
“They wanted to scare us and do it too because I am an immigrant and we (are) scared to go see any doctor and they say no. I am an immigrant, and I am scared but that is one of the things that happened to us, especially here in the hospital.” (Latino Focus Participant 5–9-19).
“They explain it that they are not going to share their names but if not, they are just like, ok why do you want to know so much about me? Are you going to implicate me?” (Latino participant – 5–9-19).
Cancer-related genetic counseling and testing communication must be culturally tailored
Culturally centered communication was a cross-cutting theme across all focus group discussions. Latino group discussions included specific suggestions for how messages should be created, should be inclusive of culture, and disseminated. Participants believed risk messages about cancer-related genetic counseling and testing would have a greater impact if they were central to everyday life and not cumbersome or an unnecessary inconvenience.
“It’s not just speaking Spanish, than to understand the culture. Others have to understand our culture, it’s not the same to speak Spanish, than to understand there’s like Columbians are different than Mexicans, are different than Venezuelans, we are not the same, we are really, really different.” (Latino participant, 5–9-19).
“I think they should have someone that is a real good speaker that can pinpoint everything and explain it to them because a lot of people are like this doctor stuff can be real.” (African American participant, 4–16-19).
Another participant from a Latino focus group mentioned the importance of a medical provider as the purveyor of this type of information.
“Come talk to my level, and tell me the right thing, don’t tell me with big words because I don’t understand them, and I think this is why people don’t get tested. I don’t want to be a guinea pig for nobody; I don’t care how much you pay me. So, educate first, educate people, the educated people are the ones that we don’t understand, tell me in my language what you are doing with my body or my blood, that’s my body, that’s my right.” (Latino participant – 5–9-19).
Discussion
This study aimed to explore an under-studied area regarding cancer-related genetic counseling and testing risk communication through a novel approach by focusing on minority and underserved populations with an undetermined risk for any type of cancer. The primary aim was to engage with members from the CAB to design a study to explore attitudes, perceptions, and beliefs toward cancer-related genetic counseling and testing risk communication among Latino and African American patient populations. Our findings highlight the need for increased awareness, knowledge, clear messaging, and transparency from the medical establishment that addresses cancer beliefs and prepares the participant on what cancer-related genetic counseling and testing may reveal.
This pilot sample was primarily composed of educated women who had never had (or been offered) genetic counseling or a germline DNA genetic test. We found that financial-related fears, i.e., loss in wages following a positive test or indicated increased risk associated with an inherited cancer syndrome, could negatively impact interest and counseling and testing completion. Although not an overarching theme, there were individuals in two focus groups who disclosed medical education backgrounds and knowledge during the focus group session and voiced concern about genetic testing and why there was hesitancy to test. Additional research should continue to fully understand how racial/ethnic minority patient populations understand, perceive, and view cancer risk in the context of cancer-related genetic counseling and testing, who is best positioned to provide this service and what barriers may be encountered.
Risk perceptions about cancer and perceptions about medical and research personnel who do or do not inform, communicate, and educate patients about cancer-related genetic counseling and testing have broad implications. Results from a brief survey administered prior to focus groups showed that most participants responded that their medical provider, if they had one, did not inform them of cancer-related genetic counseling/and or testing even where current or past family history was concerning. Some participants also expressed in focus group discussions that they felt the lack of provider communication about this type of testing only reinforced mistrust of medical personnel and underscored documented barriers that perpetuate poor genetic testing use among racial-ethnic minority populations (Underhill et al. 2016). Mistrust may create barriers to delivery of health care and health care services and indifference to perceived susceptibility, perceived benefits, and medical providers and research (Corbie-Smith et al. 2002). In addition, some African Americans and Latinos showed less interest in participating in genetic testing because of their faith and belief in God and their fear of stigmatization and discrimination (Suther and Kiros 2009). Mai and colleagues (Mai et al. 2014) found that in a large sample of non-Hispanic whites, 25 years and older (49.9%) compared to African Americans (32.9%) and Hispanics (20.6%) reported some knowledge of genetic testing to assess their risk of developing cancer (Pagán et al. 2009; Wideroff et al. 2003), but knowledge disparities still exist (Hann et al. 2017; Weise et al. 2021). Mistrust of the health care system providers and medical research in addition to psycho-social barriers, unawareness, lack of knowledge, access to health information (Pagán et al. 2009), and health literacy (Pagán et al. 2009; Singer et al. 2004; Peterson et al. 2018) also are documented contributors to poor cancer-related genetic testing (Pagán et al. 2009; Suther and Kiros 2009) and are consistent with our findings. Addressing these barriers could inform efficacious and evidence-based tailored health communication that resonates with individuals and incorporates individual risk perception from underserved communities.
