Abstract
Background
Steroids are often combined with local anesthetic (LA) and injected to reduce pain associated with various chronic non-cancer pain (CNCP) complaints. The biological rationale behind injection of a steroid solution is unclear, and it is uncertain whether the addition of steroids offers any additional benefits over injection of LA alone. We propose to conduct a systematic review and meta-analysis to summarize the evidence for using steroids and LA vs. LA alone in the treatment of CNCP.
Methods
An experienced librarian will perform a comprehensive search of EMBASE, MEDLINE, and the Cochrane Central Registry of Controlled Trials (CENTRAL) databases with search terms for clinical indications, LA, and steroid agents. We will review bibliographies of all relevant published reviews in the last 5 years for additional studies. Eligible trials will be published in English and randomly allocate patients with CNCP to treatment with steroid and LA injection therapy or injection with LA alone. We will use the guidelines published by the Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials (IMMPACT) to inform the outcomes that we collect and present. Teams of reviewers will independently and in duplicate assess trial eligibility, abstract data, and assess risk of bias among eligible trials. We will prioritize intention to treat analysis and, when possible, pool outcomes across trials using random effects models. We will report our findings as risk differences, weighted mean differences, or standardized mean differences for individual outcomes. Further, to ensure interpretability of our results, we will present risk differences and measures of relative effect for pain reduction based on anchor-based minimally important clinical differences. We will conduct a priori defined subgroup analyses and use the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) system to evaluate the certainty of the evidence on an outcome-by-outcome basis.
Discussion
Our review will evaluate both the effectiveness and the adverse events associated with steroid plus LA vs. LA alone for CNCP, evaluate the quality of the evidence using the GRADE approach, and prioritize patient-important outcomes guided by IMMPACT recommendations. Our results will facilitate evidence-based management of patients with chronic non-cancer pain and identify key areas for future research.
Trial registration
PROSPERO CRD42015020614
Similar content being viewed by others
Background
Burden of the problem
Chronic non-cancer pain (CNCP), defined as pain persisting beyond the period of normal healing (typically ≥3 months), is commonly experienced by a large proportion of adult population. In the USA, according to 2008 estimates, approximately 100 million adults were affected by CNCP with associated treatment costs ranging from $560 to $635 billion (US). This is greater than annual treatment costs of heart disease, cancer, or diabetes [1]. In the UK, 53 % of seniors reported that CNCP was the most important factor impacting their quality of life [2]. Chronic low back pain (CLBP) has been noted to be the leading cause of years lived with disability, with neck pain as the fourth common cause [3]. CNCP accounts for a large number of physician encounters in the elderly and aging population. In the USA alone, the proportion of CLBP patients requesting care from a health provider increased from 73.1 to 84.0 %, between 1992 and 2006 [4]. Conditions characterized or defined by the presence of pain accounted for five of the leading ten conditions associated with the most years lived with disability [5]. Common peripheral (non-axial) CNCP conditions include pain in upper or lower limbs, knee and shoulder joints, headache, carpal tunnel syndrome, epicondylitis, fascitis and others.
Treatment considerations
A clear understanding of the underlying pathogenesis of CNCP is important to drive treatment decisions; however, despite decades of research, the mechanisms underlying most CNCP conditions are unclear [5]. CNCP conditions involve a complex interplay of active pain pathways leading to sensory signaling, along with peripheral and central sensitization as a result of nervous system changes induced by temporary and long-term neuroplasticity. Changes resulting from sensitization lead to modulation of pain signals, which vary from patient to patient. Most CNCP conditions do not have definitive treatment, and physicians have limited options for symptomatic management. Analgesic medications are not always effective and need to be given on a daily basis; they also involve a risk of drug interaction especially in the elderly adult population. Corticosteroid injections (CSI) are commonly used to manage many CNCP conditions, despite variability in their clinical presentation and underlying pathophysiology. For neuraxial pain, epidural steroid injections (ESI) are the most commonly performed interventions, and in the USA alone, the number of ESIs administered to Medicare recipients essentially doubled between 2000 and 2004 (from 740,845 to 1,437,962 procedures/year) [6]. CSIs are also widely used as injections to knee [7], shoulder [8], carpal tunnel [9], nerve blocks for occipital nerve [10], suprascapular nerve [11], tendinous injections for medial and lateral epicondyle [12], and even for simple trigger point injections [13].
Percutaneous injections using steroids and local anesthetics
The rationale for injecting local anesthetics (LA) is to block sensory signals from the region being injected. Although often used for diagnosis—because it should only lead to a temporary blockade—an injection of LA has the potential to decrease sensitization, which is a feature of chronic or persistent pain, thereby possibly prolonging the treatment effect of LA beyond its pharmacological duration of action [14]. Historically, many investigators have published on the successful use of epidural injections of saline and LA. Cathelin. F, Pasquier and Leri, and Sicard published reports as early as 1901 [15]. Later, Evans (1931) published a successful report using procaine and saline in 22 of 40 patients [16]. Cyriax published multiple manuscripts referring to safe use of epidural injections using only LA and steroids in more than 20,000 cases [17, 18]. In fact, up until the 1950s, the injectate used for epidural injections in sciatica consisted of LA and saline. The first recorded use of steroids in epidural space was by Lievre et al. in 1953 [19]. Discovered by Philip Hench in the 1940s [20], glucocorticoids are potent anti-inflammatory agents. Since then, steroids have been injected for nearly every chronic pain indication [21]. In clinical practice, steroids are typically combined with LA, with or without saline [15]. This practice stems from the hope that the addition of steroid can lengthen the treatment effect [22]. For most CNCP conditions (except for evidently inflammatory conditions such as rheumatoid arthritis), there is no evidence that CSI are disease-modifying agents [23]. Whether steroids have any direct effect on pain generation or transmission is not clear. There is some experimental evidence demonstrating suppression of ectopic discharge in neuromas [24]. Pre-clinical experiments suggest that steroids may reduce neuropathic pain; however, a paradoxical effect of increased pain in some patients has also been shown [25]. Surprisingly, there are few clinical studies that have attempted to elicit the mechanism behind steroid’s effect on chronic pain other than as an anti-inflammatory [26]. Thus, the use of steroid for interventions in CNCP lacks clear rationale.
Harms of steroid injections
Corticosteroids can have systemic and local adverse effects. Systemic side effects are largely dependent upon the patient’s physiology, injected dose, and systemic absorption. Theoretically, these systemic effects can occur when the dose of steroids injected exceeds the rate of endogenous steroid production of about 20 mg per day of hydrocortisone or its equivalent and potentially cause suppression of pituitary adrenal axis, hypercorticism, Cushing’s syndrome, osteoporosis, avascular necrosis of bone, steroid myopathy, weight gain, fluid retention, and hyperglycemia [21]. Although these risks are unlikely with a single injection, in clinical practice most patients receive multiple CSI injections at frequent intervals, and it is not uncommon for patients to suffer from multiple chronic pain conditions treated with steroid injections by different physicians, without necessarily accounting for the systemic effects of steroid injected elsewhere. Local adverse effects include soft tissue atrophy, depigmentation [27], and alopecia [28]. Beyond the above recognized adverse effects, the neuraxial steroid injections (epidural, facet joint) risk causing rare, but catastrophic neurologic injuries such as stroke and spinal cord injury [29].
