Abstract
In the clinical setting, small intestinal bacterial overgrowth (SIBO) is a frequent, but under-diagnosed entity. SIBO is linked to various gastrointestinal (GI) and non-GI disorders with potentially significant morbidity. The optimal management of SIBO is undefined while there is a lack of published consensus guidelines. Against this background, under the auspices of the Indian Neurogastroenterology and Motility Association (INMA), formerly known as the Indian Motility and Functional Diseases Association (IMFDA), experts from the Asian-Pacific region with extensive research and clinical experience in the field of gut dysbiosis including SIBO developed this evidence-based practice guideline for the management of SIBO utilizing a modified Delphi process based upon 37 consensus statements, involving an electronic voting process as well as face-to-face meetings and review of relevant supporting literature. These statements include 6 statements on definition and epidemiology; 11 on etiopathogenesis and pathophysiology; 5 on clinical manifestations, differential diagnosis, and predictors; and 15 on investigations and treatment. When the proportion of those who voted either to accept completely or with minor reservations was 80% or higher, the statement was regarded as accepted. The members of the consensus team consider that this guideline would be valuable to inform clinical practice, teaching, and research on SIBO in the Asian-Pacific region as well as in other countries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The human gut is inhabited by an intricate population of microbes, collectively known as microbiota. The composition of microbiota in the proximal gut differs qualitatively as well as quantitatively from that in the colon [1]. Usually, the small intestine is devoid of coliform bacteria, and even if present the number is little. Small intestinal bacterial overgrowth (SIBO) is characterized by the presence of an excessive amount of bacteria within the small intestine, which may result in a constellation of gastrointestinal (GI) symptoms [2, 3].
Studies utilizing molecular techniques suggest that compared to the true prevalence, SIBO remains in the clinical setting frequently undiagnosed [4]. Etiopathogenesis of SIBO is multifactorial [1] and it is linked to several GI and non-GI disorders with significant morbidity including irritable bowel syndrome (IBS), non-alcoholic fatty liver disease (NAFLD), chronic pancreatitis, celiac disease, obesity, and inflammatory bowel disease (IBD) [5]. Contrasting the prevalence, research into SIBO has just started and this condition remains worldwide largely under-researched.
While diagnostic modalities for SIBO are still evolving, its management also remains a challenge with the limited data and the absence of consensus-based clinical guidelines. Against this background and under the auspices of the Indian Neurogastroenterology and Motility Association (INMA), formerly known as the Indian Motility and Functional Diseases Association (IMFDA), experts from the Asian-Pacific Region with clinical and research experience in the field of SIBO and gut dysbiosis collaborated with the aim to develop evidence-based practice guideline for the management of patients with SIBO. The consensus team aimed to provide valid guidance for clinical practice, teaching, and future research on SIBO across the globe with the first consensus-based guideline that utilized a rigorous Delphi process.
Methods
The members of the consensus team were selected from Asian-Pacific countries based on their interest and experience in the field of gut dysbiosis including SIBO as evidenced by an electronic literature search on PubMed. The members included experts from India, Bangladesh, China, South Korea, Singapore, Hong Kong, Malaysia, and Australia. A core group of four members was selected from among the consensus team members who made the first set of 37 statements on definition, epidemiology, etiopathogenesis, pathophysiology, clinical manifestations, differential diagnosis, predictors, investigations, and treatment. The members of the core team had a preliminary face-to-face meeting in Lucknow (India) on 10th November 2017 to develop preliminary statements for further refinement and discussion by the full consensus group.
The consensus process involved a modified Delphi method [6]. Before the first round of voting on the statements, an electronic library was created in the Digital Medical Education section of the Shanti Public Educational and Development Society website (www.spreadhealth.in). The first round of online voting was held in July 2019. The voting was conducted in an electronic online anonymous voting system developed in the Research and Innovation initiative menu in the www.spreadhealth.in and the results were analyzed electronically. The result of the first round of voting was presented to the entire consensus team in a face-to-face meeting held in Kolkata (India) on 13th December 2019, on the sidelines of the Asian-Pacific Digestive Week-2019 (APDW-2019) Conference. During this face-to-face meeting at Kolkata, a discussion was held on the modification of five statements, which could not reach 80% acceptance during the first round of voting. Also, the formulation of an algorithm for the management of SIBO was discussed. The second round of online voting was subsequently held in January 2020 in which the five modified statements were put to voting. Method of Grading of Recommendations, Assessment, Development and Evaluation (GRADE) Working group was used for deriving at the level of agreement, level of evidence, and grade of recommendation (Table 1) [7]. When the proportion of those who voted either to accept completely or with some reservation was 80% or higher, the statement was regarded as accepted. Finally, a consensus was achieved on all 37 statements, which included the five modified statements. An algorithm of management of SIBO was finalized as per suggestions of the consensus team. However, due to the pandemic of Corona Virus Disease-19 (COVID-19) that devastated the whole world, further works on this consensus got stalled for the next 2 years. On 7th May 2022, the core group members of the consensus team physically met during the 5th Annual Congress of the Indian Motility and Functional Diseases Association (now named as INMA) in Lucknow, India, to finalize the manuscript for publication. The consensus was presented on the same day to all the delegates of the 5th INMA Congress.
Consensus statements
Definition and epidemiology
Statement 1: Small intestinal bacterial overgrowth (SIBO) is defined as the growth of bacteria ≥ 105 colony-forming unit (CFU)/mL or ≥ 103 CFU/mL (particularly if coliforms are present) on a quantitative culture of upper gut aspirate.
Voting summary: Accepted completely 57.9%, accepted with some reservation 36.8%, accepted with major reservation 5.3%.
Level of evidence: II-2.
Grade of recommendation: B.
SIBO is a clinical condition caused by the presence of an excessive amount of bacteria within the small intestine. It is defined as the growth of bacteria ≥105 CFU/mL or ≥103 CFU/mL (particularly if coliforms are present) on a quantitative culture of upper gut aspirate [1, 8,9,10,11,12,13,14]. Healthy controls have generally <103CFU/mL in the upper bowel aspirate culture. However, all these cut-offs need large, good-quality validation studies from different populations across the globe.
Traditionally, a cut-off of ≥105 CFU/mL has been used to define SIBO, but some authors find it too rigorous for conditions other than blind loop syndrome [10]. Hence, a few investigators have tested lower thresholds (≥103 CFU/mL) in studies of SIBO in varied disorders [13,14,15,16,17]. Researchers from North America have recently suggested a lower cut-off of ≥103 CFU/mL for diagnosis of SIBO [18, 19]. The cut-off of ≥103 CFU/mL proposed by this group may be more relevant, especially when performing culture of duodenal aspirate as bacterial counts in the duodenum are expected to be lower due to more acidic environment than that in the jejunum [2]. A recent 16S ribosomal RNA (rRNA) gene sequencing–based study found that culture-based cut-off of >103CFU/mL for SIBO correlated well with clinical symptoms, breath test results, and sequencing [20].
Statement 2: SIBO can be high- or low-threshold depending upon the bacterial counts.
Voting summary: Accepted completely 100%.
Level of evidence: III.
Grade of recommendation: C.
The culture-based threshold for SIBO has been contentious, both as per published data as well as the opinion of the concerned experts. Several investigators have put forward their viewpoint of the low- or high-threshold for SIBO based upon the bacterial counts in the small bowel aspirate [13, 15,16,17]. Low threshold is mostly taken as counts ≥103 CFU/mL, while a high-threshold implies counts ≥105 CFU/mL. The use of varying thresholds has yielded different rates of prevalence of SIBO in several studies. It is quite understandable that the use of a lower threshold often results in a higher frequency of SIBO in the clinical studies reported to date.
A study from Sweden reported a SIBO prevalence of 4% in both IBS patients and controls while using the conventional threshold of ≥105 CFU/mL, but the prevalence was found to be significantly different (43% in IBS vs. 12% in controls) when the lower threshold was used [15]. In a vital study from India on 80 subjects with IBS, 15/80 (19%) had SIBO as per the conventional threshold of ≥105 CFU/mL, while 19/80 (23.8%) additional patients had low-grade or low-threshold SIBO (bacterial counts of ≥103 to 105 CFU/mL) [13]. In a study from the USA on 139 patients with unexplained gas, bloating and diarrhea, the prevalence of SIBO using low- and high-thresholds was 44.6% and 18%, respectively [16]. In a study from India in patients with non-alcoholic steatohepatitis (NASH), jejunal aspirate culture on 35 subjects yielded SIBO in 14/35 (40%) when a low-threshold was used, but the prevalence was only 5/35 (14.3%) when the high-threshold was used [17]. A recent North American consensus on breath testing and American College of Gastroenterology guideline document on SIBO proposed using a lower threshold, i.e. ≥103 CFU/mL in upper gut aspirate culture for diagnosis of SIBO [18, 19].
Statement 3: Microbiological spectrum in SIBO may vary based on the underlying causes.
Voting summary: Accepted completely 68.3%, accepted with some reservation 21.1%, accepted with major reservation 5.3%, rejected with reservation 5.3%.
Level of evidence: II-2.
Grade of recommendation: B.
Based on the type of microflora, the cultured bacteria in subjects with SIBO can be broadly classified as Gram-positive flora and coliform flora [21, 22]. Isolated Gram-positive flora may include Streptococcus, Staphylococcus, Enterococcus, Micrococcus, Lactobacillus, Corynebacterium, Fusobacterium, and Peptostreptococcus, while predominant among Gram-negative flora are Escherichia coli (E. coli), Klebsiella, Proteus, Acinetobacter, Enterobacter, Citrobacter, Neisseria, Bacteroides, and Clostridia. There may be a mix of Gram-positive and Gram-negative populations, as well as aerobic and anaerobic bacteria [16, 23].
The type of isolated bacterial species may vary depending upon the underlying pathophysiology [21, 24,25,26]. While depletion of the gastric acid barrier due to hypochlorhydria, use of proton pump inhibitors (PPIs), or other causes may predispose to SIBO with Gram-positive flora [24, 25], pathophysiological mechanisms like small bowel anatomical alterations and sub-optimal intestinal clearance function predisposes to SIBO with predominantly Gram-negative flora [26].
In a study from Norway [24] on fifteen healthy subjects with a mean age of 84 years, 12 (80%) were found to have hypochlorhydria with mean pH of 6.6 and a mean bacterial count of 108 CFU/mL in fasting gastric aspirate. Normochlorhydric individuals had counts of ≤101 CFU/mL. Predominant microflora detected included Streptococcus viridans, coagulase-negative staphylococci, and Haemophilus species. E. coli and Klebsiella were found in only one individual. No subject had strict anaerobes in culture of aspirate.
Similarly, data from Switzerland [25], utilizing duodenal aspirate culture performed on 25 patients with peptic ulcer disease taking omeprazole for more than 5 weeks, and 15 control subjects who were outpatients referred for upper GI endoscopy but with no exposure to PPIs found SIBO in 56% of subjects on PPI and 0% of controls. Hemolytic and non-hemolytic streptococci were the most commonly isolated bacteria.
Various etiologies of malabsorption syndrome (MAS) are associated with intestinal stasis that may result in SIBO [27, 28]. In a study from Lucknow (India) [26], jejunal aspirate cultures of 50 patients with MAS were analyzed. The culture showed growth of bacteria in 34/50 (68%) subjects with MAS with 21/50 (42%) having counts ≥105 CFU/mL. The commonest isolated bacteria were Streptococcus species and E. coli.
Statement 4: The frequency of SIBO is low among healthy subjects but is higher in the elderly.
Voting summary: Accepted completely 84.1%, accepted with some reservation 5.3%, accepted with major reservation 5.3%, rejected with reservation 5.3%.
Level of evidence: II-2.
Grade of recommendation: B.
As per different published studies with an evaluation of small sets of healthy subjects as controls, SIBO has been reported in 0% to 22% depending primarily on the type of diagnostic test used [29, 30]. Frequency of SIBO is higher in the elderly ranging from 14.5% to 56% [31, 32]. A cross-sectional survey from Germany revealed SIBO in 15.6% in older adults, compared with 5.9% in subjects aged 24 to 59 years [33]. Several studies on SIBO in GI disorders have found older age to be an independent risk factor for the occurrence of SIBO [34,35,36].
Elderly subjects are expected to be more prone to SIBO because of several factors like reduced gastric acid [24], reduced GI motility, anatomic factors like diverticula, co-morbidities like diabetes mellitus, and use of various medications, which may predispose to SIBO. A study from the UK [37] found that factors predictive of a positive glucose hydrogen breath test (GHBT) in the elderly included increasing age (>75 years), low serum vitamin B12, low serum albumin, previous partial gastrectomy, previous right hemicolectomy, presence of small bowel diverticula, and concurrent use of a PPI. In fact, a study from Lucknow, India, showed that lower levels of hemoglobin were associated with a greater likelihood of SIBO [38], which is commensurate with the data on the elderly showing low serum B12 to be predictive of the presence of SIBO.
Statement 5: In several conditions, the prevalence of SIBO is higher than in healthy controls.
Voting summary: Accepted completely 89.4%, accepted with some reservation 5.3%, accepted with major reservation 5.3%.
Level of evidence: II-2.
Grade of recommendation: A.
The true prevalence of SIBO in the general population or even in at-risk groups is not precisely established [29, 39]. Overall, as a clinical entity, it is still under-recognized. It has been associated with a plethora of gastroenterological as well as non-gastroenterological disorders [2]. The most prominent GI conditions linked with SIBO include IBS, IBD, tropical sprue, celiac disease, dyspepsia, small bowel diverticulosis/stricture/fistula, radiation enteropathy, pancreatitis, NAFLD, liver cirrhosis, and post-abdominal surgery. The most eminent non-GI disorders reported to be associated with SIBO include systemic sclerosis, diabetes mellitus, hypothyroidism, obesity, Parkinson’s disease, multiple sclerosis, muscular dystrophy, end-stage renal failure, coronary artery disease, immunodeficiency syndromes, chronic fatigue syndrome, restless leg syndrome, fibromyalgia, and rosacea [30, 39]. . More recently, utilizing a culture-independent technique, some of the authors found higher bacterial load in patients with functional GI disorders as compared to controls [4].
The frequency of SIBO in these associated disorders is highly variable, ranging from as low as 4% to as high as 93% [2, 30]. Many of these studies, which included a small set of healthy subjects as controls, reported SIBO in 0% to 22% in such subjects [29, 30]. A few more interesting clinical entities have been recently added to the list of associations with SIBO. These include environmental enteropathy, familial Mediterranean fever, deep venous thrombosis, Helicobacter pylori infection, gallstone disease, post-cholecystectomy, and post-colectomy states [39,40,41,42,43,44,45,46]. A recent study from France reported a very high (83%) prevalence of SIBO in a cohort of patients with abdominal symptoms following Roux-en-Y gastric bypass for obesity [47].
Statement 6: Among specific disorders associated with SIBO, the reported prevalence differs substantially based on the population studied and the diagnostic method/criteria used to diagnose SIBO.
Voting summary: Accepted completely 94.7%, accepted with some reservation 5.3%.
Level of evidence: II-2.
Grade of recommendation: A.