The perception about disease (cancer) and how individuals may perceive cancer prevention and treatment and evaluate risk information for counseling and testing among racial/ethnic populations was central to our investigation. Gauging how individuals perceive cancer risk and how this type of risk is presented strategically in genetic counseling or testing information may address barriers. Important work in this space (White et al. 2012; Masters and Hooker 2013; Martina et al. 2022) highlights cultural contextualization as critical to addressing cancer screening, outreach, and intervention, but less attention has illuminated these cultural issues that impinge on barriers and facilitators related to genetic counseling or testing.
Risk communication solutions and strategies
Identification of individual-level barriers including distrust of medical personnel and the fear of cancer among racial/ethnic minorities in the context of cancer-related genetic testing bolsters message relevance. Inequitable communication about cancer risk and lack of culturally relevant approaches for promulgating genetic counseling and testing among these populations (Jones et al. 2016; McCarthy et al. 2016; Smith et al. 2016) (e.g., genetic counselor bias, mistrust for medical personnel, access to health care, education) (Halbert et al. 2005) contribute to utilization disparities among these populations. Here, the disconnect between health providers and patients and the limited number of trained and licensed genetic counselors are other areas to be explored.
This sample saw the benefit of genetic testing but also had reservations for reasons why medical personnel would want to offer testing to racial/ethnic minorities. Cancer-related genetic testing risk communication that is culturally inclusive (Peterson et al. 2018; Viswanath et al. 2012) and is tailored to address cultural beliefs among these populations has the potential to offer personalized medicine opportunities to combat cancer health disparities. Community engagement and work through community health workers also hold promise as a strategy to disseminate this type of information. Community health workers or community lay advisors are traditionally trusted within the communities that they serve and are trained to discuss multiple health issues with community members (Almeida et al. 2021; Community Health Workers: Part Of The Solution 2010; Gwede et al. 2013; San Miguel-Majors et al. 2020; Sharpe et al. 2018; Vadaparampil et al. 2021).
Participants also detailed specific message tailoring tactics to improve medical provider (e.g., counselor, doctor) interactions and suggested multiple ways to inform individuals about genetic counseling and testing opportunities. An index used in public health communication helped guide our understanding of how participants could perceive and evaluate a public health risk (Covelo 1991) in terms of cancer and how cancer-related counseling and testing would mitigate that risk. Latino focus group participants provided detailed suggestions for strategies that included family communication, increasing awareness through targeted communication efforts at school and community events, and adopting appropriate language (e.g., speaking and writing in Spanish) for testing information.
Lautenbach and colleagues outline multiple evidence-based strategies to communicate genetic risk information for common medical disorders (Lautenbach et al. 2013). Presenting information in a variety of formats, avoiding framing bias (positive/gain vs. negative/loss), usage of graphics, accounting for cultural beliefs, past experiences and perceived risk, and engaging patients through risk assessment tools are all documented ways to communicate genetic risk information (Lautenbach et al. 2013). More recently, an emphasis is on addressing the influx of genetic information and broad dissemination through multiple channels that include the mass media and advertising (Patch and Middleton 2018). The changing landscape and evolving nature of testing calls for strategies that are responsive to multiple populations.