Limitations of previous reviews
Existing systematic reviews of injection therapy for CNCP conditions have not specifically compared LA vs. LA and steroid injections. Further, some reviews have considered LA injection to be a neutral agent, and combined this intervention with other biologically inactive control agents such as saline injections [12, 30]. More recently, within the last quarter of 2015, two additional reviews have been published. Manchikanti et al. reviewed all spinal injections targeted at epidural, facet joint/nerve, and disc pain conditions. Due to the existing heterogeneity, a meta-analysis was not considered feasible. All RCTs using an active control design were included. They observed that LA alone was as equally effective as LA with steroid, except in disc herniations [18]. The review by Chou et al. also focussed only on epidural injections for radiculopathy and spinal stenosis, without any restriction for the agent used and duration of chronic pain. They combined LA along with saline as placebo comparator. Their results showed a small effect favoring the use of steroids only in radiculopathy for short-term reduction in pain and function [31]. To illustrate these issues, we reviewed the systematic reviews published in English within the last 5 years, focusing on injection therapies using CSI for CNCP conditions. We identified the findings and limitations of those reviews, apart from identifying whether they included trials that addressed our review question of comparing LA and steroid with LA alone for CNCP (Table 1). Twenty seven out of forty-two reviews included trials comparing LA and steroid with LA alone [6, 12, 18, 30–53], but only some reviews have made clear observations on the comparison between LA vs. LA and steroid [18, 33, 38, 41, 45, 48, 51]. Very few conducted meta-analyses [12, 31–33, 35, 39, 41, 45, 48, 51]. The question of whether the injected steroid has any clinical benefit beyond that achieved from LA alone is an area of active debate, as existing studies across various clinical categories have shown equivalent effects comparing LA and steroid vs. only LA [54–57]. Findings from our review will help inform physicians, healthcare providers, and CNCP patients on whether the addition of steroid gives any meaningful benefit to LA injection alone.
Objectives
Our primary objective is to perform a systematic review and meta-analysis to assess the effectiveness of steroid + LA injections compared to LA injections, for pain relief among CNCP patients. Secondary objectives of our review are
-
To assess the effect of steroid + LA injections compared to LA injections alone on the duration of effect of pain relief.
-
To assess the effect of steroid + LA injections compared to LA injections alone on six core domains, described as core outcome measures by the Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials (IMMPACT) [58]. The domains other than reduction of pain include physical functioning; emotional functioning; participant ratings of global improvement and satisfaction with treatment, symptoms and adverse effects, and participant disposition.
Study question
Among adults with CNCP, does LA with corticosteroid injection (with or without saline) offer better pain relief when compared to injection with LA alone (with or without saline), as assessed at a time closest to 4 weeks after treatment?
Methods
Our review protocol has been registered with PROSPERO (registration number PROSPERO 2015:CRD42015020614). This protocol has been prepared for publication according to PRISMA-P guidelines [59].
Eligibility criteria
Participants
We will include adult (≥18 years of age) patients with CNCP, and exclude patients with a known inflammatory cause of pain such as rheumatoid arthritis, ankylosing spondylitis, systemic lupus erythematosus and gouty arthritis, and pain of generalized nature such as fibromyalgia or chronic fatigue syndrome. If a trial involves a mix of cancer and CNCP, or adult and pediatric patients, we will include the study only if they report outcomes separately for our study population of interest, or if at least 90 % of the trial patients are >18 years with CNCP.
Studies
Parallel design, randomized controlled trials (RCTs) will be eligible for our review. We will exclude trials with crossover design, N of 1 trials, and non-therapeutic trials.
Interventions
Eligible studies must randomize patients to receive LA + steroid or LA only, with or without saline, administered as percutaneous injection. We will exclude trials in which injections involve any additional agent (e.g., Hyaluronidase, dextrose, plasma), and any injection which involves a co-interventional procedure (e.g., radiofrequency treatment, epidurolysis).
Information sources
We will search the following electronic databases, from its inception till our search date: EMBASE, MEDLINE, and the Cochrane Central Registry of Controlled Trials (CENTRAL). Our search will not be limited to language. We will record the time and date of the literature search performed on each database. As a supplementary search, we will search the WHO clinical trial registry (http://apps.who.int/trialsearch/Default.aspx), and clinical trial registry (https://clinicaltrials.gov/), to look for any registered studies, which fulfill our eligibility criteria, and crosscheck for published results. Unpublished, but completed, study results will be requested from the authors or investigators. To further ensure comprehensiveness, we will review the bibliographies of relevant reviews published in English over the last 5 years (shown in Table 1).
Search strategy
The search will be performed using a sensitive strategy, prepared by an experienced librarian (RC), for each specific database, based in part on a comprehensive list of CNCP indications for which CSI are commonly utilized. The search terms will include possible indications, along with terms identifying corticosteroids, and LAs (Additional file 1).
Study records
Data management
We will conduct our review using an online software tool specially optimized to conduct systematic reviews—DistillerSR (https://distillercer.com/).
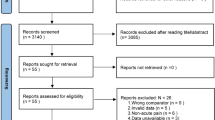
Study screening and selection
Studies fulfilling our eligibility criteria will be selected through a two-level screening process using standardized forms, applied through DistillerSR. At each stage, paired reviewers trained in health research methods will screen for studies for eligibility, independently and in duplicate. The first level will be done on titles and available abstracts of identified citations. For citations judged as potentially eligible, full-text article screening will be done. To ensure consistency, reviewers will perform a calibration exercise, before beginning with screening. Reviewers will be asked to resolve disagreement by consensus, or if a discrepancy remains, through discussion with an arbitrator (HS). A quadratic kappa statistic will be calculated as a measure of inter-observer agreement, independent of chance regarding study eligibility and interpreted as almost perfect agreement (0.81–0.99), substantial agreement (0.61–0.80), moderate agreement (0.41–0.60), fair agreement (0.21–0.40), slight agreement (0.01–0.20), <0 as less than chance agreement [60].
Data collection process
Reviewers working in pairs will extract the required data from each included study using a standardized data extraction form using DistillerSR (https://distillercer.com/). This form will be piloted between all pairs of reviewers for consistency and accuracy. To assist with the data extraction, a detailed instruction manual will be provided along with each relevant form.
Data items
Data abstracted will include study characteristics including risk of bias items, demographic information, participant flow through the study, and outcomes on continuous and binary measures captured on six core domains as recommended by the IMMPACT statement guidelines [58].
