Abstract
Background
The primary aim of this study was to evaluate the effect of acute administration of L-carnitine 100 mg·kg−1 iv on susceptibility to bupivacaine-induced cardiotoxicity in rats.
Methods
In the first of two experiments, L-carnitine 100 mg·kg−1 iv (n = 10) or saline iv (n = 10) was administered to anesthetized and mechanically ventilated Sprague-Dawley rats following which an infusion of bupivacaine 2.0 mg·kg−1·min−1 iv was given until asystole occurred. The primary outcome was the probability of survival. Secondary outcomes included times to asystole, first dysrhythmia, and to 50% reductions in heart rate (HR) and mean arterial pressure (MAP). To determine whether the same dose of L-carnitine is effective in treating established bupivacaine cardiotoxicity, we also conducted a second experiment in which bupivacaine 20 mg·kg−1 iv was infused over 20 sec. Animals (n = 10 per group) received one of four iv treatments: 30% lipid emulsion 4.0 mL·kg−1, L-carnitine 100 mg·kg−1, 30% lipid emulsion plus L-carnitine, or saline. The primary outcome was the return of spontaneous circulation (ROSC) during resuscitation.
Results
In the first study, L-carnitine 100 mg·kg−1 increased the probability of survival during bupivacaine infusion (hazard ratio, 12.0; 95% confidence interval, 3.5 to 41.5; P < 0.001). In L-carnitine-treated animals, the times to asystole, first dysrhythmia, and to 50% reductions in HR and MAP increased by 33% (P < 0.001), 65% (P < 0.001), 71% (P < 0.001), and 63% (P < 0.001), respectively. In the second study, no animal in the control or L-carnitine alone groups achieved ROSC when compared with the lipid emulsion groups (P < 0.01).
Conclusion
These findings suggest that acute administration of L-carnitine 100 mg·kg−1 decreases susceptibility to bupivacaine cardiotoxicity, but is ineffective during resuscitation from bupivacaine-induced cardiac arrest.
Résumé
Contexte
L’objectif principal de cette étude était d’évaluer l’effet d’une administration aiguë de 100 mg·kg−1 iv de L-carnitine sur la susceptibilité à une cardiotoxicité induite par la bupivacaïne chez le rat.
Méthode
Dans les deux premières expériences, on a administré 100 mg·kg−1 de L-carnitine (n = 10) ou de solution saline (n = 10) à des rats Sprague-Dawley anesthésiés et ventilés mécaniquement, puis on leur a administré une perfusion de 2,0 mg·kg−1·min−1 iv de bupivacaïne jusqu’à la survenue d’une asystolie. Le critère d’évaluation principal était la probabilité de survie. Les critères d’évaluation secondaires comportaient les temps jusqu’à l’asystolie, la première dysrythmie, et jusqu’à des réductions de 50 % de la fréquence cardiaque (FC) et de la tension artérielle moyenne (TAM). Afin de déterminer si la même dose de L-carnitine est efficace pour traiter une cardiotoxicité à la bupivacaïne déjà établie, nous avons également réalisé une deuxième expérience, dans laquelle nous avons perfusé 20 mg·kg−1 iv de bupivacaïne sur 20 sec. Les animaux (n = 10 par groupe) ont reçu l’un des quatre traitements iv suivants: 4,0 mL·kg−1 d’émulsion lipidique à 30 %, 100 mg·kg−1 de L-carnitine, émulsion lipidique à 30 % plus L-carnitine, ou solution saline. Le critère d’évaluation principal était le retour à une circulation spontanée (RCS) pendant la réanimation.
Résultats
Dans la première étude, une dose de 100 mg·kg−1 de L-carnitine a augmenté la probabilité de survie pendant une perfusion de bupivacaïne (rapport de risque, 12,0; intervalle de confiance 95 %, 3,5 à 41,5; P < 0,001). Chez les animaux traités à la L-carnitine, les temps jusqu’à l’asystolie, la première dysrythmie et à des réductions de 50 % de la FC et de la TAM ont augmenté de 33 % (P < 0,001), 65 % (P < 0,001), 71 % (P < 0,001) et 63 % (P < 0,001), respectivement. Dans la deuxième étude, aucun animal du groupe témoin ou du groupe L-carnitine seule n’est parvenu à un RCS comparativement aux groupes ayant reçu une émulsion lipidique (P < 0,01).
Conclusion
Ces résultats suggèrent que l’administration aiguë de 100 mg·kg−1 de L-carnitine réduit la susceptibilité à une cardiotoxicité à la bupivacaïne, mais que ce traitement est inefficace pendant la réanimation suite à un arrêt cardiaque induit par la bupivacaïne.
