Abstract
Purpose
The purpose of this narrative review is to address perioperative bleeding and transfusion as determinants of adverse outcomes after cardiac surgery.
Principal findings
The relationship between postoperative bleeding and adverse outcomes is non-linear, with an increase in the risk of mortality only in cases of severe perioperative bleeding. When perioperative bleeding is used as an outcome variable, it should be dichotomized according to the existing definitions. In retrospective observational studies, red blood cell transfusions have been associated with an increase in morbidity and mortality, which points to restriction of transfusion as a potential benefit. Nevertheless, randomized-controlled trials have not confirmed that restrictive transfusion policies are associated with better outcomes. Additionally, a transfusion policy that is too restrictive may actually increase postoperative mortality in cardiac surgery patients.
Conclusion
Perioperative bleeding itself is a complex syndrome that can be classified as an outcome measure. Red blood cell transfusion has limitations when considered as an outcome variable and can be biased by many confounders. Its relationship with clinical outcome remains uncertain. In addition to being potential outcome measures, transfusion rates and the number of allogeneic blood products transfused may also be considered as quality-of-care markers.
Résumé
Objectif
L’objectif de ce compte rendu narratif est de considérer l’impact des pertes sanguines et des transfusions périopératoires en tant que facteurs déterminants des complications survenant après une chirurgie cardiaque.
Constatations principales
La relation entre les saignements postopératoires et les complications n’est pas linéaire, le risque de mortalité n’augmentant que dans les cas où les saignements périopératoires sont graves. Lorsque le saignement périopératoire est utilisé comme variable d’évaluation, il devrait être dichotomisé selon les définitions existantes. Dans les études observationnelles rétrospectives, la transfusion d’érythrocytes a été associée à une augmentation de la morbidité et de la mortalité, ce qui indique qu’une restriction des transfusions pourrait être potentiellement bénéfique. Toutefois, aucune étude randomisée contrôlée n’a confirmé que des politiques de restriction des transfusions étaient associées à de meilleurs pronostics. Qui plus est, une politique transfusionnelle trop restrictive pourrait en fait augmenter la mortalité postopératoire chez les patients de chirurgie cardiaque.
Conclusion
Les saignements périopératoires sont, en soi, un syndrome complexe qui peut être utilisé comme critère d’évaluation. La transfusion d’érythrocytes comporte des limites lorsqu’elle est considérée comme variable d’évaluation et peut être biaisée par plusieurs facteurs confondants. Sa relation avec le devenir clinique demeure énigmatique. Outre le fait de constituer des critères d’évaluation potentiels, les taux de transfusion et le nombre de produits sanguins allogènes transfusés peuvent également être considérés comme des marqueurs de la qualité des soins.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Patients undergoing cardiac surgery are prone to both hemorrhagic and thrombotic complications in the early postoperative period. Due to a variety of reasons (which are not the focus of this present article), the hemostatic system is severely disturbed by cardiac operations, with or without the use of cardiopulmonary bypass (CPB).1 As a result, patients will experience variable degrees of perioperative bleeding. In the most severe cases, patients require the administration of hemostatic blood products, such as fresh frozen plasma (FFP) and platelet concentrates (PLT), to address the coagulopathy and red blood cells (RBC) to correct anemia. Additionally, a surgical revision is often required to control bleeding (or its sequelae—i.e., tamponade) in a variable percentage (2-7%) of patients.2-4
Both perioperative bleeding and transfusions have been considered determinants of adverse outcomes,5-8 and surgical reoperation to address bleeding is associated with an increased rate of perioperative mortality.2,4 Therefore, bleeding and/or transfusions have been considered as specific outcome measures in many different studies. In particular, a number of randomized-controlled trials (RCTs) exploring the efficacy of pro-hemostatic drugs have used transfusion-related measures or bleeding-related measures as primary or secondary endpoints.
The present review article addresses the respective roles of bleeding and transfusions as outcome determinants after cardiac surgery.
