Abstract
Patients with non-small cell lung cancer (NSCLC) in the postoperative recovery period often experience reduced exercise capacity and impaired lung function, which affects their overall quality of life. This paper investigated the effect of exercise interventions on exercise capacity, lung function, quality of life, and symptoms in these patients. Methods: We performed a literature search across Cochrane, Embase, PubMed, Web of Science, and EBSCO databases were comprehensively searched for randomized controlled trials (RCTs) from inception to September 2023, all English RCTs were eligible if they assessed the effects of exercise interventions on postoperative NSCLC patients. Results: Twelve articles met our inclusion criteria, evidencing that exercise interventions could significantly improve the functional capacity of NSCLC patients in postoperative recovery. Notably, Forced Expiratory Volume in 1 s (FEV1) was improved, indicating enhanced lung function. Furthermore, exercise improved the physical and mental health scores of SF-36, along with increased quadriceps strength and relieved dyspnea. However, fatigue levels were not significantly changed. Conclusions: Exercise interventions of NSCLC patients in the postoperative recovery are associated with improved functional capacity, lung function, quality of life, and quadriceps strength, as well as alleviated symptoms of dyspnea. These findings underscore the potential benefits of incorporating exercise into postoperative care for NSCLC patients. Nonetheless, further large-scale RCTs are required to solidify the evidence base on the clinical outcomes of exercise following pneumonectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Lung cancer is the foremost cause of mortality among malignant neoplasms, with the highest incidence and prevalence [1]. According to global cancer statistics from 185 nations, lung cancer is the second most prevalent malignancy, accounting for 11.4% of all reported cases. According to the latest data (2020), lung cancer stands out as the most frequent cancer for males and the third most prevalent for females. Moreover, its mortality is significantly high, contributing to 18.0% of all cancer-related deaths [2]. Among various histological subtypes of lung cancer, non-small cell lung carcinoma (NSCLC) represents the predominant subtype with an incidence of approximately 85% to 90% [3].
Surgery is primarily to prolong the survival of lung cancer patients. Long-term survival outcomes and potential disability risks of surgery are increasingly significant for lung cancer patients [4]. Complete surgical resection remains the most effective option for stage I and II lung cancer [5]. However, systemic inflammation, impaired physical condition, inadequate nutritional status, and surgical stress contribute to postoperative functional decline, which is a crucial predictor of morbidity and mortality after pneumonectomy [6,7,8]. A longitudinal study conducted by Handy et al. showed a significant decline in quality of life (QOL) in 139 patients within six months after pneumonectomy [9]. Furthermore, dyspnea is strongly correlated with reduced QOL five years after surgery [10]. Additionally, dyspnea may result in decreased physical activity [11], which in turn affects skeletal muscle and cardiovascular function [12, 13], ultimately hindering the exercise capacity of lung cancer patients. Additionally, lung cancer patients may experience weight loss, loss of appetite, anemia, protein catabolism, and muscle atrophy [14, 15]. These factors all negatively impact exercise capacity. Furthermore, adjuvant treatments like chemotherapy may trigger exercise intolerance due to alterations in substrate transportation and utilization in the body [16]. Therefore, it is imperative to improve exercise capacity and QOL and alleviate associated symptoms in postoperative NSCLC patients.
Numerous studies have highlighted the importance of exercise in maintaining overall health. Specifically, both exercise training [4] and respiratory training [17] have positive effects on postoperative recovery of NSCLC patients. However, there is no consensus on the impact of exercise on postoperative outcomes in NSCLC patients [4, 18]. Granger conducted a meta-analysis in 2011 to examine the effect of exercise on NSCLC patients and unraveled that exercise capacity was improved, but QOL was not immediately improved [19]. Most studies included were case series (n = 9), with only two RCTs, potentially introducing bias and limiting the reliability and generalizability of findings. In contrast, Cavalieri (2019) conducted a meta-analysis on postoperative NSCLC patients and evinced that exercise improved both exercise capacity and QOL [20]. Nevertheless, the original studies included in Cavalheri’s meta-analysis were outdated and inadequate, casting doubt on their suitability for analyzing pooled results [20]. Specifically, some outcome measures reported final values after exercise rather than within-group differences (changes from baseline to post-intervention), which reduced the credibility of the combined results and increased the likelihood of bias. Moreover, this analysis did not distinguish between different types of exercise, thereby constraining our comprehension of how specific exercise affect postoperative recovery in NSCLC patients and hindering the development of personalized exercise programs for clinical application. Given the large number of recent research on the effects of exercise on postoperative NSCLC patients, a thorough review of the latest studies is crucial to elucidate the benefits of exercise for this population.
This meta-analysis of current data was to elucidate the impact of exercise on postoperative NSCLC patients. Different from recent studies, this innovative research incorporated the most up-to-date studies from the past five years and analyzed baseline and post-intervention changes. Additionally, subgroup analyses were implemented to assess exercise capacity and QOL. Given that lung function, exercise capacity, QOL, and cancer-related symptoms are crucial influencing factors for postoperative recovery in NSCLC patients [21] and that data on other factors are limited, this meta-analysis was to comprehensively summarize the effects of exercise on lung function, exercise capacity, QOL, and cancer-related symptoms in postoperative NSCLC patients.
2 Materials and methods
This meta-analysis followed the PRISMA guidelines [22], and the systematic review has also been registered on PROSPERO (CRD42023488002).
2.1 Data sources and searches
Relevant studies were comprehensively searched on PubMed, Cochrane, Embase, Web of Science, and EBSCO databases. The search strategy utilized MeSH terms in PubMed/Cochrane and Emtree terms in Embase.
Appendix S2 gives details of the search strategy for each database.
The search strategy was based on the PICOS: (P) Population: NSCLC patients; (I) Intervention: exercise; (C) Controls: usual care, or no exercise training, or only general exercise instructions; (O) Outcome: postoperative recovery: pulmonary function, exercise capacity, QOL, muscle strength, dyspnea, and fatigue; (5) Study type: RCT. In addition, we searched the reference lists of selected articles to identify any relevant studies that might have been missed by the electronic search. All English RCTs published from database inception to September 2023 were included.
