Abstract
Purpose
The management of chronic pain often involves interventional procedures such as injections. Nevertheless, there have been concerns raised regarding the frequency with which these injections are being performed. We conducted a descriptive study to examine trends in the use of pain injections over a ten-year time period in Ontario, Canada.
Methods
We used provincial administrative data to conduct a retrospective observational study of the most common pain injections performed from 2010 to 2019 in Ontario. We determined the frequency of pain injections and their associated physician billings from physician billing data.
Results
A total of 18,050,058 pain injections were included in this study with an associated total cost of CAD 865,431,605. There was a threefold increase in the number of blocks performed annually and associated costs, rising from 1,009,324 blocks (CAD 50,026,678) in 2010 to 3,198,679 blocks (CAD 156,809,081) in 2019. The majority of injections were performed by general practioners (70.8%), followed by anesthesiologists (8.3%).
Conclusion
This descriptive study revealed a rapid increase in the frequency of pain injections performed in Ontario from 2010 to 2019. Given the associated costs and potential risks, this warrants further investigation to ensure that these interventions are being administered appropriately.
Résumé
Objectif
La prise en charge de la douleur chronique implique souvent des procédures interventionnelles telles que des injections. Néanmoins, des préoccupations ont été soulevées quant à la fréquence à laquelle ces injections sont administrées. Nous avons réalisé une étude descriptive pour examiner les tendances dans l’utilisation d’injections pour soulager la douleur sur une période de dix ans en Ontario, au Canada.
Méthode
Nous avons utilisé les données administratives provinciales pour réaliser une étude observationnelle rétrospective des injections pour soulager la douleur les plus courantes effectuées de 2010 à 2019 en Ontario. Nous avons déterminé la fréquence des injections pour soulager la douleur et les facturations des médecins associées à partir des données de facturation des médecins.
Résultats
Au total, 18 050 058 injections pour soulager la douleur ont été incluses dans cette étude, avec un coût total associé de 865 431 605 CAD. Le nombre de blocs exécutés chaque année et les coûts associés ont triplé, passant de 1 009 324 blocs (50 026 678 CAD) en 2010 à 3 198 679 blocs (156 809 081 CAD) en 2019. La majorité des injections ont été administrées par des médecins généralistes (70,8 %), suivis par des anesthésiologistes (8,3 %).
Conclusion
Cette étude descriptive a révélé une augmentation rapide de la fréquence des injections pour soulager la douleur et administrées en Ontario de 2010 à 2019. Compte tenu des coûts associés et des risques potentiels, cela justifie une enquête plus approfondie pour s’assurer que ces interventions sont administrées de manière appropriée.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Nearly one in five Canadians will experience chronic pain during their lifetime.1 Beyond experiencing discomfort, this debilitating condition can have significant detrimental impacts on numerous domains including sleep, function, social relationships, and mental health.2 A key therapeutic approach in the management of chronic pain has been the use of interventional therapies such as the injection of a local anesthetic and/or steroid around nerves to interrupt transmission and/or reduce perineural inflammation.3 While pain injections can provide relief, the procedures are not benign and can be associated with significant risks such as nerve damage.4 Further, strong evidence to support the widespread use of pain injections is lacking. For example, a systematic review examining the effectiveness of low-back pain found insufficient evidence to support injection therapy for chronic low-back pain.5 Existing trials have also been fraught with limitations such as variations in technique, difficulty blinding, lack of allocation concealment, differential dropout rates, and heterogeneity of patient pain presentations.6,7,8
Thus, the existing literature to date provides little guidance about which patients will benefit from these injections and the frequency with which they should be administered. Recent reports have raised questions about the high frequency of these procedures being performed in the province of Ontario, Canada.9,10 We therefore sought to conduct a descriptive study examining the use of injections for chronic pain over a ten-year time period.
Methods
We conducted a retrospective observational study of pain injections performed in Ontario, Canada from 1 January 2010 to 31 December 2019. Data were obtained from ICES (formerly the Institute for Clinical and Evaluative Sciences), which is an independent, non-profit research institute whose legal status under Ontario’s health information privacy law allows it to collect and analyze healthcare and demographic data, without consent, for health system evaluation and improvement. We used physician billing data from the Ontario Health Insurance Plan (OHIP) to identify the number of pain injections administered by physicians. To ensure that only outpatient injections were captured, we excluded records that were billed during a hospitalization or if the physician administering the injection did not have any outpatient OHIP claims in 2019. Patient records with a missing or invalid age or sex and those associated with non-Ontario residents or those with a physician who was out of province or could not be linked to Ontario databases were also excluded.
To determine which set of injections for chronic pain should be included in the analysis, we first conducted a literature search to identify potential billing codes used in previous studies, resulting in a total of 65 codes. Two individuals with expertise and experience in chronic pain management (K. L. and H. C.) independently reviewed these codes and excluded codes related to obstetrics and surgery, resulting in 57 codes typically used in the management of chronic pain. We then divided the top 15 codes of this group (accounting for > 95% of all billings) into three categories based on region: axial/back, facial, and peripheral/extremity. A list of codes considered in this study can be found in Electronic Supplementary Material (ESM) eTable 1.