Perioperative bleeding
The importance of a standardized definition
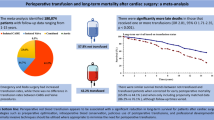
Perioperative bleeding is a natural continuous variable that can be expressed in terms of flow (i.e., volume of blood loss over a defined time period). The continuous nature of perioperative bleeding makes it a challenge to consider as an outcome measure without dichotomization into a binary variable based on specific thresholds. Indeed, every patient will experience a certain degree of postoperative bleeding, but even relatively large differences in rates of bleeding (e.g., 150 mL·12 hr−1 vs 300 mL·12 hr−1) are not necessarily accompanied by a clinically relevant difference in outcome, particularly if limited by a relatively short duration. The Figure shows the relationship between the degree of postoperative bleeding and postoperative mortality in a series of 16,400 adult patients undergoing cardiac operations at our institution during the last 14 years (data partially published).6 It is quite evident that there was an impact on mortality only in those patients who experienced severe (defined as > 850 mL·12 hr−1) postoperative bleeding.
Therefore, given the non-linear relationship between postoperative bleeding and clinically relevant adverse outcomes, it is important to define optimal threshold values to standardize the bleeding rate as a pertinent outcome variable.
A second problem when considering bleeding as an outcome variable is the limited information obtained from measuring chest tube output. This measurement can begin only once the chest is closed and the drains are connected to a standard reservoir. Therefore, it does not take into account the intraoperative blood loss, particularly the potentially important measure of intraoperative blood loss that occurs between heparin reversal (i.e., protamine administration) and chest closure.
Various studies have attempted to address this subtle though complex point. The proposed approaches to assess intraoperative bleeding include an evaluation of the amount of blood processed with the cell saver and the time to achieve a satisfactory surgical hemostasis (i.e., the time from the end of CPB to sternal closure). Additionally, some authors have proposed more sophisticated techniques based on the weight of the surgical sponges before and after being placed in the surgical field for a given time period.9,10 In these studies, bleeding (usually non-surgical) was considered to have occurred if the weight of the sponges increased > 60 g over a five-minute observation period.
This last approach, theoretically being the most reliable measure of intraoperative bleeding, is routinely used in only a minority of cardiac surgery institutions. Therefore, its role still seems limited to specific RCTs, and adopting it as a more routine measure is uncertain.
Finally, within the concept of grading bleeding severity, the effects of the therapeutic measures should also be included. An important bleeding event in the first postoperative hour (i.e., > 500 mL) may trigger a surgical revision without additional bleeding in the following hours. Although this condition is not characterized by a large loss of total blood volume, it certainly represents a case of severe bleeding given the deleterious consequences of any surgical revision. Similarly, the need to use procoagulant drugs (i.e., prothrombin complex concentrate, fibrinogen concentrate, recombinant activated factor VII) or large doses of blood products (RBC, FFP, PLT, cryoprecipitate) is a marker of a clinically relevant bleeding. The use of these procoagulant strategies per se is important as some of the drugs/blood component products used to control bleeding may also be determinants of thromboembolic events.11,12
In 2014, a consortium of clinicians, including cardiac surgeons, cardiac anesthesiologists, and pharmacoeconomists, attempted to address the problem of defining and grading perioperative bleeding in adult cardiac surgery.13 The universal definition for perioperative bleeding (UDPB) that they proposed is based on nine items: delayed sternal closure; chest drain blood loss; amount of RBCs transfused; use of any FFP, PLT, cryoprecipitates, prothrombin complex concentrates, recombinant activated factor VII; and presence of surgical revision/re-exploration. Based on these factors, the bleeding can be defined as insignificant, mild, moderate, severe, or massive. The potential advantage of using this UDPB is that bleeding, as an outcome measure, can now be dichotomized (i.e., severe/massive bleeding vs minor grades). Additionally, the adoption of the UDPB may standardize the concept of bleeding as an outcome measure, for example, in RCTs exploring the efficacy of pro-hemostatic drugs or techniques.
At present, the UDPB has been successfully used in two cohort studies.14,15 There are certainly limitations in the UDPB, including an incomplete assessment of intraoperative blood loss; the inability to account for the effects of local policies for administration of FFP, PLT, cryoprecipitate, prothrombin complex concentrates, recombinant activated factor VII; as well as different approaches for deciding the need for surgical re-exploration.