2.2 Study selection
The literature was screened by two independent researchers based on predefined inclusion and exclusion criteria using a double-blind approach. Initially, articles were selected by reviewing the title and abstract, followed by full-text reading to determine the inclusion. Any disagreement was addressed by a third author who made the final decision. Eligible studies met the following criteria: (1) RCTs, (2) participants aged ≥ 18 years undergoing pneumonectomy, (3) control groups receiving usual or standard care without exercise training or with only general exercise instruction, (4) interventions involving aerobic training, resistance training, strength training, or respiratory exercises combined with other exercises, (5) comparison of experimental groups receiving structured exercise training for at least four weeks, (6) assessment of changes in factors related to postoperative recovery before and after exercise, and (7) reporting of at least one outcome measure related to pulmonary function, exercise capacity, or QOL. Studies were excluded for duplicate publications, literature reviews, letters to the editor, conference abstracts, assessing acute effects of single bouts of exercise, animal studies, and lacking primary data or where attempts to contact authors proved unsuccessful.
2.3 Data extraction and quality assessment
All data were extracted and compiled independently by two researchers to ensure consistency. A third author was asked for help to make the final decision in case of disagreement. If relevant data were missing, we contacted the authors to obtain the original information. The extracted information encompassed lead author details, country of affiliation, year of publication, TNM cancer stage; baseline characteristics: age, sample size, and type of surgery (open thoracic or minimally invasive) in both experimental and control groups; exercise characteristics: type, frequency, duration, and intensity of intervention; and reported outcomes. The risk of bias was appraised using the Cochrane Bias risk tool [23] in seven aspects: (1) randomization generation, (2) concealment of allocation, (3) blinding of participants and personnel, (4) blinding of outcome assessment, (5) incomplete outcome data, (6) selective reporting bias, and (7) other bias.
2.4 Data synthesis and analysis
Odds ratios (ORs) with 95% confidence intervals (CI) were utilized as pooled estimates for dichotomous outcomes. Conversely, mean differences (MDs) accompanied by a 95% CI were computed for continuous outcomes. Due to similar units of measurement and statistical methods of most data, MDs and their 95% CI were adopted. However, for a small proportion of data with different units of measurement, standardized mean differences (SMDs) and 95% CI were calculated. Changes in the intervention group compared to the control group were also summarized to estimate the effect of each outcome. Heterogeneity across studies was judged using the I2 statistic and Cochran’s Q test. Significant heterogeneity was considered present when I2 > 50% or when the p-value from the Q test ≤ 0.10. Random-effects models were employed if significant heterogeneity was discovered; otherwise, fixed-effects models were used. Subgroup analyses were conducted to ascertain sources of significant heterogeneity while simultaneously examining the effects of different exercise modalities. Publication bias was discerned by funnel plots and Egger’s and Begg’s methods. Sensitivity analyses tested the robustness of pooled results by excluding each RCT. Quantitative syntheses of data were done using Review Manager software 5.3 or Stata software 17.
3 Results
3.1 Literature selection
The flowchart of selection process is presented in Fig. 1. 5470 potentially eligible articles were retrieved from which duplicates and reviews were removed, resulting in 3275 articles for screening. After evaluating titles and abstracts, 3181 articles were excluded, followed by the removal of 82 articles after reading their full texts. Ultimately, only 12 eligible articles were enrolled.
3.2 Description of the included RCTs
3.2.1 Participants
The characteristics of the included RCTs are summarized in Table 1. 413 cases in the experimental group and 407 cases in the control group were included. Ten RCTs included only postoperative NSCLC patients. Two RCTs included postoperative patients with NSCLC and small cell lung cancer (SCLC). Ten RCTs reported the surgical approach used, video-assisted thoracoscopic surgery (VATS) or open thoracic surgery. The mean age of the study participants ranged from 56 to 68 years, with the majority being middle-aged or older.
3.2.2 Interventions
A concise overview of exercise programs is presented in Table 1. Twelve studies implemented exercise interventions during the postoperative period, encompassing six articles using aerobic and resistance exercises, two articles using HIIT with resistance exercise, one article combining aerobic, HIIT, and resistance exercises, one article combining resistance and cardiovascular exercises, one article combining aerobic, resistance, and respiratory exercises, and one article solely on aerobic and respiratory exercises. The primary forms of aerobic exercise were cycling, walking, and treadmill activities. The main form of resistance training was the range of motion exercises for the trunk and limbs. Chest breathing techniques, abdominal breathing methods, or ventilator assistance, were primary forms of respiratory exercise. All interventions lasted at least four weeks. During this period, the frequency of each exercise intervention varied. The control group in each study received either standard care no, specific exercise training, or only general instructions regarding physical activity.
3.2.3 Outcome
The outcome measures are presented in Table 1. These studies primarily focused on pulmonary function [e.g., forced expiratory volume (FEV), forced expiratory volume in 1 s (FEV1)], exercise capacity [e.g., six-minute walk distance (6MWD), peak oxygen uptake (VO2peak)], QOL [the 36-item short form health survey (SF-36), the European organization for research and treatment of cancer (EORTC QLQ-C30)], muscle strength (e.g., quadriceps, grip strength), dyspnea, fatigue, postoperative complications, and length of hospitalization. Two studies examined the impact of exercise on forced vital capacity (FVC) and various aspects of functional status, symptoms, role functioning, cognitive functioning, social functioning, grip strength, handgrip strength, anxiety levels, depression levels, and oxygen saturation (SPO2) in postoperative lung cancer patients. Due to limited data available for FVC, postoperative complications, functional status, symptoms, role functioning, cognitive functioning, social functioning, anxiety levels, depression levels, and SPO2 from the EORTC QLQ-C30 questionnaire were not included in this analysis. Additionally, other outcome indicators such as the ratio of spirometry to airflow capacity (FEV1/FVC), diffusion function, and St George’s respiratory questionnaire (SGRQ) were studied but could not be analyzed due to insufficient data.