Similar content being viewed by others
Local anesthetic systemic toxicity (LAST) is a rare complication of regional anesthesia, occurring with an incidence of up to nine per 10,000 regional anesthetics in the adult patient population.1,2,3 Although lipid emulsion has gained widespread acceptance in the management of LAST,4 cardiovascular collapse remains the most difficult manifestation of LAST to treat.5,6 Inhibition of myocardial cation channels is considered a predominant mechanism by which local anesthetics cause cardiotoxicity in overdose.7 Nevertheless, other potential mechanisms include impairment of cellular energy metabolism via inhibition of oxidative phosphorylation.8,9,10,11,12
Bupivacaine is a potent inhibitor of lipid-based respiration in myocardial mitochondria via the carnitine system.12 Carnitine is a naturally occurring amino acid derivative that is essential in the transfer of long-chain fatty acids into the mitochondrial matrix for beta-oxidation.13,14 We have shown in a rodent model of LAST that a deficiency of L-carnitine increases susceptibility to bupivacaine-induced cardiotoxicity, an effect that was completely reversed by acute repletion with L-carnitine 100 mg·kg−1.15 Our previous findings indicated a significant reduction in time to asystole during intravenous infusion of bupivacaine in carnitine-deficient animals when compared with control and carnitine-replete animals. There was also a trend toward increased duration of survival in the L-carnitine-replete group compared with controls. Given these findings, we sought to determine if L-carnitine has a role in preventing bupivacaine-induced cardiotoxicity. We hypothesized that acute administration of L-carnitine 100 mg·kg−1 increases the probability of survival in rats during intravenous infusion of bupivacaine.
Methods
The Animal Care Committee of the Hospital for Sick Children, Toronto, Canada gave their approval (November, 2011) for all experiments, and we adhered to the Canadian Council on Animal Care guidelines for the care and use of animals. The animals used in our study were adult (aged nine to ten weeks) pathogen-free, drug and test-naïve male Sprague-Dawley rats (Charles River Breeding Laboratories, St. Constance, QC, Canada) weighing 300-400 g. The animals were housed in rectangular polycarbonate cages (two animals per cage) in a temperature-controlled 12-hr light/dark cycle. They were provided with unlimited access to water and were fed a standard non-purified diet (Prolab® RMH 1000 LabDiet®, PMI Nutrition International, Brentwood, MO, USA). After arrival at the animal lab facility, the animals were acclimatized for seven days before any experiments took place, and an animal laboratory technician assessed the animals daily. Experiments were carried out from 0800-1400 hr in the animal laboratory at the Hospital for Sick Children.
Experimental protocols
To determine the effect of acute intravenous L-carnitine administration on the threshold for bupivacaine-induced cardiotoxicity, we anesthetized and surgically prepared 20 rats as previously described.15 Anesthesia was induced with 2% isoflurane in oxygen, and the trachea was intubated via tracheostomy. A rodent ventilator (Harvard Apparatus, Saint-Laurent, QC, Canada) delivered a tidal volume of 10 mL·kg−1 and a respiratory rate of 65 breaths·min−1. Ventilation of the lungs was adjusted to maintain normocarbia (PaCO2 35-45 mmHg) according to arterial blood gas analysis (ABL700 Series blood gas analyzer, Radiometer, Copenhagen, Denmark). The tail vein and carotid artery were cannulated using a 24G Angiocath™ catheter (Becton Dickinson, Franklin Lakes, NJ, USA), and arterial blood (0.5 mL) was sampled for blood gas analysis and L-carnitine concentration. Electrocardiography, arterial blood pressure, and rectal temperature were monitored continuously (Biopac Data Acquisition System, Harvard Apparatus, Saint-Laurent, QC, Canada), and normothermia (36.5-37.5°C) was maintained using underbody warming.
Experiment 1
In the first experiment, the animals were allocated to one of two groups and received L-carnitine 100 mg·kg−1 (n = 10) or an equal volume of normal saline (n = 10) by intravenous bolus injection. L-carnitine was reconstituted with sterile water to a concentration of 250 mg·mL−1. The volumes administered ranged from 0.12-0.16 mL. Bupivacaine 0.5% (Astra Zeneca, Mississauga, ON, Canada) was then infused intravenously at a rate of 2 mg·kg−1·min−1 using an Alaris™ Syringe Module calibrated infusion pump (Cardinal Health, Vaughan, ON, Canada) until asystole, which was defined as the absence of electrocardiograph activity for ten seconds after the last systole. At this point, arterial blood was sampled to determine plasma bupivacaine and serum L-carnitine concentration. The primary outcome measure was the probability of survival, with asystole being the event of interest. Secondary outcomes included the time to asystole, a 20% increase in PR and QRS intervals, the first dysrhythmia, and a 50% reduction in heart rate (HR) and mean arterial pressure (MAP). We also measured plasma carnitine and bupivacaine concentrations and blood chemistry at the end of resuscitation. The first dysrhythmia was defined as the first abnormal electrocardiograph complex that was accompanied by an abnormal systole on the arterial blood pressure trace.