A final consideration concerning postoperative bleeding that challenges including it as an outcome is the relevance not only in the amount of bleeding but also in its location. For example, a relatively limited amount of bleeding that leads to a locally compressive thrombus may be a determinant of an adverse outcome (i.e., a bleeding mass compressing heart chambers). In addition, patients’ tolerance to the anemia resulting from the bleeding is variable and may partially depend on their preoperative (i.e., baseline) hemoglobin level.
Perioperative bleeding as an outcome measure in RCTs
Several recent cardiac surgery studies (reported in 2013-2015) of various pro-hemostatic treatments, techniques, and protocols have used perioperative bleeding as a specific endpoint. The amount of perioperative bleeding was defined in a heterogeneous way, either as a primary or (more frequently) secondary endpoint of the study. The following treatments have recently been evaluated for efficacy in reducing perioperative bleeding: use of transfusion algorithms based on point of care,15 fibrinogen concentrate,9,10,16,17 tranexamic acid/epsilon-aminocaproic acid,18-20 antithrombin-III,21 heparin monitoring systems,22 and shed blood processing.23,24 Notably, the objective for all these treatments was a direct reduction in postoperative bleeding; however, in the majority of the cases, the primary endpoint was avoidance of transfusion. Consequently, there were some conflicting results between the two outcome measurements—i.e., a reduction in postoperative bleeding and the rate of surgical revision did not translate into a significant reduction in transfusions.20 The reasons for this inconsistency are not clear but may be due to the trial design or to limited efficacy of the tested treatments.
Allogeneic blood product transfusions as outcome measures
Is RBC transfusion a suitable measurement of adverse outcome in cardiac surgery?
Many studies, including some of our own, provide background material and rationale for considering the need for transfusion as an “adverse event”. Indeed, “considerable evidence suggests that transfusion increases the risk of serious complications and death in critically ill patients, especially in patients who are undergoing cardiac surgery”.8 Nevertheless, the level of evidence for this concept is based on retrospective studies where the short- and even long-term outcome of patients receiving vs not receiving allogeneic transfusions is compared.7,8,25-27 Of course, the authors of these studies attempt to take into account that patients receiving allogeneic RBCs generally represent a patient population at higher risk than those not receiving transfusions and accordingly adjust for both preoperative (i.e., preoperative anemia, age, female sex, renal dysfunction, etc.) and intraoperative risk factors (i.e., urgent/emergent operations, redo surgery, complexity of surgery, and duration of CPB). To adjust for these risk factors, the authors use various statistical tools, often propensity-based matching. Nevertheless, even after adjustment for these potential confounders, transfusions generally remain independently associated with poor outcomes.27
Then again, recent studies have challenged this concept. For example, if transfusions are independent determinants of adverse outcomes, a restrictive transfusion policy should be associated with a lower rate of morbidity and mortality. To test this hypothesis and to substantiate the retrospective studies that generated this hypothesis, several RCTs have already been reported or are underway.