3.3 Methodological quality assessment
The results of Cochrane risk evaluation are presented in Fig. 2. Among the enrolled articles, twelve explicitly reported randomization methods and ten had concealed the allocation of groups. Given that all studies involved human subjects, blinding of participants and personnel was a challenge. However, informed consent forms were signed by participants, and exercise interventions were supervised by researchers. Consequently, all articles were deemed a high risk of bias. Seven articles described blinding for outcome analysis, but three were rated as high risk due to a significant loss of personnel during the intervention. Some papers clearly outlined how missing data were handled and the methods used, while five papers selectively reported outcomes. When reviewing the trial registers, it was found that not all prespecified results were reported in the published papers. In addition, some outcomes appeared in the papers but not in the registers, leading to three articles being rated as high risk due to baseline differences.
3.4 Synthesis of the results
3.4.1 Analysis of pulmonary function
Lung function was measured in six studies, with FEV1 and FEV analyzed. Among the five studies investigating FEV1, no great difference was noted between the intervention and control groups (MD = 0.20; 95% CI [− 0.10, 0.51]; P = 0.20; I2 = 94%) (Fig. 3). In three studies on FEV, there was also no marked difference (MD = 1.17; 95% CI [− 2.64, 4.97]; P = 0.55; I2 = 0%) (Fig. 4).
3.4.2 Analysis of 6MWD
The effect of exercise on 6MWD is summarized in Fig. 5. Nine studies with 6MWD as a measure of exercise capacity were included, including 455 participants. Due to substantial heterogeneity (I2 = 71%), a random-effects model was employed to estimate combined effects, and the analysis demonstrated substantial differences between the intervention and control groups (MD = 35.80; 95% CI [13.99, 57.62]; P = 0.001).
3.4.3 Analysis of VO2peak
Five studies reported VO2peak as an indicator of exercise capacity, with 255 participants providing data. Four of these studies utilized the statistical unit of mL/kg/min to measure VO2peak, while the remaining study used ml O2/min. Considering the different units, we employed SMD for data comparison and analysis. Due to substantial heterogeneity (I2 = 80%), random-effects models were applied for combined effects estimation. The results noted a significant disparity between the intervention and control groups (SMD = 1.05; 95% CI [0.35, 1.76]; P = 0.003) (Fig. 6). Sensitivity analyses were conducted to identify potential sources of heterogeneity.
3.4.4 Analysis of QOL
To comprehensively investigate the impact of postoperative exercise on QOL in patients undergoing pneumonectomy, we conducted a statistical analysis using SF-36 and EORTC QLQ-C30.
Six studies assessed QOL using the SF-36 questionnaire. The pooled results demonstrated a significantly improved physical domain score of SF-36 after postoperative exercise (MD = 3.10, 95% CI [1.28, 4.93]; P = 0.0008; I2 = 29%) (Appendix S3-1). However, substantial heterogeneity was noticed (I2 = 89%). Therefore, a random-effects model was employed for analysis (MD = 4.76, 95% CI [− 1.78, 11.30]; P = 0.15; I2 = 89%). Notably, no prominent differences were found between the two groups in the psychological domains of SF-36 (Appendix S3-2).
Postoperative exercise training was significantly correlated with improved physical function (MD = 7.91, 95% CI [0.84, 14.98]; P = 0.03; I2 = 76%) and role physical (MD = 7.73, 95% CI [2.91, 12.55]; P = 0.002; I2 = 37%) (Appendix S3-3).
Postoperative motor rehabilitation was significantly correlated with social functioning (MD = 6.80, 95% CI [3.63, 9.98]; P < 0.0001; I2 = 0%) and psychological well-being (MD = 9.47, 95% CI [7.54, 11.41]; P < 0.00001; I2 = 18%) within the four psychological domains (Appendix S3-4).
Six studies reported disease-specific health-related quality of life (HRQoL) using the EORTC QLQ-C30, while five studies reported global health component scores on the same questionnaire. No noticeable differences were found in global health component scores (MD = 1.39, 95% CI [− 2.53, 5.32]; P = 0.49; I2 = 0%). However, significant differences were observed in body composition across four studies (MD = 4.88, 95% CI [2.05, 7.72]; P = 0.0007; I2 = 0%). In contrast, no significant differences were found between in three studies investigating affective functioning (MD = 11.47, 95% CI [− 4.58, 27.53]; P = 0.16; I2 = 77%) (Appendix S3-5).
3.4.5 Analysis of quadriceps
Four studies reported the intervention's impact on quadriceps muscle, with 133 participants providing data. Substantial evidence indicated high heterogeneity (I2 = 78%). Consequently, a random-effects model was employed for analysis (MD = 18.85; 95% CI [1.36, 36.33]; P = 0.03) (Fig. 7). The findings demonstrated visible differences in quadriceps muscle, and sensitivity analysis was conducted to identify the source of heterogeneity.
3.4.6 Analysis of dyspnea
Three studies examined the impact of interventions on dyspnea, involving 192 participants. A remarkable difference was noted between the intervention and control groups (MD = − 6.58, 95% CI [− 12.04, 1.13]; P = 0.02) (Fig. 8). The low heterogeneity across these studies (I2 = 13%, P for heterogeneity = 0.32) suggests that exercise interventions may effectively alleviate dyspnea in postoperative NSCLC patients.
3.4.7 Analysis of fatigue
Five studies with participants reported the impact of the intervention on fatigue. Among these, three studies utilized the fatigue component score of the EORTC QLQ-C30, while the remaining two employed functional assessment of chronic illness therapy—fatigue (FACIT-Fatigue) for measuring fatigue levels. Higher scores on the EORTC QLQ-C30 indicate more severe fatigue, whereas lower scores on FACIT-Fatigue suggest greater fatigue severity. During data sorting and collection, we reversed the direction of the average change in FACIT-Fatigue scores (i.e., negative values were treated as positive). Due to different assessment methods, number of questions, and score ranges, SMD was calculated to analyze the data. The results obtained through fixed-effects model analysis unveiled no significant difference in fatigue (SMD = − 0.18; 95% CI [− 0.46, 0.11]; P = 0.22; I2 = 0%) (Fig. 9).
