Abstract
Background
Extending the time a parturient is left sitting after induction of spinal anesthesia (i.e., the seated time) has had varying success in decreasing hypotension at Cesarean delivery. This may be due to the current lack of information concerning the dose-response relationship of seated time and rates of hypotension.
Methods
Term parturients scheduled for Cesarean delivery were randomized to receive 11.25 or 15.0 mg of 0.75% intrathecal hyperbaric bupivacaine, and they remained seated after injection for a length of time determined by an up-down sequential method. They were then placed in a wedged position and their blood pressure was measured every minute. Pre-delivery hypotension was considered present if there was a > 20% from baseline drop in systolic blood pressure. The seated time at which 50% of parturients avoided pre-delivery hypotension (median effective seated time) was determined with isotonic regression.
Results
Fifty patients were studied. For the 11.25-mg and 15.0-mg groups, the median effective seated time (95% confidence interval [CI]) was 130 sec (95% CI 117 to 150) and 385 sec (95% CI 381 to 396), respectively.
Conclusions
There exists a seated time after intrathecal injection of hyperbaric bupivacaine where 50% of parturients do not experience hypotension. This seated time increases with an increased dose of bupivacaine. Further work is required to determine the full relationship between seated time and hypotension for other doses of anesthetic and to investigate the clinical utility of this technique for prevention of hypotension. This trial was registered at www.clinicaltrials.gov (NCT01561274).
Résumé
Contexte
La prolongation de la durée pendant laquelle une parturiente est laissée assise après l’induction d’une rachianesthésie (c’est-à-dire le temps assis) a connu des succès variables pour la réduction de l’hypotension au cours de césariennes. Cela peut-être dû au manque de renseignements concernant la relation dose-réponse des temps assis et de la fréquence de l’hypotension.
Méthodes
Des parturientes à terme dont l’accouchement par césarienne était programmé ont été randomisées pour recevoir 11,25 mg ou 15,0 mg de bupivacaïne hyperbare à 0,75 % par voie intrathécale et elles sont restées en position assise après l’injection pendant une durée déterminée par une méthode d’allocation haut-bas séquentielle. Elles ont alors été placées dans une position couchée avec tilt latéral et leur tension artérielle a été mesurée toutes les minutes. Une hypotension préaccouchement a été estimée présente si on constatait une chute de la pression artérielle systolique > 20 % par rapport à la valeur de référence. Le temps assis auquel 50 % des parturientes évitaient l’hypotension préaccouchement (temps assis médian efficace) a été déterminé par régression isotonique.
Résultats
Cinquante patientes ont été étudiées. Dans les groupes 11,25 mg et 15,0 mg, le temps assis médian efficace (intervalle de confiance [IC] à 95 %) a été, respectivement, de 130 secondes (IC à 95 %: 117 à 150) et de 385 secondes (IC à 95 %: 381 à 396).
Conclusions
Il existe un temps assis après injection intrathécale de bupivacaïne hyperbare où 50 % des patientes n’éprouvent pas d’hypotension. Ce temps assis augmente avec l’augmentation de la dose de bupivacaïne. De nouvelles études sont requises pour déterminer la relation complète entre le temps assis et l’hypotension pour d’autres doses d’anesthésiques et pour étudier l’utilité clinique de cette technique pour la prévention de l’hypotension. Cette étude a été enregistrée sur le site www.clinicaltrials.gov (NCT01561274).
Similar content being viewed by others
It is unclear if extending the duration of time a parturient is left in the sitting position (i.e., the seated time) following intrathecal injection of hyperbaric local anesthesia has an effect on the incidence of hypotension during Cesarean delivery. Previous studies that have randomized patients to prolonged seated times showed variable changes in the incidence of hypotension.1–3 Nevertheless, the wide range of seated times and doses of intrathecal anesthetic investigated in these trials makes it difficult to draw any conclusions on the effect, if any, of extended seated time on hypotension. Since the dose-response relationship of seated time with the incidence of hypotension has not been determined, the existence and duration of a seated time where 50% (or any other percentage) of parturients will not experience hypotension is uncertain. In addition, it is unknown if other factors that affect the rate of hypotension, most notably the intrathecal local anesthetic dose, will alter this 50% point. We hypothesized that there is a seated time where 50% of parturients would not experience hypotension (called the median effective seated time) and that its duration would vary with the dose of intrathecal anesthetic. To test this hypothesis, we randomized patients to receive either 11.25 or 15 mg of intrathecal bupivacaine, and we then used separate up-down sequential allocations to determine if there existed a seated time for each group where 50% did not experience hypotension.