Outcomes and prioritization
We will consider pain relief as our primary outcome. We will also capture other outcomes (as guided by IMMPACT) including reporting of adverse effects. We will also prioritize the use of intention to treat analysis (ITT). We will only pool data across trials if there are three or more studies contributing to an outcome domain. It is recognized that presentation of relative effects will facilitate interpretation of treatment effects, and clinicians generally find dichotomous presentation of continuous outcomes more useful [61]. In the following section, we will explain the method of analysis as considered for pain relief. We will perform a similar analysis, as appropriate, for other IMMPACT outcomes.
Data synthesis and analysis of outcomes
We expect that all included trials will have captured a measure of pain relief, and this domain could be expressed in any of the following types: outcomes reported as binary (successful or not successful), outcomes reported in ordinal categorical scale (mild, moderate and severe), and outcomes reported in various continuous outcome scales. For the primary outcome, we will consider the outcomes reported closest to 4 weeks after the study interventions. Pain relief measured at this time will give us indication of treatment efficacy beyond the effects of placebo. For the primary analysis, we will use a complete case analysis with ITT. Analysis and synthesis will be done using revman (review manager) 5.3. Using random effects model for pooling, we will calculate the risk ratio (to be interpreted as the risk of having success) for dichotomous outcomes and weighted mean difference (WMD) for continuous outcomes converted into 0–10 (11 point) numerical rating scale (NRS) for pain. Further, we will dichotomize all included patients into proportion of successful patients for pain relief, to be able to report risk ratio across all included studies. However, dichotomising continuous outcomes will result in a loss of statistical power. Hence, we will also report the WMD. To achieve this, we will be performing the following methodological steps.
-
1.
Converting outcomes reported in various continuous scales to a reference instrument scale of 0 to 10 NRS: According to IMMPACT, the 11-point NRS measure of pain intensity is recommended as a core outcome measure in clinical trials of chronic pain treatments. Furthermore, the 0–10 NRS is preferred over the VAS (visual analog scale) by patients and clinicians for its relative simplicity and ease of administration [58].
-
2.
Converting continuous outcomes from 0–10 NRS into dichotomous data. A reduction of two points on the 0–10 NRS could be considered as the threshold to establish minimally important difference (MID), reflecting an average reduction of pain by 30 % [58, 62]. For studies, which report only end scores, we will consider a threshold of 4 or less in a 0–10 NRS, to dichotomize the patients. A score of 4 or less is considered as mild pain [63].
-
3.
Converting categorical measurement results to a dichotomous data. The categories of ordinal scale commonly used in pain studies could include mild, moderate and severe pain. It has been shown that these categories correspond to the following thresholds of 0–10 NRS. Mild pain 0–4, moderate pain 5–7, and severe pain 8–10 [63]. Any change from a higher ordinal category to a lower ordinal category would be considered as a successful outcome for patients reported in a particular study, allowing us to dichotomize the study outcomes into success and failures for each arm.
-
4.
Imputation for participants treated as lost to follow up for continuous and dichotomous outcomes (for sensitivity analyses). We will consider patient LTFU subsequent to randomization as missing for data analysis, and will be explored further for imputation, if it is >5 %. For trials in which the authors report total missing participant data only, without specifying at what stage the participants were missing, we will consider the total sample size and the actual sample size included for final analysis and assume that missing data were equally distributed between the arms. For trials in which the authors reported imputed analysis only, we will use the imputed results for the meta-analysis. We will perform imputational strategies as described by Ebrahim et al. [64] and Akl et al. [65], for continuous measures and dichotomous measures, respectively.
For secondary outcomes, we will pool the outcomes for other IMMPACT domains using a random effects model only if there are three or more studies for a particular domain. We will report the pooled outcome as WMD or standardized mean difference (SMD) as appropriate.
Risk of bias assessment and identification
Each included study will be assessed for risk of bias at the study level, using the Cochrane risk of bias tool, based on the components of random sequence generation, allocation concealment, blinding of participants, blinding of outcome assessment, incomplete outcome data, and selective outcome reporting. We will use a modified Cochrane risk of bias instrument, with response options of “definitely yes,” “probably yes,” “probably no,” and “definitely no.” We will assign trials in the “definitely yes” and “probably yes” categories a high risk of bias and those in the “probably no” and “definitely no” categories a low risk of bias. These items for each study will be extracted, in duplicate, during the data extraction stage, using the DistillerSR web tool. Any disagreement on the risk of bias item scoring will be noted and arbitrated by the primary investigator (HS). Agreement on risk of bias scoring will be assessed on a component-by-component basis, using quadratic kappa weighting and interpreted as stated before. No study will be excluded based on its risk of bias. We will contact study authors if limitations in reporting lead to uncertainties in eligibility, risk of bias, or outcome.
Assessment of heterogeneity
Statistical heterogeneity will be calculated using Cochrane’s Q test, with a threshold of p value at 0.10, and I 2 statistic to describe the percentage variability in individual effect estimates that could be due to true differences between the studies rather than a sampling error.
Subgroup and sensitivity analysis to explore heterogeneity
The following a priori hypotheses would be considered for subgroup analyses, and as possible reasons for unexplained heterogeneity in the pooled estimates. The subgroup analysis will only be done if there are more than two studies per subgroup.
-
1.
Clinical category level subgroup analysis. Although, the underlying rationale that adding steroids to LA may not provide any meaningful improvement to pain reduction is consistent across all clinical indications and trials, there is potential for clinical heterogeneity in these conditions because of the variation in underlying pain pathways, pain sensitization, and hence the possibility of varying effects of steroids. Considering this, we will perform subgroup analysis of pain outcomes based on target structures injected. The seven clinical categories considered are as follows.
-
1.
Peripheral joint: hip, knee, shoulder joint injections, and other joint injections.
-
2.
Spinal joint/facet nerve (medial branch block)/ spinal disc: Facet joint or disc injections.
-
3.
Spinal nerve or epidural or intrathecal: Epidural injections including transforaminal epidural.
-
4.
Peripheral nerve: various nerves including occipital nerve, suprascapular, and median nerve.
-
5.
Autonomic ganglia: injections to stellate ganglia, celiac plexus, lumbar sympathetic block.
-
6.
Soft tissue injection: injections for lateral or medial elbow ligaments, subacromial bursa, or plantar fascia.
-
7.
Trigger point or intramuscular: injections to trigger point, piriformis muscle, or any other intramuscular injections.
-
1.
-
2.
Larger effects toward steroids could be observed in studies with components of higher risk of bias; we will conduct this subgroup analysis on a risk of bias component-by-component basis, only if there is considerable variability within the risk of bias component.
-
3.
Sensitivity analysis for LTFU will be conducted as described previously.
-
4.
Studies which involved treatment interventions as a series, rather one specific injection (for example, three steroid injections over 1 month). We anticipate that the direction of effect would favor the steroid treatment due to systemic additive effect.