Ethical considerations and limitations
There were ethical considerations as well as limitations to the study. Ethical considerations originating from the target communities arose as perceptions about this type of research and testing (genetic) were beneficial to researchers and clinicians, and not patients. African Americans and female participants in the present study voiced outrage that there were cancer prevention tools available but had no awareness of counseling or testing before or during their cancer experience. While these perceptions are like those reported in the literature (Adams et al. 2015; Jones et al. 2016), there are unique points to this study. A small percentage of participants were from a single family and members of community organizations; some family members may have felt pressured to conform to more dominant individuals of the family. Moderators were diligent in including all participants throughout the focus group sessions as some participants were hesitant to speak during parts of the discussion. One African American focus group session (April 6, 2019) was not recorded, and subsequently, data was not transcribed for final analysis. However, the moderator and research assistant were able to use field notes for the coding process. Data from this and most focus group discussions included an overwhelming theme of disenfranchisement, mistrust and distrust of medical doctors, and the lack of transparency among researchers and medical professionals. In addition, the sample was mostly female, especially among the African American focus group discussions; had health insurance; and had completed high school or a GED. A few of these factors may have led to the consensus of mistrust and distrust and how women may perceive cancer throughout the continuum (Molina et al. 2015; Mouslim et al. 2020). Additionally, those who are underinsured or uninsured and have less education may have different perspectives and experiences not represented in the study sample. These additional perspectives may be more representative in Latino populations who are under-represented and uninsured in the nation. Finally, among the Latino-focus groups, the discussions were conducted exclusively in English because of budget limitations to translate research materials and transcripts. Recruitment of English-speaking and bilingual Latino participants may have contributed to a sample of higher educated, higher-income, insured Latino participants. Therefore, results do not reflect additional barriers that many Spanish-speaking Latinos may face (e.g., language, lower access to care, lower literacy level).
To address gaps in knowledge about this type of genetic susceptibility testing and counseling, the research staff and CAB offered free informational sessions following focus group sessions. The team wanted to provide participants and family members of focus groups an opportunity to ask additional questions and access to complementary genetic counseling and testing with genetic counselors on the research team. The study team also disseminated results of findings within established community-based networks to identify ways to improve awareness, knowledge, and information dissemination to decrease genetic testing disparities within these populations.
Conclusion
To our knowledge, this is one of the first studies to apply a community-engaged approach to inform the development of a risk communication model designed to strengthen genetic counseling and testing efforts among racial/ethnic minority populations. This study added to the growing body of precision cancer health equity literature that focuses on awareness and knowledge of cancer-related genetic counseling and testing among racial/ethnic minorities. Improved access to germline DNA testing may detect inheritable cancer syndromes; however, these populations have limited access to testing due to multiple barriers including physician recommendation, limited awareness and knowledge, and perceptions hindering equity in precision cancer prevention. Results from this study, which assembled a cohort of African Americans and Latinos from a city in the Midwest, are representative of gaps in cancer communication nationally and point to a need for additional targeted communication for these racial/ethnic minority populations. Our findings demonstrate that there are essential factors that must be included as part of cancer risk communication. Communicating effectively about cancer risks requires interdisciplinary best practice and input from engagement with a diversity of cultures and patients. Furthermore, this study demonstrates that communications about cancer risk require greater exploration by individuals focused on clinical benefits and utility for racial/ethnic minority populations. The results from our study support and advance previous literature that demonstrates racial/ethnic minority groups are often disproportionately impacted by limited access and/or awareness of cancer-related counseling and testing (Smith, Fullerton, Dookeran, Hampel, Tin, Maruthur, Schisler, et al., 2016). Additional research that engages the community will continue to inform clinical health communication strategies that are relevant and appeal to underserved and diverse populations and increase the reach of public health communication and emerging precision public health efforts. In an effort to help bridge study participants and their families to counseling and testing, two 90-min informational sessions were held at a centrally located Latino community center and cancer support center near predominately African American neighborhoods in mid-town Kansas City in July and August of 2019. Co-authors were also part of creating the Center for Genetic Services and Health Equity the following year in 2021 that facilitated access to racial/ethnic minorities and under-insured individuals in the urban core of the Kansas City Metropolitan area.