In particular, disorders associated with SIBO, the published prevalence differs considerably based on the study population and type of diagnostic modality [11, 29, 48]. Such large variability in the prevalence of SIBO in disease populations as well as in healthy controls is primarily due to limitations of current diagnostic technologies [39]. If the breath test is used for evaluation, the frequency of SIBO varies further depending on the nature and dosage of the test substrate used for testing. If upper gut aspirate culture analysis is used for diagnosis, then the diagnostic threshold used for diagnosis often decides the prevalence rates. A recent meta-analysis [49] which included 19 case-control studies of SIBO in chronic liver disease (CLD) found the prevalence of SIBO in CLD using the breath tests was 35.80% compared with 8.0% in controls. However, with culture-based methods, the prevalence was 68.31% in CLD patients as compared with 7.94% in controls.
The best GI disorder which exemplifies the essence of this statement is IBS. Posserud et al. reported a SIBO prevalence of only 4% in IBS patients and controls while using the culture threshold of ≥105 CFU/mL, but the prevalence was 43% in IBS vs. 12% in controls when a lower threshold of ≥103 CFU/mL was used [15]. Ghoshal et al., in a study on 80 patients with IBS, found SIBO in 15/80 (19%) as per the conventional threshold of ≥105 CFU/mL in upper gut aspirate culture [13, 14]. Assuming culture to be the gold standard, 4/15 (27%) with and none of 65 without SIBO had a positive result on GHBT (sensitivity 27%, specificity 100%). None of 15 with and one of 65 without SIBO had documented double peaks on lactulose hydrogen breath test (LHBT) (sensitivity 0%, specificity 98%); and 5/15 (33%) with and 23/65 (35%) without SIBO had an early peak documented on LHBT (sensitivity 33%, specificity 65%) [13]. A very recent systematic review and meta-analysis summarizing 6 case-control and cohort studies also pointed towards a link between SIBO and functional dyspepsia [50].
In a meta-analysis of 12 studies of SIBO in IBS [51], with 1921 subjects, the pooled prevalence of a positive LHBT or GHBT was 54% and 31%, respectively while the prevalence of a positive jejunal aspirate and culture was only 4%. The prevalence in IBS compared with the control subjects varied according to the criteria used to define a positive test. A recent review reported wide variations in prevalence of SIBO as per culture/GHBT/LHBT in controls (0–4%/1–13%/7–40%) and patients with IBS (4.3–44.6%/6.2–45.8%/10–78%) [48]. A recent meta-analysis of fifty studies of SIBO in IBS showed that pooled prevalence of SIBO in IBS was higher in studies diagnosed by breath tests (40%) compared with aspirate cultures (19%) [36]. Another meta-analysis [52] that included 25 studies found that SIBO prevalence in patients with IBS vs. controls showed wide variability depending on the diagnostic method used (breath testing: 35.5% vs. 29.7%; culture with ≥105 CFU/mL cut-off: 13.9% vs. 5.0%; culture with ≥103 CFU/mL cut-off: 33.5% vs. 8.2%). SIBO prevalence diagnosed by LHBT was much higher in both IBS (3.6-folds) and controls (7.6-folds) compared to GHBT. Similarly, LHBT over-diagnosed SIBO as compared to culture. The most recent meta-analysis [53] analyzed 37 studies and found an overall prevalence of SIBO in IBS as 36.7% (range: 4.3% to 83.7%). The range of prevalence as per GHBT, LHBT, and upper gut aspirate culture was 6.2% to 45.8%, 18.4% to 83.7%, and 4.3% to 44.6%, respectively. In addition, IBD also appears to be associated with SIBO [54], which has also been shown in a recent study from India [55]. Patients with Crohn’s disease more often had SIBO than those with ulcerative colitis in this study [55].
Etiopathogenesis and pathophysiology
Statement 7: Disruption of endogenous gut defense mechanisms is known to result in SIBO.
Voting summary: Accepted completely 52.6%, accepted with some reservation 36.8%, accepted with major reservation 10.6%.
Level of evidence: II-2.
Grade of recommendation: B.
Several host defense mechanisms help to prevent SIBO. These include gastric acid, bacteriostatic properties of pancreatobiliary secretions, maintained GI motility especially the coordinated antegrade small bowel peristalsis with intact migratory motor complex (MMC), intact structure and function of the ileocecal cecal valve, salivary immunoglobulin (Ig)-A, pentavalent IgA in the intestinal secretions, defensins from Paneth cells, protective intestinal mucus layer, intact intestinal mucosal immune system, and protective effects of some beneficial commensal flora like lactobacilli [1, 11, 19, 21, 29]. Disruption or deficiency of any one or more of these protective mechanisms may result in the development of SIBO.
Loss of protective gastric acid barrier for any reason may result in SIBO, especially with Gram-positive bacteria [21, 24]. In vitro and in vivo studies indicate that more than 99% of the ingested bacteria get killed within minutes by the physiological gastric acid barrier thus, preventing their colonization in the upper GI tract [56]. Hypochlorhydia or achlorhydria due to any cause like aging, autoimmune gastritis, H. pylori–related atrophic gastritis, or partial or total gastrectomy increases the risk of SIBO [19, 24, 57,58,59]. In a study from Norway [24] on fifteen healthy elderly subjects, 12 (80%) were found to have hypochlorhydria and had an average bacterial count of 108 CFU/mL in fasting gastric aspirate as against counts of ≤101 CFU/mL in normochlorhydric subjects. Predominant bacteria detected were Gram-positive. A case-control study from Korea [58] compared the prevalence of SIBO in post-gastrectomy patients and controls using GHBT. The frequency of SIBO was significantly higher in these patients than in controls (77.6% vs. 6.7%). SIBO was shown to be associated with postprandial intestinal symptoms and late hypoglycemia. Hypochlorhydria caused by treatment with PPI has been reported to be associated with SIBO in several studies [25, 60,61,62,63,64]. However, a few other studies had different conclusions [65,66,67].
Small bowel motility with intact antegrade peristalsis is a vital protective mechanism against SIBO. Any primary or acquired disorder that hampers the enteric neuromuscular system may result in bacterial overgrowth [21]. Disorders like scleroderma, diabetes mellitus, hypothyroidism, and drugs like opioids may disrupt this critical defense mechanism, thus predisposing to SIBO [35, 68,69,70,71,72,73,74,75,76,77]. Prolongation of oro-cecal transit time (OCTT) and small bowel transit time (SBTT) have both been shown to be associated with SIBO [73,74,75, 78,79,80,81,82]. Intact competence of ileocecal valve has also been shown to be an important defense against SIBO [82, 83].
Since intestinal mucosal immunity regulates gut microbiota, its disruption may predispose to SIBO. But there are limited studies to support this issue. Local (GI) and systemic immune deficiency have both been reported to be associated with an increased risk of SIBO [84,85,86]. A study from Italy evaluated SIBO in children with IgA deficiency, T-cell deficiency, and hypogammaglobulinemia [86]. SIBO was detected in 5/12 (41.6%) using an upper gut aspirate culture [86]. A study from Mexico evaluated 18 adult patients with small bowel nodular lymphoid hyperplasia [87]. Nine patients (50%) had evidence of immunodeficiency and SIBO was detected in 3 (17%) subjects.
Statement 8: Several disorders that alter GI motility may lead to SIBO.
Voting summary: Accepted completely 89.4%, accepted with some reservation 5.3%, accepted with major reservation 5.3%.
Level of evidence: II-1.
Grade of recommendation: A.
Normal small intestinal motility driven by MMC and coordinated antegrade peristalsis helps in the propulsion of food, microbes, and secretions, thus protecting against bacterial or fungal overgrowth [19, 88]. Slowing of intestinal motility either by drugs or disease conditions leads to stagnation of intraluminal contents, which assists in the development of SIBO [70, 81]. Origin of intestinal dysmotility may be neuropathic or myopathic, which in turn can be either primary or secondary to a variety of disorders like scleroderma, amyloidosis, muscular dystrophy, radiation enteropathy, and even paraneoplastic syndrome [21, 89]. Chronic intestinal pseudo-obstruction (CIPO) represents a most severe form of many of these underlying disorders. Several other systemic disorders like diabetes mellitus, hypothyroidism, chronic renal failure, and neurodegenerative conditions (Parkinsonism, multiple sclerosis) can affect GI motility and predispose to SIBO [11, 39]. Dysfunction of the ileocecal valve has also been shown to contribute to the pathogenesis of SIBO [82]. An interesting study from the USA [63] evaluated subjects with unexplained GI symptoms and found GI dysmotility and PPI use to be independent predictors of SIBO or small intestinal fungal overgrowth (SIFO).
The prototype of disorders that predispose to SIBO by altering GI motility is systemic sclerosis (SSc). A study from Italy evaluated 55 patients with SSc and 60 healthy controls [68]. LHBT was used for the assessment of OCTT and SIBO. Frequency of SIBO was significantly higher in SSc than in controls (55.6% vs. 6.7%) and average OCTT was significantly longer in SSc than in controls (150 vs. 105 min) suggesting impaired intestinal motility in SSc. A study from France [69] evaluated 51 subjects with SSc for SIBO using GHBT. The prevalence of SIBO was 43.1% and predictors of SIBO included the presence of diarrhea or constipation. Another study from France used GHBT to evaluate SIBO in 37 subjects with SSc having GI symptoms [70]. Prevalence of SIBO in these subjects was found to be 38%, and predictors of SIBO included longer disease duration and significant weight loss in the last 6 months. A recent study from Thailand evaluated 89 patients with SSc for SIBO using GHBT [90]. Of 89 patients included in this study, 12 had SIBO by GHBT yielding prevalence of 13.5% and longer disease duration was a predictor of SIBO [90]. A study from Chandigarh (India) performed GHBT for SIBO and LHBT for OCTT in 37 patients with SSc [91]. SIBO was found in 7/37 and OCTT was prolonged in 23/37 patients. A recent systematic review from Poland analyzed 7 studies on this issue [71]. The analysis showed a pooled prevalence of SIBO of 39% in patients suffering from SSc. Longer duration of illness predisposed to SIBO in these patients.
Another important systemic condition that may predispose to SIBO by affecting GI motility is diabetes mellitus. A case-control study from Chandigarh (India) evaluated the frequency of SIBO in 84 patients with diabetes mellitus and 45 controls using GHBT) [73]. In addition, an estimate was made of the OCTT. The prevalence of SIBO in patients was significantly higher than in controls (15.5% vs. 2.2%). OCTT was significantly higher in diabetic patients with SIBO. In another case-control study from India, 175 patients with diabetes mellitus and an equal number of healthy controls were evaluated for SIBO and OCTT using GHBT and LHBT, respectively [74]. The prevalence of SIBO was significantly higher in patients as compared to controls (14.8% vs. 2.8%). The OCTT in diabetic patients was significantly longer than in controls, and that in patients with SIBO was higher than in those without SIBO. In another case-control study, Malik et al. evaluated 75 patients with type I diabetes mellitus and 75 healthy subjects using GHBT (for SIBO) and LHBT (for OCTT) [75]. They also measured plasma levels of inflammatory cytokines and anti-oxidants, as well as oxidative stress parameters, to assess the interplay of SIBO with these factors. The prevalence of SIBO was significantly higher in patients as compared to controls (22.7% vs. 1.3%). The OCTT in patients was significantly higher than in controls, and that in patients with SIBO was higher than those without SIBO. Levels of inflammatory cytokines, superoxide dismutase, and catalase were significantly higher but levels of reduced glutathione significantly lower in patients as compared to controls. A study from Italy [72] evaluated 74 subjects with diabetes using LHBT and found that 21 of them had SIBO and delayed OCTT. These 21 subjects were tested again with LHBT after a course of rifaximin. Sixty-two percent of patients showed a significant decrease in OCTT along with eradication of SIBO, 24% had relief of SIBO but still had delayed OCTT, and three subjects (14%) had persistence of SIBO despite treatment with rifaximin.
Another condition that may predispose to SIBO by altering GI motility is hypothyroidism [2, 19, 76]. Several reports suggest that hypothyroidism reduces GI motility [92,93,94]. A study from Italy evaluated 50 patients with hypothyroidism and 40 controls for SIBO using GHBT [76]. Prevalence of SIBO was significantly higher in patients than in controls (54% vs. 5%). Abdominal discomfort, flatulence, and bloating were more frequent in patients who were positive for SIBO. These abdominal symptoms improved significantly after antibiotic therapy.
Some neurological conditions like Parkinson’s disease have also been reported to be associated with SIBO [2, 19, 29, 95, 96]. A study from Italy [97] evaluated 33 patients with Parkinson’s disease and 30 controls for SIBO. The prevalence of SIBO was significantly higher in patients than in controls (54.5% vs. 20.0%) and SIBO was associated with unpredictable motor fluctuations in patients with Parkinson’s disease. Moreover, the eradication of SIBO resulted in an improvement in motor fluctuations. A multicenter study evaluated the prevalence of SIBO in 103 patients with Parkinson’s disease using LHBT [98]. Prevalence of SIBO in Parkinson’s disease was 25.3% and SIBO independently predicted worse motor function. A recent case-control study from China evaluated 182 patients with Parkinson’s disease and 200 controls for SIBO using GHBT [99]. Prevalence of SIBO was significantly higher in patients with Parkinson’s disease than in controls (30.2% vs. 9.5%), and SIBO was associated with worse GI symptoms and worse motor function.
Statement 9: Drugs that retard GI motility, reduce acid, or break mucosal integrity may predispose to SIBO.
Voting summary: Accepted completely 68.4%, accepted with some reservation 31.6%.
Level of evidence: II-2.
Grade of recommendation: B.
Several classes of drugs may predispose to SIBO. These include drugs that slow down the gut motility like opioids, anticholinergics, antidiarrheals, and tricyclic antidepressants [2, 19, 21, 100, 101]. A study from Mayo Clinic (USA) evaluated clinical predictors of SIBO in duodenal aspirate culture and found narcotic use to be one of the factors associated with SIBO with odds ratio (OR) of 2.7 [35]. A recent study from the USA reported opioid use to be one of the predictors of SIBO in patients with chronic pancreatitis [77].
Drugs that break mucosal integrity of the small intestine may predispose to SIBO. These include primarily non-steroidal anti-inflammatory drugs (NSAIDs). Small intestinal injury induced by NSAIDs is dependent on bile secretion and is reported to augment the growth of several bacterial species, especially enterococci. An experimental rat study from Texas (USA) evaluated the relationship between indomethacin-related intestinal injury and SIBO [102]. The colony counts of ileal enterococci were significantly increased (500- to 1000-folds) in indomethacin-treated rats. Gut injury in these rats was associated with enterococcal overgrowth. Indomethacin-induced gut injury and bacterial overgrowth were independent of the route of administration of indomethacin. A study from Japan evaluated 43 patients taking NSAIDs for over 3 months [103]. All the subjects were examined with LHBT and video capsule endoscopy. Twenty-two (51%) patients had severe small intestinal damage. SIBO was detected in 5 of 21 patients (24%) without severe small intestinal damage and in 13 of 21 patients (59%) with severe small intestinal damage. SIBO on LHBT was significantly associated with an increased OR for severe small intestinal damage (OR, 6.54).
PPIs represent the prototype of acid-lowering drugs that have been shown in several studies to be associated with increased risk of SIBO [25, 60,61,62,63,64]. A few studies, however, have not supported this association [65,66,67]. PPIs are commonly prescribed drugs for several upper GI disorders like gastroesophageal reflux disease, H. pylori–related gastritis, gastroduodenal ulcers or erosions, and functional dyspepsia. PPIs are potent inhibitors of gastric acid secretion and since gastric acidity is an important gatekeeper defense against bacterial colonization in the upper GI tract, the use of PPIs, especially if use is prolonged [61], may increase the risk of bacterial overgrowth in the upper GI tract. Association of PPI use with SIBO has been shown by both breath testing [61, 62] and culture methods [25, 60, 63, 64].