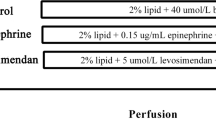
Experiment 2
Based on the results of the experiments described above, we conducted a second experiment to determine whether L-carnitine 100 mg·kg−1 improves survival during resuscitation from bupivacaine-induced cardiac arrest. Given that lipid emulsion is the only known antidote for bupivacaine-induced cardiotoxicity,6 we studied the efficacy of L-carnitine 100 mg·kg−1 alone and in combination with lipid emulsion. In this experiment, 40 animals were anesthetized and surgically prepared as described above. Using a computer-generated table of random numbers, the animals were randomized to one of four iv treatment groups (n = 10 per group): 1) 30% lipid emulsion 4 mL·kg−1 (Fresenius-Kabi, Uppsala, Sweden), 2) L-carnitine 100 mg·kg−1 (Sigma-Aldrich, St. Louis, MO, USA) diluted in normal saline, 3) 30% lipid emulsion 4 mL·kg−1 plus L-carnitine 100 mg·kg−1, and 4) normal saline (control group). Bupivacaine 0.5% was infused as a 20 mg·kg−1 iv injection over 20 sec - i.e., a dose of bupivacaine that reliably produces asystole in rats from which spontaneous hemodynamic recovery does not occur.16
At time zero (i.e., the end of the infusion), isoflurane was discontinued and chest compressions were commenced to achieve a rate pressure product (RPP; RPP = HR x systolic blood pressure) of at least 25% of baseline. A single investigator performed chest compressions at a rate of at least 150 compressions∙min−1 (i.e., 50% of baseline HR). Continuous arterial waveform monitoring determined the depth of compression to achieve a systolic blood pressure of at least 50% of baseline. The RPP in humans has been shown to correlate linearly with myocardial work and oxygen consumption.17,18,19 The RPP has been used to monitor adequacy of resuscitation and recovery of circulation in experimental models studying bupivacaine toxicity and as an indicator of cardiac work or oxygen consumption.16,20,21,22
Mechanical ventilation continued with 100% oxygen. One minute after time zero, the animals received an equal volume of one of the four treatments. Each therapy was administered by intravenous bolus and repeated at two minutes and four minutes after time zero. The primary outcome was the probability of survival, with the event of interest being return of spontaneous circulation (ROSC), defined as recovery of RPP to within 50% of baseline for at least one minute.16,20,21,22 Chest compressions were interrupted for ten seconds every minute to assess native electrocardiogram and RPP. The chest compressions were then continued for a maximum of ten minutes from the onset of resuscitation. Recorded data included times to achieve ROSC and RPP, plasma L-carnitine and bupivacaine concentrations, and blood chemistry at the end of resuscitation. Blood sampling for bupivacaine and carnitine concentrations and blood gas analysis occurred at the end of the experiments. Isoflurane 1% was re-introduced when ROSC was achieved. Animals that achieved ROSC were later euthanized using 0.5% bupivacaine 20 mg·kg−1 iv. The electrocardiogram was monitored to confirm asystole. Pentobarbital 240 mg·kg−1 iv was available if bupivacaine was unsuccessful in achieving asystole.
Measurement of bupivacaine and L-carnitine concentrations
Bupivacaine concentration was measured using the 4000 QTRAP® tandem mass spectrometer (Applied Biosystems, Foster City, CA, USA) in accordance with a technique previously described.15,23 Separation of bupivacaine to the mass spectrometer was accomplished by high-performance liquid chromatography and electrospray ionization. The mass spectrometer consists of a triple quadrapole system and an ion trap system. Collision-induced dissociation produces a product ion from a precursor ion. The system monitors for a specific ion pair based on mass-to-charge ratio, in this case, 289.3:140.2 for bupivacaine. The detector monitors, amplifies, and transmits the ion current signal to the data system where it is recorded in the form of a mass spectrum. Bupivacaine quantification is based on analyzing a six-point calibration curve (0-150 mg·L−1). The mass-to-charge ratio for prilocaine (221.2:86.1) is included as an internal standard with each calibration, quality control, or animal sample. The coefficient of variation was ± 4% at the detection limit of 0.05 mg·L−1, with between-batch variability of 4%.
The L-carnitine concentration was determined by spectrophotometric enzymatic assay using a Roche Cobas Mira analyzer (Roche Diagnostics, Nutley, NJ, USA). The coefficient of variation was 4-12%. The method is based on a process by which the enzyme carnitine acetyltransferase catalyzes a reaction that acts on L-carnitine. The resulting free coenzyme A is combined with 5,5′-dithiobis-2-nitrobenzoic acid to form a phenolate ion that is spectrometrically measured at 405 nm.24
Statistical analysis
Data are presented as mean (standard deviation [SD]) or median [interquartile range (IQR)]. For the first experiment, sample size estimation was based on previous work demonstrating a mean (SD) time to asystole of 1,082 (210) sec in controls.15 To show a 25% difference in time to asystole, we estimated that ten animals per group were required for a two-tailed alpha equal to 0.05 and 80% power. For the second experiment, preliminary work demonstrated that no control animals (treated with saline) had ROSC. To show a 60% difference in response to therapy, we estimated that 10 animals per group were required for alpha 0.05 (two-tailed) and 80% power.