Exploring existing attitudes, perceptions, and beliefs toward cancer-related genetic counseling and testing risk communication among minority and underserved patient populations was the focus of this exploratory study. Based on our previous study of African American faith populations (Lumpkins et al. 2020) and our current community-engagement work with Latinos and African American populations who did not self-identify as from faith communities, we may better define beliefs (and access) and identify specific attitudes and risk perceptions toward cancer and cancer-related genetic counseling and testing among racial/ethnic populations. We also have some understanding for how this type of risk communication may be tailored and disseminated to individuals, groups, and on societal levels. This study will serve as a building block to bolster risk communication strategies that address cancer health inequities, communication inequities, and improvement in genetic testing.
Lessons learned here are both relevant for public health communication research and programmatic health promotion. The community networks were not only important for recruitment of individuals into the study but also for dissemination of information following data collection. These networks may also serve as communication infrastructure that will help build trusted networks of information and knowledge among these populations. Programmatically, public health communication programs that are inclusive of community members where their opinions and input are integrated have implications for bolstering evidence-based practice. Lessons may also be gained from current public health testing issues. Improved messaging regarding the importance and availability of SARS-CoV-2 testing among racial/ethnic populations may also be applied here as we see novel testing technologies unveiled and rapidly disseminated to reach the masses (Khoury and Holt 2021). However, existing beliefs, distrust, and false information have kept many racial/ethnic populations test averse and vaccine hesitant. Culturally inclusive strategies and counseling and testing risk communication that is inclusive of and sensitive to cultural factors have the potential to offer personalized medicine opportunities to combat barriers and cancer health disparities.
Data Availability
The authors confirm that the data supporting the findings of this study are available within the article [and/or] its supplementary materials. Will Share upon Request.
References
ACS (2019) Cancer facts and figures for African Americans 2019–2021. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/cancer-facts-and-figures-for-african-americans/cancer-facts-and-figures-for-african-americans-2019-2021.pdf
Adams I, Christopher J, Williams KP, Sheppard VB (2015) What black women know and want to know about counseling and testing for BRCA1/2. J Cancer Educ 30(2):344–352. https://doi.org/10.1007/s13187-014-0740-9
Ajzen I (1991) The theory of planned behavior. Organ Behav Hum Decis Process 50(2):179–211. https://doi.org/10.1016/0749-5978(91)90020-T
Alcaraz KI, Wiedt TL, Daniels EC, Yabroff KR, Guerra CE, Wender RC (2020) Understanding and addressing social determinants to advance cancer health equity in the United States: a blueprint for practice, research, and policy. CA: A Cancer J Clin 70(1):31–46. https://doi.org/10.3322/caac.21586
Almeida R, Lopez-Macha A, Dugatkin T, Joseph G, Duron Y, Hurtado de Mendoza A, Graves KD, Fejerman, L (2021) Community research collaboration to develop a promotores-based hereditary breast cancer education program for Spanish-speaking Latinas. Health Educ Res 36(3):319–336. https://doi.org/10.1093/her/cyab011