Addressing potential biases
Publication bias will be assessed using a funnel plot, if there are more than ten studies included in a meta-analysis. Further, it will be explored by the test of Egger [66]. Selective outcome reporting is difficult to identify when the study protocols are not available or published. For our review, we will consider the possibility of selective outcome reporting, when the outcomes are described in the Methods section but not identified or reported in the results section of the same study report [67].
Interpretation and reporting
We will report our findings as risk ratios, WMD, or SMD for individual outcomes, along with their 95 % confidence intervals. Within each clinical category (subgroups), similar findings will be reported. We will also report the outcome for pain relief as a single pooled estimate of risk ratio by dichotomising the continuous outcomes. This method has been suggested as appropriate and meaningful for interpretation in systematic reviews of pain studies [54]. We will also report the findings in measures of relative risk reduction and absolute risk reduction. Rating of quality of evidence will also be done using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach. This will enable us to report our study findings in the form of “summary of findings” table and allow us to evaluate the certainty in effect estimates.
Discussion
Despite the several advances in the field of chronic pain, we still do not fully understand the nature and mechanisms causing CNCP. Although steroids are being used in nearly every injection or interventional therapy, the reasons for its use are unclear. Our comprehensive systematic review will assess the clinical benefits of steroids when used along with LA, by comparing it with the effects of LA alone. This evaluation of both the effectiveness and the adverse events will include patient-important outcomes as outlined in IMMPACT recommendations, thereby enhancing comparability and external validity. Our results will facilitate evidence-based management of patients with chronic non-cancer pain and identify key areas for future research.
The review as such will be limited by the included studies and their quality. As highlighted above, we will attempt to decrease the potential for bias by performing reasonable subgroup and sensitivity analysis, including imputation for missed outcomes.
Abbreviations
- CLBP:
-
chronic low back pain
- CNCP:
-
chronic non-cancer pain
- CSI:
-
corticosteroid injections
- ESI:
-
epidural steroid injections
- IA:
-
intra-articular injection
- IMMPACT:
-
Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials
- ITT:
-
intention to treat
- LA:
-
local anesthetics
- LE:
-
lateral epicondylitis
- LTFU:
-
loss to follow up
- ME:
-
medial epicondylitis
- MID:
-
minimally important difference
- NRS:
-
numerical rating scale
- OS:
-
observational study
- PNB:
-
peripheral nerve block
- RCT:
-
randomized controlled trials
- RD:
-
risk difference
- SMD:
-
standardized mean difference
- TFESI:
-
transforaminal epidural steroid injection
- TPI:
-
trigger point injection
- VAS:
-
visual analog scale
- WMD:
-
weighted mean difference
References
Gaskin DJ, Richard P. The economic costs of pain in the United States. J Pain. 2012;13(8):715–24.
Parker L, Moran GM, Roberts LM, Calvert M, McCahon D. The burden of common chronic disease on health-related quality of life in an elderly community-dwelling population in the UK. Fam Pract. 2014;31(5):557–63.
Murray CJ, Atkinson C, Bhalla K, Birbeck G, Burstein R, Chou D, et al. The state of US health, 1990–2010: burden of diseases, injuries, and risk factors. Jama. 2013;310(6):591–608.
Freburger JK, Holmes GM, Agans RP, Jackman AM, Darter JD, Wallace AS, et al. The rising prevalence of chronic low back pain. Arch Intern Med. 2009;169(3):251–8.
Hooten WM, Cohen SP, Rathmell JP. Introduction to the Symposium on Pain Medicine. Mayo Clin Proc. 2015;90(1):4–5.
Pinto RZ, Maher CG, Ferreira ML, Hancock M, Oliveira VC, McLachlan AJ, et al. Epidural corticosteroid injections in the management of sciatica: a systematic review and meta-analysis. Ann Intern Med. 2012;157(12):865–77.
Arroll B, Goodyear-Smith F. Corticosteroid injections for osteoarthritis of the knee: meta-analysis. BMJ (Clinical research ed). 2004;328(7444):869.
Buchbinder R, Green S, Youd JM. Corticosteroid injections for shoulder pain. Cochrane Database Syst Rev. 2003;1:CD004016.
Marshall S, Tardif G, Ashworth N. Local corticosteroid injection for carpal tunnel syndrome. Cochrane Database Syst Rev. 2007;2:CD001554.
Leroux E, Valade D, Taifas I, Vicaut E, Chagnon M, Roos C, et al. Suboccipital steroid injections for transitional treatment of patients with more than two cluster headache attacks per day: a randomised, double-blind, placebo-controlled trial. Lancet Neurol. 2011;10(10):891–7.
Shanahan EM, Ahern M, Smith M, Wetherall M, Bresnihan B, FitzGerald O. Suprascapular nerve block (using bupivacaine and methylprednisolone acetate) in chronic shoulder pain. Ann Rheum Dis. 2003;62(5):400–6.
Coombes BK, Bisset L, Vicenzino B. Efficacy and safety of corticosteroid injections and other injections for management of tendinopathy: a systematic review of randomised controlled trials. Lancet. 2010;376(9754):1751–67.
Cummings TM, White AR. Needling therapies in the management of myofascial trigger point pain: a systematic review. Arch Phys Med Rehabil. 2001;82(7):986–92.
Arner S, Lindblom U, Meyerson BA, Molander C. Prolonged relief of neuralgia after regional anesthetic blocks. A call for further experimental and systematic clinical studies. Pain. 1990;43(3):287–97.
Kepes ER, Duncalf D. Treatment of backache with spinal injections of local anesthetics, spinal and systemic steroids. A review Pain. 1985;22(1):33–47.
Evans W. Intrasacral epidural injection in the treatment of sciatica. The Lancet. 1930;216(5597):1225–9.
Coomes EN. A comparison between epidural anaesthesia and bed rest in sciatica. Br Med J. 1961;1(5218):20–4.
Manchikanti L, Nampiaparampil DE, Manchikanti KN, Falco FJ, Singh V, Benyamin RM, et al. Comparison of the efficacy of saline, local anesthetics, and steroids in epidural and facet joint injections for the management of spinal pain: A systematic review of randomized controlled trials. Surgical neurology international. 2015;6 Suppl 4:S194–235.
Cohen SP, Bicket MC, Jamison D, Wilkinson I, Rathmell JP. Epidural steroids: a comprehensive, evidence-based review. Reg Anesth Pain Med. 2013;38(3):175–200.
Hench PS, Kendall EC, et al. The effect of a hormone of the adrenal cortex (17-hydroxy-11-dehydrocorticosterone; compound E) and of pituitary adrenocorticotropic hormone on rheumatoid arthritis. Proc Staff Meet Mayo Clin. 1949;24(8):181–97.
Wong SH, Wong CS, Li TT. Steroids in regional analgesia. Expert Opin Pharmacother. 2010;11(17):2839–48.
Stevens T, Costanzo A, Lopez R, Kapural L, Parsi MA, Vargo JJ. Adding triamcinolone to endoscopic ultrasound-guided celiac plexus blockade does not reduce pain in patients with chronic pancreatitis. Clin Gastroenterol Hepatol. 2012;10(2):186–91. 91 e1.