Survival between treatment arms was compared using Kaplan-Meier analysis and the log-rank test with Bonferroni adjustment where appropriate. The hazard ratio and its 95% confidence interval (CI) were computed using the Mantel-Haenszel method. Unpaired Student’s t test, Mann-Whitney rank-sum test, one-way analysis of variance, Kruskal-Wallis, and/or the Chi square test were used for statistical comparisons as appropriate. Post-hoc Sidak or Bonferroni’s multiple comparison tests were used for pair-wise comparisons. All statistical tests were two-tailed, and P < 0.05 was considered statistically significant unless dictated by Bonferroni correction. Statistical analyses were performed using Stata® version 10.0 (Statacorp, College Station, TX, USA) or GraphPad Prism version 5.0 (GraphPad Software, San Diego, CA, USA).
Results
Experiment 1
Body weight, arterial blood gas analysis, and plasma electrolyte and L-carnitine concentrations did not differ significantly between groups (Table 1). In addition, baseline hemodynamic parameters were no different between control and experimental animals (Table 1).
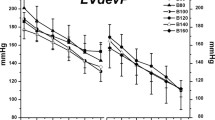
Log-rank analysis of the Kaplan Meier curves revealed increased survival in the L-carnitine group compared with the control group (hazard ratio, 12.0; 95% CI, 3.5 to 41.5; P < 0.001) (Fig. 1). Median [IQR] time to asystole was increased by 33% in the L-carnitine-treated group vs control (1,977 [1,813-2,420] sec vs 1,486 [1,290-1,720] sec, respectively; P < 0.001) (Fig. 2). Times to 20% prolongation of PR and QRS intervals were not significantly different between groups (Fig. 2). Nevertheless, in the L-carnitine vs control group (Mann-Whitney rank-sum test), there was a 65% increase in the time to first dysrhythmia (1,414 [1,259-1,820] sec vs 855 [658-991] sec, respectively; P < 0.001), a 71% increase in time to 50% reduction in HR (1,622 [1,292-1,838] sec vs 947 [745-1,048] sec, respectively; P < 0.001), and a 63% increase in time to 50% reduction in MAP (1,822 [1,528-2,184] sec vs 1,115 [823-1,269] sec, respectively; P < 0.001) (Fig. 2).
Experiment 1: Times to defined electrocardiographic and hemodynamic end points during bupivacaine infusion in control (dark bars; n = 10) and L-carnitine pre-treated rats (light bars; n = 10). Data are median, interquartile range, range. *P < 0.001 compared with control group. Increase PR 20% = 20% increase in PR interval. Increase QRS 20% = 20% increase in QRS interval. Heart rate (HR) 50% = 50% decrease in heart rate. Mean arterial pressure (MAP) 50% = 50% decrease in mean arterial pressure
In keeping with longer times to asystole, the total amount of bupivacaine infused and the resulting bupivacaine concentrations were significantly greater in the L-carnitine pretreated group (Table 2). Serum L-carnitine levels were also predictably increased in the L-carnitine group (Table 2). Arterial blood gas analysis revealed significant differences in pH, PaCO2, PaO2, lactate, K+, base excess, HCO3 −, and glucose, which were clinically favourable in the L-carnitine-treated group (Table 2).
Experiment 2
In experiment 2, baseline values for body weight, arterial blood gas analysis, and electrolyte and carnitine concentrations did not differ significantly between groups (Table 3). In addition, baseline hemodynamic parameters were no different between control and experimental animals (Table 3). Asystole occurred in all animals at the end of the bolus bupivacaine injection. None of the animals in the control and L-carnitine only groups were successfully resuscitated within the time frame of the experiment. In comparison, all animals in the lipid group and 60% of the lipid plus L-carnitine group achieved ROSC (i.e., RPP > 50% of baseline). In these animals, ROSC occurred after four minutes of resuscitation, by which time two treatment doses had been administered. Kaplan-Meier curves showing the percentage of animals achieving ROSC during the experiments are presented in Fig. 3. Analysis of the curves using the log-rank test with Bonferroni adjustment indicated a significant difference in the probability of survival between the lipid receiving groups compared with the non-lipid groups (P < 0.001). The difference in survival between the lipid only group and the lipid plus L-carnitine group was also significant (hazard ratio, 5.3; 95% CI, 1.7 to 16.8; P < 0.01).