Butler EN, Umar A, Heckman-Stoddard BM, Kundrod KA, Signorello LB, Castle PE (2022) Redefining precision cancer prevention to promote health equity. Trends in Cancer 8(4):295–302. https://doi.org/10.1016/j.trecan.2022.01.009
Canedo JR, Miller ST, Myers HF, Sanderson M (2019) Racial and ethnic differences in knowledge and attitudes about genetic testing in the US: systematic review. J Genet Couns 28(3):587–601. https://doi.org/10.1002/jgc4.1078
Carroll NM, Blum-Barnett E, Madrid SD, Jonas C, Janes K, Alvarado M, Bedoy R, Paolino V, Aziz N, McGlynn EA, Burnett-Hartman AN (2020) Demographic differences in the utilization of clinical and direct-to-consumer genetic testing. J Genet Couns 29(4):634–643. https://doi.org/10.1002/jgc4.1193
Chavez-Yenter D, Chou WS, Kaphingst KA (2020) State of recent literature on communication about cancer genetic testing among Latinx populations. J Genet Couns. https://doi.org/10.1002/jgc4.1351
Community Health Workers: Part Of The Solution (2010) Health Affairs, 29(7), 1338-1342. https://doi.org/10.1377/hlthaff.2010.0081
Corbie-Smith G, Thomas SB, St George DM (2002) Distrust, race, and research. Arch Intern Med 162(21):2458–2463. https://doi.org/10.1001/archinte.162.21.2458
Covelo VT (1991) Risk Communication: an Emerging Area of Health Communication Research. Annals Int Commun Assoc 15(1):359–373
Denzin NK, Lincoln YS (2011) The SAGE handbook of qualitative research. Fourth edition. Thousand Oaks: SAGE, [2011] ©2011. https://search.library.wisc.edu/catalog/9910109320302121
DeSantis CE, Ma J, Gaudet MM, Newman LA, Miller KD, Goding Sauer A, Jemal A, Siegel RL (2019) Breast cancer statistics. CA: A Cancer J Clin 69(6):438–451. https://doi.org/10.3322/caac.21583
Dettenborn L, Duhamel K, Butts G, Thompson H, Jandorf L (2004) Cancer fatalism and its demographic correlates among African American and Hispanic women. J Psychosoc Oncol 22(4):47–60. https://doi.org/10.1300/J077v22n04_03
Domecq JP, Prutsky G, Elraiyah T, Wang Z, Nabhan M, Shippee N, Brito JP, Boehmer K, Hasan R, Firwana B, Erwin P, Eton D, Sloan J, Montori V, Asi N, Abu Dabrh AM, Murad MH (2014) Patient engagement in research: a systematic review. BMC Health Services Research 14(1):89. https://doi.org/10.1186/1472-6963-14-89
Gwede CK, Ashley AA, McGinnis K, Montiel-Ishino FA, Standifer M, Baldwin J, Williams C, Sneed KB, Wathington D, Dash-Pitts L, Green BL (2013) Designing a community-based lay health advisor training curriculum to address cancer health disparities. Health Promot Pract 14(3):415–424. https://doi.org/10.1177/1524839912458675
Halbert CH, Kessler LJ, Mitchell E (2005) Genetic testing for inherited breast cancer risk in African Americans. Cancer Invest 23(4):285–295. https://doi.org/10.1081/cnv-58819
Hann KEJ, Freeman M, Fraser L, Waller J, Sanderson SC, Rahman B, Side L, Gessler S, Lanceley A, team, P. s. (2017) Awareness, knowledge, perceptions, and attitudes towards genetic testing for cancer risk among ethnic minority groups: a systematic review. BMC Public Health 17(1):503–503. https://doi.org/10.1186/s12889-017-4375-8
Harrison JD, Auerbach AD, Anderson W, Fagan M, Carnie M, Hanson C, Banta J, Symczak G, Robinson E, Schnipper J, Wong C, Weiss R (2019) Patient stakeholder engagement in research: A narrative review to describe foundational principles and best practice activities. Health Expect 22(3):307–316. https://doi.org/10.1111/hex.12873
Jatoi I, Sung H, Jemal A (2022) The emergence of the racial disparity in U.S. breast-cancer mortalitY. New England J Med 386(25):2349–2352. https://doi.org/10.1056/NEJMp2200244