Uthman I, Raynauld JP, Haraoui B. Intra-articular therapy in osteoarthritis. Postgrad Med J. 2003;79(934):449–53.
Devor M, Govrin-Lippmann R, Raber P. Corticosteroids suppress ectopic neural discharge originating in experimental neuromas. Pain. 1985;22(2):127–37.
Rijsdijk M, van Wijck AJ, Kalkman CJ, Yaksh TL. The effects of glucocorticoids on neuropathic pain: a review with emphasis on intrathecal methylprednisolone acetate delivery. Anesth Analg. 2014;118(5):1097–112.
Caldwell JR. Intra-articular corticosteroids. Guide to selection and indications for use. Drugs. 1996;52(4):507–14.
Papadopoulos PJ, Edison JD. The Clinical Picture - Soft tissue atrophy after corticosteroid injection. Cleve Clin J Med. 2009;76(6):373–4.
Lambru G, Lagrata S, Matharu MS. Cutaneous atrophy and alopecia after greater occipital nerve injection using triamcinolone. Headache. 2012;52(10):1596–9.
Rathmell JP, Benzon HT, Dreyfuss P, Huntoon M, Wallace M, Baker R, et al. Safeguards to prevent neurologic complications after epidural steroid injections: consensus opinions from a multidisciplinary working group and national organizations. Anesthesiology. 2015;122(5):974–84.
Engel A, King W, MacVicar J. The effectiveness and risks of fluoroscopically guided cervical transforaminal injections of steroids: a systematic review with comprehensive analysis of the published data. Pain medicine (Malden, Mass). 2014;15(3):386–402.
Chou R, Hashimoto R, Friedly J, Fu R, Bougatsos C, Dana T, et al. Epidural Corticosteroid Injections for Radiculopathy and Spinal Stenosis: A Systematic Review and Meta-analysis. Ann Intern Med. 2015;163(5):373–81.
Arroll B, Goodyear-Smith F. Corticosteroid injections for painful shoulder: a meta-analysis. Br J Gen Pract. 2005;55(512):224–8.
Benyamin RM, Manchikanti L, Parr AT, Diwan S, Singh V, Falco FJ, et al. The effectiveness of lumbar interlaminar epidural injections in managing chronic low back and lower extremity pain. Pain Physician. 2012;15(4):E363–404.
Benyamin RM, Wang VC, Vallejo R, Singh V, Helm IS. A systematic evaluation of thoracic interlaminar epidural injections. Pain Physician. 2012;15(4):E497–514.
Bicket MC, Gupta A, Brown CH, Cohen SP. Epidural injections for spinal pain: a systematic review and meta-analysis evaluating the "control" injections in randomized controlled trials. Anesthesiology. 2013;119(4):907–31.
Bicket MC, Horowitz JM, Benzon HT, Cohen SP. Epidural injections in prevention of surgery for spinal pain: systematic review and meta-analysis of randomized controlled trials. The spine journal : official journal of the North American Spine Society. 2015;15(2):348–62.
Bresnahan BW, Rundell SD, Dagadakis MC, Sullivan SD, Jarvik JG, Nguyen H, et al. A systematic review to assess comparative effectiveness studies in epidural steroid injections for lumbar spinal stenosis and to estimate reimbursement amounts. PM & R : the journal of injury, function, and rehabilitation. 2013;5(8):705–14.
Diwan S, Manchikanti L, Benyamin RM, Bryce DA, Geffert S, Hameed H, et al. Effectiveness of cervical epidural injections in the management of chronic neck and upper extremity pain. Pain Physician. 2012;15(4):E405–34.
Quraishi NA. Transforaminal injection of corticosteroids for lumbar radiculopathy: systematic review and meta-analysis. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2012;21(2):214–9.
Ashkenazi A, Blumenfeld A, Napchan U, Narouze S, Grosberg B, Nett R, et al. Peripheral nerve blocks and trigger point injections in headache management - a systematic review and suggestions for future research. Headache. 2010;50(6):943–52.
Bhatia A, Flamer D, Shah PS. Perineural steroids for trauma and compression-related peripheral neuropathic pain: a systematic review and meta-analysis. Canadian journal of anaesthesia = Journal canadien d'anesthesie. 2015;62(6):650–62.
Buenaventura RM, Datta S, Abdi S, Smith HS. Systematic review of therapeutic lumbar transforaminal epidural steroid injections. Pain Physician. 2009;12(1):233–51.
Keith MW, Masear V, Amadio PC, Andary M, Barth RW, Graham B, et al. Treatment of carpal tunnel syndrome. J Am Acad Orthop Surg. 2009;17(6):397–405.
Koester MC, Dunn WR, Kuhn JE, Spindler KP. The efficacy of subacromial corticosteroid injection in the treatment of rotator cuff disease: A systematic review. J Am Acad Orthop Surg. 2007;15(1):3–11.
Krogh TP, Bartels EM, Ellingsen T, Stengaard-Pedersen K, Buchbinder R, Fredberg U, et al. Comparative effectiveness of injection therapies in lateral epicondylitis: a systematic review and network meta-analysis of randomized controlled trials. Am J Sports Med. 2013;41(6):1435–46.
Kruse DW. Intraarticular cortisone injection for osteoarthritis of the hip. Is it effective? Is it safe? Current reviews in musculoskeletal medicine. 2008;1(3–4):227–33.
Manchikanti KN, Atluri S, Singh V, Geffert S, Sehgal N, Falco FJ. An update of evaluation of therapeutic thoracic facet joint interventions. Pain Physician. 2012;15(4):E463–81.
Olaussen M, Holmedal O, Lindbaek M, Brage S, Solvang H. Treating lateral epicondylitis with corticosteroid injections or non-electrotherapeutical physiotherapy: a systematic review. BMJ open. 2013;3(10):e003564.
Roberts ST, Willick SE, Rho ME, Rittenberg JD. Efficacy of lumbosacral transforaminal epidural steroid injections: a systematic review. PM & R : the journal of injury, function, and rehabilitation. 2009;1(7):657–68.
Sims SE, Miller K, Elfar JC, Hammert WC. Non-surgical treatment of lateral epicondylitis: a systematic review of randomized controlled trials. Hand (New York, NY). 2014;9(4):419–46.
Smidt N, Assendelft WJ, van der Windt DA, Hay EM, Buchbinder R, Bouter LM. Corticosteroid injections for lateral epicondylitis: a systematic review. Pain. 2002;96(1–2):23–40.
Tobin J, Flitman S. Occipital nerve blocks: when and what to inject? Headache. 2009;49(10):1521–33.
Falco FJ, Manchikanti L, Datta S, Sehgal N, Geffert S, Onyewu O, et al. An update of the effectiveness of therapeutic lumbar facet joint interventions. Pain Physician. 2012;15(6):E909–53.