3.5 Subgroup analysis
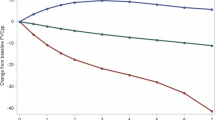
3.5.1 Subgroup analysis of FEV1
Regarding the impact on postoperative NSCLC patients, our previous analysis of the overall sample did not disclose any significant findings (p > 0.05) in FEV1 for lung function. However, subgroup analyses (Fig. 10) unveiled some intriguing results. Three studies (n = 225 patients) reported aerobic and resistance exercise, which demonstrated notable differences between the intervention and control groups (MD = 0.12; 95% CI [0.04, 0.21]; P = 0.006; I2 = 0%). One study (n = 90 patients) provided data on FEV1 for breathing exercises combined with other forms of exercise, showing marked differences (MD = 0.81; 95% CI [0.62, 1.00]; P < 0.00001). Additionally, one study (n = 90 patients) presented FEV1 measurements for HIIT, revealing significant differences (MD = − 0.10; 95% CI [− 0.20, 0.00]; P = 0.05).
3.5.2 Subgroup analysis of 6MWD
Figure 11 presents a summary of the impact of exercise on 6MWD. A random-effects model was employed for estimating combined effects, considering data from nine RCTs involving 455 participants. Overall, exercise demonstrated a noticeable increase in 6MWD levels (MD = 35.80; 95% CI [13.99, 57.62]; P = 0.004; I2 = 73%). Subgroup analyses yielded varying results. Six studies (n = 297 patients) reporting aerobic and resistance exercises manifested significant differences (MD = 33.24; 95% CI [6.09, 60.39]; P = 0.02; I2 = 64%). However, two studies (n = 144 patients) providing data on breathing and other exercises did not show any notable differences (MD = 36.92; 95% CI [− 23.11, 96.95]; P = 0.23; I2 = 92%). Additionally, one study (n = 14 patients) examining HIIT exhibited no marked difference (MD = 53.00; 95% CI [− 4.85, 110.85]; P = 0.07).
3.5.3 Subgroup analysis of physical domain
Figure 12 presents a summary of the impact of exercise on physical aspects of QOL, with random-effects models utilized for combined effects estimation. Six RCTs with 336 participants assessed the SF-36 physical domain. Overall, exercise visibly improved bodily domains (MD = 3.10; 95% CI [1.28, 4.93]; P = 0.00008; I2 = 29%). Subgroup analyses yielded consistent results. Four studies (n = 258 patients) reported physical domains combining aerobic and resistance exercise, and analyses demonstrated prominent differences (MD = 2.15; 95% CI [0.06, 4.24]; P = 0.04; I2 = 0%). Two studies (n = 78 patients) reported the physical domains of HIIT, and analysis proved substantial differences (MD = 6.13; 95% CI [2.41, 9.85]; P = 0.001; I2 = 29%).
3.5.4 Subgroup analysis of mental domain
Previous results from the overall sample analysis implied no statistical significance (P > 0.05) for the mental domain outcome metrics of the SF-36 questionnaire. However, noteworthy findings emerged after subgroup analyses on exercise interventions (Fig. 13). Four articles (n = 258 patients) reported notable differences in the mental domain outcomes for combined aerobic and resistance exercise (MD = 7.23; 95% CI [− 0.09, 14.55]; P = 0.05; I2 = 89%). Two articles (n = 78 patients) reported no notable difference in the mental domain outcomes for HIIT (MD = − 0.44; 95% CI [− 17.00, 16.12]; P = 0.96; I2 = 92%). To comprehensively explore the impact of postoperative exercise on QOL, we conducted a statistical analysis using SF-36 and EORTC QLQ-C30.
3.6 Sensitivity analysis
To evaluate the stability of the meta-analysis, a sensitivity analysis was conducted. After excluding the study by Messaggi-sartor 2019 [29], heterogeneity for VO2peak greatly decreased (I2 = 12%), indicating that this study contributed to the observed heterogeneity. However, there was no significant change in the adjusted combined estimate (SMD = 0.55; 95% CI [0.29, 0.82]; P < 0.0001). Similarly, the removal of Arbane's study led to a significant reduction in heterogeneity for SF-36 physical functional values (I2 = 24%) [25], but it did not result in any substantial changes in the adjusted combined estimates (MD = 4.84; 95% CI [0.02, 9.67]; P = 0.05). The elimination of Arbane's study [4] substantially reduced heterogeneity for quadriceps data (I2 = 0%), suggesting it was a major source of heterogeneity; however, there were no evident alterations in the adjusted combined estimates (MD = 27.98; 95% CI [16.09, 39.87]; P < 0.00001). These findings indicated that the results obtained from this meta-analysis were relatively robust.
Sensitivity analyses were done for FEV1, 6MWD, physical domain, and psychological domain. Upon exclusion of each study, the sensitivity analyses demonstrated robustness and stability in the overall findings (Appendix S4).
3.7 Evolution of publication bias
The funnel plot showed no significant evidence of asymmetric distribution for FEV1, 6MWD, physical domain, and psychological domain. Begg's and Egger's tests indicated no significant publication bias in FEV1 (Pr >|z|= 0.624 > 0.05) (t = 1.11, P = 0.349), 6MWD (Pr >|z|= 0.404 > 0.05) (t = 0.39, P = 0.706), physical domain (Pr >|z|= 0.188 > 0.05) (t = -0.30, P = 0.782), and psychological domain (Pr >|z|= 0.573 > 0.05) (t = 0.74, P = 0.502) (Appendix S5).
4 Discussion
This systematic review presents a comprehensive synthesis of recent RCTs, employing meta-analysis to examine the impact of exercise on postoperative recovery in NSCLC patients. The findings substantiate that exercise interventions offer numerous advantages for postoperative NSCLC patients, including improved FEV1, enhanced exercise capacity, better QOL across specific domains, improved quadriceps function, and alleviated dyspnea. However, no significant effects were observed on fatigue.
Many systematic reviews and meta-analyses have shown that exercise interventions can significantly improve cardiopulmonary function and reduce the risk of respiratory diseases such as upper respiratory tract infections and pneumonia [33]. However, these recent meta-analyses presented somewhat negative results when assessing the effects of exercise on the psychological domains of pulmonary function and QOL in NSCLC patients after surgery [34, 35]. However, through the inclusion of new literature and in-depth subgroup analysis, we observed encouraging findings. The combination of aerobic and resistance exercise demonstrated significant positive effects on the psychological dimensions of lung function and QOL in this population. Notably, the recovery of lung function and the improvement of QOL are both important factors for clinical outcomes in lung cancer patients [36]. It has been found that postoperative lung cancer patients may have damaged lung tissues and decreased lung function, which increases the risk of respiratory infections in patients [37]. Therefore, good lung function recovery is important for improving the QOL and prolonging the survival of lung cancer patients. Numerous studies have been conducted on the effects of exercise on postoperative recovery in NSCLC patients [4, 18, 32, 38], but the results vary widely. In this study, we summarized the recently published studies and found that long-term exercise can improve the postoperative recovery (lung function, exercise capacity, and QOL) of NSCLC patients and alleviate dyspnea to a certain extent.