Jones T, Lockhart JS, Mendelsohn-Victor KE, Duquette D, Northouse LL, Duffy SA, Donley R, Merajver SD, Milliron KJ, Roberts JS, Katapodi MC (2016) Use of cancer genetics services in African American young breast cancer survivors. Am J Prev Med 51(4):427–436. https://doi.org/10.1016/j.amepre.2016.03.016
Khoury MJ, Holt KE (2021) The impact of genomics on precision public health: beyond the pandemic. Genome Medicine 13(1):67–67. https://doi.org/10.1186/s13073-021-00886-y
Kinney AY, Gammon A, Coxworth J, Simonsen SE, Arce-Laretta M (2010) Exploring attitudes, beliefs, and communication preferences of Latino community members regarding BRCA1/2 mutation testing and preventive strategies. Genet Med 12(2):105–115. https://doi.org/10.1097/GIM.0b013e3181c9af2d
Komenaka IK, Nodora JN, Madlensky L, Winton LM, Heberer MA, Schwab RB, Weitzel JN, Martinez ME (2016) Participation of low-income women in genetic cancer risk assessment and BRCA 1/2 testing: the experience of a safety-net institution. J Community Genet 7(3):177–183. https://doi.org/10.1007/s12687-015-0257-x
Kreuter MW, Lukwago SN, Bucholtz RD, Clark EM, Sanders-Thompson V (2003) Achieving cultural appropriateness in health promotion programs: targeted and tailored approaches. Health Educ Behav 30(2):133–146. https://doi.org/10.1177/1090198102251021
Lautenbach DM, Christensen KD, Sparks JA, Green RC (2013) Communicating genetic risk information for common disorders in the era of genomic medicine. Annu Rev Genomics Hum Genet 14:491–513. https://doi.org/10.1146/annurev-genom-092010-110722
Lumpkins CY, Philp A, Nelson KL, Miller LM, Greiner KA (2020) A road map for the future: an exploration of attitudes, perceptions, and beliefs among African Americans to tailor health promotion of cancer-related genetic counseling and testing. J Genet Couns 29(4):518–529. https://doi.org/10.1002/jgc4.1277
Lynce F, Graves KD, Jandorf L, Ricker C, Castro E, Moreno L, Augusto B, Fejerman L, Vadaparampil ST (2016) Genomic disparities in breast cancer among Latinas. Cancer Control 23(4):359–372. https://doi.org/10.1177/107327481602300407
Mai PL, Vadaparampil ST, Breen N, McNeel TS, Wideroff L, Graubard BI (2014) Awareness of cancer susceptibility genetic testing: the 2000, 2005, and 2010 National Health Interview Surveys. Am J Prev Med 46(5):440–448. https://doi.org/10.1016/j.amepre.2014.01.002
Martina D, Kustanti CY, Dewantari R, Sutandyo N, Putranto R, Shatri H, Effendy C, van der Heide A, Rietjens JAC, van der Rijt C (2022) Opportunities and challenges for advance care planning in strongly religious family-centric societies: a Focus group study of Indonesian cancer-care professionals. BMC Palliat Care 21(1):110. https://doi.org/10.1186/s12904-022-01002-6
Masters KS, Hooker SA (2013) Religiousness/spirituality, cardiovascular disease, and cancer: cultural integration for health research and intervention. American Psychological Association. https://doi.org/10.1037/a0030813
McCarthy AM, Bristol M, Domchek SM, Groeneveld PW, Kim Y, Motanya UN, Shea JA, Armstrong K (2016) Health care segregation, physician recommendation, and racial disparities in BRCA1/2 testing among women with breast cancer. J Clin Oncol 34(22):2610–2618. https://doi.org/10.1200/jco.2015.66.0019
McQueen A, Kreuter MW, Kalesan B, Alcaraz KI (2011) Understanding narrative effects: The impact of breast cancer survivor stories on message processing, attitudes, and beliefs among African American women. Health Psychol 30(6):674–682. https://doi.org/10.1037/a0025395
Molina Y, Kim S, Berrios N, Calhoun EA (2015) Medical mistrust and patient satisfaction with mammography: the mediating effects of perceived self-efficacy among navigated African American women. Health Expectations 18(6):2941–2950. https://doi.org/10.1111/hex.12278