An interesting study from India evaluated the impact of the addition of prokinetics to PPI on the frequency of SIBO. The authors observed that the group receiving PPI alone had a SIBO prevalence of 13.2% as against a prevalence of only 1.8% (p<0.05) in the group receiving PPI with prokinetics. The latter group also had faster OCTT as expected, and this was the possible reason for lower rates of SIBO in the dual therapy group [104]. A recent study utilizing a molecular technique also found increased bacterial load in PPI users as compared to non-PPI users, irrespective of comorbidities [4].
A meta-analysis of 11 studies showed an association of SIBO with PPI use when the upper gut aspirate culture was used for the diagnosis of SIBO [105]. A recent meta-analysis that included 19 studies and 7055 subjects also supported this association, but the pooled OR for this association was only 1.71, which is quite modest [106]. Subgroup analyses showed an association between SIBO and PPI use in studies that used aspirate culture and GHBT for diagnostic evaluation. A recent meta-analysis evaluated the prevalence and predictors of SIBO in IBS [36] and reported that PPI use was not associated with SIBO in patients with IBS.
Statement 10: A proportion of patients with functional GI disorders (FGIDs) especially those with IBS have been reported to be having SIBO.
Voting summary: Accepted completely 73.6%, accepted with some reservation 21.1%, accepted with major reservation 5.3%.
Level of evidence: II-2.
Grade of recommendation: A.
Several studies both in adults and children have reported SIBO in a fraction of patients with FGIDs, currently called disorders of gut-brain interaction, prominent among which by all means is IBS. In a study from Chile [107] in 367 patients with FGIDs, LHBT was used to evaluate for SIBO. SIBO was reported in 76% of subjects with IBS, 73% of those with functional constipation, 69% of those with functional diarrhea, and 68% of patients with functional bloating. In a study from the Netherlands [108] in pediatric patients with abdominal pain, GHBT was used for the evaluation of SIBO. SIBO was found in 14.3% of the subjects. IBS, altered defecation pattern, loss of appetite, and belching were predictors of the occurrence of SIBO. In a study from the USA, 75 children with chronic abdominal pain and 40 healthy controls were evaluated for SIBO using LHBT. The prevalence of abnormal LHBT in patients and controls was 91% and 35%, respectively [109]. In a study from India on 62 children with functional abdominal pain, SIBO as defined by abnormal GHBT was found in 17% [110].
A study from the USA evaluated 52 subjects with chronic functional bloating using a wireless motility capsule and LHBT. SIBO as defined by abnormal LHBT was found in 40% of cases and delayed GI motility was evidenced in 54% of cases [111]. In a recent study on functional bloating from Korea, SIBO was detected in 42.8% of patients, and SIBO was associated with significant dysbiosis as detected on fecal microbiota composition analysis by 16S ribosomal RNA amplification and sequencing [112]. A study from the USA evaluated 139 patients with unexplained gas, bloating, and diarrhea with duodenal aspirate culture and GHBT for the presence of SIBO. GHBT was positive in 27.3% of patients while culture was positive in 44.6% of subjects [16].
A case-control study from Brazil [113] evaluated 23 patients with functional dyspepsia and 11 controls for the presence of SIBO using LHBT. SIBO as defined by positive LHBT was observed in 56.5% of functional dyspepsia as compared to 0% in controls. The frequency of SIBO in functional dyspepsia subjects taking PPI was 75%. A study from Japan [114] evaluated the prevalence of SIBO by GHBT in patients with refractory FGIDs. Of the 38 FGID patients enrolled, 11 had functional dyspepsia, 10 had IBS, and 17 had IBS- functional dyspepsia overlap. SIBO was detected in overall 5.3% of the patients.
The FGID, which has attracted maximum global attention during the last two decades in terms of association with SIBO, is undoubtedly IBS. There are several seminal publications and exciting high-quality research in this particular arena, so much so that several meta-analyses are now available on this issue. Two most recent meta-analyses in the year 2020 highlighted some very interesting messages. The meta-analysis by Shah et al. [52] emphasized extensive variability in the prevalence of SIBO in IBS depending on the type of diagnostic technique used. Breath testing gave a yield of 35.5%, while culture gave a prevalence of 13.9% and 33.5% depending upon the use of a cut-off threshold of 105 CFU/mL or 103 CFU/mL, respectively. The meta-analysis by Ghoshal et al. [53] reported an overall prevalence of SIBO in IBS as 36.7%. Subjects with IBS were 2.6 and 8.3 times more likely to have SIBO as compared with healthy subjects using GHBT and upper gut aspirate culture, respectively. Subjects with IBS-D were more likely to have SIBO as per this meta-analysis. Interestingly, a recent study comparing the effect of antimicrobial therapy in patients with functional dyspepsia with and without concomitant IBS revealed that the improvement of dyspeptic symptoms was unrelated to the concomitant IBS symptoms suggesting that SIBO indeed is the cause of at least a subgroup of functional dyspepsia patients [115].
Statement 11: Fat in the small bowel induces ileal brake, which potentially promotes SIBO that may further lead to fat malabsorption.
Voting summary: Accepted completely 100%.
Level of evidence: II-2.
Grade of recommendation: B.
One of the postulated mechanisms of SIBO in patients with MAS (like tropical sprue, and celiac disease) is that intra-luminal unabsorbed fat induces slowing of proximal gut motility (also called ileal brake) through the liberation of hormones like peptide YY, neurotensin, and glucagon-like peptide [27, 78]. This ileal brake promotes SIBO, which may further promote fat malabsorption, resulting in a vicious cycle [27].
A landmark study from the UK [116] evaluated the possibility that malabsorbed fat in the ileum exerts an inhibitory feedback effect on intestinal motility. The investigators enrolled 24 healthy subjects and perfused the ileum with a fat-containing solution intended to produce ileal luminal fat levels similar to those in steatorrhea. Mean intestinal transit times through a saline-perfused jejunal segment were measured. After perfusion of fat into the ileum, mean transit times increased considerably. In addition, ileal fat perfusion resulted in a remarkable reduction of jejunal pressure wave activity. Ileal fat perfusion was also associated with a notable increase in plasma levels of neurotensin and enteroglucagon.
Another elegant study from the UK [117] evaluated the ileal brake effect of ileal infusion of partial digests of fat (oleic acid, triolein, medium-chain triglycerides). Marked reduction of jejunal pressure wave activity was observed after all three different lipid infusions. All three lipid infusions increased plasma levels of peptide YY (PYY), enteroglucagon, and neurotensin emphasizing the likely mechanism of the intestinal brake.
In the most comprehensive study to date on the issue of fat-induced ileal brake, Ghoshal et al. from India evaluated the effect of infusion of fat or placebo in the duodenum in patients with tropical sprue and healthy subjects on antroduodenal manometry, duodenocecal transit time (DCTT), and mediators of the ileal brake [28]. After fat infusion, proximal gut motility index was decreased as compared to fasting state in patients with tropical sprue, and DCTT was longer in patients as compared to healthy subjects. Fat infusion resulted in higher neurotensin and PYY levels in patients as compared to those in controls; and these levels were higher in patients with than those without SIBO.
Statement 12: Several systemic disorders (hepatic, pancreatic, others) are associated with SIBO.
Voting summary: Accepted completely 73.6%, accepted with some reservation 15.8%, accepted with major reservation 10.6%.
Level of evidence: II-2.
Grade of recommendation: A.
Though recent literature suggests an association of SIBO with several systemic disorders in terms of higher prevalence than in controls, this relationship with many of these systemic disorders is either multifactorial or unclear in terms of pathophysiology [1, 118]. Prominent among these disorders are hepatic diseases (cirrhosis, portal hypertension, NAFLD, and other CLDs), pancreatic disorders (acute and chronic pancreatitis), neurogenerative disorders (Parkinsonism, multiple sclerosis), cardiovascular disorders (coronary artery disease, and other atherosclerosis, deep venous thrombosis), end-stage renal disease, and other disorders like scleroderma, amyloidosis, human immunodeficiency virus infection, hypothyroidism, and diabetes mellitus [2, 19, 29, 39, 118]. Some of these associations are so well reported that even meta-analyses have been published regarding the relation of these disorders with SIBO.
SIBO has been frequently reported to be associated with CLD. Altered gut barrier function, reduced immunity, and impaired motility may contribute to the pathogenesis of SIBO in patients with CLD, especially those with cirrhosis and portal hypertension [39]. A recent meta-analysis by Shah et al. included 19 studies: 12 on cirrhosis, 5 on NAFLD/NASH, and 2 on CLD [49]. They reported a SIBO prevalence of 35.8% in studies that used breath tests, but the prevalence was as high as 68.3% in studies that used culture techniques. Pooled OR for the occurrence of SIBO was 7.15 as compared to controls. There was no significant difference between pooled prevalence in those with cirrhotic vs. non-cirrhotic CLD. Another meta-analysis from Russia [119] included 21 studies that involved 1264 patients with cirrhosis and 36 controls. The overall prevalence of SIBO in patients with cirrhosis and controls was 40.8% and 10.7%, respectively. Prevalence was 50.5% in those with decompensated cirrhosis. Pooled OR for the occurrence of SIBO was 6.83 as compared to controls. Predictors of SIBO in cirrhosis included the presence of minimal hepatic encephalopathy (MHE), ascites, spontaneous bacterial peritonitis (SBP), increased OCTT, and bacterial translocation. In a recent meta-analysis on the issue of SIBO in patients with NAFLD, Wijarnpreecha et al. evaluated 10 studies that included 1093 participants [120]. Significant association was found between NAFLD and SIBO with a pooled OR of 3.82.
Several studies have reported an increased frequency of SIBO in patients with chronic pancreatitis as compared to controls. The factors that may contribute to the pathogenesis of SIBO in these patients include impaired intestinal motility due to local inflammation, reduction in the secretion of pancreatic enzymes, effects of drugs like opioid analgesics, and in a few cases intestinal narrowing due to surrounding inflammatory process [39]. A meta-analysis from Italy evaluated 9 studies that included 336 patients [121]. They reported a pooled prevalence of SIBO as 36%. The pooled prevalence fell to 21.7% when studies using LHBT were excluded. Pooled OR for the occurrence of SIBO was 4.1. A recent meta-analysis from the USA included 13 studies with 518 patients with chronic pancreatitis [122]. They reported a pooled prevalence of SIBO as 38.6% with pooled OR of 5.58. A recent study by Chonchubhair el al. reported presence of diabetes, PPI use, alcoholic etiology, and use of pancreatic enzyme replacement therapy to be predictors of SIBO in patients with chronic pancreatitis [123]. One recent study from China reported SIBO to be associated with acute pancreatitis [124]. In this study, prevalence of SIBO in mild acute pancreatitis was lower (8.4%) than that in moderate (25.6%) or severe acute pancreatitis (25.9%). Also, frequency of SIBO was higher in those having organ dysfunction.
Statement 13: Lifestyle factors like chronic alcohol intake, and obesity may predispose to SIBO.
Voting summary: Accepted completely 31.6%, accepted with some reservation 52.6%, accepted with major reservation 15.8%.
Level of evidence: II-2.
Grade of recommendation: B.
Some lifestyle factors have been shown to increase the risk of occurrence of SIBO. One such factor is chronic alcohol intake. Chronic heavy alcohol intake has been reported to be associated with SIBO [125, 126]. This linkage can be explained by a variety of mechanisms as alcohol can modify intestinal defense through various mechanisms like direct toxic effect on the mucosal epithelium, decrease in the level of brush border enzymes, and induction of mucosal fibrosis [127,128,129]. Alcohol intake has also been shown to be associated with prolonged OCTT due to direct toxic damage of the intestinal smooth muscle [130]. Also, alcohol intake has been shown to adversely affect the intestinal mucosal immune system [131] predisposing to SIBO.
A study from Cleveland (USA) [132] evaluated the association between moderate alcohol consumption and SIBO. A total of 196 subjects were evaluated for SIBO using LHBT. Of them, 88 (45%) were alcohol consumers. Overall, the prevalence of positive LHBT was 47.4%. Among those who consumed alcohol, 58% had a positive LHBT, compared to 38.9% of abstainers (p = 0.008). There was a positive dose-response relationship between the amount of alcohol consumption and the positivity of LHBT [132].
With the background of the proposed metabolic role of gut microbiota in the pathogenesis of obesity [133, 134], several investigators tried to evaluate the relationship between obesity and SIBO. A few studies reported a positive relationship between these two entities [135,136,137,138] but one study from Korea noted an inverse relationship [139].
A recent meta-analysis evaluated the relationship between obesity and SIBO [140]. A total of five studies including 515 patients were included in this meta-analysis. The risk of SIBO among obese subjects was greater than in the non-obese but it did not reach statistical significance with a pooled OR of 2.08. When only Western studies were analyzed, the pooled OR became 3.41 and reached desired statistical significance.
Statement 14: Gut dysfunction in SIBO results from the altered luminal microenvironment, bacterial metabolites, altered motility and defense, and barrier dysfunction.
Voting summary: Accepted completely 63.1%, accepted with some reservation 21.1%, accepted with major reservation 15.8%.
Level of evidence: II-2.
Grade of recommendation: B.
Pathophysiology of gut dysfunction in SIBO is multifactorial [1, 29, 141]. Predominant mechanisms include gut inflammation, immune activation/dysfunction, altered motility, disturbed serotonergic activity, increased intestinal permeability, reduced luminal disaccharidase levels, deconjugation of bile salts, and nutrient and water malabsorption resulting in augmented intraluminal osmotic load [1, 142,143,144,145]. The metabolomic profile of intestinal contents in SIBO differs substantially from that in controls. An elegant study from India [146] did a H1-NMR spectroscopic analysis of the upper-gut aspirate in 31 patients with MAS with and without SIBO, and 10 control subjects. In comparison to control subjects, the patients with MAS had greater quantities of acetate, lactate, formate, and total bile acids/cholesterol in gut aspirate. Furthermore, MAS patients with SIBO had higher quantities of acetate, lactate, formate, and unconjugated bile acids than those without SIBO. In patients with MAS, the level of acetate correlated with the grade of SIBO, while the level of unconjugated bile salts correlated with the severity of steatorrhea, thereby indicating that bacteria in the small intestine generate acetate and induce deconjugation of bile salts, which in turn cause fat malabsorption resulting in steatorrhea.
Fat malabsorption in SIBO may also be associated with impaired absorption of lipid-soluble vitamins. The bacterial population in SIBO may induce vitamin B12 deficiency using ingested B12 to generate inactive cobamides, which in turn with dietary B12 intestinal binding sites, results in reduced B12 absorption and its deficiency [141, 147]. SIBO induces carbohydrate malabsorption by reducing enterocyte brush border disaccharidase activity [142]. Bacterial fermentation of carbohydrates into gas [145] results in bloating, distension, and abdominal discomfort. Protein malabsorption can result from multiple factors like decreased absorption of amino acids and peptides; decreased level of enterokinase, which may hamper activation of pancreatic proteases; and protein-losing enteropathy [148,149,150]. Increased intestinal permeability in SIBO patients has been shown to facilitate malabsorption and diarrhea [151]. This leaky gut in SIBO may contribute to mucosal immune activation resulting from the entry of luminal antigens into the mucosa [1, 152, 153]. Bacteria in SIBO may produce certain compounds that may have systemic effects. These agents include D-lactate, ammonia, ethanol, bacterial peptidoglycans, and endotoxins [29, 154]. These compounds are clinically relevant in the context of SIBO associated with short bowel syndrome [155]. A recent study from the USA described a syndrome of brain fogginess (BF) possibly related to SIBO and D-lactic acidosis in a cohort without short bowel syndrome patients [156].