We explored lung function, exercise capacity, QOL, and cancer-related symptoms. Because evidence suggests that FEV1, VO2peak, and QOL are directly or indirectly associated with survival in NSCLC patients [36, 39, 40]. Reduced FEV1 may diminish the lung's ability to remove air, leading to decreased gas exchange efficiency, predisposing to hypoxemia and hypercapnia, and increasing the risk of postoperative complications [37]. Reduced VO2peak decreases the ability of the cardiopulmonary system to deliver oxygen to the tissues, affecting the oxygen supply to tissues throughout the body [41]. Pneumonectomy may lead to poorer physical, social, and psychological well-being [9, 10]. Therefore, there is a need to improve the abnormally lowered FEV1, VO2peak, and QOL in postoperative NSCLC patients. Our study evinced that exercise significantly elevated FEV1, VO2peak, and QOL in postoperative NSCLC patients, thereby effectively improving postoperative recovery status and the utilization of oxygen by FEV1 and VO2peak. Improvement of postoperative recovery status can effectively prevent NSCLC patients from developing complications or prevent the aggravation of existing complications, and accelerate the recovery process to a certain extent.
According to our analysis, no overall improvement was revealed in lung function indices (FEV1, FEV) after exercise training. However, subgroup analyses by different types of exercise evinced noteworthy findings. Three studies combining aerobic and resistance exercise reported an improvement in FEV1, while another study also demonstrated an enhancement in FEV1 after combining respiratory and other exercises. Only one article was available in the HIIT subgroup, which disclosed significant results (p < 0.05); however, the value obtained was negative, suggesting a potential adverse effect of this form of exercise on lung function. Certain studies have reported the benefits of HIIT in improving FEV1 among lung cancer patients; even perioperative HIIT has shown favorable outcomes for FEV1 [42]. Given the limited number of included articles for FEV1, further research would be valuable to elucidate existing findings.
Following exercise interventions, our analyses demonstrated improvements in exercise capacity indices, including 6MWD and VO2peak. Specifically, the effect size of 6MWD (MD = 35.80 m) exceeded the minimum significant difference range for lung cancer patients (i.e., 22–42 m) [43], indicating clinical relevance. Subgroup analyses proved that combined aerobic and resistance exercises markedly improved 6MWD, but it was not significantly improved by HIIT and respiratory exercises combined with other exercises. There was moderate heterogeneity between the aerobic and resistance combined subgroups, which may be attributed to differences in intervention methods, duration, or preoperative health status of patients. Furthermore, there were insufficient data to support comparisons between respiratory exercises combined with other exercise subgroups and control groups; however, two articles [31, 32] reported favorable effects of breathing training combined with other exercises on exercise capacity, as evidenced by elevated levels of 6MWD compared to controls. Given these findings, further studies are recommended to fully substantiate the effectiveness of breathing combined with other exercises on exercise capacity index 6MWD among NSCLC patients.
The combined results elicited that exercise improved VO2peak. The VO2 peak effect size was found in this study (MD = 1.05). For every 1 mL/kg/min increase in VO2peak in NSCLC patients, there is a 4% reduction in all-cause mortality [44]. Another study reported [45] that HIIT increased VO2peak in preoperative (4–6 weeks of training) [46] and postoperative (14 weeks of training) [47] NSCLC patients by 2.4 mL/kg 1/min 1 (14.6%) and 1.7 mL/kg 1/min 1 (11%), respectively. A combination of aerobic and resistance training maximizes VO2peak levels in postoperative NSCLC patients [48]. Thus, exercise improves VO2peak in postoperative NSCLC patients. In addition, skeletal muscle function has important prognostic value in NSCLC [49]. Our analyses suggest that exercise (excluding respiratory exercise) can strengthen the quadriceps. However, the moderate heterogeneity in the quadriceps analysis may be due to different methods and durations of exercise, as well as the patient's preoperative health status. Postoperative NSCLC patients tend to be more likely to improve muscle function by increasing their VO2peak [50].
Two evaluation methods assessed QOL: the SF-36 and the EORTC QLQ-C30. According to the combined results, exercise training improved the SF-36 body domain scores in NSCLC patients after pneumonectomy. The study found a 3.10-point difference in HRQoL physical domain scores between groups within the median SF-36 interval (i.e., 3–5 points) [51]. However, mental domain scores for HRQoL were not improved. Subgroup analyses by different exercise types revealed new findings. Four studies combining aerobic and resistance exercises reported improvements in the mental domains. However, there was no significant improvement in the two studies in the HIIT subgroup. One of the studies [28] found no marked difference between the HIIT group and the control group in mental domain values. Another trial [26] analyzed the effects of HIIT and found considerable improvements in the psychological domains. Wang et al. concluded [52] that resistance training in the postoperative period in conjunction with HIIT is particularly effective for improving QOL. Due to the small number of psychological domain indicators, further research may be needed to address this issue.
By taking measurements with the EORTC QLQ-C30, we found that exercise could improve physical functions. However, no improvement was observed in overall health using the EORTC QLQ-C30., indicating that exercise training alone has a limited impact on this domain. Therefore, it is necessary to combine exercise training with other interventions by a multidisciplinary team, including various health professionals, to achieve more comprehensive improvements.