The Transfusion Requirements After Cardiac Surgery (TRACS) study compared a restrictive vs a liberal strategy in cardiac surgery patients (trigger for RBC transfusion, hematocrit [HCT] < 24% vs HCT < 30%, respectively).28 The study was a single-centre RCT conducted in an intensive care unit at a university hospital cardiac surgery referral centre in Brazil. The study included 502 consecutive adult patients who underwent cardiac surgery with CPB. The composite endpoint of mortality and major morbidity was comparable in the two groups, with a 30-day mortality of 5% (95% confidence interval [CI], 2 to 7) in the liberal strategy arm and 6% (95% CI, 3 to 9) in the restrictive strategy arm (P = 0.93). The results of this study can be interpreted from two different perspectives: On the one hand, it is safe to apply a restrictive transfusion strategy in cardiac surgery patients. On the other hand (and consistent with the retrospective studies), one would expect the liberal group to have higher morbidity/mortality rate, or at least a trend in that direction. Conversely, despite receiving transfusions at a considerably higher rate (78%, liberal vs 47%, restrictive; P < 0.001), patients in the liberal group did not show any increase in adverse outcomes. Nevertheless, the TRACS study highlighted that patients receiving large amounts of transfusions, independent of group assignment, actually had a higher mortality rate. Even more interesting results come from the recent RCT by Murphy et al.29 Their Transfusion Indication Threshold Reduction-2 (TITRe2) study was a multicentre RCT that included 2,007 adult patients undergoing non-emergency cardiac surgery in 17 centres in the United Kingdom. Here, the authors also compared a restrictive vs a liberal strategy in cardiac surgery patients (trigger for transfusion of RBCs: hemoglobin < 7.5 g·dL−1 vs hemoglobin < 9 g·dL−1, respectively). Again, the composite outcome of major morbidity and early mortality was not different between groups. In contrast, late (90-day) mortality was significantly higher in the restrictive group than in the liberal group (4.2% vs 2.6%, respectively; hazard ratio, 1.64; 95% CI, 1.00 to 2.67).
Accordingly, that study not only negated the hypothesis that an increased transfusion rate results in bad outcomes, but it also introduced the possibility that too restrictive a transfusion protocol may actually increase mortality in cardiac surgery patients.
As with every study, the TITRe2 had its own limitations relating to protocol deviations in both groups, including the absence of accounting for data (e.g., elective/urgent surgery and central venous oxygen saturation values) before transfusions and a lack of adjustment for multiple secondary outcomes. Additionally, the study did not consider the possible effects of different levels of postoperative anemia in the two groups as a confounding factor as well as the possible bias introduced by the presence of transfusions before randomization. It is difficult to interpret that a more severe postoperative anemia in the restrictive group would be a determinant of mortality since this would have more impact on early rather than on late mortality.
Taken together, the concept that transfusions are independent determinants of adverse outcomes (with the exception of extreme volumes of blood and blood products) after cardiac surgery has now been seriously questioned.
The problems when considering transfusions as a determinant of adverse outcomes
The above-described conflicting results between the retrospective studies and the RCTs may be explained in part by the respective statistical methodology used. In RCTs, the homogeneity and comparability of the groups can be better assured by the randomization process. In retrospective studies, similar comparability relies on adequate adjustments in patient population profiles, frequently by propensity matching. Nevertheless, propensity matching is arguably inadequate to adjust for all the confounding effects of pre- and intraoperative variables. For example, only the variables included in the databases queried can be used to create propensity matching. In general, even the most complete databases do not include a number of potentially important variables. The most important variable among these is the clinical judgement of the attending physician (i.e., anesthesiologist, intensivist, cardiac surgeon) making the decision regarding the transfusion. For example, although RBC transfusions are intended to correct what the physician considers as an inadequate oxygen delivery, some of the variables pertaining to this decision may be missing in the database: How does the patient look from a clinical standpoint? Is the patient showing signs of a poor oxygen delivery (i.e., low central venous oxygen saturation and/or dyspnea and tachycardia when attempting to ambulate)? Is the patient to follow a normal rehabilitation program? All of these considerations pertain to the decision to administer RBCs, and their exclusion from a propensity matching approach creates an environment for incomplete and incorrect matching. In effect, it is likely that retrospective studies were actually comparing populations with differing degrees of morbidity and mortality risk.
A final point of discussion pertains to the temporal relationship between transfusion administration and outcomes. The retrospective analysis of databases rarely allows for the consideration of important data pertaining to the timing of transfusions. This drawback may make it difficult to understand if the outcome of interest (e.g., acute kidney injury) was present before or after the transfusion. As a result, in some cases, the adverse outcome itself was possibly the trigger for the transfusion, not the reverse—i.e., only an association between the two, not a causative relationship.