Statement 15: Small Intestinal biopsy changes in patients with SIBO are non-specific.
Voting summary: Accepted completely 100%.
Level of evidence: II-2.
Grade of recommendation: C.
Morphologic changes associated with SIBO have not been studied extensively. Small intestinal histology in patients with SIBO may be either normal or may show subtle or non-specific abnormalities [141]. Since mucosal histology is quite variable, it is virtually impossible to diagnose SIBO conclusively on endoscopic biopsy [157].
An elegant experimental study using electron microscopy reported subtle enterocyte abnormalities like mitochondrial swelling and vacuolization of the microvillus membranes [158]. A recent experimental study in a post-infection IBS model of mice found a reduced density of interstitial cells of Cajal (ICC) and increased intra-epithelial lymphocyte (IEL) count in the ileum to be associated with the development of SIBO [159].
A study from Australia reported increased IEL and elevated IgA-containing plasma cells in the lamina propria as the standout features in the histology of small bowel in subjects with SIBO [160]. A study from the USA found that villous blunting was the only feature, which was more common in SIBO than in controls but more than half of biopsies from SIBO patients were histologically unremarkable [161].
Statement 16: Methane-producing bacteria slow gut transit and cause constipation.
Voting summary: Accepted completely 68.4%, accepted with some reservation 26.3%, accepted with major reservation 5.3%.
Level of evidence: II-2.
Grade of recommendation: A.
About 30% to 62% of healthy human beings have methane-producing bacteria in their gut [162]. Experimental and clinical studies indicate that methane inhibits GI motility and hence its concentration may inversely correlate with stool form and frequency [163, 164]. Also, the degree of breath methane production has been shown to correlate with the severity of constipation [163]. Moreover, therapy with antibiotics targeted to gut methanogens has been shown to improve intestinal transit as well as constipation [165]. A meta-analysis [166] established a significant association between methane on a breath test and constipation and also an association between methane and delayed transit. More recently, a systematic review and meta-analysis reported an association of methane positivity on breath testing with constipation-predominant IBS and inversely with IBD [167]. The North American Consensus defined a cut-off for high breath methane levels to be ≥10 parts per million (PPM) [18]. Excess methane production in the human gut is predominantly contributed by Methanobrevibacter smithii, which is a single-celled microorganism from the Archaea domain [168]. Since subjects with high breath methane may also have increased methanogen levels in stools, experts from North America have recently suggested a new terminology called “intestinal methanogen overgrowth (IMO)” [19].
There are limited studies on the role of methane in causing or promoting constipation. An experimental study from Korea [169] reported that infusion of methane significantly decreased peristaltic velocity and increased contraction amplitude of guinea pig ileum. Another interesting study from Korea [170] found breath methane positivity to be more frequent in patients with slow transit constipation than those with normal transit constipation and healthy subjects.
A landmark Indian study [171] found a greater number of Methanobrevibacter smithii in fecal samples of patients with IBS especially constipation-predominant IBS in comparison to healthy subjects. There was an inverse correlation between the copy number and the stool frequency, and the copy number was greater among methane producers than non-methane producers. The degree of breath methane correlated with the M. smithii copy number among methane producers. A recently published randomized controlled trial from India showed that reduction of breath methane using rifaximin shortens colonic transit time and improves constipation [172].
A recent meta-analysis on SIBO in IBS reported that methane-positive breath tests were more prevalent in IBS constipation than IBS diarrhea with an OR of 2.3 [52].
Statement 17: Small intestinal fungal overgrowth (SIFO) may coexist in patients with SIBO.
Voting summary: Accepted completely 57.9%, accepted with some reservation 26.2%, accepted with major reservation 5.3%, rejected with reservation 10.6%.
Level of evidence: II-2.
Grade of recommendation: B.
SIFO is an emerging entity. Very little published literature is available on this condition. Since risk factors for SIBO and SIFO are similar, both may coexist. Since normal intestinal propulsion helps to cleanse the intestine of bacteria and other microbes, intestinal stasis/dysmotility/post-surgical blind loop may predispose to SIBO as well as SIFO. In a study from the USA [63], GI dysmotility and PPI use were found to be independent predictors of SIBO or SIFO in patients with unexplained GI symptoms. Out of 150 evaluated patients, 94 (63%) had an overgrowth of whom 38/94 (40%) had SIBO, 24/94 (26%) had SIFO, and 32/94 (34%) had mixed SIFO/SIBO. Candida species were documented in those with SIFO. GI dysmotility was documented in 80/150 (53%) and PPI use was present in 65/150 (43%).
In another study from the USA [45], patients with unexplained abdominal pain, gas, bloating, and diarrhea, and without colectomy (controls), and with colectomy were evaluated for SIBO and SIFO. The severity of GI symptoms was greater in the post-colectomy group. Prevalence of SIBO (62% vs. 32%) SIFO/SIFO (24% vs. 8%) was also significantly higher in the post-colectomy group, indicating that colectomy predisposes to SIBO/SIFO and that these two may coexist.
Clinical manifestations, differential diagnosis, and predictors
Statement 18: Clinical presentation may vary according to the severity of involvement and the underlying disease-causing SIBO.
Voting summary: Accepted completely 78.9%, accepted with some reservation 10.5%, accepted with major reservation 10.6%.
Level of evidence: II-2.
Grade of recommendation: B.
SIBO can present with a wide range of symptoms, many of which are non-specific and can occur in other GI disorders. Clinical symptoms may vary depending upon the severity of involvement and also the primary disease-causing bacterial overgrowth [1, 29]. The symptoms may occur due to malabsorption of nutrients, altered gut permeability, and effects of gut inflammation and immune activation. Subjects with SIBO may also be asymptomatic as illustrated in several case-control studies that have enrolled apparently healthy subjects as controls [29, 30].
Abdominal pain, bloating, gas, distension, flatulence, and diarrhea are the most common symptoms [16, 19, 63]. But no particular symptom can be specifically ascribed to SIBO. Symptoms often overlap with those of FGIDs. In severe cases, there may be additional clinical features like steatorrhea, peripheral edema, anemia, weight loss, deficiencies of fat- or water-soluble vitamins, especially vitamin D and B12, other micronutrient deficiencies, and failure to thrive in the pediatric population [1]. In addition to these symptoms, there may be apparent clinical features of the underlying disease predisposing to SIBO, like scleroderma, hypothyroidism, IBD, chronic pancreatitis, celiac disease, cirrhosis, and Parkinsonism [1, 19].
There may be additional systemic symptoms like fatigue, bodyache, poor concentration, and neurological symptoms [1, 19, 29]. Recently, a syndrome of BF, gas, and bloating was proposed as one of the presentations of SIBO [156, 173, 174]. D-lactic acidosis was more prevalent in BF compared to the non-BF group. None of these patients had short bowel, which is classically the situation predisposing to lactic acidosis and BF-like symptoms [29]. One recent study also suggested an association of SIBO with hyperammonemia encephalopathy [175].
Statement 19: Symptomatic patients with SIBO do not necessarily have nutrient deficiencies.
Voting summary: Accepted completely 84.2%, accepted with some reservation 15.8%.
Level of evidence: II-2.
Grade of recommendation: B.
Patients with SIBO generally have only mild non-specific symptoms like bloating, flatulence, abdominal discomfort, or distension with no sign of any nutrient deficit [16, 63]. This is the most usual clinical scenario of SIBO wherein the symptom profile mimics that of common FGIDs like IBS [21]. In contrast to this milder clinical profile, features of nutrient malabsorption and deficiencies like steatorrhea, anemia, sarcopenia, edema of lower extremities, neuropathy, metabolic bone disease, or tetany may be seen in more severe cases like the ones associated with scleroderma, jejuno-colonic fistulae, CIPO, intestinal strictures, or postsurgical blind loops [10, 19, 29, 71, 176].
The symptoms related to nutritional consequences of intestinal malabsorption occur over a substantial period of time and may result in significant malnutrition, weight loss, and growth failure (in children) [1]. Anemia in SIBO can be multifactorial. Iron, as well as vitamin B12, may be deficient due to malabsorption as well as sub-optimal intake due to associated anorexia or nausea [177]. Since iron deficiency causes microcytic anemia while B12 deficiency results in macrocytic anemia, the peripheral smear in SIBO subjects may show a dimorphic picture.
Statement 20: Physical examination may reveal features of predisposing conditions as well as sequelae of SIBO but it may also be entirely normal.
Voting summary: Accepted completely 84.2%, accepted with some reservation 15.8%
Level of evidence: II-2.
Grade of recommendation: B.
Physical examination findings in SIBO are non-specific [29]. It may be entirely normal in milder cases. The presence or absence of physical signs depends not only on the severity of SIBO but also on the type of primary underlying disease. The genesis of the physical signs may be related to malabsorbed nutrients, nutritional consequences of malabsorption, changes in gut permeability, systemic effects of intestinal inflammation, and immune activation resulting from pathologic bacterial fermentation in the small intestine [1, 19].
In severe cases, there may be features of malnutrition or malabsorption like anemia, pedal edema, sarcopenia, growth failure (in children), features of fat-soluble vitamin deficiency, tetany, polyneuropathy/other features of vitamin B12 deficiency, and features of other micronutrient deficiency [1]. Such florid signs are usually seen with certain particular causes of SIBO like a post-surgical blind loop, entero-colonic fistulae, or scleroderma [19, 71]. In addition to these features, the physical examination may reveal features of the associated/underlying disorders like hypothyroidism, CLD, Parkinsonism, scleroderma, rosacea, or scars of previous abdominal surgery if any.
Statement 21: Differential diagnosis may range from functional GI disorders in those with a milder clinical presentation to malabsorption syndrome in severe cases.
Voting summary: Accepted completely 94.7%, accepted with some reservation 5.3%.
Level of evidence: III.
Grade of recommendation: B.
The spectrum of differential diagnosis of SIBO is quite extensive since its clinical profile varies widely from asymptomatic or minimally symptomatic to full-blown features of malabsorption and malnutrition [19, 29]. The milder clinical version consists of non-specific symptoms like bloating, flatulence, distension, altered bowel habits, and abdominal discomfort or pain, which may mimic common FGIDs like IBS, dyspepsia, and functional bloating [16, 63]. The other extreme of the clinical scenario is epitomized by various features of MAS as can be seen with other causes of MAS like tropical sprue, celiac disease, hypogammaglobinemia, human immunodeficiency virus (HIV) infection, giardiasis, and strongyloidiasis [1, 19, 27, 178, 179]. In a study from India on 50 patients with MAS, SIBO was present in 42% cases [26]. Another study from the same center evaluated 13 patients with tropical sprue and found SIBO in 30.8% of these subjects [27]. A recent meta-analysis reported an overall pooled SIBO prevalence of 20% in patients with celiac disease which is an important cause of malabsorption all across the globe [180].
The features of malabsorption in SIBO may include steatorrhea, anemia, hypoproteinemia, sarcopenia, peripheral edema, weight loss or failure to thrive, and features of water- and fat-soluble vitamins especially vitamin B12 and vitamin D [1, 19, 29]. The patients with severe SIBO are usually associated with predisposing anatomic abnormalities like entero-colonic fistula, post-surgical blind loop, intestinal strictures, and small bowel diverticulosis; or major gut motility dysfunction like scleroderma or CIPO [71, 141]. Hence, SIBO must be considered in the differential diagnosis of any patient with malabsorption associated with a predisposing structural or functional cause. Recently, a few authors have suggested SIBO to be a possible etiopathogenetic link between post-infection IBS and post-infectious malabsorption syndrome (PI-MAS), traditionally known as tropical sprue [181].
Statement 22: Clinical predictors of SIBO in patients with IBS include female gender, old age, marked bloating and flatulence, long-term treatment with PPI, narcotic intake, low hemoglobin, and diarrheal subtype of IBS.
Voting summary: Accepted completely 68.4%, accepted with some reservation 26.3%, accepted with major reservation 5.3%.
Level of evidence: II-2.
Grade of recommendation: B.
SIBO in IBS is one of the most sought-after themes among FGID researchers during the last two decades [11, 19]. There are several publications including meta-analysis to suggest an association between these two entities; however, the puzzle is yet to be fully solved and several key aspects of this association need to be explored further [36, 51,52,53]. One key area of interest has been to explore the clinical predictors of SIBO in patients with IBS. The potential predictors include female gender, elderly age, long-term therapy with PPIs, narcotic intake, low hemoglobin, the diarrheal subtype of IBS, and presence of marked bloating or flatulence [1].
In a study from the USA, Reddymassu et al. evaluated 98 subjects with IBS for SIBO using GHBT [34]. A positive GHBT result was found to be more likely in patients with age >55 years and females (OR 4.0). Predominant bowel patterns or concurrent use of tegaserod, PPIs, or opiate analgesics were not found to be predictors of SIBO in this study.
In a study from India, Ghoshal et al. used GHBT to study SIBO in patients with IBS, those with chronic non-specific diarrhea (CNSD), and healthy controls (HC) [38]. Prevalence of SIBO in CNSD, IBS, and HC was 21.9%, 8.5%, and 2%, respectively. Older age and low hemoglobin were found to be predictors of SIBO in these patients.
A study from Mayo Clinic (USA) evaluated clinical predictors of SIBO by duodenal aspirate culture in the study population, which included IBS as well as non-IBS subjects [35]. Older age, narcotic use, and steatorrhea were associated with SIBO. Use of PPI was associated with bacterial overgrowth just falling short of meeting the criteria for SIBO.
In another study from India, Sachdeva et al. used GHBT to evaluate SIBO in patients with IBS and healthy controls [182]. SIBO was found to be more frequent in patients with IBS than HC (23.7% vs. 2.7%). Female gender, bloating, and IBS-D subtype were found to be predictors of SIBO in patients with IBS.
In one of the comprehensive studies published concerning SIBO in IBS, Ghoshal et al. used GHBT and LHBT as well as upper gut culture to evaluate SIBO in 80 patients with IBS [13]. A total of 15/80 (19%) patients were found to be having SIBO (bacterial counts ≥105 CFU/mL on culture). SIBO was more common in IBS-D than in other IBS subtypes.
In a vital meta-analysis, Chen et al. analyzed 50 studies that have evaluated SIBO in IBS [36]. Overall pooled prevalence of SIBO in IBS was 38%, which was significantly higher than in healthy controls. Among patients with IBS, older age, female gender, and IBS-D subtype, but not PPI use, were associated with SIBO.
In a recent meta-analysis, Shah et al. evaluated 25 case-control studies with 3192 patients with IBS and 3320 controls [52]. Prevalence of SIBO in patients with IBS was 35.5% using hydrogen breath tests, 33.5% with culture using ≥103 CFU/mL as cut-off, and 13.9% with culture cut-off of ≥105 CFU/mL. OR for SIBO in IBS-D compared with IBS-C was 1.86. Use of PPI was not found to be associated with SIBO in patients with IBS (OR = 0.8).
In the most recent analysis, Ghoshal et al. evaluated 47 studies that have evaluated SIBO in IBS [53]. Overall pooled prevalence of SIBO in IBS was 36.7%. Patients with IBS-D were more likely to have SIBO as compared to other IBS subtypes.
Investigations and treatment
Statement 23: The currently used tests for SIBO include GHBT and LHBT, and quantitative culture of upper gut aspirate.