Dyspnea is a common symptom in lung cancer patients in the early and middle stages. After pneumonectomy, dyspnea, physical activity, exercise tolerance, climbing ability, and QOL may worsen and remain impaired for 6 months or more [9, 53,54,55,56]. In addition, adjuvant therapies (e.g., chemotherapy or radiation) may negatively affect patients' symptoms and physical status, similar to those of other cancer patients [54]. Bailey et al. [57] have reported that because medications do not completely relieve symptoms and increase the risk of side effects, future research must focus on promising non-pharmacologic interventions to manage dyspnea. Our study suggests that a combination of exercise and breathing training may be a promising non-pharmacological intervention. It can increase diaphragmatic activity, improve alveolar ventilation, reduce energy expenditure during respiration, and alleviate shortness of breath in lung cancer patients [58]. Therefore, this method may be an effective method to control dyspnea in NSCLC patients after pneumonectomy.
The combined results showed no change in fatigue levels after exercise training. Interventional studies have reported [24, 27,28,29] no change in fatigue levels after targeted exercise programs. A trial randomized 17 NSCLC stage I–III A patients 6–10 weeks after lobectomy into an exercise group (8 weeks of aerobic and resistance training) and a control group (usual care). After intervention, no significant changes in fatigue were found in either group [28]. In contrast, Quist reported [30] that early postoperative exercise reduced fatigue in patients with operable NSCLC. Although these findings seem to support the benefit of exercise on fatigue in postoperative NSCLC patients, based on our results, we are still unable to conclude that exercise significantly affects fatigue. Therefore, further studies are required to explore the true contribution of exercise to fatigue in postoperative NSCLC.
Among the 12 included studies, various interventions were employed, encompassing aerobic exercise, resistance exercise, and HIIT. While aerobic exercise and resistance training were more commonly utilized, additional interventions such as respiratory muscle training (RMT) and combinations of exercises were also implemented. Pneumonectomy can result in significant reductions in exercise capacity, respiratory muscle strength, lung volumes, and HRQoL among patients. However, previous research demonstrated that exercise training could enhance both exercise capacity and HRQoL in individuals with various chronic diseases, including COPD [59] and heart failure [60], as well as those diagnosed with prostate or breast cancer [61, 62]. Moreover, programs involving exercise training reported similar benefits for NSCLC patients after pneumonectomy [20]. The combination of aerobic and resistance training enhanced VO2peak, while the complementary physiological adaptations resulting from combined training promote cardiovascular oxygen delivery, skeletal muscle oxidative phosphorylation, muscle strength, and optimal fiber type composition. Consequently, this improved muscular endurance, reduced fatigue, elevated exercise metabolic waste thresholds, and decreased ventilatory requirements during physical activity [36]. On the other hand, HIIT induced a protective cardiorespiratory phenotype while improving oxygen extraction from skeletal muscle by increasing capillary density and mitochondrial oxidative capacity [63, 64]. Studies demonstrated that HIIT intervention in lung cancer patients enhanced their VO2peak, which in turn improved circulatory, respiratory, and muscular functions, consequently enhancing exercise capacity and lung function and relieving dyspnea [50]. Moreover, RMT, comprising inspiratory muscle training (IMT) and expiratory muscle training (EMT), either alone or combined with other exercises, represented an innovative and highly valuable physical activity therapy for patients undergoing major surgery. Zou et al. discovered that the combination of RMT and aerobic exercise was linked to decreased postoperative hospital stay and reduced incidence of postoperative complications while increasing exercise capacity along with FEV1 and FEV1/FVC values [32]. Therefore, the combination of RMT, especially IMT, and other exercises should be regarded as one of the optimal exercise rehabilitation treatments for patients undergoing pre- and postoperative pneumonectomy. It is crucial to investigate the effects of the combination of RMT and other exercises on the clinical outcomes of patients undergoing pneumonectomy.
4.1 Limitations
Our meta-analysis has several limitations. First, many factors may contribute to clinical heterogeneity, such as differences in procedures, interventions, and control group characteristics. Second, due to differences in intervention methods, it is necessary to clarify which intervention specifically produced the overall effect. This issue requires further research. Third, due to insufficient supporting data, we did not perform subgroup analyses by VO2peak based on exercise training and the combination of exercise and breathing exercises. We did not analyze essential metrics such as inspiratory and expiratory muscle pressures. This issue also needs to be addressed in future studies.
5 Conclusions and suggestions
This paper illustrates the benefits of exercise for NSCLC patients in improving exercise capacity, lung function, and QOL in selected domains, enhancing quadriceps function, and relieving dyspnea. However, we cannot draw rigorous conclusions about the effects of different exercise modalities on exercise capacity in NSCLC patients due to the lack of in-depth exploration. Given the paucity of data on outcomes other than exercise capacity (including QOL and various symptoms), our study focused on analyzing lung function, exercise capacity, QOL, quadriceps function, dyspnea, and fatigue. Future studies should focus on other factors influencing cardiovascular adaptive capacity and respiratory muscle function in NSCLC patients. The effects of combining exercise training with other interventions delivered by a multidisciplinary team (e.g., psychologists, etc.) also need to be integrated into future RCTs.
Data availability
All data supporting the findings of this study are available within the paper and its Supplementary materials.
References
Canadian Cancer Statistics. A 2022 special report on cancer prevalence. Health Promot Chronic Dis Prev Can. 2023;43(1):49.
Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49.
Novello S, Barlesi F, Califano R, et al. Metastatic non-small-cell lung cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2016;27(suppl 5):v1–27.
Arbane G, Tropman D, Jackson D, Garrod R. Evaluation of an early exercise intervention after thoracotomy for non-small cell lung cancer (NSCLC), effects on quality of life, muscle strength and exercise tolerance: randomised controlled trial. Lung Cancer. 2011;71(2):229–34.
Sherwood JT, Brock MV. Lung cancer: new surgical approaches. Respirology. 2007;12(3):326–32.
Carli F, Scheede-Bergdahl C. Prehabilitation to enhance perioperative care. Anesthesiol Clin. 2015;33(1):17–33.
Bagan P, Berna P, De Dominicis F, et al. Nutritional status and postoperative outcome after pneumonectomy for lung cancer. Ann Thorac Surg. 2013;95(2):392–6.
Pouwels S, Fiddelaers J, Teijink JA, et al. Preoperative exercise therapy in lung surgery patients: a systematic review. Respir Med. 2015;109(12):1495–504.
Handy JR Jr, Asaph JW, Skokan L, et al. What happens to patients undergoing lung cancer surgery? Outcomes and quality of life before and after surgery. Chest. 2002;122(1):21–30.