Transfusions as quality of care measures
The above considerations and the lack of a clear causative effect of transfusion on adverse outcomes challenge whether to consider transfusion per se as an outcome measure. Some might consider transfusion as a surrogate for perioperative bleeding, e.g., in studies exploring the effects of hemostatic drugs or techniques.18,30 Nevertheless, even in this setting, some important methodological points must be considered. The most important consideration is that transfusions in cardiac surgery patients may be triggered by factors other than directly from bleeding—e.g., preoperative anemia and intraoperative hemodilution. Both of these conditions are important determinants of perioperative transfusions, even in the absence of any significant bleeding, and both are determinants of adverse outcomes independent of any related transfusions.6 In particular, preoperative anemia may be a co-factor of the bleeding-related complications, since preoperatively anemic patients may have a low tolerance to even relatively small amounts of bleeding. To limit the effects of these confounders, some RCTs have successfully introduced strict exclusion criteria based on preoperative anemia and/or very low body surface area as well as withdrawal criteria in case of excessive hemodilution during CPB.18,30 In addition, whenever transfusions are the primary endpoint in an RCT, a well-defined transfusion protocol needs to be strictly followed with few protocol deviations.
Despite the uncertainty and questionable reliability regarding the transfusion of allogeneic blood products as a direct outcome measure, it is still a valuable measure to document in cardiac surgery databases (in terms of both transfusion rate and volume). Although it is currently difficult to reach a definite conclusion that RBC transfusion is an independent determinant of adverse outcomes (unless massive), in many cases, it is possible that they could be avoided. Thus, although rarely dangerous, they may often be inappropriate.
Independent of any potential relationship to adverse outcome, there are several remaining reasons why transfusion should still be contained. Many of these are determined by the concept of patient blood management (PBM).31 First, transfusions are relatively expensive.32 In addition, an ageing population in developed countries is leading to shifts (i.e., declines) in the ratio of potential blood donors to potential blood recipients, with a predictable blood shortage in upcoming years.33 Furthermore, transfusion rates and the number of units transfused may be important markers of the quality of care during the hospital stay.
Many quality of care markers are integrated into PBM programs and can be assessed over time using RBC transfusions as a primary endpoint. All the interventions included in a PBM program are directly or indirectly related to containing the use of allogeneic blood products. For example, correcting preoperative anemia and limiting blood loss resulting from diagnostic laboratory sampling are in what is considered the first (i.e., preoperative) pillar of the PBM and have particular relevance to cardiac surgery settings. The second (i.e., intraoperative) pillar includes a number of interventions that also have particular relevance to cardiac surgery. These include judicious use of cell salvage and limiting hemodilution during CPB; early and directed diagnosis of bleeding mechanisms using point-of-care coagulation testing; and the use of factor concentrates instead of FFP. With respect to the third (i.e., postoperative) pillar of PBM, permissive anemia may also be considered an option. As previously discussed, however, the application of a transfusion protocol that is too restrictive may itself lead to adverse effects. Conversely, it may be beneficial to apply a well-defined transfusion protocol that avoids inhospital variations in the transfusion policy.
Conclusions
In conclusion, perioperative bleeding is a complex clinical entity, though its relationship with increased rates of morbidity/mortality is only robust in cases of massive bleeding. Accordingly, if perioperative bleeding is dichotomized based on severity, it may be considered a relevant outcome in cardiac surgery. In contrast to bleeding, RBC transfusions are not a syndrome, a disease, or a specific adverse outcome. The causative effect of transfusion on adverse outcomes in cardiac surgery remains uncertain. An ongoing RCT, the Transfusion Requirements in Cardiac Surgery III (TRICS III) trial,Footnote 1 is expected to randomize more than 3,600 patients testing different transfusion triggers. The trial is expected to be closed in 2017 and should certainly offer new and relevant information in this field.
Transfusion rates and volumes may be used as primary endpoints as a surrogate for bleeding in studies exploring the effects of hemostatic drugs/products, but such studies must strictly adhere to the transfusion protocols and measures to avoid the confounding effects of anemia. Transfusion-related endpoints may be good markers of quality of care and are appropriate to assess the success of PBM programs.