Voting summary: Accepted completely 89.5%, accepted with some reservation 10.5%
Level of evidence: II-2.
Grade of recommendation: A.
Though quantitative upper gut aspirate culture is the current gold standard for the diagnosis of SIBO despite its limitation because only 30% of the gut bacteria can be cultured, hydrogen breath tests are popular due to their non-invasiveness [1]. Quantitative upper gut aspirate culture is better performed with a double-lumen catheter assembly that prevents contamination with nasopharyngeal flora (Ghoshal Gut Microbiota Sampler [GMS™]; patent application no. 20171104037). A cut-off of ≥105 colony-forming unit (CFU)/mL is conventionally considered as diagnostic of SIBO [1, 183]. However, recently, even a lower level of bacterial overgrowth in the upper gut (≥103 CFU/mL) has been found clinically important and hence, termed as low-grade SIBO [17]. In a North American consensus, a colony count ≥103 CFU/mL has been considered diagnostic of SIBO. Even though only 30% of gut bacteria are cultured, the quantitative upper gut aspirate is considered the gold standard for diagnosis of SIBO. However, considering its invasiveness and need for considerable microbiological support, hydrogen breath tests are more popular in clinical practice. Recently, capsule measuring intraluminal hydrogen gas is being evaluated for diagnosis of SIBO and is being shown to be superior to breath hydrogen measurement [184].
Statement 24: Among non-invasive tests, GHBT is preferred over LHBT.
Voting summary: Accepted completely 78.9%, accepted with some reservation 21.1%.
Level of evidence: II-2.
Grade of recommendation: A.
The literature on this statement is reviewed along with that on statement 25.
Statement 25: Better tests for SIBO are needed as the culture of gut aspirate is invasive and more than 70% of microbes are non-culturable and the hydrogen breath tests are either insensitive or non-specific.
Voting summary: Accepted completely 89.4%, accepted with some reservation 5.3%, rejected completely 5.3%.
Level of evidence: II-1.
Grade of recommendation: A.
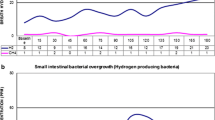
Two commonly performed hydrogen breath tests include GHBT and LHBT. In GHBT and LHBT, fasting breath hydrogen and methane are estimated 3–4 times using a commercially available gas chromatograph [185]. In many machines, the value of carbon-di-oxide is also recorded, which is used as a correction factor for the adequacy of breath collection. Subsequently, the subject ingests either 75–100 g glucose dissolved in 150–200 mL water or 10 g lactulose contained in a 15-mL solution. End-expiratory breath hydrogen/methane is estimated every 10–15 min for 2–4 h. A rise in breath hydrogen 12 PPM above the average basal value following glucose ingestion is considered diagnostic of SIBO. The conventional criterion for diagnosis of SIBO on LHBT includes a double peak in breath hydrogen, the earlier one produced by the overgrown bacteria in the small bowel and the later one from the colon. Of late, an early-peak criterion for the diagnosis of SIBO has been proposed; it suggests that if a peak in breath hydrogen occurs within 90 minutes after lactulose ingestion, it is diagnostic of SIBO. However, this is based on the presumption that mouth-to-cecum transit time is always more than 90 minutes although several studies showed that mouth-to-cecum transit time may be much shorter [1, 48, 185]. Moreover, a few studies showed that when lactulose was co-administered with a radionuclide, in many subjects though peak the hydrogen occurred within 90 min after ingestion, the radionuclide was seen to have reached cecum. Accordingly, the early peak criterion to diagnose SIBO is not acceptable. In a recent meta-analysis, the sensitivity and specificity of GHBT were higher than LHBT (Fig. 1) [186]. Hence, GHBT should be preferred over LHBT for making the diagnosis of SIBO non-invasively. However, it is important to note that though the specificity of GHBT may reach 80% to 100%, its sensitivity has been reported to be as low as 30% to 40%; hence, though a positive GHBT is quite confirmatory of the presence of SIBO, a negative test may not mean the absence of it.
Forest plots of pooled sensitivity (A) and specificity (B) of glucose hydrogen breath test (GHBT); and pooled sensitivity (C) and specificity (D) of lactulose hydrogen breath test (LHBT). Reproduced from Losurdo et. al. [186]. It is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited
Statement 26: The role of newer diagnostic methods like culturomics, metabolomics, D-xylose, and 13C-based breath tests needs further evaluation.
Voting summary: Accepted completely 78.9%, accepted with some reservation 15.8%, rejected completely 5.3%.
Level of evidence: III.
Grade of recommendation: B.
In view of the low sensitivity and specificity of hydrogen breath tests, the invasive nature of quantitative upper gut aspirate culture, and the inability to culture as high as 70% gut bacteria, a search for better tests for the diagnosis of SIBO continues. D-xylose, a pentose sugar, is absorbed predominantly in the upper gut. D-xylose does not produce hydrogen due to bacterial fermentation as this sugar does not reach the large bowel in healthy subjects. Overgrown bacteria in the proximal gut in SIBO patients produce hydrogen by fermentation of D-xylose that is estimated in the exhaled breath. However, data on D-xylose breath tests are uncommonly reported. In a study, 513 (55%) of 932 consecutive subjects had SIBO on D-xylose breath test [187]. This was a retrospective study, and no gold standard method was used to verify the diagnosis of SIBO. Because bacteria in patients with SIBO deconjugate bile acids, the 13C or 14C glycocholic acid breath test has also been used for the diagnosis of SIBO [188]. This test involves ingestion of the 14C or 13C glycocholic acids, which are bile acids, and detection of 14CO2 or 13CO2 in the breath, which are expected to be high in SIBO patients [188]. However, data on the clinical utility of 13C or 14C glycocholic acid breath tests are scanty. In an earlier study, the lactose-13C ureide breath test was compared with GHBT, considering jejunal aspirate culture as the gold standard [189]. It had a sensitivity of 66.7% and a specificity of 100%, which were higher than GHBT.
Statement 27: Besides definitive tests for establishing SIBO, other ancillary tests are needed: (a) to investigate the underlying cause and (b) to evaluate for the sequelae.
Voting summary: Accepted completely 84.2%, accepted with some reservation 15.8%.
Level of evidence: III.
Grade of recommendation: B.
Table 2 lists the causes of SIBO. It is important to diagnose the causes of SIBO during careful history taking, physical examination, and appropriate investigations, as some of these disorders are potentially treatable. Treatment of the primary disorders may help to eradicate SIBO and prevent its recurrence and hence, finding out the underlying causes and mechanisms may have therapeutic implications. For example, prokinetic treatment delayed recurrence of SIBO after successful treatment with antibiotics in a retrospective study on patients with IBS with SIBO [190]. In another study on 15 patients with HIV-associated autonomic neuropathy with SIBO, pyridostigmine treatment alone resulted in the eradication of SIBO in 87% of patients during 2-month follow-up [191].
Statement 28: Key components of management of SIBO include the followings: (a) treatment of predisposing conditions, (b) appropriate antibiotics, and (c) correction of nutritional deficiencies.
Voting summary: Accepted completely 89.5%, accepted with some reservation 10.5%.
Level of evidence: I.
Grade of recommendation: A.
The literature on this statement is reviewed along with that on statement 29.
Statement 29: Though small bowel bacteria in patients with SIBO are sensitive in vitro to several antibiotics, rifaximin may be preferred due to its broad spectrum and lack of systemic adverse effects.
Voting summary: Accepted completely 78.9%, accepted with some reservation 10.5%, Accepted with major reservation 10.6%.
Level of evidence: I.
Grade of recommendation: A.
Treatment of primary disorders predisposing to the development of SIBO, if any (Table 2), not only helps to alleviate the condition but also prevents its recurrence following successful treatment. Hence, attention to detecting these predisposing conditions and their appropriate treatment is essential.
Though several methods to manage the SIBO may be potentially useful, the broad-spectrum gut-specific antibiotic rifaximin is the most studied drug. Figure 2 presents a simplified algorithm for diagnosis and pharmacotherapy of SIBO. Several other antibiotics have also been tried in the treatment of SIBO such as norfloxacin, ciprofloxacin, tetracycline, doxycycline, neomycin, co-trimoxazole, ampicillin-clavulanic acids, and metronidazole. In a study from India, the bacterial populations causing SIBO were found to be more often sensitive to fluoroquinolones than to other antibiotics [26]. However, rifaximin was not evaluated in that study.
Rifaximin (C43H51N3O11), a structural analogue of rifampin that inhibits bacterial RNA synthesis by binding to the DNA-dependent RNA polymerase, is a non-absorbable antimicrobial drug effective against both aerobic and anaerobic Gram-positive as well as Gram-negative bacteria [1]. In a meta-analysis of 32 studies including 1331 patients with SIBO, frequency of eradication SIBO with rifaximin treatment by intention-to-treat analysis was 70.8% (95% CI: 61.4–78.2; I2 to 89.4%) and by per-protocol analysis 72.9% (95% CI: 65.5–79.8; I2 to 87.5%) [192]. In another meta-analysis of five non-randomized studies on patients with SSc including 78 patients with SIBO, though the antibiotics were found to eradicate SIBO, the probiotics and prokinetics were of uncertain efficacy [193].
IBS, a common disorder of gut-brain interaction, is known to be associated with SIBO [53]. The popularity of rifaximin among gastroenterologists and physicians was brought in by a RCT of this drug in the management of IBS that showed rifaximin to be 41% effective to relieve the symptoms of IBS in contrast to 31% efficacy of placebo that led to the approval of the drug in the treatment of non-constipated IBS patients by the Food and Drug Administration of USA [194]. However, that study did not evaluate for SIBO in IBS patients and hence, treatment response in relation to the presence and absence of SIBO was not known. In a study, it was found that the bacterial populations causing SIBO are more often responsive to fluoroquinolones than to other antibiotics [26].
A meta-analysis of eight studies showed that the overall normalization rate of breath test with rifaximin was 49.5% (95% CI, 44.0 to 55.1). Antibiotics like metronidazole, neomycin, and ciprofloxacin (four studies) showed a higher response rate than placebo in normalizing breath tests with an OR of 2.55 (95% CI, 1.29 to 5.04) [195].
Currently, most patients with SIBO may be diagnosed much before severe nutritional deficiencies develop. However, nutritional deficiencies, if present, must be identified and treated appropriately. Whereas vitamin B12 deficiency is common among these patients, serum folate levels may be normal or high due to the bioavailability of bacterially synthesized folic acid except in patients with tropical sprue who often have folate deficiency [179]. Vitamin B12 should be supplemented in patients with SIBO parenterally.
Statement 30: Patients with IBS with SIBO show a better response to antibiotics as compared to those without SIBO.
Voting summary: Accepted completely 100%.
Level of evidence: I
Grade of recommendation: A
In a proof of concept double-blind randomized-controlled trial, one of the authors found that SIBO was highly reliable to predict response to treatment with antibiotics among IBS patients [14]. In this study, 80 patients with IBS diagnosed by Rome III criteria were evaluated for SIBO (≥105 CFU/mL) by upper gut aspirate culture; patients with and without SIBO were separately randomized (stratified randomization) either to norfloxacin 400 mg twice daily and placebo. 87.5% of 15 patients with SIBO responded to treatment at 1 month in contrast to 25% of 65 without SIBO. This study [14] evaluated norfloxacin instead of rifaximin as the latter drug was not available in India at the time of study. Two subsequent studies, one from China [196] and another from the USA [197], further reproduced similar observations. However, both these studies used hydrogen breath tests to diagnose SIBO. More studies are needed on this issue.
Statement 31: Patients with slow transit chronic constipation associated with high breath methane on LHBT may respond to treatment with rifaximin.
Voting summary: Accepted completely 57.9%, accepted with some reservation 31.6%, accepted with major reservation 10.6%.
Level of evidence: I.
Grade of recommendation: B.
Several studies and meta-analysis showed that excess breath methane on LHBT is associated with chronic constipation and slow colon transit [166]. Three RCT, two from the USA [165, 198] and one from India [172], showed that reduction in breath methane by treatment with antibiotics such as rifaximin, neomycin, or a combination of these two was associated with improvement of constipation. One study also showed that reduction in breath methane by rifaximin treatment was associated with acceleration of colon transit [172]. More studies are needed on this issue.
Statement 32: SIBO is known to recur following successful treatment with rifaximin.
Voting summary: Accepted completely 78.9%, accepted with some reservation 21.1%
Level of evidence: II-2.
Grade of recommendation: A.
The literature on this statement is reviewed along with that on statement 33.
Statement 33: Predictors of recurrence of SIBO include older age, long-term treatment with PPIs, prior abdominal surgery, and persistence of predisposing condition.
Voting summary: Accepted completely 68.4%, accepted with some reservation 31.6%.
Level of evidence: II-2.
Grade of recommendation: B.
SIBO often recurs following its successful treatment, particularly in absence of a cause or in presence of a treatable predisposing condition that has not been treated. In an Italian study, 12.6%, 27.5%, and 43.7% of 80 patients with SIBO successfully treated with rifaximin had a recurrence of it on GHBT at 3-, 6-, and 9-month follow-up, respectively [199]. Older age, history of appendectomy, and long-term PPI intake were associated with recurrence during follow-up [199]. Recurrence of SIBO was often associated with recurrence of GI symptoms. In an Indian study, of 78 patients with SIBO diagnosed by GHBT and successfully treated with rifaximin, 18% and 43% had recurrence at 3 and 6 months, respectively [200].
Statement 34: Drugs promoting GI motility and treating the predisposing conditions may prevent the recurrence of SIBO.
Voting summary: Accepted completely 31.6%, accepted with some reservation 52.6%, accepted with major reservation 15.8%.
Level of evidence: III.
Grade of recommendation: C.
Since SIBO recurrence after successful treatment is quite high (almost 40% during 6 months) [200], the prevention of recurrence is of utmost importance. Since small bowel stasis predisposes to SIBO, increasing gut motility should prevent SIBO recurrence. In a retrospective study, recurrence of symptoms presumed to result from SIBO was delayed among patients treated with tegaserod or erythromycin than those without these drugs [190]. In another study, 15 patients with well-controlled HIV infection with autonomic neuropathy and SIBO have treated with pyridostigmine 30 mg thrice daily for 2 months. GHBT, gastric emptying (GE), plasma sCD14 (a marker of macrophage activation and indirect measure of translocation), interleukin (IL)-6, tumor necrosis factor-alpha (TNFα), and GI autonomic symptoms were compared before and after treatment [191] The authors found that SIBO improved in 13 (87%) patients; though GE did not improve, (TNF-α) and sCD14 levels declined by 12% and 19% (p<0.05 for both), and IL-6 or GI symptoms were comparable. Though this study was done on a small sample of patients, it did support the possibility of beneficial effect of improving gut motility on patients with SIBO.
Statement 35: Patients with recurrent symptoms following response to rifaximin respond to re-treatment with it.
Voting summary: Accepted completely 57.9%, accepted with some reservation 36.8%, accepted with major reservation 5.3%.
Level of evidence: II-1.
Grade of recommendation: B.
The data on retreatment of SIBO after recurrence following successful treatment is limited. No study has yet been reported on the efficacy of rifaximin in the re-treatment of recurrent SIBO. Since an earlier study showed that recurrent SIBO after successful treatment with rifaximin was associated with recurrence of symptoms [199], the TARGET 3 study that evaluated the efficacy of rifaximin for recurrent symptoms after successful rifaximin treatment for IBS may be considered as the evidence for the above statement. TARGET 3 study showed the safety and efficacy of re-treatment with rifaximin among 636 patients with IBS-D, who had previously responded to rifaximin but developed recurrent IBS symptoms over 18 weeks follow-up [201]. Another study showed that short-term re-treatment of these patients with rifaximin did not alter the stool microbial susceptibility to rifaximin, rifampin, and non-rifamycin antibiotics [202]. More studies are needed on this issue.