Experiment 2: Kaplan-Meier curves showing percentage of animals achieving return of spontaneous circulation (ROSC) over time in each group. The groups receiving lipids were significantly more likely to achieve ROSC (P < 0.001). Neither the control nor the L-carnitine only groups achieved ROSC (superimposed)
Fig. 4 shows the variation of mean RRP in each group over time and illustrates lack of recovery in the control and L-carnitine groups at all time points. The lipid group is again shown to have a greater rate of recovery than the lipid plus L-carnitine group. Bupivacaine concentrations were not significantly different between groups. Predictably, serum carnitine levels were significantly increased in the two groups that received L-carnitine vs the two groups that did not (P < 0.0001). Arterial blood gas analysis revealed significant differences in HCO3 − and base excess, which were least favourable in the L-carnitine only group (Table 4). There were no modifications to the protocol in any of the experimental groups.
Discussion
In the current study, acute intravenous administration of L-carnitine 100 mg·kg−1 decreased susceptibility to bupivacaine-induced dysrhythmia, hypotension, and asystole in normal rats. These findings are consistent with those of our previous studies, which showed that L-carnitine deficiency increased susceptibility to bupivacaine cardiotoxicity, an effect completely reversed by acute L-carnitine repletion.15
L-carnitine is essential for the transfer of long-chain fatty acids from the cytoplasm into the mitochondrial matrix where beta-oxidation occurs and supplies the cardiac mitochondrion with over 70% of its energy requirements under normal physiological conditions.13,14 Bupivacaine-induced cardiotoxicity is explained in part by interference with lipid oxidation in myocardial mitochondria.8,9,10,11,12 The present findings also support studies demonstrating a role of bupivacaine in inhibiting lipid-based respiration in myocardial mitochondria via inhibition of carnitine-dependent processes.12
The reduction in susceptibility to bupivacaine cardiotoxicity led us to hypothesize that administration of L-carnitine 100 mg·kg−1 iv may also be potentially useful in the treatment of established bupivacaine toxicity. Nevertheless, the findings of our second series of experiments did not support this hypothesis, demonstrating not only that L-carnitine 100 mg·kg−1 did not improve survival but also that, when co-administered with lipid emulsion, L-carnitine may reduce the effectiveness of lipid emulsion alone.
The use of lipid emulsion to treat local anesthetic toxicity originated from an unexpected result in a study in rats.25 Subsequent work in rodent and canine models supported this serendipitous finding.26,27 Since its adoption into clinical practice, several case reports have described the effectiveness of lipid emulsion in treating refractory cardiac arrest secondary to local anesthetic toxicity.28,29,30,31,32 The exact mechanism of action is uncertain, but it is postulated to be due in part to a direct inotropic or cardiotonic effect on the heart, membrane stabilization, and/or creation of a lipid phase in blood (the “lipid sink” theory) that is able to reduce the effective plasma concentration of bupivacaine by dynamic scavenging and sequestration of the lipophilic molecules from tissue receptors.6,33,34,35,36
Under normal aerobic conditions, the myocardium preferentially depends on lipids for the majority of its energy requirements.37 Nevertheless, the mammalian heart utilizes a variety of energy substrates under different physiological and pathological conditions.38 For example, oxidation of glucose and lactate increases significantly during moderate intensity exercise.39 Likewise, in the ischemic heart, mitochondrial acetyl Co-A production is more reliant on glycolysis and lactate or pyruvate oxidation, although fatty acid oxidation recovers quickly during reperfusion.40 Studies examining substrate utilization in non-ischemic cardiac arrest with warm cardioplegia demonstrated that energy was derived almost exclusively from fatty acid oxidation, with negligible contribution from lactate and glucose metabolism, suggesting that fatty acids remain the key energy source for the non-ischemic heart.41
Bupivacaine has been shown to inhibit the availability of lipid substrate in cardiac mitochondria.12 Accordingly, the administration of lipid emulsion may overcome bupivacaine-induced blockade of fatty acid transport by mass action. Lipid emulsion is predominantly comprised of long-chain fatty acids42 that require transport into mitochondria via the carnitine system. We postulated that the presence of additional L-carnitine would aid in this process of energy substrate transfer and therefore improve myocardial recovery. Possible mechanisms for the lack of efficacy of L-carnitine when used in resuscitation include the inability of the already failing myocardium to process additional metabolic substrate or to benefit from increased availability of long-chain fatty acids. Additional substrate in such a scenario may contribute to myocardial failure by diverting bioenergetic processes toward fatty acid oxidation and away from anerobic pathways such as anerobic glycolysis, which may be important for survival in the setting of established local anesthetic cardiac arrest.40 Nevertheless, we investigated only a single fixed dose of 100 mg·kg−1 L-carnitine based on the results of the previous experiments, and dose-response data are lacking.