Notes
ClinicalTrials.gov. Transfusion Requirements in Cardiac Surgery III (TRICS-III). Available from URL: https://clinicaltrials.gov/ct2/show/NCT02042898 (accessed September 2015)
References
Ranucci M. Hemostatic and thrombotic issues in cardiac surgery. Semin Thromb Hemost 2015; 41: 84-90.
Biancari F, Mikkola R, Heikkinen J, Lahtinen J, Airaksinen KE, Juvonen T. Estimating the risk of complications related to re-exploration for bleeding after adult cardiac surgery: a systematic review and meta-analysis. Eur J Cardiothorac Surg 2012; 41: 50-5.
Canadyova J, Zmeko D, Mokracek A. Re-exploration for bleeding or tamponade after cardiac operation. Interact Cardiovasc Thorac Surg 2012; 14: 704-7.
Ranucci M, Bozzetti G, Ditta A, Cotza M, Carboni G, Ballotta A. Surgical reexploration after cardiac operations: why a worse outcome? Ann Thorac Surg 2008; 86: 1557-62
Vivacqua A, Koch CG, Yousuf AM, et al. Morbidity of bleeding after cardiac surgery: is it blood transfusion, reoperation for bleeding, or both? Ann Thorac Surg 2011; 91: 1780-90.
Ranucci M, Baryshnikova E, Castelvecchio S, Pelissero G. Major bleeding, transfusions, and anemia: the deadly triad of cardiac surgery. Ann Thorac Surg 2013; 96: 478-85.
Koch CG, Li L, Duncan AI, et al. Transfusion in coronary artery bypass grafting is associated with reduced long-term survival. Ann Thorac Surg 2006; 81: 1650-7.
Koch CG, Li L, Sessler DI, et al. Duration of red-cell storage and complications after cardiac surgery. N Engl J Med 2008; 358: 1229-39.
Rahe-Meyer N, Hanke A, Schmidt DS, Hagl C, Pichlmaier M. Fibrinogen concentrate reduces intraoperative bleeding when used as first-line hemostatic therapy during major aortic replacement surgery: Results from a randomized, placebo-controlled trial. J Thorac Cardiovasc Surg 2013; 145(3 Suppl): S178-85.
Solomon C, Rahe-Meyer N. Fibrinogen concentrate as first-line therapy in aortic surgery reduces transfusion requirements in patients with platelet counts over or under 100×109/L. Blood Transfus 2015; 13: 248-54.
Sorensen B, Spahn DR, Innerhofer P, Spannagl M, Rossaint R. Clinical review: Prothrombin complex concentrates - evaluation of safety and thrombogenicity. Crit Care 2011; 15: 201.
Gill R, Herbertson M, Vuylsteke A, et al. Safety and efficacy of recombinant activated factor VII: a randomized placebo-controlled trial in the setting of bleeding after cardiac surgery. Circulation 2009; 120: 21-7.
Dyke C, Aronson S, Dietrich W, et al. Universal definition of perioperative bleeding in adult cardiac surgery. J Thorac Cardiovasc Surg 2014; 147(1458-63): e1.
Greiff G, Pleym H, Stenseth R, Berg KS, Wahba A, Videm V. Prediction of bleeding after cardiac surgery: comparison of model performances: a prospective observational study. J Cardiothorac Vasc Anesth 2015; 29: 311-9.
Kinnunen EM, Juvonen T, Airaksinen KE, et al. Clinical significance and determinants of the universal definition of perioperative bleeding classification in patients undergoing coronary artery bypass surgery. J Thorac Cardiovasc Surg 2014; 148(1640-46): e2.
Nakayama Y, Nakajima Y, Tanaka KA, et al. Thromboelastometry-guided intraoperative haemostatic management reduces bleeding and red cell transfusion after paediatric cardiac surgery. Br J Anaesth 2015; 114: 91-102.
Galas FR, de Almeida JP, Fukushima JT, et al. Hemostatic effects of fibrinogen concentrate compared with cryoprecipitate in children after cardiac surgery: a randomized pilot trial. J Thorac Cardiovasc Surg 2014; 148: 1647-55.