Methods
This study received approval from the McGill University Health Centre Research Ethics Office (Nov 14, 2011), and written consent was obtained from all patients. The trial was registered on March 2012 at www.clinicaltrials.gov (NCT01561274). Term non-labouring parturients scheduled for Cesarean delivery were eligible for inclusion. We excluded all patients unable to communicate in English or French as well as those with a body mass index (BMI) of ≥ 35, multiple gestations, fetal or placental abnormalities, hypertensive diseases, or American Society of Anesthesiologists’ physical status ≥ III.
Patient allocation to dose and seated time
Patients were randomized to receive 11.25 or 15 mg of intrathecal bupivacaine, and were then assigned a seated time using an up-down sequence. The randomization to bupivacaine dose occurred after epidural placement using a computer-generated randomization assignment that had been placed in sealed opaque envelopes before commencement of the study. Randomization was first completed in one block of 40 patients and then in five blocks of two patients. The first patient in each group sat for 180 sec after completion of the intrathecal injection. The seated duration for each subsequent patient was determined by the hypotensive response of the previous patient in the same bupivacaine group. If the previous patient in the same bupivacaine group experienced hypotension, the next patient remained seated for 15 sec longer or, conversely, 15 sec less if no hypotension was experienced. If a patient did not develop a T6 blockade by 15 min, the seated time did not change for the next patient in the same bupivacaine group.
Anesthetic management
Patients were allowed clear fluids up to three hours before the surgery. Preoperatively, the L4-5 and L3-4 vertebral interspaces were identified by ultrasound, and after sterile preparation of the skin a double-puncture combined spinal-epidural technique was performed. The epidural space was identified in the L3-4 vertebral interspace with a loss of resistance to < 2 mL of saline through a 16G Tuohy needle. A 20G Perifix® catheter (B. Braun Medical, Inc, Bethlehem, PA, USA) was then introduced 5 cm into the epidural space and fixed in place. The intrathecal space was identified in the L4-5 vertebral interspace with a 27G Whitacre needle. After confirmation by aspiration of < 0.2 mL of cerebrospinal fluid, the intrathecal medication was injected over 30 sec. The bevel of the needle pointed upwards, and there was no barbotage or midpoint verification for cerebrospinal fluid. The intrathecal medication had been prepared immediately beforehand and consisted of 150 µg of preservative-free morphine with the assigned dose of bupivacaine. A physician not involved in the care of the patient prepared a 3 mL syringe with the appropriate medications and placed a sterile bandage over the syringe to mask the volume of liquid. The syringe was left visible up to the 1 mL mark to allow confirmation of placement. After intrathecal injection, the patient was then left in the sitting position for the duration of time predetermined by the up-down sequential method. Each individual patient’s seated time was known only to the physician who had prepared the intrathecal medication, who was responsible for informing the clinical care team when the duration of seated time had been completed. Patients were then immediately positioned supine, and a wedge (10 × 30 × 60 cm) was placed under their right hip. A 10 mL·kg−1 bolus of normal saline was administered and their blood pressure was measured every minute with a noninvasive blood pressure cuff placed on the same arm used for the preoperative assessment. Hypotension was defined as either a > 20% drop in the average of three systolic blood pressures that had been measured in the recumbent position preoperatively (i.e. baseline blood pressure) or a spontaneous complaint from the patient of any nausea, dizziness or faintness. Treatment of hypotension was by intermittent intravenous boluses of phenylephrine 100 µg unless the patient’s heart rate was < 60 beats·min−1, in which case, intravenous ephedrine 5 mg was administered. Any intraoperative complaints of pain were treated with an initial intravenous bolus of fentanyl 50 µg and an epidural injection of 2% lidocaine 5 mL. The height of anesthetic blockade was measured by loss of cold sensation to ice at one, five, ten, and 15 min after being placed supine and then at every ten-minute interval until skin closure. If the patient did not achieve a T6 blockade within the first 15 min, the epidural catheter was used to extend the blockade according to the discretion of the attending anesthesiologist, and a protocol violation was declared for failed spinal.