Statement 36: Probiotics may be of some benefit but more evidence is required.
Voting summary: Accepted completely 100%.
Level of evidence: II-2.
Grade of recommendation: B.
Despite the ability of probiotics to alter gut microbiota, their efficacy in treatment of SIBO is not encouraging. In a recent meta-analysis [203], of the five studies on probiotics including 266 patients with SIBO diagnosed using hydrogen breath test (three studies used probiotics only, and two with antibiotics), two studies comparing probiotics and placebo showed a positive result and the other one showed a negative result. Both the studies on probiotics and antibiotics showed that probiotic treatment in addition to antibiotics was superior. In another randomized crossover trial not included in this meta-analysis on 10 SIBO patients treated with norfloxacin, amoxicillin-clavulanic acid, and Saccharomyces boulardii over 7 days, though both the antibiotics conferred a positive result, S. boulardii was not useful [204]. More studies are needed on this issue.
Statement 37: The role of the low fermentable oligosaccharides, disaccharides, monosaccharides and polyols (FODMAP) diet in the management of SIBO needs further evaluation.
Voting summary: Accepted completely 63.2%, accepted with some reservation 26.2%, accepted with major reservation 5.3%, rejected with reservation 5.3%.
Level of evidence: III.
Grade of recommendation: C.
Since dietary modification is known to alter gut microbiota [205, 206], changing the diet may be a potential method to treat SIBO. However, the data on this are scanty. A single study evaluated the role of an elemental diet in patients with SIBO. The authors concluded that an elemental diet was effective in normalizing an abnormal LHBT in patients with IBS, who also experienced symptomatic improvement [207]. More studies are needed on this issue.
References
Ghoshal UC, Ghoshal U. Small intestinal bacterial overgrowth and other intestinal disorders. Gastroenterol Clin North Am. 2017;46:103–20.
Rao SSC, Bhagatwala J. Small intestinal bacterial overgrowth: Clinical features and therapeutic management. Clin Transl Gastroenterol. 2019;10:e00078.
Shah A, Morrison M, Holtmann GJ. Gastroduodenal “Dysbiosis”: a new clinical entity. Curr Treat Options Gastroenterol. 2018;16:591–604.
Shah A, Talley NJ, Koloski N, et al. Duodenal bacterial load as determined by quantitative polymerase chain reaction in asymptomatic controls, functional gastrointestinal disorders and inflammatory bowel disease. Aliment Pharmacol Ther. 2020;52:155–67.
Quigley EMM, Murray JA, Pimentel M. AGA clinical practice update on small intestinal bacterial overgrowth: Expert review. Gastroenterology. 2020;159:1526–32.
Murphy MK, Black NA, Lamping DL, et al. Consensus development methods, and their use in clinical guideline development. Health Technol Assess. 1998;2: i-iv, 1–88.
Atkins D, Best D, Briss PA, et al. Grading quality of evidence and strength of recommendations. BMJ. 2004;328:1490.
Toskes PP. Bacterial overgrowth of the gastrointestinal tract. Adv Intern Med. 1993;38:387–407.
Bauer TM, Steinbruckner B, Brinkmann FE, et al. Small intestinal bacterial overgrowth in patients with cirrhosis: prevalence and relation with spontaneous bacterial peritonitis. Am J Gastroenterol. 2001;96:2962–7.
Khoshini R, Dai SC, Lezcano S, Pimentel M. A systematic review of diagnostic tests for small intestinal bacterial overgrowth. Dig Dis Sci. 2008;53:1443–54.
Quigley EM, Abu-Shanab A. Small intestinal bacterial overgrowth. Infect Dis Clin North Am. 2010;24:943–59.
Gabrielli M, D'Angelo G, Di Rienzo T, et al. Diagnosis of small intestinal bacterial overgrowth in the clinical practice. Eur Rev Med Pharmacol Sci. 2013;17(Suppl 2):30–5.
Ghoshal UC, Srivastava D, Ghoshal U, Misra A. Breath tests in the diagnosis of small intestinal bacterial overgrowth in patients with irritable bowel syndrome in comparison with quantitative upper gut aspirate culture. Eur J Gastroenterol Hepatol. 2014;26:753–60.
Ghoshal UC, Srivastava D, Misra A, Ghoshal U. A proof-of-concept study showing antibiotics to be more effective in irritable bowel syndrome with than without small-intestinal bacterial overgrowth: a randomized, double-blind, placebo-controlled trial. Eur J Gastroenterol Hepatol. 2016;28:281–9.
Posserud I, Stotzer PO, Björnsson ES, et al. Small intestinal bacterial overgrowth in patients with irritable bowel syndrome. Gut. 2007;56:802–8.
Erdogan A, Rao SS, Gulley D, et al. Small intestinal bacterial overgrowth: duodenal aspiration vs glucose breath test. Neurogastroenterol Motil. 2015;27:481–9.
Ghoshal UC, Baba CS, Ghoshal U, et al. Low-grade small intestinal bacterial overgrowth is common in patients with nonalcoholic steatohepatitis on quantitative jejunal aspirate culture. Indian J Gastroenterol. 2017;36:390–9.
Rezaie A, Buresi M, Lembo A, et al. Hydrogen and methane-based breath testing in gastrointestinal disorders: the North American Consensus. Am J Gastroenterol. 2017;112:775–84.
Pimentel M, Saad RJ, Long MD, Rao SSC. ACG clinical guideline: Small intestinal bacterial overgrowth. Am J Gastroenterol. 2020;115:165–78.
Leite G, Morales W, Weitsman S, et al. The duodenal microbiome is altered in small intestinal bacterial overgrowth. PLoS One. 2020;15:e0234906.
Bohm M, Siwiec RM, Wo JM. Diagnosis and management of small intestinal bacterial overgrowth. Nutr Clin Pract. 2013;28:289–99.
Yang CY, Chang CS, Chen GH. Small-intestinal bacterial overgrowth in patients with liver cirrhosis, diagnosed with glucose H2 or CH4 breath tests. Scand J Gastroenterol. 1998;33:867–71.
Bouhnik Y, Alain S, Attar A, et al. Bacterial populations contaminating the upper gut in patients with small intestinal bacterial overgrowth syndrome. Am J Gastroenterol. 1999;94:1327–31.
Husebye E, Skar V, Hoverstad T, Melby K. Fasting hypochlorhydria with Gram positive gastric flora is highly prevalent in healthy old people. Gut. 1992;33:1331–7.
Fried M, Siegrist H, Frei R, et al. Duodenal bacterial overgrowth during treatment in outpatients with omeprazole. Gut. 1994;35:23–6.
Ghoshal U, Ghoshal UC, Ranjan P, et al. Spectrum and antibiotic sensitivity of bacteria contaminating the upper gut in patients with malabsorption syndrome from the tropics. BMC Gastroenterol. 2003;3:9.
Ghoshal UC, Ghoshal U, Ayyagari A, et al. Tropical sprue is associated with contamination of small bowel with aerobic bacteria and reversible prolongation of orocecal transit time. J Gastroenterol Hepatol. 2003;18:540–7.
Ghoshal UC, Kumar S, Misra A, Choudhuri G. Pathogenesis of tropical sprue: a pilot study of antroduodenal manometry, duodenocaecal transit time & fat-induced ileal brake. Indian J Med Res. 2013;137:63–72.
Bures J, Cyrany J, Kohoutova D, et al. Small intestinal bacterial overgrowth syndrome. World J Gastroenterol. 2010;16:2978–90.
Grace E, Shaw C, Whelan K, Andreyev HJ. Review article: small intestinal bacterial overgrowth--prevalence, clinical features, current and developing diagnostic tests, and treatment. Aliment Pharmacol Ther. 2013;38:674–88.
Lewis SJ, Potts LF, Malhotra R, Mountford R. Small bowel bacterial overgrowth in subjects living in residential care homes. Age Ageing. 1999;28:181–5.
Hellemans J, Joosten E, Ghoos Y, et al. Positive 14CO2 bile acid breath test in elderly people. Age Ageing. 1984;13:138–43.
Parlesak A, Klein B, Schecher K, et al. Prevalence of small bowel bacterial overgrowth and its association with nutrition intake in nonhospitalized older adults. J Am Geriatr Soc. 2003;51:768–73.
Reddymasu SC, Sostarich S, McCallum RW. Small intestinal bacterial overgrowth in irritable bowel syndrome: are there any predictors? BMC Gastroenterol. 2010;10:23.
Choung RS, Ruff KC, Malhotra A, et al. Clinical predictors of small intestinal bacterial overgrowth by duodenal aspirate culture. Aliment Pharmacol Ther. 2011;33:1059–67.
Chen B, Kim JJ, Zhang Y, et al. Prevalence and predictors of small intestinal bacterial overgrowth in irritable bowel syndrome: a systematic review and meta-analysis. J Gastroenterol. 2018;53:807–18.
Elphick DA, Chew TS, Higham SE, et al. Small bowel bacterial overgrowth in symptomatic older people: can it be diagnosed earlier? Gerontology. 2005;51:396–401.
Ghoshal UC, Kumar S, Mehrotra M, et al. Frequency of small intestinal bacterial overgrowth in patients with irritable bowel syndrome and chronic non-specific diarrhea. J Neurogastroenterol Motil. 2010;16:40–6.
Quigley EMM. The Spectrum of small intestinal bacterial overgrowth (SIBO). Curr Gastroenterol Rep. 2019;21:3.
Donowitz JR, Haque R, Kirkpatrick BD, et al. Small intestine bacterial overgrowth and environmental enteropathy in Bangladeshi children. mBio. 2016;7:e02102–15.
Verrecchia E, Sicignano LL, La Regina M, et al. Small intestinal bacterial overgrowth affects the responsiveness to colchicine in familial mediterranean fever. Mediators Inflamm. 2017;2017:7461426.
Fialho A, Fialho A, Schenone A, et al. Association between small intestinal bacterial overgrowth and deep vein thrombosis. Gastroenterol Rep (Oxf). 2016;4:299–303.
Enko D, Kriegshauser G. Functional 13C-urea and glucose hydrogen/methane breath tests reveal significant association of small intestinal bacterial overgrowth in individuals with active Helicobacter pylori infection. Clin Biochem. 2017;50:46–9.
Kim DB, Paik CN, Song DS, et al. The characteristics of small intestinal bacterial overgrowth in patients with gallstone diseases. J Gastroenterol Hepatol. 2018;33:1477–84.
Rao SSC, Tan G, Abdulla H, et al. Does colectomy predispose to small intestinal bacterial (SIBO) and fungal overgrowth (SIFO)? Clin Transl Gastroenterol. 2018;9:146.
Sung HJ, Paik CN, Chung WC, et al. Small intestinal bacterial overgrowth diagnosed by glucose hydrogen breath test in post-cholecystectomy patients. J Neurogastroenterol Motil. 2015;21:545–51.
Mouillot T, Rhyman N, Gauthier C, et al. Study of small intestinal bacterial overgrowth in a cohort of patients with abdominal symptoms who underwent bariatric surgery. Obes Surg. 2020;30:2331–7.
Ghoshal UC, Shukla R, Ghoshal U. Small intestinal bacterial overgrowth and irritable bowel syndrome: a bridge between functional organic dichotomy. Gut Liver. 2017;11:196–208.
Shah A, Shanahan E, Macdonald GA, et al. Systematic review and meta-analysis: Prevalence of small intestinal bacterial overgrowth in chronic liver disease. Semin Liver Dis. 2017;37:388–400.
Gurusamy SR, Shah A, Talley NJ, et al. Small intestinal bacterial overgrowth in functional dyspepsia: a systematic review and meta-analysis. Am J Gastroenterol. 2021;116:935–42.
Ford AC, Spiegel BM, Talley NJ, Moayyedi P. Small intestinal bacterial overgrowth in irritable bowel syndrome: systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2009;7:1279–86.
Shah A, Talley NJ, Jones M, et al. Small intestinal bacterial overgrowth in irritable bowel syndrome: a systematic review and meta-analysis of case-control studies. Am J Gastroenterol. 2020;115:190–201.
Ghoshal UC, Nehra A, Mathur A, Rai S. A meta-analysis on small intestinal bacterial overgrowth in patients with different subtypes of irritable bowel syndrome. J Gastroenterol Hepatol. 2020;35:922–31.
Shah A, Morrison M, Burger D, et al. Systematic review with meta-analysis: the prevalence of small intestinal bacterial overgrowth in inflammatory bowel disease. Aliment Pharmacol Ther. 2019;49:624–35.
Ghoshal UC, Yadav A, Fatima B, et al. Small intestinal bacterial overgrowth in patients with inflammatory bowel disease: a case-control study. Indian J Gastroenterol. 2022;41:96–103.
Giannella RA, Broitman SA, Zamcheck N. Gastric acid barrier to ingested microorganisms in man: studies in vivo and in vitro. Gut. 1972;13:251–6.
Kawaguchi H, Haruma K, Komoto K, et al. Helicobacter pylori infection is the major risk factor for atrophic gastritis. Am J Gastroenterol. 1996;91:959–62.
Paik CN, Choi MG, Lim CH, et al. The role of small intestinal bacterial overgrowth in postgastrectomy patients. Neurogastroenterol Motil. 2011;23:e191–6.
Saltzman JR, Kowdley KV, Pedrosa MC, et al. Bacterial overgrowth without clinical malabsorption in elderly hypochlorhydric subjects. Gastroenterology. 1994;106:615–23.
Shindo K, Machida M, Fukumura M, et al. Omeprazole induces altered bile acid metabolism. Gut. 1998;42:266–71.
Lombardo L, Foti M, Ruggia O, Chiecchio A. Increased incidence of small intestinal bacterial overgrowth during proton pump inhibitor therapy. Clin Gastroenterol Hepatol. 2010;8:504–8.
Compare D, Pica L, Rocco A, et al. Effects of long-term PPI treatment on producing bowel symptoms and SIBO. Eur J Clin Invest. 2011;41:380–6.
Jacobs C, Coss Adame E, Attaluri A, et al. Dysmotility and proton pump inhibitor use are independent risk factors for small intestinal bacterial and/or fungal overgrowth. Aliment Pharmacol Ther. 2013;37:1103–11.
Franco DL, Disbrow MB, Kahn A, et al. Duodenal aspirates for small intestine bacterial overgrowth: yield, PPIs, and outcomes after treatment at a tertiary academic medical center. Gastroenterol Res Pract. 2015;2015:971582.
Ratuapli SK, Ellington TG, O'Neill MT, et al. Proton pump inhibitor therapy use does not predispose to small intestinal bacterial overgrowth. Am J Gastroenterol. 2012;107:730–5.
Giamarellos-Bourboulis EJ, Pyleris E, Barbatzas C, et al. Small intestinal bacterial overgrowth is associated with irritable bowel syndrome and is independent of proton pump inhibitor usage. BMC Gastroenterol. 2016;16:67.
Weitsman S, Celly S, Leite G, et al. Effects of proton pump inhibitors on the small bowel and stool microbiomes. Dig Dis Sci. 2022;67:224–32.
Parodi A, Sessarego M, Greco A, et al. Small intestinal bacterial overgrowth in patients suffering from scleroderma: clinical effectiveness of its eradication. Am J Gastroenterol. 2008;103:1257–62.