Mouslim MC, Johnson RM, Dean LT (2020) Healthcare system distrust and the breast cancer continuum of care. Breast Cancer Res Treat 180(1):33–44. https://doi.org/10.1007/s10549-020-05538-0
NCI, NCI (2021) Cancer stat facts: cancer disparities Retrieved 05/11/2021 from https://seer.cancer.gov/statfacts/html/disparities.html
Olaya W, Esquivel P, Wong JH, Morgan JW, Freeberg A, Roy-Chowdhury S, Lum SS (2009) Disparities in BRCA testing: when insurance coverage is not a barrier. Am J Surg 198(4):562–565. https://doi.org/10.1016/j.amjsurg.2009.07.003
Pagán JA, Su D, Li L, Armstrong K, Asch DA (2009) Racial and ethnic disparities in awareness of genetic testing for cancer risk. Am J Prev Med 37(6):524–530. https://doi.org/10.1016/j.amepre.2009.07.021
Parrott RL, Worthington AK, Smith RA, Chadwick AE (2015) Communicating about genes, health and risk. Oxford Research Encyclopedia of Communication. https://doi.org/10.1093/acrefore/9780190228613.013.8
Patch C, Middleton A (2018) Genetic counselling in the era of genomic medicine. Br Med Bull 126(1):27–36. https://doi.org/10.1093/bmb/ldy008
Peterson EB, Chou WS, Gaysynsky A, Krakow M, Elrick A, Khoury MJ, Kaphingst KA (2018) Communication of cancer-related genetic and genomic information: a landscape analysis of reviews. Transl Behav Med 8(1):59–70. https://doi.org/10.1093/tbm/ibx063
Powe BD, Finnie R (2003) Cancer fatalism: the state of the science. Cancer Nursing, 26(6), 454–467. https://journals.lww.com/cancernursingonline/Fulltext/2003/12000/Cancer_Fatalism__The_State_of_the_Science.5.aspx
Price E, Robbins SJ, Valverde K (2020) Increasing diversity in the genetic counseling profession: development of recruitment tools for African American undergraduate students. J Genet Couns 29(2):224–233. https://doi.org/10.1002/jgc4.1280
Ricker C, Lagos V, Feldman N, Hiyama S, Fuentes S, Kumar V, Gonzalez K, Palomares M, Blazer K, Lowstuter K, MacDonald D, Weitzel J (2006) If we build it … will they come?–establishing a cancer genetics services clinic for an underserved predominantly Latina cohort. J Genet Couns 15(6):505–514. https://doi.org/10.1007/s10897-006-9052-5
Ricker CN, Koff RB, Qu C, Culver J, Sturgeon D, Kingham KE, Lowstuter K, Chun NM, Rowe-Teeter C, Lebensohn A, Levonian P, Partynski K, Lara-Otero K, Hong C, Petrovchich IM, Mills MA, Hartman AR, Allen B, Ladabaum U, . . . Idos GE (2018) Patient communication of cancer genetic test results in a diverse population. Transl Behav Med, 8(1), 85-94. https://doi.org/10.1093/tbm/ibx010
Roche J, Bell L, Galvão C, Golumbic YN, Kloetzer L, Knoben N, Laakso M, Lorke J, Mannion G, Massetti L, Mauchline A, Pata K, Ruck A, Taraba P, Winter S (2020) Citizen science, education, and learning: challenges and opportunities [Conceptual Analysis]. Front Sociol 5. https://doi.org/10.3389/fsoc.2020.613814
San Miguel-Majors SL, Whitaker DE, Davis BC, Bailey LO, Springfield SA (2020) Education on cancer risk assessment and genetic counseling to address cancer health disparities among racial/ethnic groups and rural populations: implementing culturally tailored outreach through community health educators. J Genet Couns 29(2):243–246. https://doi.org/10.1002/jgc4.1272
Senier L, McBride CM, Ramsey AT, Bonham VL, Chambers DA (2019) Blending insights from implementation science and the social sciences to mitigate inequities in screening for hereditary cancer syndromes. Int J Environ Res Public Health, 16(20). https://doi.org/10.3390/ijerph16203899