Ranucci M, Baryshnikova E, Crapelli GB, et al. Randomized, double-blinded, placebo-controlled trial of fibrinogen concentrate supplementation after complex cardiac surgery. J Am Heart Assoc 2015; 4: e002066.
Faraoni D, Cacheux C, Van Aelbrouck C, Ickx BE, Barvais L, Levy JH. Effect of two doses of tranexamic acid on fibrinolysis evaluated by thromboelastography during cardiac surgery: a randomised, controlled study. Eur J Anaesthesiol 2014; 31: 491-8.
Makhija N, Sarupria A. Kumar Choudhary S, Das S, Lakshmy R, Kiran U. Comparison of epsilon aminocaproic acid and tranexamic acid in thoracic aortic surgery: clinical efficacy and safety. J Cardiothorac Vasc Anesth 2013; 27: 1201-7.
Sigaut S, Tremey B, Ouattara A, et al. Comparison of two doses of tranexamic acid in adults undergoing cardiac surgery with cardiopulmonary bypass. Anesthesiology 2014; 120: 590-600.
Paparella D, Rotunno C, De Palo M, et al. Antithrombin administration in patients with low antithrombin values after cardiac surgery: a randomized controlled trial. Ann Thorac Surg 2014; 97: 1207-13.
Vonk AB, Veerhoek D, van den Brom CE, van Barneveld LJ, Boer C. Individualized heparin and protamine management improves rotational thromboelastometric parameters and postoperative hemostasis in valve surgery. J Cardiothorac Vasc Anesth 2014; 28: 235-41.
Gabel J, Hakimi CS, Westerberg M, Radulovic V, Jeppsson A. Retransfusion of cardiotomy suction blood impairs haemostasis: ex vivo and in vivo studies. Scand Cardiovasc J 2013; 47: 368-76.
Leal-Noval SR, Rincon-Ferrari MD, García-Curiel A, et al. Transfusion of blood components and postoperative infection in patients undergoing cardiac surgery. Chest 2001; 119: 1461-8.
Koch CG, Li L, Duncan AI, et al. Morbidity and mortality risk associated with red blood cell and blood-component transfusion in isolated coronary artery bypass grafting. Crit Care Med 2006; 34: 1608-16.
Murphy GJ, Reeves BC, Rogers CA, Rizvi SI, Culliford L, Angelini GD. Increased mortality, postoperative morbidity, and cost after red blood cell transfusion in patients having cardiac surgery. Circulation 2007; 116: 2544-52.
Hajjar LA, Vincent JL, Galas FR, et al. Transfusion requirements after cardiac surgery: the TRACS randomized controlled trial. JAMA 2010; 304: 1559-67.
Murphy GJ, Pike K, Rogers CA, et al. Liberal or restrictive transfusion after cardiac surgery. N Engl J Med 2015; 372: 997-1008.
Karkouti K, von Heymann C, Jespersen CM, et al. Efficacy and safety of recombinant factor XIII on reducing blood transfusions in cardiac surgery: a randomized, placebo-controlled, multicenter clinical trial. J Thorac Cardiovasc Surg 2013; 146: 927-39.
Shander A, Hofmann A, Isbister J, Van Aken H. Patient blood management-the new frontier. Best Pract Res Clin Anaesthesiol 2013; 27: 5-10.
Hofmann A, Ozawa S, Farrugia A, Farmer SL, Shander A. Economic considerations on transfusion medicine and patient blood management. Best Pract Res Clin Anaesthesiol 2013; 27: 59-68.
Lattimore S, Wickenden C, Brailsford SR. Blood donors in England and North Wales: demography and patterns of donation. Transfusion 2015; 55: 91-9.
Conflicts of interest
Dr. Ranucci is a member of the Steering Committee in Grifols SA for studies on antithrombin in cardiac surgery and received speaker honoraria from CSL Behring, Medtronic Inc., Roche, Medival and Grifols SA.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ranucci, M. Outcome measures and quality markers for perioperative blood loss and transfusion in cardiac surgery. Can J Anesth/J Can Anesth 63, 169–175 (2016). https://doi.org/10.1007/s12630-015-0515-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-015-0515-8