Sarna L, Evangelista L, Tashkin D, et al. Impact of respiratory symptoms and pulmonary function on quality of life of long-term survivors of non-small cell lung cancer. Chest. 2004;125(2):439–45.
Granger CL, McDonald CF, Irving L, et al. Low physical activity levels and functional decline in individuals with lung cancer. Lung Cancer. 2014;83(2):292–9.
Burtin C, Franssen FME, Vanfleteren L, et al. Lower-limb muscle function is a determinant of exercise tolerance after lung resection surgery in patients with lung cancer. Respirology. 2017;22(6):1185–9.
Cavalheri V, Jenkins S, Cecins N, et al. Impairments after curative intent treatment for non-small cell lung cancer: a comparison with age and gender-matched healthy controls. Respir Med. 2015;109(10):1332–9.
Baracos VE, Reiman T, Mourtzakis M, Gioulbasanis I, Antoun S. Body composition in patients with non-small cell lung cancer: a contemporary view of cancer cachexia with the use of computed tomography image analysis. Am J Clin Nutr. 2010;91(4):1133s-s1137.
Murphy RA, Mourtzakis M, Chu QS, Reiman T, Mazurak VC. Skeletal muscle depletion is associated with reduced plasma (n-3) fatty acids in non-small cell lung cancer patients. J Nutr. 2010;140(9):1602–6.
Jones LW, Eves ND, Haykowsky M, Joy AA, Douglas PS. Cardiorespiratory exercise testing in clinical oncology research: systematic review and practice recommendations. Lancet Oncol. 2008;9(8):757–65.
Brocki BC, Andreasen JJ, Langer D, Souza DS, Westerdahl E. Postoperative inspiratory muscle training in addition to breathing exercises and early mobilization improves oxygenation in high-risk patients after lung cancer surgery: a randomized controlled trial. Eur J Cardiothorac Surg. 2016;49(5):1483–91.
Stigt JA, Uil SM, van Riesen SJ, et al. A randomized controlled trial of postthoracotomy pulmonary rehabilitation in patients with resectable lung cancer. J Thorac Oncol. 2013;8(2):214–21.
Granger CL, McDonald CF, Berney S, Chao C, Denehy L. Exercise intervention to improve exercise capacity and health related quality of life for patients with Non-small cell lung cancer: a systematic review. Lung Cancer. 2011;72(2):139–53.
Cavalheri V, Burtin C, Formico VR, et al. Exercise training undertaken by people within 12 months of lung resection for non-small cell lung cancer. Cochrane Database Syst Rev. 2019;6(6):Cd009955.
Book reviews. Appl Physiol Nutr Metab. 2012;37(4):807–8.
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700.
Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Granger CL, Chao C, McDonald CF, Berney S, Denehy L. Safety and feasibility of an exercise intervention for patients following lung resection: a pilot randomized controlled trial. Integr Cancer Ther. 2013;12(3):213–24.
Arbane G, Douiri A, Hart N, et al. Effect of postoperative physical training on activity after curative surgery for non-small cell lung cancer: a multicentre randomised controlled trial. Physiotherapy. 2014;100(2):100–7.
Edvardsen E, Skjønsberg OH, Holme I, et al. High-intensity training following lung cancer surgery: a randomised controlled trial. Thorax. 2015;70(3):244–50.
Salhi B, Huysse W, Van Maele G, et al. The effect of radical treatment and rehabilitation on muscle mass and strength: a randomized trial in stages I-III lung cancer patients. Lung Cancer. 2014;84(1):56–61.
Cavalheri V, Jenkins S, Cecins N, et al. Exercise training for people following curative intent treatment for non-small cell lung cancer: a randomized controlled trial. Braz J Phys Ther. 2017;21(1):58–68.
Messaggi-Sartor M, Marco E, Martínez-Téllez E, et al. Combined aerobic exercise and high-intensity respiratory muscle training in patients surgically treated for non-small cell lung cancer: a pilot randomized clinical trial. Eur J Phys Rehabil Med. 2019;55(1):113–22.
Quist M, Sommer MS, Vibe-Petersen J, et al. Early initiated postoperative rehabilitation reduces fatigue in patients with operable lung cancer: a randomized trial. Lung Cancer. 2018;126:125–32.
Liu JF, Kuo NY, Fang TP, et al. A six-week inspiratory muscle training and aerobic exercise improves respiratory muscle strength and exercise capacity in lung cancer patients after video-assisted thoracoscopic surgery: a randomized controlled trial. Clin Rehabil. 2021;35(6):840–50.
Zou H, Qin Y, Gong F, et al. ABCDEF pulmonary rehabilitation program can improve the mid-term lung function of lung cancer patients after thoracoscopic surgery: a randomized controlled study. Geriatr Nurs. 2022;44:76–83.
Wang J, Deng N, Qi F, et al. The effectiveness of postoperative rehabilitation interventions that include breathing exercises to prevent pulmonary atelectasis in lung cancer resection patients: a systematic review and meta-analysis. BMC Pulm Med. 2023;23(1):276.
Cavalheri V, Tahirah F, Nonoyama M, Jenkins S, Hill K. Exercise training undertaken by people within 12 months of lung resection for non-small cell lung cancer. Cochrane Database Syst Rev. 2013;7:Cd009955.
Cavalheri V, Granger C. Preoperative exercise training for patients with non-small cell lung cancer. Cochrane Database Syst Rev. 2017;6(6):Cd012020.
Jones LW, Watson D, Herndon JE 2nd, et al. Peak oxygen consumption and long-term all-cause mortality in nonsmall cell lung cancer. Cancer. 2010;116(20):4825–32.
Nakahara K, Ohno K, Hashimoto J, et al. Prediction of postoperative respiratory failure in patients undergoing lung resection for lung cancer. Ann Thorac Surg. 1988;46(5):549–52.
Brocki BC, Andreasen J, Nielsen LR, et al. Short and long-term effects of supervised versus unsupervised exercise training on health-related quality of life and functional outcomes following lung cancer surgery - a randomized controlled trial. Lung Cancer. 2014;83(1):102–8.