Sharpe PA, Wilcox S, Kinnard D, Condrasky MD (2018) Community health advisors’ participation in a dissemination and implementation study of an evidence-based physical activity and healthy eating program in a faith-based setting. J Community Health 43(4):694–704. https://doi.org/10.1007/s10900-018-0473-5
Singer E, Antonucci T, Van Hoewyk J (2004) Racial and ethnic variations in knowledge and attitudes about genetic testing. Genet Test 8(1):31–43. https://doi.org/10.1089/109065704323016012
Smith CE, Fullerton SM, Dookeran KA, Hampel H, Tin A, Maruthur NM, Schisler JC, Henderson JA, Tucker KL, Ordovás JM (2016) Using genetic technologies to reduce, rather than widen health disparities. Health Aff (Millwood) 35(8):1367–1373. https://doi.org/10.1377/hlthaff.2015.1476
Story L, Hinton A, Wyatt SB (2010) The role of community health advisors in community-based participatory research. Nurs Ethics 17(1):117–126. https://doi.org/10.1177/0969733009350261
Suther S, Kiros GE (2009) Barriers to the use of genetic testing: a study of racial and ethnic disparities. Genet Med 11(9):655–662. https://doi.org/10.1097/GIM.0b013e3181ab22aa
Timmermans S (2020) The engaged patient: the relevance of patient–physician communication for twenty-first-century health. J Health Soc Behav 61(3):259–273. https://doi.org/10.1177/0022146520943514
Underhill MLPRNA, Jones TPRNA, Habin KMSNRNCNS (2016) Disparities in cancer genetic risk assessment and testing. Oncol Nurs Forum 43(4):519–523. https://doi.org/10.1188/16.ONF.519-523
Vadaparampil ST, Moreno Botero L, Fuzzell L, Garcia J, Jandorf L, Hurtado-de-Mendoza A, Campos-Galvan C, Peshkin BN, Schwartz MD, Lopez K, Ricker C, Fiallos K, Quinn GP, Graves KD (2021) Development and pilot testing of a training for bilingual community education professionals about hereditary breast and ovarian cancer among Latinas: ÁRBOLES Familiares. Trans Behav Med, 12(1). https://doi.org/10.1093/tbm/ibab093
Viswanath K, Nagler RH, Bigman-Galimore CA, McCauley MP, Jung M, Ramanadhan S (2012) The Communications Revolution and Health Inequalities in the 21st Century: implications for cancer control. Cancer Epidemiol Biomark Prev 21(10):1701–1708. https://doi.org/10.1158/1055-9965.Epi-12-0852
Weise N, Shaya J, Javier-Desloges J, Cheng HH, Madlensky L, McKay RR (2021) Disparities in germline testing among racial minorities with prostate cancer. Prostate Cancer Prostatic Dis. https://doi.org/10.1038/s41391-021-00469-3
White K, Garces IC, Bandura L, McGuire AA, Scarinci IC (2012) Design and evaluation of a theory-based, culturally relevant outreach model for breast and cervical cancer screening for Latina immigrants. Ethn Dis 22(3):274–280
Wideroff L, Vadaparampil ST, Breen N, Croyle RT, Freedman AN (2003) Awareness of genetic testing for increased cancer risk in the year 2000 National Health Interview Survey. Community Genet 6(3):147–156. https://doi.org/10.1159/000078162
Acknowledgements
The authors would like to acknowledge the support of the Sean D. Biggs Memorial Foundation, Frontiers Clinical and Translational Science Institute, and the Kansas Institute for Precision Medicine. We thank all our community partner organizations and the focus group participants.
Funding
This work was supported in part by a grant from the Frontiers Institute (UL1TR002366) and the NIGMS (P20 GM130423).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lumpkins, C.Y., Nelson, R., Twizele, Z. et al. Communicating risk and the landscape of cancer prevention — an exploratory study that examines perceptions of cancer-related genetic counseling and testing among African Americans and Latinos in the Midwest. J Community Genet 14, 121–133 (2023). https://doi.org/10.1007/s12687-022-00629-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12687-022-00629-5