Busse JW, Bartlett SJ, Dougados M, Johnston BC, Guyatt GH, Kirwan JR et al. Optimal Strategies for Reporting Pain in Clinical Trials and Systematic Reviews: Recommendations from an OMERACT 12 Workshop. The Journal of rheumatology. 2015.
Wolf JM, Ozer K, Scott F, Gordon MJ, Williams AE. Comparison of autologous blood, corticosteroid, and saline injection in the treatment of lateral epicondylitis: a prospective, randomized, controlled multicenter study. J Hand Surg Am. 2011;36(8):1269–72.
Misirlioglu TO, Akgun K, Palamar D, Erden MG, Erbilir T. Piriformis syndrome: comparison of the effectiveness of local anesthetic and corticosteroid injections: a double-blinded, randomized controlled study. Pain Physician. 2015;18(2):163–71.
Friedly JL, Comstock BA, Turner JA, Heagerty PJ, Deyo RA, Sullivan SD, et al. A randomized trial of epidural glucocorticoid injections for spinal stenosis. N Engl J Med. 2014;371(1):11–21.
Dworkin RH, Turk DC, Farrar JT, Haythornthwaite JA, Jensen MP, Katz NP, et al. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain. 2005;113(1–2):9–19.
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ (Clinical research ed). 2015;349:g7647.
Viera AJ, Garrett JM. Understanding interobserver agreement: the kappa statistic. Fam Med. 2005;37(5):360–3.
Forrow L, Taylor WC, Arnold RM. Absolutely relative: how research results are summarized can affect treatment decisions. Am J Med. 1992;92(2):121–4.
Farrar JT, Young Jr JP, LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94(2):149–58.
Jones KR, Vojir CP, Hutt E, Fink R. Determining mild, moderate, and severe pain equivalency across pain-intensity tools in nursing home residents. J Rehabil Res Dev. 2007;44(2):305–14.
Ebrahim S, Johnston BC, Akl EA, Mustafa RA, Sun X, Walter SD, et al. Addressing continuous data measured with different instruments for participants excluded from trial analysis: a guide for systematic reviewers. J Clin Epidemiol. 2014;67(5):560–70.
Akl EA, Johnston BC, Alonso-Coello P, Neumann I, Ebrahim S, Briel M, et al. Addressing dichotomous data for participants excluded from trial analysis: a guide for systematic reviewers. PLoS One. 2013;8(2):e57132.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ (Clinical research ed). 1997;315(7109):629–34.
Chan AW, Altman DG. Identifying outcome reporting bias in randomised trials on PubMed: review of publications and survey of authors. BMJ (Clinical research ed). 2005;330(7494):753.
Benny BV, Patel MY. Predicting epidural steroid injections with laboratory markers and imaging techniques. The spine journal : official journal of the North American Spine Society. 2014;14(10):2500–8.
Wijayasinghe N, Andersen KG, Kehlet H. Neural blockade for persistent pain after breast cancer surgery. Reg Anesth Pain Med. 2014;39(4):272–8.
Colen S, Geervliet P, Haverkamp D, Van Den Bekerom MP. Intra-articular infiltration therapy for patients with glenohumeral osteoarthritis: A systematic review of the literature. International journal of shoulder surgery. 2014;8(4):114–21.
Song A, Higgins LD, Newman J, Jain NB. Glenohumeral corticosteroid injections in adhesive capsulitis: a systematic search and review. PM & R : the journal of injury, function, and rehabilitation. 2014;6(12):1143–56.
Dorleijn DM, Luijsterburg PA, Bierma-Zeinstra SM, Bos PK. Is anesthetic hip joint injection useful in diagnosing hip osteoarthritis? A meta-analysis of case series. J Arthroplasty. 2014;29(6):1236–42. e1.
Rinkel WD, Schreuders TA, Koes BW, Huisstede BM. Current evidence for effectiveness of interventions for cubital tunnel syndrome, radial tunnel syndrome, instability, or bursitis of the elbow: a systematic review. Clin J Pain. 2013;29(12):1087–96.
Louwerens JK, Sierevelt IN, van Noort A, van den Bekerom MP. Evidence for minimally invasive therapies in the management of chronic calcific tendinopathy of the rotator cuff: a systematic review and meta-analysis. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons [et al]. 2014;23(8):1240–9.
Aaron DL, Patel A, Kayiaros S, Calfee R. Four common types of bursitis: diagnosis and management. J Am Acad Orthop Surg. 2011;19(6):359–67.
Lu Y, Guzman JZ, Purmessur D, Iatridis JC, Hecht AC, Qureshi SA, et al. Nonoperative management of discogenic back pain: a systematic review. Spine. 2014;39(16):1314–24.
Malik KM, Cohen SP, Walega DR, Benzon HT. Diagnostic criteria and treatment of discogenic pain: a systematic review of recent clinical literature. Spine J. 2013;13(11):1675–89.
Annaswamy TM, De Luigi AJ, O'Neill BJ, Keole N, Berbrayer D. Emerging concepts in the treatment of myofascial pain: a review of medications, modalities, and needle-based interventions. Pm r. 2011;3(10):940–61.
Scott NA, Guo B, Barton PM, Gerwin RD. Trigger point injections for chronic non-malignant musculoskeletal pain: a systematic review. Pain medicine (Malden, Mass). 2009;10(1):54–69.
Anderberg L, Annertz M, Persson L, Brandt L, Säveland H. Transforaminal steroid injections for the treatment of cervical radiculopathy: A prospective and randomised study. Eur Spine J. 2007;16:321–8.
Béliveau P. A comparison between epidural anaesthesia with and without corticosteroid in the treatment of sciatica. Rheumatol Phys Med. 1971;11:40–3.
Breivik H, Hesla PE, Molnar I, Lind B. Treatment of chronic low back pain and sciatica. Comparison of caudal epidural injections of bupivacaine and methylprednisolone with bupivacaine followed by saline. Adv Pain Res Therapy. 1976;1:927–32.
Cohen SP, White RL, Kurihara C, Larkin TM, Chang A, Griffith SR, et al. Epidural steroids, etanercept, or saline in subacute sciatica: A multicenter, randomized trial. Ann Intern Med. 2012;156:551–9.
Cuckler JM, Bernini PA, Wiesel SW, Booth Jr RE, Rothman RH, Pickens GT. The use of epidural steroids in the treatment of lumbar radicular pain. A prospective, randomized, doubleblind study. J Bone Joint Surg Am. 1985;67:63–6.
Ghahreman A, Ferch R, Bogduk N. The efficacy of transforaminal injection of steroids for the treatment of lumbar radicular pain. Pain Med. 2010;11:1149–68.
Klenerman L, Greenwood R, Davenport HT, White DC, Peskett S. Lumbar epidural injections in the treatment of sciatica. Br J Rheumatol. 1984;23:35–8.