We tabulated the overall number of pain injections performed and their associated costs from physician billings over the study period. For the final year of the study (2019), we derived several additional metrics including the number of injections performed per patient, and the distribution of injections across physician specialties.
Results
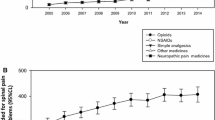
A total of 18,388,171 pain injections were administered over the ten-year study period, and after exclusions 18,050,058 were included in this study (ESM eFigure). The associated total cost was CAD 865,431,605. There was a threefold increase in the number of blocks performed annually and their associated costs, rising from 1,009,324 blocks (CAD 50,026,678) in 2010 to 3,198,679 blocks (CAD 156,809,081) in 2019 (Table 1; Figure). The proportion of pain injections administered varied by injection type, with injections of extremities and other peripheral/myofascial blocks being responsible for 58.2% of all injections administered in 2019 (1,860,359 of 3,198,679) and 46.3% of total costs (CAD 72,618,063 of CAD 156,809,081; Table 1). A breakdown of the number of injections and costs for each billing code is presented in ESM eTable 2a–c.
In 2019, 312,828 patients received a chronic pain injection, the majority of whom (298,065, 95.3%) received at least one block of an extremity or other peripheral/myofascial block (Table 2). The median [interquartile range (IQR)] number of injections administered per patient in 2019 was 2 [1–3]; however, 10.6% of patients received more than 11 injections in 2019. These injections took place during a median [IQR] of 1 [1–2] visit, with 5.4% of patients having more than 11 visits for blocks. The number of visits per patient varied by type of injection, with 40.5% of patients receiving more than 11 visits for facial injections versus 4.9% for peripheral injections. General practitioners performed the majority of injections (70.8%), followed by anesthesiologists (8.3%), although this varied by injection type, with 84.1% of facial nerve blocks being administered by general practitioners and 11.4% of axial/back blocks being administered by anesthesiologists. The median [IQR] number of injections per physician who administered injections in 2019 was 12 [3–44]. Nevertheless, when broken down by type of injection, this was much higher among physicians administering axial/back injections (median [IQR] per physician annually, 239 [8–1,971]) and facial injections (median [IQR] per physician annually, 283 [10–1,110]).
Discussion
This descriptive study revealed a threefold increase in the administration of injections to manage chronic pain in Ontario over the ten-year period from 2010 to 2019. Further, the cost of physician billings for these injections totalled nearly 900 million CAD. Importantly, these data represent only the 15 most common procedures, and excluded costs for injections administered by salaried physicians (~5% of all injections), meaning that the true number of injections and resultant costs are likely much greater. We also found that these patterns were not consistent across injection types and physician specialty, with the majority of the injections being administered to extremities and being performed by general practitioners, and a large proportion of patients undergoing multiple injections per year.
Injections are widely considered to be an important tool in the management of chronic pain and have been used for decades. Nevertheless, there has been no significant change in the evidence base surrounding their role in pain management to explain their increased use. While data are sparse elsewhere in Canada, a study in the USA among Medicare recipients reported an annual 2.5% decline in the rate of epidural injections for chronic pain from 2009 to 2018.11 This suggests that there are factors particular to Ontario that have led to the rise of these interventional pain procedures.
Although the underlying drivers of the increase in injections found in our study cannot be discerned from our data, there are a few potential explanations. First, the increase could represent better access to interventional pain therapies, with these trends representing a positive development for patients with chronic pain. On the other hand, the growth in injections could represent an overuse of these procedures as a response to financial incentives tied to physician reimbursement in Ontario.9 Importantly, these interpretations are not mutually exclusive and determining the balance of access to care against inappropriate administration is difficult to do using administrative health data. One previous study based in Ontario, which examined the impact of paravetebral blocks, showed an increase in resource use and no change in opioid use following the procedure.10 While this suggests limited added value from these procedures, studies with administrative data could be prone to confounding by indication making it difficult to assert causality.12 Therefore, to answer this question, granular data from multiple providers on both procedures and patient outcomes such as pain intensity, pain interference, and side effects is required. Indeed, expanding data collection related to chronic pain interventions has been deemed a crucial step towards improving health system quality by the Canadian Pain Task Force.1
The study has several limitations, which should be noted when interpreting the data. First, the study relied on billing codes, which may or may not be reflective of the actual procedure performed. Further, the same procedure can be performed in different ways, e.g., with or without imaging guidance. Additionally, overall healthcare use was not considered. Thus, the costs calculated in this study may not be significant if healthcare expenditures were decreased as a result of the injection, e.g., fewer presentations to the Emergency Department for pain. Future studies that examine healthcare use and pain medication use at the individual level with a comparator group are needed to characterize the impact of injections at the patient and system levels.