Statistical analysis
Due to a lack of prior studies, we had no information to allow an a priori sample size calculation for the assessment of between-dose differences in sitting time. We elected to randomize 20 patients to each dose, as a sample size of 20 to 40 has been shown to provide reliable estimates of median effective dose in up-down sequential designs. We selected an initial seated time of 180 seconds based on the study by Kohler et al. showing a 54% incidence of hypotension in parturients receiving hyperbaric bupivacaine 15 mg with a seated time of three minutes. Analysis after 40 patients showed that our predicted median effective seated time for the bupivacaine 15.0-mg group was inaccurate, and we found that we had not yet reached the median effective seated time for that group. We therefore randomized five more patients to each group, for a total of 50 patients.
The median effective seated time was determined using isotonic regression with a pooled adjacent violators algorithm.4 As recommended by Stylianou, the linearly interpolated third estimator of median effectiveness was taken as the median effective seated time.5 Bias-corrected 95% confidence intervals (CI) were determined by bootstrapping.6 Statistical analysis was performed with SPSS® statistics version 19 (SPSS Inc., Chicago, IL, USA), while the isotonic regression was performed with the R statistical package version 3.0.2 (R Foundation for Statistical Computing, Vienna, Austria) using functions written and provided by Pace and Stylianou (personal communication) and the Canty Bootstrap package.
Results
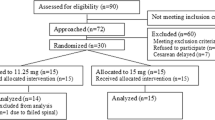
We assessed 143 patients for eligibility and approached 77 patients for consent, 15 of whom refused (Fig. 1). Twelve of the patients who consented were not included, eight due to the delay or cancellation of the Cesarean delivery and four because the neuraxial technique was too difficult to perform in the intended intervertebral spaces. There were no clinically important differences in the baseline characteristics (Table). The 16th patient in the 15-mg group did not develop a T6 blockade before the start of surgery and required additional epidural medication before incision. As per the protocol, the 17th patient in the 15 mg group also remained seated for the same duration as the 16th patient. Due to a data transcription error, the 21st patient in the 11.25-mg group had a seated time that was decreased by 30 sec from the previous patient. No patients developed hypotension in the first two minutes after being placed supine. No difference in baseline variables was observed between the patients who did and did not experience hypotension when comparing patients within one bupivacaine group only or when comparing all patients. For the 11.25-mg and 15.0-mg bupivacaine groups, the median effective seated time was 130 sec (95% CI 117 to 150) and 385 sec (95% CI 381 to 396), respectively (Fig. 2). No patients required additional medication for intraoperative pain before delivery, but there were seven patients in the 11.25-mg group and four in the 15.0-mg group who required additional analgesia for peritoneal closure (Fig. 2). The mean (SD) time after being placed supine for supplemental analgesia administration was 43 (16) min. The onset and maximum cranial spread of the anesthetic blockade was similar in the two groups and was similar amongst those who experienced and did not experience hypotension (Fig. 3).
Discussion
Hypotension is a common complication after neuraxial anesthesia for Cesarean delivery,7 and extending the duration of seated time after intrathecal injection of hyperbaric local anesthetic could possibly reduce its incidence. Since the spread of hyperbaric medication in the intrathecal space is influenced by gravity, remaining seated after an intrathecal injection of hyperbaric local anesthesia may result in decreased cranial spread of the medication, less sympathetic nervous system blockade, and perhaps less hypotension. Nevertheless, it is unclear if a dose-response relationship exists between seated time and the incidence of spinal anesthesia-induced hypotension during Cesarean delivery. We have determined a median effective seated time where 50% of parturients do not experience hypotension after intrathecal injection of hyperbaric bupivacaine.
Previous randomized trials comparing patients assigned to seated times have had varying success in the prevention of hypotension. Kohler et al. randomized parturients to a seated time of zero or three minutes after inducing spinal anesthesia with hyperbaric bupivacaine 14 mg.1 Mardirosoff et al. injected intrathecal hyperbaric bupivacaine 15 mg and randomized non-obstetric patients to seated times of one or four minutes.2 In both studies, the observed rates of hypotension were higher in the groups with the shorter seated time (Kohler et al. 67% vs 54% and Mardirosoff et al. 53% vs 33%); however, the estimates of the differences were imprecise and the results did not achieve statistical significance. In our study, however, we determined that the median effective seated time for patients receiving 15 mg of bupivacaine is more than six minutes. Had Kohler and Mardirosoff extended seated time in their studies, it is possible that larger differences in rates of hypotension may have resulted. El-Hakeem et al. randomized parturients to a seated time of zero or five minutes after intrathecal injection of hyperbaric bupivacaine 10 mg, and they were able to show a decrease in the use of ephedrine from 47% to 8% (difference = 39%; 95% CI 23 to 52).3 It is interesting to point out that El-Hakeem assigned participants to seated times on either side of the median effective seated time that we determined for bupivacaine 11.25 mg.