L-carnitine-dependent production of acetyl Co-A in the mitochondrial matrix can enhance glucose oxidation.14 While experimental evidence suggests that L-carnitine is protective in models of ischemia, it is thought that this effect of L-carnitine cannot be explained by stimulation of fatty acid oxidation exclusively but is dependent on glucose oxidation.43 Nevertheless, myocardial substrate metabolism during ischemia is dependent on the severity of ischemia,14 and in our experimental setting of LAST, significant reduction of substrate flux into the mitochondria may result in lack of benefit from L-carnitine. Indeed, we found that the L-carnitine-treated groups were most acidotic and had a higher lactate level than the other groups, including the control group which similarly failed to achieve ROSC.
Our study has important limitations. In particular, we investigated a single dose of L-carnitine previously shown to decrease susceptibility to bupivacaine cardiotoxicity in the carnitine-deficient animal.15 This dose was used in other experimental studies 44,45,46 and is consistent with the recommended dosage used clinically in the treatment of acute carnitine deficiency resulting from valproate toxicity.47,48 Dose-response experiments would strengthen an apparent causal relationship between L-carnitine administration and decreased susceptibility to bupivacaine-induced cardiotoxicity. In addition, we administered the lipid emulsion by bolus during resuscitation, not as an infusion as is recommended for clinical practice.4 That said, in the time frame of our experiment, the bolus doses given exceeded the dose that would be administered via infusion. This was considered consistent with treatment that would be administered in the early stages of a clinical scenario of resuscitation from local anesthetic cardiotoxicity.
Preemptive administration of L-carnitine to the general population in the preoperative setting in order to avoid the rare complication of LAST is unlikely to be adopted clinically. Nonetheless, we have provided evidence to support a role for L-carnitine in decreasing susceptibility to bupivacaine-induced cardiotoxicity, and these data add to the existing body of work elucidating mechanisms of LAST. Of clinical relevance, these findings support our previous work showing that L-carnitine plasma concentration influences susceptibility to LAST.15 Clinicians should be aware that experimental15 as well as clinical49 evidence suggests that L-carnitine deficiency predisposes to local anesthetic toxicity and that acute L-carnitine repletion reverses this effect.15
In conclusion, our data suggest that L-carnitine administration decreases susceptibility to bupivacaine cardiotoxicity, which is in keeping with previous studies demonstrating a role for the carnitine system in local anesthetic cardiotoxicity.
References
Mulroy MF. Systemic toxicity and cardiotoxicity from local anesthetics: incidence and preventive measures. Reg Anesth Pain Med 2002; 27: 556-61.
Barrington MJ, Kluger R. Ultrasound guidance reduces the risk of local anesthetic systemic toxicity following peripheral nerve blockade. Reg Anesth Pain Med 2013; 38: 289-97.
Sites BD, Taenzer AH, Herrick MD, et al. Incidence of local anesthetic systemic toxicity and postoperative neurologic symptoms associated with 12,668 ultrasound-guided nerve blocks: an analysis from a prospective clinical registry. Reg Anesth Pain Med 2012; 37: 478-82.
Neal JM, Bernards CM, Butterworth JF 4th, et al. ASRA practice advisory on local anesthetic systemic toxicity. Reg Anesth Pain Med 2010; 35: 152-61.
Corcoran W, Butterworth J, Weller RS, et al. Local anesthetic-induced cardiac toxicity: a survey of contemporary practice strategies among academic anesthesiology departments. Anesth Analg 2006; 103: 1322-6.
Bern S, Akpa BS, Kuo I, Weinberg G. Lipid resuscitation: a life-saving antidote for local anesthetic toxicity. Curr Pharm Biotechnol 2011; 12: 313-9.
Clarkson CW, Hondeghem LM. Mechanism for bupivacaine depression of cardiac conduction: fast block of sodium channels during the action potential with slow recovery from block during diastole. Anesthesiology 1985; 62: 396-405.
Stehr SN, Ziegeler JC, Pexa A, et al. The effects of lipid infusion on myocardial function and bioenergetics in l-bupivacaine toxicity in the isolated rat heart. Anesth Analg 2007; 104: 186-92.
Sztark F, Malgat M, Dabadie P, Mazat JP. Comparison of the effects of bupivacaine and ropivacaine on heart cell mitochondrial bioenergetics. Anesthesiology 1998; 88: 1340-9.
Irwin W, Fontaine E, Agnolucci L, et al. Bupivacaine myotoxicity is mediated by mitochondria. J Biol Chem 2002; 277: 12221-7.
Edelman LB, Ripper R, Kelly K, Di Gregorio G, Weinberg GL. Metabolic context affects hemodynamic response to bupivacaine in the isolated rat heart. Chem Biol Interact 2008; 172: 48-53.