Marie I, Ducrotté P, Denis P, et al. Small intestinal bacterial overgrowth in systemic sclerosis. Rheumatology (Oxford). 2009;48:1314–9.
Tauber M, Avouac J, Benahmed A, et al. Prevalence and predictors of small intestinal bacterial overgrowth in systemic sclerosis patients with gastrointestinal symptoms. Clin Exp Rheumatol. 2014 Nov-Dec;32 6 Suppl 86:S-82–7.
Polkowska-Pruszynska B, Gerkowicz A, Szczepanik-Kulak P, Krasowska D. Small intestinal bacterial overgrowth in systemic sclerosis: a review of the literature. Arch Dermatol Res. 2019;311:1–8.
Cuoco L, Montalto M, Jorizzo RA, et al. Eradication of small intestinal bacterial overgrowth and oro-cecal transit in diabetics. Hepatogastroenterology. 2002;49:1582–6.
Rana S, Bhansali A, Bhadada S, et al. Orocecal transit time and small intestinal bacterial overgrowth in type 2 diabetes patients from North India. Diabetes Technol Ther. 2011;13:1115–20.
Rana SV, Malik A, Bhadada SK, et al. Malabsorption, orocecal transit time and small intestinal bacterial overgrowth in type 2 diabetic patients: a connection. Indian J Clin Biochem. 2017;32:84–9.
Malik A, Morya RK, Bhadada SK, Rana S. Type 1 diabetes mellitus: complex interplay of oxidative stress, cytokines, gastrointestinal motility and small intestinal bacterial overgrowth. Eur J Clin Invest. 2018;48:e13021.
Lauritano EC, Bilotta AL, Gabrielli M, et al. Association between hypothyroidism and small intestinal bacterial overgrowth. J Clin Endocrinol Metab. 2007;92:4180–4.
Lee AA, Baker JR, Wamsteker EJ, et al. Small intestinal bacterial overgrowth is common in chronic pancreatitis and associates with diabetes, chronic pancreatitis severity, low zinc levels, and opiate use. Am J Gastroenterol. 2019;114:1163–71.
Ghoshal UC, Ghoshal U, Das K, Misra A. Utility of hydrogen breath tests in diagnosis of small intestinal bacterial overgrowth in malabsorption syndrome and its relationship with oro-cecal transit time. Indian J Gastroenterol. 2006;25:6–10.
Lunia MK, Sharma BC, Sachdeva S. Small intestinal bacterial overgrowth and delayed orocecal transit time in patients with cirrhosis and low-grade hepatic encephalopathy. Hepatol Int. 2013;7:268–73.
Rana SV, Sharma S, Malik A, et al. Small intestinal bacterial overgrowth and orocecal transit time in patients of inflammatory bowel disease. Dig Dis Sci. 2013;58:2594–8.
Roland BC, Ciarleglio MM, Clarke JO, et al. Small intestinal transit time is delayed in small intestinal bacterial overgrowth. J Clin Gastroenterol. 2015;49:571–6.
Chander Roland B, Mullin GE, Passi M, et al. A prospective evaluation of ileocecal valve dysfunction and intestinal motility derangements in small intestinal bacterial overgrowth. Dig Dis Sci. 2017;62:3525–35.
Roland BC, Ciarleglio MM, Clarke JO, et al. Low ileocecal valve pressure is significantly associated with small intestinal bacterial overgrowth (SIBO). Dig Dis Sci. 2014;59:1269–77.
Riordan SM, McIver CJ, Wakefield D, et al. Serum immunoglobulin and soluble IL-2 receptor levels in small intestinal overgrowth with indigenous gut flora. Dig Dis Sci. 1999;44:939–44.
Belitsos PC, Greenson JK, Yardley JH, et al. Association of gastric hypoacidity with opportunistic enteric infections in patients with AIDS. J Infect Dis. 1992;166:277–84.
Pignata C, Budillon G, Monaco G, et al. Jejunal bacterial overgrowth and intestinal permeability in children with immunodeficiency syndromes. Gut. 1990;31:879–82.
Rubio-Tapia A, Hernandez-Calleros J, Trinidad-Hernandez S, Uscanga L. Clinical characteristics of a group of adults with nodular lymphoid hyperplasia: a single center experience. World J Gastroenterol. 2006;12:1945–8.
Deloose E, Tack J. Redefining the functional roles of the gastrointestinal migrating motor complex and motilin in small bacterial overgrowth and hunger signaling. Am J Physiol Gastrointest Liver Physiol. 2016;310:G228–33.
Ghoshal UC, Bhut B, Misra A. Patients with specific gastrointestinal motility disorders are commonly diagnosed as functional GI disorders in the early stage by community physicians due to lack of awareness. Turk J Gastroenterol. 2021;32:336–48.
Sawadpanich K, Soison P, Chunlertrith K, et al. Prevalence and associated factors of small intestinal bacterial overgrowth among systemic sclerosis patients. Int J Rheum Dis. 2019;22:695–9.
Adarsh MB, Sharma SK, Sinha SK, et al. Gastrointestinal dysmotility and infections in systemic sclerosis- an Indian scenario. Curr Rheumatol Rev. 2018;14:172–6.
Almandoz JP, Gharib H. Hypothyroidism: etiology, diagnosis, and management. Med Clin North Am. 2012;96:203–21.
Ciobanu L, Dumitrascu DL. Gastrointestinal motility disorders in endocrine diseases. Pol Arch Med Wewn. 2011;121:129–36.
Yaylali O, Kirac S, Yilmaz M, et al. Does hypothyroidism affect gastrointestinal motility? Gastroenterol Res Pract. 2009;2009:529802.
Barboza JL, Okun MS, Moshiree B. The treatment of gastroparesis, constipation and small intestinal bacterial overgrowth syndrome in patients with Parkinson’s disease. Expert Opin Pharmacother. 2015;16:2449–64.
Vizcarra JA, Wilson-Perez HE, Fasano A, Espay AJ. Small intestinal bacterial overgrowth in Parkinson’s disease: tribulations of a trial. Parkinsonism Relat Disord. 2018;54:110–2.
Fasano A, Bove F, Gabrielli M, et al. The role of small intestinal bacterial overgrowth in Parkinson’s disease. Mov Disord. 2013;28:1241–9.
Tan AH, Mahadeva S, Thalha AM, et al. Small intestinal bacterial overgrowth in Parkinson’s disease. Parkinsonism Relat Disord. 2014;20:535–40.
Niu XL, Liu L, Song ZX, et al. Prevalence of small intestinal bacterial overgrowth in Chinese patients with Parkinson’s disease. J Neural Transm (Vienna). 2016;123:1381–6.
Rezaie A, Pimentel M, Rao SS. How to test and treat small intestinal bacterial overgrowth: an evidence-based approach. Curr Gastroenterol Rep. 2016;18:8.
Achufusi TGO, Sharma A, Zamora EA, Manocha D. Small intestinal bacterial overgrowth: comprehensive review of diagnosis, prevention, and treatment methods. Cureus. 2020;12:e8860.
Mayo SA, Song YK, Cruz MR, et al. Indomethacin injury to the rat small intestine is dependent upon biliary secretion and is associated with overgrowth of enterococci. Physiol Rep. 2016;4:e12725.
Muraki M, Fujiwara Y, Machida H, et al. Role of small intestinal bacterial overgrowth in severe small intestinal damage in chronic non-steroidal anti-inflammatory drug users. Scand J Gastroenterol. 2014;49:267–73.
Revaiah PC, Kochhar R, Rana SV, et al. Risk of small intestinal bacterial overgrowth in patients receiving proton pump inhibitors versus proton pump inhibitors plus prokinetics. JGH Open. 2018;2:47–53.
Lo WK, Chan WW. Proton pump inhibitor use and the risk of small intestinal bacterial overgrowth: a meta-analysis. Clin Gastroenterol Hepatol. 2013;11:483–90.
Su T, Lai S, Lee A, et al. Meta-analysis: proton pump inhibitors moderately increase the risk of small intestinal bacterial overgrowth. J Gastroenterol. 2018;53:27–36.
Madrid AM, Defilippi CC, Defilippi GC, et al. Small intestinal bacterial overgrowth in patients with functional gastrointestinal diseases. Rev Med Chil. 2007;135:1245–52.
Korterink JJ, Benninga MA, van Wering HM, Deckers-Kocken JM. Glucose hydrogen breath test for small intestinal bacterial overgrowth in children with abdominal pain-related functional gastrointestinal disorders. J Pediatr Gastroenterol Nutr. 2015;60:498–502.
Collins BS, Lin HC. Chronic abdominal pain in children is associated with high prevalence of abnormal microbial fermentation. Dig Dis Sci. 2010;55:124–30.
Garg N, Basu S, Singh P, et al. Prevalence of abnormal lactose breath hydrogen tests in children with functional abdominal pain. Indian J Gastroenterol. 2017;36:179–83.
Triadafilopoulos G. Utility of wireless motility capsule and lactulose breath testing in the evaluation of patients with chronic functional bloating. BMJ Open Gastroenterol. 2016;3:e000110.
Noh CK, Lee KJ. Fecal microbiota alterations and small intestinal bacterial overgrowth in functional abdominal bloating/distention. J Neurogastroenterol Motil. 2020;26:539–49.
Costa MB, Azeredo IL Jr, Marciano RD, et al. Evaluation of small intestine bacterial overgrowth in patients with functional dyspepsia through H2 breath test. Arq Gastroenterol. 2012;49:279–83.
Shimura S, Ishimura N, Mikami H, et al. Small intestinal bacterial overgrowth in patients with refractory functional gastrointestinal disorders. J Neurogastroenterol Motil. 2016;22:60–8.
Shah A, Gurusamy SR, Hansen T, et al. Concomitant irritable bowel syndrome does not influence the response to antimicrobial therapy in patients with functional dyspepsia. Dig Dis Sci. 2022;67:2299–309.
Spiller RC, Trotman IF, Higgins BE, et al. The ileal brake--inhibition of jejunal motility after ileal fat perfusion in man. Gut. 1984;25:365–74.
Spiller RC, Trotman IF, Adrian TE, et al. Further characterisation of the ‘ileal brake’ reflex in man-effect of ileal infusion of partial digests of fat, protein, and starch on jejunal motility and release of neurotensin, enteroglucagon, and peptide YY. Gut. 1988;29:1042–51.
Bushyhead D, Quigley EMM. Small intestinal bacterial overgrowth pathophysiology and its implications for definition and management. Gastroenterology. 2022;S0016-5085(22):00357–2.
Maslennikov R, Pavlov C, Ivashkin V. Small intestinal bacterial overgrowth in cirrhosis: systematic review and metaanalysis. Hepatol Int. 2018;12:567–76.
Wijarnpreecha K, Kim D, Raymond P, et al. Associations between sarcopenia and nonalcoholic fatty liver disease and advanced fibrosis in the USA. Eur J Gastroenterol Hepatol. 2019;31:1121–8.
Capurso G, Signoretti M, Archibugi L, et al. Systematic review and meta-analysis: small intestinal bacterial overgrowth in chronic pancreatitis. United European Gastroenterol J. 2016;4:697–705.
El Kurdi B, Babar S, El Iskandarani M, et al. Factors that affect prevalence of small intestinal bacterial overgrowth in chronic pancreatitis: a systematic review, meta-analysis, and meta-regression. Clin Transl Gastroenterol. 2019;10:e00072.
Ní Chonchubhair HM, Bashir Y, Dobson M, et al. The prevalence of small intestinal bacterial overgrowth in non-surgical patients with chronic pancreatitis and pancreatic exocrine insufficiency (PEI). Pancreatology. 2018;18:379–85.
Zhang M, Zhu HM, He F, et al. Association between acute pancreatitis and small intestinal bacterial overgrowth assessed by hydrogen breath test. World J Gastroenterol. 2017;23:8591–6.
Bode JC, Bode C, Heidelbach R, et al. Jejunal microflora in patients with chronic alcohol abuse. Hepatogastroenterology. 1984;31:30–4.
Hauge T, Persson J, Danielsson D. Mucosal bacterial growth in the upper gastrointestinal tract in alcoholics (heavy drinkers). Digestion. 1997;58:591–5.
Bode JC, Knuppel H, Schwerk W, Bode C. Activities of cytoplasmic, mitochondrial and brush border enzymes in jejunal mucosa of chronic alcoholics. Z Gastroenterol. 1982;20:228–33.
Beck IT, Dinda PK. Acute exposure of small intestine to ethanol: effects on morphology and function. Dig Dis Sci. 1981;26:817–38.
Bode C, Bode JC. Effect of alcohol consumption on the gut. Best Pract Res Clin Gastroenterol. 2003;17:575–92.
Addolorato G, Capristo E, Gasbarrini G, Stefanini GF. Depression, alcohol abuse and orocaecal transit time. Gut. 1997;41:417–8.
Maier A, Bode C, Fritz P, Bode JC. Effects of chronic alcohol abuse on duodenal mononuclear cells in man. Dig Dis Sci. 1999;44:691–6.
Gabbard SL, Lacy BE, Levine GM, Crowell MD. The impact of alcohol consumption and cholecystectomy on small intestinal bacterial overgrowth. Dig Dis Sci. 2014;59:638–44.
Victor DW 3rd, Quigley EM. The microbiome and the liver: the basics. Semin Liver Dis. 2016;36:299–305.
Quigley EM, Abu-Shanab A, Murphy EF, et al. The metabolic role of the microbiome: implications for NAFLD and the metabolic syndrome. Semin Liver Dis. 2016;36:312–6.
Ierardi E, Losurdo G, Sorrentino C, et al. Macronutrient intakes in obese subjects with or without small intestinal bacterialovergrowth: an alimentary survey. Scand J Gastroenterol. 2016;51:277–80.
Fialho A, Fialho A, Thota P, et al. Higher visceral to subcutaneous fat ratio is associated with small intestinal bacterial overgrowth. Nutr Metab Cardiovasc Dis. 2016;26:773–7.
Sabate JM, Coupaye M, Ledoux S, et al. Consequences of small intestinal bacterial overgrowth in obese patients before and after bariatric surgery. Obes Surg. 2017;27:599–605.
Roland BC, Lee D, Miller LS, et al. Obesity increases the risk of small intestinal bacterial overgrowth (SIBO). Neurogastroenterol Motil. 2018;30. https://doi.org/10.1111/nmo.13199.
Jung SE, Joo NS, Han KS, Kim KN. Obesity is inversely related to hydrogen-producing small intestinal bacterial overgrowth in non-constipation irritable bowel syndrome. J Korean Med Sci. 2017;32:948–53.
Wijarnpreecha K, Werlang ME, Watthanasuntorn K, et al. Obesity and risk of small intestine bacterial overgrowth: a systematic review and meta-analysis. Dig Dis Sci. 2020;65:1414–22.
Rana SV, Bhardwaj SB. Small intestinal bacterial overgrowth. Scand J Gastroenterol. 2008;43:1030–7.
Sherman P, Wesley A, Forstner G. Sequential disaccharidase loss in rat intestinal blind loops: impact of malnutrition. Am J Physiol. 1985;248:G626–32.
Mathias JR, Clench MH. Review: pathophysiology of diarrhea caused by bacterial overgrowth of the small intestine. Am J Med Sci. 1985;289:243–8.
Fan X, Sellin JH. Review article: small intestinal bacterial overgrowth, bile acid malabsorption and gluten intolerance as possible causes of chronic watery diarrhoea. Aliment Pharmacol Ther. 2009;29:1069–77.