While the exact cause of the increase in chronic pain injections in Ontario is unknown, the sheer number of procedures in 2019, alongside their rapid growth and associated costs over the last decade, indicate that further investigation into these trends is warranted. Given limited healthcare resources, it is imperative that policy makers appropriately allocate funding to effective interventions to ensure that chronic pain patients receive the best possible care. Unlike chronic pain injections, many other evidenced-based components of multimodal chronic pain therapy such as acupuncture, physical therapy, and psychotherapy are not routinely covered by provincial health plans. Further research is needed to determine the appropriateness and utility of chronic pain injections for individual patients in a manner that does not compromise access to care for those who benefit from these procedures.
References
Health Canada. Canadian Pain Task Force report: March 2021. Available from URL: https://www.canada.ca/en/health-canada/corporate/about-health-canada/public-engagement/external-advisory-bodies/canadian-pain-task-force/report-2021.html (accessed September 2022).
Dueñas M, Ojeda B, Salazar A, Mico JA, Failde I. A review of chronic pain impact on patients, their social environment and the health care system. J Pain Res 2016; 9: 457–67. https://doi.org/10.2147/jpr.s105892
Rosenquest RW, Benzon HT, Connis RT, et al. Practice guidelines for chronic pain management: an updated report by the American Society of Anesthesiologists Task Force on Chronic Pain Management and the American Society of Regional Anesthesia and Pain Medicine. Anesthesiology 2010; 112: 810–33. https://doi.org/10.1097/aln.0b013e3181c43103
Lee LA, Domino KB. Complications associated with peripheral nerve blocks: lessons from the ASA Closed Claims Project. Int Anesthesiol Clin 2005; 43: 111–8. https://doi.org/10.1097/01.aia.0000166329.31133.68
Staal JB, de Bie RA, de Vet Henrica CW, Hildebrandt J, Nelemans P. Injection therapy for subacute and chronic low back pain: an updated Cochrane review. Spine 2009; 34: 49–59. https://doi.org/10.1097/brs.0b013e3181909558
Merrill DG. Hoffman’s glasses: evidence-based medicine and the search for quality in the literature of interventional pain medicine. Reg Anesth Pain Med 2003; 28: 547–60. https://doi.org/10.1016/s1098-7339(03)00234-7
Carr DB. Evidence-based pain medicine: inconvenient truths. Pain Med 2017; 18: 2049–50. https://doi.org/10.1093/pm/pnx252
Staal JB, Nelemans PJ, dem Bie RA. Spinal injection therapy for low back pain. JAMA 2013; 309: 2439–40. https://doi.org/10.1001/jama.2013.5892
Boyle T, McLean J, Oved M, Bailey A. ‘That’s an injection mill.’ Ontario’s top-billing pain doctors capitalize on province’s lax rules, running up the public’s tab for chronic pain management. Toronto Star, 2020. Available from URL: https://www.thestar.com/news/investigations/2020/09/28/thats-an-injection-mill-ontarios-top-billing-pain-doctors-capitalize-on-provinces-lax-rules-running-up-the-publics-tab-for-chronic-pain-management.html (accessed September 2022).
Deng G, Gofeld M, Reid JN, Welk B, Agur AM, Loh E. A retrospective cohort study of healthcare utilization associated with paravertebral blocks for chronic pain management in Ontario. Can J Pain 2021; 5: 130–8. https://doi.org/10.1080/24740527.2021.1929883
Manchikanti L, Sanapati MR, Soin A, et al. An updated analysis of utilization of epidural procedures in managing chronic pain in the medicare population from 2000 to 2018. Pain Physician 2020; 23: 111–26.
Kyriacou DN, Lewis RJ. Confounding by indication in clinical research. JAMA 2016; 316: 1818–9. https://doi.org/10.1001/jama.2016.16435
Acknowledgements
This study was supported by ICES, which receives funding from the Ontario Ministry of Health (MOH) and Ministry of Long-Term Care. The opinions, results, and conclusions reported in this paper are those of the authors and are independent from the funding sources. Parts of this material are based on data and/or information compiled and provided by CIHI and the Ontario MOH. The analyses, conclusions, opinions, and statements expressed herein are solely those of the authors and do not reflect those of the funding or data sources; no endorsement is intended or should be inferred. This document used data adapted from the Statistics Canada Postal CodeOM Conversion File, which is based on data licensed from Canada Post Corporation, and/or data adapted from the Ontario MOH Postal Code Conversion File, which contains data copied under license from ©Canada Post Corporation and Statistics Canada.
Disclosures
Karim Ladha and Hance Clarke are supported in part by Merit Awards from the Department of Anesthesia and Pain Medicine at the University of Toronto and are co-principal investigators of an observational study on medical cannabis funded by Shoppers Drug Mart. Tara Gomes is supported by a Tier 2 Canada Research Chair.
Funding statement
This study was funded by a grant from Canadian Institutes for Health Research (Grant # 153070). Editorial responsibility: This submission was handled by Dr. Philippe Richebé, Associate Editor, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ladha, K.S., Kitchen, S., Miles, S. et al. Use of injections for chronic pain from 2010 to 2019 in Ontario, Canada. Can J Anesth/J Can Anesth 70, 100–105 (2023). https://doi.org/10.1007/s12630-022-02357-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-022-02357-3