Weinberg GL, Palmer JW, Vade Boncouer TR, Zuechner MB, Edelman G, Hoppel CL. Bupivacaine inhibits acylcarnitine exchange in cardiac mitochondria. Anesthesiology 2000; 92: 523-8.
Mayes PA. Oxidation of fatty acids: ketogenesis. In: Murray RK, Granner DK, Mayes PA, Rodwell VW, editors. Harper’s Biochemistry. 25th ed. NY: McGraw-Hill Publishing; 2000. p. 238-49.
Calvani M, Reda E, Arrigoni-Martelli E. Regulation by carnitine of myocardial fatty acid and carbohydrate metabolism under normal and pathological conditions. Basic Res Cardiol 2000; 95: 75-83.
Wong GK, Crawford MW. Carnitine deficiency increases susceptibility to bupivacaine-induced cardiotoxicity in rats. Anesthesiology 2011; 114: 1417-24.
Hiller DB, Di Gregio G, Ripper R, et al. Epinephrine impairs lipid resuscitation from bupivacaine overdose: a threshold effect. Anesthesiology 2009; 111: 498-505.
Gobel FL, Norstrom LA, Nelson RR, Jorgensen CR, Wang Y. The rate pressure product as an index of myocardial oxygen consumption during exercise in patients with angina pectoris. Circulation 1978; 57: 549-56.
Ansari M, Javadi H, Pourbehi M, et al. The association of rate pressure product (RPP) and myocardial perfusion imaging (MPI) findings: a preliminary study. Perfusion 2012; 27: 207-13.
Prema S, Sembulingam K, Saraswathi I, Sridevi G. Rate pressure product as a determinant of physical fitness in normal young adults. IOSR-JDMS 2015; 14: 8-12.
Di Gregorio G, Schwartz D, Ripper R, et al. Lipid emulsion is superior to vasopressin in a rodent model of resuscitation from toxin-induced cardiac arrest. Crit Care Med 2009; 37: 993-9.
Jin Z, Xia Y, Xia F, et al. Epinephrine administration in lipid-based resuscitation in a rat model of bupivacaine-induced cardiac arrest: optimal timing. Reg Anesth Pain Med 2015; 40: 223-31.
Weinberg GL, Di Gregorio G, Ripper R, et al. Resuscitation with lipid versus epinephrine in a rat model of bupivacaine overdose. Anesthesiology 2008; 108: 907-13.
St Louis P, Das I, Rybczynski J, Bissonnette B, Hartley EJ. Determination of bupivacaine in plasma by high-performance liquid chromatography. Levels after scalp infiltration in children. Clin Biochem 1991; 24: 463-7.
Galan A, Padros A, Arambarri M, Martin S. Automation of a spectrophotometric method for measuring L-carnitine in human blood serum. J Automat Chem 1998; 20: 23-6.
Weinberg GL, VadeBoncouer T, Ramaraju GA, Garcia-Amaro MF, Cwik MJ. Pretreatment or resuscitation with a lipid infusion shifts the dose-response to bupivacaine-induced asystole in rats. Anesthesiology 1998; 88: 1071-5.
Weinberg GL, Ripper R, Feinstein DL, Hoffman W. Lipid emulsion infusion rescues dogs from bupivacaine-induced cardiac toxicity. Reg Anesth Pain Med 2003; 28: 198-202.
Weinberg GL, Ripper R, Murphy P, et al. Lipid infusion accelerates removal of bupivacaine and recovery from bupivacaine toxicity in the isolated rat heart. Reg Anesth Pain Med 2006; 31: 296-303.
Ludot H, Tharin JY, Belouadah M, Mazoit JX, Malinovsky JM. Successful resuscitation after ropivacaine and lidocaine-induced ventricular arrhythmia following posterior lumbar plexus block in a child. Anesth Analg 2008; 106: 1572-4.
Rosenblatt MA, Abel M, Fischer GW, Itzkovich CJ, Eisenkraft JB. Successful use of a 20% lipid emulsion to resuscitate a patient after presumed bupivacaine-related cardiac arrest. Anesthesiology 2006; 105: 217-8.
Litz RJ, Popp M, Stehr SN, Koch T. Successful resuscitation of a patient with ropivacaine-induced asystole after axillary plexus block using lipid infusion. Anaesthesia 2006; 61: 800-1.
Litz RJ, Roessel T, Heller AR, Stehr SN. Reversal of central nervous system and cardiac toxicity after local anesthetic intoxication by lipid emulsion injection. Anesth Analg 2008; 106: 1575-7.
Warren JA, Thoma RB, Georgescu A, Shah SJ. Intravenous lipid infusion in the successful resuscitation of local anesthetic-induced cardiovascular collapse after supraclavicular brachial plexus block. Anesth Analg 2008; 106: 1578-80.
Stojiljkovic MP, Zhang D, Lopes HF, Lee CG, Goodfriend TL, Egan BM. Hemodynamic effects of lipids in humans. Am J Physiol Regul Integr Comp Physiol 2001; 280: 1674-9.