Manchikanti L, Singh V, Cash KA, Pampati V, Damron KS, Boswell MV. Preliminary results of a randomized, equivalence trial of fluoroscopic caudal epidural injections in managing chronic low back pain: Part 2—Disc herniation and radiculitis. Pain Physician. 2008;11:801–15.
Manchikanti L, Cash KA, McManus CD, Pampati V, Smith HS. One-year results of a randomized, double-blind, active controlled trial of fluoroscopic caudal epidural injections with or without steroids in managing chronic discogenic low back pain without disc herniation or radiculitis. Pain Physician. 2011;14:25–6.
Manchikanti L, Malla Y, Cash KA, McManus CD, Pampati V. Fluoroscopic cervical interlaminar epidural injections in managing chronic pain of cervical postsurgery syndrome: Preliminary results of a randomized, double-blind, active control trial. Pain Physician. 2012;15:13–5.
Manchikanti L, Cash KA, McManus CD, Pampati V, Fellows B. Results of 2-year follow-up of a randomized, double-blind, controlled trial of fluoroscopic caudal epidural injections in central spinal stenosis. Pain Physician. 2012;15:371–84.
Manchikanti L, Cash KA, McManus CD, Damron KS, Pampati V, Falco FJ. Lumbar interlaminar epidural injections in central spinal stenosis: Preliminary results of a randomized, double-blind, active control trial. Pain Physician. 2012;15:51–3.
Manchikanti L, Malla Y, Cash KA, McManus CD, Pampati V. Fluoroscopic epidural injections in cervical spinal stenosis: Preliminary results of a randomized, double-blind, active control trial. Pain Physician. 2012;15:E59–70.
Nam HS, Park YB. Effects of transforaminal injection for degenerative lumbar scoliosis combined with spinal stenosis. Ann Rehabil Med. 2011;35:514–23.
Ng L, Chaudhary N, Sell P. The efficacy of corticosteroids in periradicular infiltration for chronic radicular pain: A randomized, double-blind, controlled trial. Spine (Phila Pa 1976). 2005;30:857–62.
Rogers P, Nash T, Schiller D, Norman J. Epidural steroids for sciatica. Pain Clinic. 1992;5:67–2.
Sayegh FE, Kenanidis EI, Papavasiliou KA, Potoupnis ME, Kirkos JM, Kapetanos GA. Efficacy of steroid and nonsteroid caudal epidural injections for low back pain and sciatica: A prospective, randomized, double-blind clinical trial. Spine (Phila Pa 1976). 2009;34:1441–7.
Tafazal S, Ng L, Chaudhary N, Sell P. Corticosteroids in peri-radicular infiltration for radicular pain: A randomised double blind controlled trial. One year results and subgroup analysis. Eur Spine J. 2009;18:1220–5.
Fukusaki M, Kobayashi I, Hara T, Sumikawa K. Symptoms of spinal stenosis do not improve after epidural steroid injection. Clin J Pain. 1998;14:148–51.
El Zahaar M. The value of caudal epidural steroids in the treatment of lumbar neural compression syndromes. J Neurol Orthop Med Surg. 1991;12:181–4.
Manchikanti L, Cash KA, Pampati V, Wargo BW, Malla Y. The effectiveness of fluoroscopic cervical interlaminar epidural injections in managing chronic cervical disc herniation and radiculitis: Preliminary results of a randomized, double-blind, controlled trial. Pain Physician. 2010;13:223–36.
Manchikanti L, Cash KA, Pampati V, Malla Y. Fluoroscopic cervical epidural injections in chronic axial or discogenic neck pain without disc herniation or facet joint pain or radiculitis. J Pain Res. 2012;5:227–36.
Manchikanti L, Singh V, Cash KA, Pampati V, Damron KS, Boswell MV. Effect of fluoroscopically guided caudal epidural steroid or local anesthetic injections in the treatment of lumbar disc herniation and radiculitis: a randomized, controlled, double blind trial with a two-year follow-up. Pain Physician. 2012;15(4):273–86.
Manchikanti L, Cash KA, McManus CD, Pampati V, Benyamin RM. A randomized, double-blind, active-controlled trial of fluoroscopic lumbar interlaminar epidural injections in chronic axial or discogenic low back pain: results of 2-year follow-up. Pain Physician. 2013;16(5):E491–504.
Hegihara Y, Ogata S, Hirayama H, Koyama T, Watanabe E. Why use steroids in lumbar selective nerve root block? A randomized control study. Chiba Med J. 2009;85:71–6.
Riew KD, Yin Y, Gilula L, Bridwell KH, Lenke LG, Lauryssen C, et al. The effect of nerve-root injections on the need for operative treatment of lumbar radicular pain. A prospective, randomized, controlled, double-blind study. J Bone Joint Surg Am. 2000;82-A:1589–93.
Swerdlow M, Sayle-Creer WS. A study of extradural medication in the relief of the lumbosciatic syndrome. Anaesthesia. 1970;25:341–5.
Manchikanti L, Singh V, Cash KA, Pampati V, Damron KS, Boswell MV. A randomized, controlled, double-blind trial of fluoroscopic caudal epidural injections in the treatment of lumbar disc herniation and radiculitis. Spine (Phila Pa 1976). 2011;36:1897–905.
Manchikanti L, Singh V, Falco FJ, Cash KA, Pampati V. Evaluation of the effectiveness of lumbar interlaminar epidural injections in managing chronic pain of lumbar disc herniation or radiculitis: a randomized, double-blind, controlled trial. Pain Physician. 2010;13:343–55.
Manchikanti L, Cash KA, McManus CD, Pampati V, Benyamin RM. A preliminary report of a randomized double-blind, active controlled trial of fluoroscopic thoracic interlaminar epidural injections in managing chronic thoracic pain. Pain Physician. 2010;13(6):E357–69.
Riew KD, Park JB, Cho YS, Gilula L, Patel A, Lenke LG, et al. Nerve root blocks in the treatment of lumbar radicular pain. A minimum five-year follow-up. J Bone Joint Surg Am. 2006;88:1722–5.
Karadas O, Tok F, Akarsu S, Tekin L, Balaban B. Triamcinolone acetonide vs procaine hydrochloride injection in the management of carpal tunnel syndrome: randomized placebo-controlled study. J Rehabil Med. 2012;44:601–4.
Karadas O, Tok F, Ulas¸ UH, Odabasi Z. The effectiveness of triamcinolone acetonide vs. procaine hydrochloride injection in the management of carpal tunnel syndrome: a double-blind randomized clinical trial. Am J Phys Med Rehabil. 2011;90:287–92.
Eker HE, Cok OY, Aribogan A, Arslan G. Management of neuropathic pain with methylprednisolone at the site of nerve injury. Pain Med. 2012;13:443–51.
Thomson CE, Beggs I, Martin DJ, et al. Methylprednisolone injections for the treatment of Morton neuroma: a patient-blinded randomized trial. J Bone Joint Surg Am. 2013;95:790–8.