Ferguson MK, Watson S, Johnson E, Vigneswaran WT. Predicted postoperative lung function is associated with all-cause long-term mortality after major lung resection for cancer. Eur J Cardiothorac Surg. 2014;45(4):660–4.
Pompili C, Salati M, Refai M, et al. Preoperative quality of life predicts survival following pulmonary resection in stage I non-small-cell lung cancer. Eur J Cardiothorac Surg. 2013;43(5):905–10.
Pianosi PT, Liem RI, McMurray RG, et al. Pediatric exercise testing: value and implications of peak oxygen uptake. Children (Basel). 2017. https://doi.org/10.3390/children4010006.
Chen Z, Jia J, Gui D, et al. Functional and postoperative outcomes after high-intensity interval training in lung cancer patients: a systematic review and meta-analysis. Front Oncol. 2022;12:1029738.
Granger CL, Holland AE, Gordon IR, Denehy L. Minimal important difference of the 6-minute walk distance in lung cancer. Chron Respir Dis. 2015;12(2):146–54.
Hoffman AJ, Brintnall RA. A home-based exercise intervention for non-small cell lung cancer patients post-thoracotomy. Semin Oncol Nurs. 2017;33(1):106–17.
Jones LW, Eves ND, Waner E, Joy AA. Exercise therapy across the lung cancer continuum. Curr Oncol Rep. 2009;11(4):255–62.
Jones LW, Peddle CJ, Eves ND, et al. Effects of presurgical exercise training on cardiorespiratory fitness among patients undergoing thoracic surgery for malignant lung lesions. Cancer. 2007;110(3):590–8.
Jones LW, Eves ND, Peterson BL, et al. Safety and feasibility of aerobic training on cardiopulmonary function and quality of life in postsurgical nonsmall cell lung cancer patients: a pilot study. Cancer. 2008;113(12):3430–9.
Jones LW, Eves ND, Kraus WE, et al. The lung cancer exercise training study: a randomized trial of aerobic training, resistance training, or both in postsurgical lung cancer patients: rationale and design. BMC Cancer. 2010;10:155.
Deschenes MR, Kraemer WJ. Performance and physiologic adaptations to resistance training. Am J Phys Med Rehabil. 2002;81(11 Suppl):S3-16.
Hwang CL, Yu CJ, Shih JY, Yang PC, Wu YT. Effects of exercise training on exercise capacity in patients with non-small cell lung cancer receiving targeted therapy. Support Care Cancer. 2012;20(12):3169–77.
Samsa G, Edelman D, Rothman ML, et al. Determining clinically important differences in health status measures: a general approach with illustration to the Health Utilities Index Mark II. Pharmacoeconomics. 1999;15(2):141–55.
Wang J, Dong Y, Su J, et al. Postoperative exercise training improves the quality of life in patients receiving pulmonary resection: a systematic review and meta-analysis based on randomized controlled trials. Respir Med. 2022;192:106721.
Nagamatsu Y, Maeshiro K, Kimura NY, et al. Long-term recovery of exercise capacity and pulmonary function after lobectomy. J Thorac Cardiovasc Surg. 2007;134(5):1273–8.
Jack S, West MA, Raw D, et al. The effect of neoadjuvant chemotherapy on physical fitness and survival in patients undergoing oesophagogastric cancer surgery. Eur J Surg Oncol. 2014;40(10):1313–20.
Ni HJ, Pudasaini B, Yuan XT, et al. Exercise training for patients pre- and postsurgically treated for non-small cell lung cancer: a systematic review and meta-analysis. Integr Cancer Ther. 2017;16(1):63–73.
Cesario A, Ferri L, Galetta D, et al. Post-operative respiratory rehabilitation after lung resection for non-small cell lung cancer. Lung Cancer. 2007;57(2):175–80.
Bailey CD, Wagland R, Dabbour R, et al. An integrative review of systematic reviews related to the management of breathlessness in respiratory illnesses. BMC Pulm Med. 2010;10:63.
Liu W, Pan YL, Gao CX, et al. Breathing exercises improve post-operative pulmonary function and quality of life in patients with lung cancer: a meta-analysis. Exp Ther Med. 2013;5(4):1194–200.
Gloeckl R, Schneeberger T, Jarosch I, Kenn K. Pulmonary rehabilitation and exercise training in chronic obstructive pulmonary disease. Dtsch Arztebl Int. 2018;115(8):117–23.
Puhan MA, Gimeno-Santos E, Cates CJ, Troosters T. Pulmonary rehabilitation following exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2016;12(12):Cd005305.
Lahart IM, Metsios GS, Nevill AM, Carmichael AR. Physical activity for women with breast cancer after adjuvant therapy. Cochrane Database Syst Rev. 2018;1(1):Cd011292.
Mishra SI, Scherer RW, Geigle PM, et al. Exercise interventions on health-related quality of life for cancer survivors. Cochrane Database Syst Rev. 2012;2012(8):Cd007566.
Powers SK, Smuder AJ, Kavazis AN, Quindry JC. Mechanisms of exercise-induced cardioprotection. Physiology. 2014;29(1):27–38.
Reis Gonçalves CT, Reis Gonçalves CG, de Almeida FM, et al. Protective effects of aerobic exercise on acute lung injury induced by LPS in mice. Crit Care. 2012;16(5):R199.
Acknowledgments
Not applicable.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
Conceptualization, M.-Y.J.; methodology, M.-Y.J., M.-G.Z. and H.-P.L.; software, M.-Y.J. and M.-G.Z.; validation, M.-Y.J., M.-G.Z. and H.-P.L.; formal analysis, M.-Y.J. and M.-G.Z., investigation, M.-Y.J., M.-G.Z. and H.-P.L.; resources, M.-Y.J. and M.-G.Z.; writing—original draft preparation, M.-Y.J., M.-G.Z. and H.-P.L.; writing—review and editing, M.-Y.J., M.-G.Z. and H.-P.L.; visualization, M.-Y.J.; supervision, M.-Y.J.; project administration, M.-Y.J. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jiao, M., Liang, H. & Zhang, M. Effect of exercise on postoperative recovery of patients with non-small cell lung cancer: a systematic review and meta-analysis. Discov Onc 15, 230 (2024). https://doi.org/10.1007/s12672-024-01079-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12672-024-01079-w