Fettiplace MR, Akpa BS, Ripper R, et al. Resuscitation with lipid emulsion: dose-dependent recovery from cardiac pharmacotoxicity requires a cardiotonic effect. Anesthesiology 2014; 120: 915-25.
Kuo I, Akpa BS. Validity of the lipid sink as a mechanism for the reversal of local anesthetic systemic toxicity: a physiologically based pharmacokinetic model study. Anesthesiology 2013; 118: 1350-61.
Fettiplace MR, Weinberg G. Past, present, and future of lipid resuscitation therapy. JPEN J Parenter Enteral Nutr 2015; 39(1 Suppl): 72S-83S.
Grynberg A, Demaison L. Fatty acid oxidation in the heart. J Cardiovasc Pharmacol 1996; 28(Suppl 1): S11-7.
Kolwicz SC Jr, Purohit S, Tian R. Cardiac metabolism and its interactions with contraction, growth, and survival of cardiomyocytes. Circ Res 2013; 113: 603-16.
Gertz EW, Wisneski JA, Stanley WC, Neese RA. Myocardial substrate utilization during exercise in humans: dual carbon-labeled carbohydrate isotope experiments. J Clin Invest 1988; 82: 2017-25.
Kantor PF, Dyck JR, Lopaschuk GD. Fatty acid oxidation in the reperfused ischemic heart. Am J Med Sci 1999; 318: 3-14.
Larsen TS, Irtun O, Steigen TK, Andreasen TV, Sørlie D. Myocardial substrate oxidation during warm continuous blood cardioplegia. Ann Thorac Surg 1996; 62: 762-8.
Intralipid ®. Package insert. Uppsala, Sweden: Fresenius Kabi; 2013. Available from URL: http://fresenius-kabi.ca/en/wp-content/uploads/sites/2/2013/07/Intralipid-Package-Insert.pdf (accessed October 2016).
Ferrari R, Merli E, Cicchitelli G, Mele D, Fucili A, Ceconi C. Therapeutic effects of L-carnitine and propionyl-L-carnitine on cardiovascular diseases: a review. Ann N Y Acad Sci 2004; 1033: 79-91.
Onem G, Aral E, Enli Y, et al. Neuroprotective effects of L-carnitine and vitamin E alone or in combination against ischemia-reperfusion injury in rats. J Surg Res 2006; 131: 124-30.
Marzo A, Cardace G, Corbelleta C, et al. Homeostatic equilibrium of L-carnitine family before and after i.v. administration of propionyl-L-carnitine in humans, dogs and rats. Eur J Drug Metab Pharmacokinet 1991; 3: 357-63.
Suzuki Y, Kamikawa T, Yamazaki N. Effect of L-carnitine on cardiac hemodynamics. Jpn Heart J 1981; 22: 219-25.
Russell S. Carnitine as an antidote for acute valproate toxicity in children. Curr Opin Pediatr 2007; 19: 206-10.
Lheureux PE, Penaloza A, Zahir S, Gris M. Science review: carnitine in the treatment of valproic acid-induced toxicity - what is the evidence? Crit Care 2005; 9: 431-40.
Wong GK, Joo DT, McDonnell C. Lipid resuscitation in a carnitine deficient child following intravascular migration of an epidural catheter. Anaesthesia 2010; 65: 192-5.
Acknowledgements
The authors are grateful to Warren Walsh (B.Sc., Resource Technologist, Therapeutic Drug Monitoring and Toxicology, Department of Pediatric Laboratory Medicine, The Hospital for Sick Children, Toronto, Ontario, Canada) and Marvin A. Estrada (Dip. Vet. Tech., Surgical Supervisor, Department of Laboratory Animal Services, Research Institute, The Hospital for Sick Children, Toronto, Ontario, Canada) for their advice and assistance.
Conflicts of interest
None declared.
Editorial responsibility
This submission was handled by Dr. Hilary P. Grocott, Editor-in-Chief, Canadian Journal of Anesthesia.
Author contributions
Gail K. Wong and Mark W. Crawford helped design the study. Gail K. Wong and Carolyne Pehora helped conduct the study. Gail K. Wong, Carolyne Pehora, and Mark W. Crawford helped analyze the data and write the manuscript. They have seen the original study data and reviewed the analysis of the data. Mark W. Crawford is the author responsible for archiving the study files.
Funding
This research was supported by a Merit Award from the Department of Anesthesia, University of Toronto, ON, Canada.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wong, G.K., Pehora, C. & Crawford, M.W. L-carnitine reduces susceptibility to bupivacaine-induced cardiotoxicity: an experimental study in rats. Can J Anesth/J Can Anesth 64, 270–279 (2017). https://doi.org/10.1007/s12630-016-0797-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-016-0797-5