Ashkenazi A, Young WB. The effects of greater occipital nerve block and trigger point injection on brush allodynia and pain in migraine. Headache. 2005;45:350–4.
Armstrong T, Devor W, Borschel L, Contreras R. Intracarpal steroid injection is safe and effective for short-term management of carpal tunnel syndrome. Muscle Nerve. 2004;29:82–8.
Afridi SK, Shields KG, Bhola R, Goadsby PJ. Greater occipital nerve injection in primary headache syndromes – Prolonged effects from a single injection. Pain. 2006;122:126–9.
Ambrosini A, Vandenheede M, Rossi P, et al. Suboccipital injection with a mixture of rapid- and long-acting steroids in cluster headache: A double-blind placebo-controlled study. Pain. 2005;118:92–6.
Blair B, Rokito AS, Cuomo F, et al. Efficacy of injections of corticosteroids for subacromial impingement syndrome. J Bone Joint Surg. 1996;78:1685–9.
Plafki C, Steffen R, Willburger RE, Wittenberg RH. Local anaesthetic injection with and without corticosteroids for subacromial impingement syndrome. Int Orthop. 2000;24(1):40–2.
Vecchio PC, Hazleman BL, King RH. A double-blind trial comparing subacromial methylprednisolone and lignocaine in acute rotator cuff tendinitis. Br J Rheumatol. 1993;32(8):743–5.
Akgun K, Birtane M, Akarirmak U. Is local subacromial corticosteroid injection beneficial in subacromial impingement syndrome? Clin Rheumatol. 2004;23:496–500.
Alvarez CM, Litchfield R, Jackowski D, Griffin S, Kirkley A. A prospective, double-blind, randomized clinical trial comparing subacromial injection of betamethasone and xylocaine to xylocaine alone in chronic rotator cuff tendinosis. Am J Sports Med. 2005;33:255–62.
Petri M, Dobrow R, Neiman R, Whiting-O'Keefe Q, Seaman WE. Randomized, double-blind, placebocontrolled study of the treatment of the painful shoulder. Arthritis Rheum. 1987;30:1040–5.
Withrington RH, Girgis FL, Seifert MH. A placebo-controlled trial of steroid injections in the treatment of supraspinatus tendonitis. Scand J Rheumatol. 1985;14:76–8.
Lambert RGW, Hutchings EJ, Grace MGA, Jhangri GS, Conner-Spady B, Maksymowych WP. Steroid injection for osteoarthritis of the hip. A randomized, double-blind, placebo-controlled trial. Arthritis Rheum. 2007;56(7):2278–87.
Flannagan J, Thomas TL, Casale FF, Desai KB. Intraarticular injection for pain relief in patients awaiting hip replacement. Ann R Coll Surg Engl. 1988;70:156–7.
Dogramaci Y, Kalaci A, Savas N, Duman IG, Yanat AN. Treatment of lateral epicondilitis using three different local injection modalities: a randomized prospective clinical trial. Arch Orthop Trauma Surg. 2009;129:1409–14.
Lindenhovius A, Henket M, Gilligan BP, Lozano-Calderon S, Jupiter JB, Ring D. Injection of dexamethasone versus placebo for lateral elbow pain: a prospective, double-blind, randomized clinical trial. J Hand Surg Am. 2008;33:909–19.
Newcomer KL, Laskowski ER, Idank DM, McLean TJ, Egan KS. Corticosteroid injection in early treatment of lateral epicondylitis. Clin J Sport Med. 2001;11:214–22.
Price R, Sinclair H, Heinrich I, Gibson T. Local injection treatment of tennis elbow—hydrocortisone, triamcinolone and lignocaine compared. STUDY 1. Br J Rheumatol. 1991;30:39–44.
Price R, Sinclair H, Heinrich I, Gibson T. Local injection treatment of tennis elbow—hydrocortisone, triamcinolone and lignocaine compared. STUDY 2. Br J Rheumatol. 1991;30:39–44.
Altay T, Gunal I, Ozturk H. Local injection treatment for lateral epicondylitis. Clin Orthop Relat Res. 2002;398:127–30.
Stahl S, Kaufman T. The efficacy of an injection of steroids for medial epicondylitis. A prospective study of sixty elbows. J Bone Joint Surg Am. 1997;79:1648–52.
Adebajo AO, Nash P, Hazleman BL. A prospective double blind dummy placebo controlled study comparing triamcinolone hexacetonide injection with oral diclofenac 50 mg TDS in patients with rotator cuff tendinitis. J Rheumatol. 1990;17:1207–10.
Ekeberg OM, Bautz-Holter E, Tveita EK, Juel NG, Kvalheim S, Brox JI. Subacromial ultrasound guided or systemic steroid injection for rotator cuff disease: randomised double blind study. BMJ. 2009;338:a3112.
McInerney J, Dias J, Durham S, Evans A. Randomised controlled trial of single, subacromial injection of methylprednisolone in patients with persistent, post-traumatic impingment of the shoulder. Emerg Med J. 2003;20:218–21.
Manchikanti L, Singh V, Falco FJ, Cash KA, Pampati V, Fellows B. The role of thoracic medial branch blocks in managing chronic mid and upper back pain: a randomized, double-blind, active-control trial with a 2-year followup. Anesthesiol Res Pract. 2012;2012:585806. doi:10.1155/2012/585806. Epub 2012 Jul 19.
Manchikanti L, Pampati V, Bakhit C, Rivera J, Beyer C, Damron K, et al. Effectiveness of lumbar facet joint nerve blocks in chronic low back pain: A randomized clinical trial. Pain Physician. 2001;4:101–17.
Acknowledgements
We acknowledge the help and suggestions provided by Samantha Craigie, Research Coordinator, Michael G. DeGroote National Pain Centre, in designing the screening and data abstraction forms for DistillerSR.
We also acknowledge the suggestions provided by Sun Makosso-Kallyth, Biostatistician, Michael G. DeGroote Institute for Pain Research and Care, McMaster University, Hamilton, for the statistical analyses of the review.
Funding
No funds were received for the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
None of the authors have any financial or non-financial competing interests in the manuscript.
Authors’ contributions
HS conceived the study design, will supervise and be involved in the conduct of the review. LT, JWB, and JP provided inputs to improve the study design and outcome analyses. RC designed and carried out the database specific literature search. HS, HC, AK, PH, IK, and ES will screen potentially eligible studies for the review and abstract data from eligible trials. HS participated in the writing of the manuscript with inputs from JWB, LT, and JP. All authors have reviewed the final draft of the manuscript and approved the final version.
Additional file
Additional file 1:
Search strategy.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Shanthanna, H., Busse, J.W., Thabane, L. et al. Local anesthetic injections with or without steroid for chronic non-cancer pain: a protocol for a systematic review and meta-analysis of randomized controlled trials. Syst Rev 5, 18 (2016). https://doi.org/10.1186/s13643-016-0190-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13643-016-0190-z