Sachdev AH, Pimentel M. Gastrointestinal bacterial overgrowth: pathogenesis and clinical significance. Ther Adv Chronic Dis. 2013;4:223–31.
Bala L, Ghoshal UC, Ghoshal U, et al. Malabsorption syndrome with and without small intestinal bacterial overgrowth: a study on upper-gut aspirate using 1H NMR spectroscopy. Magn Reson Med. 2006;56:738–44.
Giannella RA, Broitman SA, Zamcheck N. Competition between bacteria and intrinsic factor for vitamin B : implications for vitamin B malabsorption in intestinal bacterial overgrowth. Gastroenterology. 1972;62:255–60.
Jones EA, Craigie A, Tavill AS, et al. Protein metabolism in the intestinal stagnant loop syndrome. Gut. 1968;9:466–9.
Rutgeerts L, Mainguet P, Tytgat G, Eggermont E. Enterokinase in contaminated small-bowel syndrome. Digestion. 1974;10:249–54.
King CE, Toskes PP. Protein-losing enteropathy in the human and experimental rat blind-loop syndrome. Gastroenterology. 1981;80:504–9.
Riordan SM, McIver CJ, Thomas DH, et al. Luminal bacteria and small-intestinal permeability. Scand J Gastroenterol. 1997;32:556–63.
Al-Khatib K, Lin HC. Immune activation and gut microbes in irritable bowel syndrome. Gut Liver. 2009;3:14–9.
Srivastava D, Ghoshal U, Mittal RD, Ghoshal UC. Associations between IL-1RA polymorphisms and small intestinal bacterial overgrowth among patients with irritable bowel syndrome from India. Neurogastroenterol Motil. 2014;26:1408–16.
Spinucci G, Guidetti M, Lanzoni E, Pironi L. Endogenous ethanol production in a patient with chronic intestinal pseudo obstruction and small intestinal bacterial overgrowth. Eur J Gastroenterol Hepatol. 2006;18:799–802.
Dibaise JK, Young RJ, Vanderhoof JA. Enteric microbial flora, bacterial overgrowth, and short-bowel syndrome. Clin Gastroenterol Hepatol. 2006;4:11–20.
Rao SSC, Rehman A, Yu S, Andino NM. Brain fogginess, gas and bloating: a link between SIBO, probiotics and metabolic acidosis. Clin Transl Gastroenterol. 2018;9:162.
Greenson JK. The biopsy pathology of non-coeliac enteropathy. Histopathology. 2015;66:29–36.
Toskes PP, Giannella RA, Jervis HR, et al. Small intestinal mucosal injury in the experimental blind loop syndrome. Light- and electron-microscopic and histochemical studies. Gastroenterology. 1975;68:1193–203.
Chen B, Zhu S, Du L, et al. Reduced interstitial cells of Cajal and increased intraepithelial lymphocytes are associated with development of small intestinal bacterial overgrowth in post-infectious IBS mouse model. Scand J Gastroenterol. 2017;52:1065–71.
Riordan SM, McIver CJ, Wakefield D, et al. Small intestinal mucosal immunity and morphometry in luminal overgrowth of indigenous gut flora. Am J Gastroenterol. 2001;96:494–500.
Lappinga PJ, Abraham SC, Murray JA, et al. Small intestinal bacterial overgrowth: histopathologic features and clinical correlates in an underrecognized entity. Arch Pathol Lab Med. 2010;134:264–70.
Attaluri A, Jackson M, Valestin J, Rao SS. Methanogenic flora is associated with altered colonic transit but not stool characteristics in constipation without IBS. Am J Gastroenterol. 2010;105:1407–11.
Chatterjee S, Park S, Low K, et al. The degree of breath methane production in IBS correlates with the severity of constipation. Am J Gastroenterol. 2007;102:837–41.
Pimentel M, Lin HC, Enayati P, et al. Methane, a gas produced by enteric bacteria, slows intestinal transit and augments small intestinal contractile activity. Am J Physiol Gastrointest Liver Physiol. 2006;290:G1089–95.
Pimentel M, Chang C, Chua KS, et al. Antibiotic treatment of constipation-predominant irritable bowel syndrome. Dig Dis Sci. 2014;59:1278–85.
Kunkel D, Basseri RJ, Makhani MD, et al. Methane on breath testing is associated with constipation: a systematic review and meta-analysis. Dig Dis Sci. 2011;56:1612–8.
Gandhi A, Shah A, Jones MP, et al. Methane positive small intestinal bacterial overgrowth in inflammatory bowel disease and irritable bowel syndrome: a systematic review and meta-analysis. Gut Microbes. 2021;13:1933313.
Kim G, Deepinder F, Morales W, et al. Methanobrevibacter smithii is the predominant methanogen in patients with constipation-predominant IBS and methane on breath. Dig Dis Sci. 2012;57:3213–8.
Jahng J, Jung IS, Choi EJ, et al. The effects of methane and hydrogen gases produced by enteric bacteria on ileal motility and colonic transit time. Neurogastroenterol Motil. 2012;24(185–90):e192.
Lee KM, Paik CN, Chung WC, et al. Breath methane positivity is more common and higher in patients with objectively proven delayed transit constipation. Eur J Gastroenterol Hepatol. 2013;25:726–32.
Ghoshal U, Shukla R, Srivastava D, Ghoshal UC. Irritable bowel syndrome, particularly the constipation-predominant form, involves an increase in Methanobrevibacter smithii, which Is associated with higher methane production. Gut Liver. 2016;10:932–8.
Ghoshal UC, Srivastava D, Misra A. A randomized double-blind placebo-controlled trial showing rifaximin to improve constipation by reducing methane production and accelerating colon transit: A pilot study. Indian J Gastroenterol. 2018;37:416–23.
Sachdeva S, Puri AS, Kumar A, et al. Brain fogginess and SIBO: A link or just a mirage? Clin Transl Gastroenterol. 2018;9:184.
Rao SSC, Yu S. Response to Sachdeva et al: Brain fogginess and SIBO is not a mirage. Clin Transl Gastroenterol. 2018;9:194.
McIntosh S, Medjoub K, Deans K, Sexton S. Hyperammonaemic encephalopathy following an uncomplicated surgery. BMJ Case Rep. 2017;2017:bcr2017221458.
Gasbarrini A, Lauritano EC, Gabrielli M, et al. Small intestinal bacterial overgrowth: diagnosis and treatment. Dig Dis. 2007;25:237–40.
Lykova EA, Bondarenko VM, Parfenov AI, Matsulevich TV. Bacterial overgrowth syndrome in the small intestine: pathogenesis, clinical significance and therapy tactics. Eksp Klin Gastroenterol. 2005;113:51–7.
Ranjan P, Ghoshal UC, Aggarwal R, et al. Etiological spectrum of sporadic malabsorption syndrome in northern Indian adults at a tertiary hospital. Indian J Gastroenterol. 2004;23:94–8.
Ghoshal UC, Mehrotra M, Kumar S, et al. Spectrum of malabsorption syndrome among adults and factors differentiating celiac disease & tropical malabsorption. Indian J Med Res. 2012;136:451–9.
Losurdo G, Marra A, Shahini E, et al. Small intestinal bacterial overgrowth and celiac disease: a systematic review with pooled-data analysis. Neurogastroenterol Motil. 2017;29. https://doi.org/10.1111/nmo.13028.
Ghoshal UC, Gwee KA. Post-infectious IBS, tropical sprue and small intestinal bacterial overgrowth: the missing link. Nat Rev Gastroenterol Hepatol. 2017;14:435–41.
Sachdeva S, Rawat AK, Reddy RS, Puri AS. Small intestinal bacterial overgrowth (SIBO) in irritable bowel syndrome: frequency and predictors. J Gastroenterol Hepatol. 2011;26(Suppl 3):135–8.
Ghoshal UC, Goel A, Quigley EMM. Gut microbiota abnormalities, small intestinal bacterial overgrowth, and non-alcoholic fatty liver disease: an emerging paradigm. Indian J Gastroenterol. 2020;39:9–21.
Berean KJ, Ha N, Ou JZ, et al. The safety and sensitivity of a telemetric capsule to monitor gastrointestinal hydrogen production in vivo in healthy subjects: a pilot trial comparison to concurrent breath analysis. Aliment Pharmacol Ther. 2018;48:646–54.
Ghoshal UC. How to interpret hydrogen breath tests. J Neurogastroenterol Motil. 2011;17:312–7.
Losurdo G, Leandro G, Ierardi E, et al. Breath tests for the non-invasive diagnosis of small intestinal bacterial overgrowth: A systematic review with meta-analysis. J Neurogastroenterol Motil. 2020;26:16–28.
Schatz RA, Zhang Q, Lodhia N, et al. Predisposing factors for positive D-Xylose breath test for evaluation of small intestinal bacterial overgrowth: a retrospective study of 932 patients. World J Gastroenterol. 2015;21:4574–82.
Ghoshal UC, Srivastava D. Irritable bowel syndrome and small intestinal bacterial overgrowth: meaningful association or unnecessary hype. World J Gastroenterol. 2014;20:2482–91.
Berthold HK, Schober P, Scheurlen C, et al. Use of the lactose-[13C] ureide breath test for diagnosis of small bowel bacterial overgrowth: comparison to the glucose hydrogen breath test. J Gastroenterol. 2009;44:944–51.
Pimentel M, Morales W, Lezcano S, et al. Low-dose nocturnal tegaserod or erythromycin delays symptom recurrence after treatment of irritable bowel syndrome based on presumed bacterial overgrowth. Gastroenterol Hepatol (N Y). 2009;5:435–42.
Robinson-Papp J, Nmashie A, Pedowitz E, et al. The effect of pyridostigmine on small intestinal bacterial overgrowth (SIBO) and plasma inflammatory biomarkers in HIV-associated autonomic neuropathies. J Neurovirol. 2019;25:551–9.
Gatta L, Scarpignato C. Systematic review with meta-analysis: rifaximin is effective and safe for the treatment of small intestine bacterial overgrowth. Aliment Pharmacol Ther. 2017;45:604–16.
Pittman N, Rawn SM, Wang M, et al. Treatment of small intestinal bacterial overgrowth in systemic sclerosis: a systematic review. Rheumatology (Oxford). 2018;57:1802–11.
Pimentel M, Lembo A, Chey WD, et al. Rifaximin therapy for patients with irritable bowel syndrome without constipation. N Engl J Med. 2011;364:22–32.
Shah SC, Day LW, Somsouk M, Sewell JL. Meta-analysis: antibiotic therapy for small intestinal bacterial overgrowth. Aliment Pharmacol Ther. 2013;38:925–34.
Zhao J, Zheng X, Chu H, et al. A study of the methodological and clinical validity of the combined lactulose hydrogen breath test with scintigraphic oro-cecal transit test for diagnosing small intestinal bacterial overgrowth in IBS patients. Neurogastroenterol Motil. 2014;26:794–802.
Rezaie A, Heimanson Z, McCallum R, Pimentel M. Lactulose breath testing as a predictor of response to rifaximin in patients with irritable bowel syndrome with diarrhea. Am J Gastroenterol. 2019;114:1886–93.
Low K, Hwang L, Hua J, et al. A combination of rifaximin and neomycin is most effective in treating irritable bowel syndrome patients with methane on lactulose breath test. J Clin Gastroenterol. 2010;44:547–50.
Lauritano EC, Gabrielli M, Scarpellini E, et al. Small intestinal bacterial overgrowth recurrence after antibiotic therapy. Am J Gastroenterol. 2008;103:2031–5.
Sangam A, Dalal A, Arivarasan K, et al. Recurrence of small intestinal bacterial overgrowth after successful antibiotic therapy in patients with irritable bowel syndrome: frequency and predictors. J Neurogastroenterol Motil. 2015;21:S3.
Lembo A, Pimentel M, Rao SS, et al. Repeat treatment with rifaximin is safe and effective in patients with diarrhea predominant irritable bowel syndrome. Gastroenterology. 2016;151:1113–21.
Pimentel M, Cash BD, Lembo A, et al. Repeat rifaximin for irritable bowel syndrome: no clinically significant changes in stool microbial antibiotic sensitivity. Dig Dis Sci. 2017;62:2455–63.
Nickles MA, Hasan A, Shakhbazova A, et al. Alternative treatment approaches to small intestinal bacterial overgrowth: a systematic review. J Altern Complement Med. 2021;27:108–19.
Attar A, Flourié B, Rambaud JC, et al. Antibiotic efficacy in small intestinal bacterial overgrowth-related chronic diarrhea: a crossover, randomized trial. Gastroenterology. 1999;117:794–7.
Galie S, Garcia-Gavilan J, Papandreou C, et al. Effects of mediterranean diet on plasma metabolites and their relationship with insulin resistance and gut microbiota composition in a crossover randomized clinical trial. Clin Nutr. 2021;40:3798–806.
Abreu YAAT, Milke-Garcia MP, Arguello-Arevalo GA, et al. Dietary fiber and the microbiota: A narrative review by a group of experts from the Asociacion Mexicana de Gastroenterologia. Rev Gastroenterol Mex (Engl Ed). 2021;86:287–304.
Pimentel M, Constantino T, Kong Y, et al. A 14-day elemental diet is highly effective in normalizing the lactulose breath test. Dig Dis Sci. 2004;49:73–7.
Acknowledgements
The authors thank Indian Neurogastroenterology and Motility Association (INMA; www.gimotilityindia.in; earlier named Indian Motility and Functional Diseases Association) and the Shanti Public Educational and Development Society (www.spreadhealth.in). The authors thank Priyanka Tiwari, School of Telemedicine and Biomedical Informatics, SGPGIMS, Lucknow, for her support towards the development of the voting system for this consensus. The authors thank Dr. Uzma Mustafa for her support. The authors thank Sun Pharma Laboratories Ltd., India, for contribution to the Indian Neurogastroenterology and Motility Association.
Author information
Authors and Affiliations
Contributions
UCG, SS, UG, AM, and NP composed the statements first; subsequently, all the authors modified and finalized the statements. All the authors voted for the statements. UCG and SS wrote the first draft of the manuscript, which was edited by all the authors. All the authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Copyright
Indian Neurogastroenterology and Motility Association.
Conflict of interest
UCG has patent applications for upper gut aspirate culture, FODMAP fermentation chamber, and BreathCalc. KAG is an advisory board member to Adare. GH report to be on the advisory boards of Australian Biotherapeutics, Glutagen, Bayer and received research support from Bayer, Abbott, Pfizer, Janssen, Takeda, Allergan. He serves on the Boards of the West Moreton Hospital and Health Service, Queensland, UQ Healthcare, Brisbane, and the Gastro-Liga, Germany. He has a patent for the Brisbane aseptic biopsy device and serves as Editor of the Gastro-Liga Newsletter. None of the other authors have any conflict of interest to declare in relation to this paper.
Disclaimer
The authors are solely responsible for the data and the contents of the paper. In no way, the Honorary Editor-in-Chief, Editorial Board Members, the Indian Society of Gastroenterology or the printer/publishers are responsible for the results/findings and content of this article.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ghoshal, U.C., Sachdeva, S., Ghoshal, U. et al. Asian-Pacific consensus on small intestinal bacterial overgrowth in gastrointestinal disorders: An initiative of the Indian Neurogastroenterology and Motility Association. Indian J Gastroenterol 41, 483–507 (2022). https://doi.org/10.1007/s12664-022-01292-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12664-022-01292-x