It is known that the dose of intrathecal local anesthetic alters rates of hypotension and duration of spinal blockade.8 We hypothesized that the dose of hyperbaric medication would alter the median effective seated time for hypotension, although the effect of anesthetic dose on the relation of seated time with hypotension was unknown. To test our hypothesis we determined the median effective seated time for two different doses of intrathecal local anesthetic. We showed non-overlapping 95% CIs in the effective seated times for 15 and 11.25 mg of bupivacaine. This provides evidence that the relationship between seated time and hypotension is dependent on the dose of local anesthetic. It is important to emphasize that we chose to study bupivacaine 15 mg because many practitioners in our institution routinely utilize this dose for Cesarean deliveries, which can be prolonged in duration.
It remains to be seen if the determination of a median effective seated time for avoidance of hypotension prior to Cesarean delivery will have any clinical utility. The median effective time was over six minutes for the 15-mg group, which may be considered too long in a busy clinical setting. The median effective seated time for the 11.25-mg group was just over two minutes, which would be more acceptable. The number of patients who required supplemental analgesia for peritoneal closure may also limit the clinical utility of an extended seated time, as we found that 28% and 16% of the patients in the 11.25-mg and 15-mg groups, respectively, required supplemental analgesia. Nevertheless, the expected need for supplemental analgesia in Cesarean delivery performed under spinal anesthesia without opioids is 24%, decreasing to 4% if opioids are used.9 It is possible that the addition of an intrathecal lipophilic opioid, like fentanyl or sufentanil, may decrease the requirement for supplemental analgesia and make the use of a prolonged seated time more appealing.
The mechanism by which the incidence of hypotension is decreased with prolonged seated times is most likely related to decreased cranial spread of the hyperbaric local anesthetic and decreased sympathetic blockade. There is evidence that a higher anesthetic blockade is associated with greater rates of hypotension,10–12 which supports this possible mechanism. In this study, we did not formally analyze differences in the spread of blockade between patients who experienced hypotension and those who did not. Nevertheless, the observed heights of blockade over time were similar between the two groups. Since our study was not designed to show differences in blockade, it should not be used to refute the relationship of the height of the blockade and hypotension.
There are limitations to this study. We studied patients with singleton pregnancies and with a BMI of < 35. Our results may not be applicable to other patient groups. We did not measure the blood pressure while seated and do not know how the seated time affects the blood pressure before being placed supine. We do know, however, that it took several minutes after the patients were placed supine for hypotension to develop. We utilized a double-puncture combined spinal-epidural anesthetic and do not know if our results can be extrapolated to other anesthesia techniques. Our pre-study estimated median effective seated time for the 15-mg group was much lower than what we actually determined, necessitating an extension to our study. In order to maintain randomization, we chose to enrol more patients in both groups. We cannot state what effect the extended enrolment had on the final results.
We have determined a seated time for hypotension in 50% of patients, but a more clinically important measure would be the seated time where 95% of patients do not experience hypotension. The up-down method utilized in our study provides a good estimate of median effectiveness but does not provide accurate estimates of other effective values. We determined a single point on the dose-response curve for seated time and Cesarean hypotension for two doses of hyperbaric bupivacaine. Further studies would be needed to determine other quantiles (e.g., 95% effective seated time) or a complete dose-response curve for different anesthetic doses and to assess the clinical relevance of seated time for the prevention of hypotension.
References
Kohler F, Sorensen JF, Helbo-Hansen HS. Effect of delayed supine positioning after induction of spinal anaesthesia for caesarean section. Acta Anaesthesiol Scand 2002; 46: 441-6.
Mardirosoff C, Dumont L, Deyaert M, Leconte M. Posture-related distribution of hyperbaric bupivacaine in cerebro-spinal fluid is influenced by spinal needle characteristics. Acta Anaesthesiol Scand 2001; 45: 772-5.
El-Hakeem EE, Kaki AM, Almazrooa AA, Al-Mansouri NM, Alhashemi JA. Effects of sitting up for five minutes versus immediately lying down after spinal anesthesia for cesarean delivery on fluid and ephedrine requirement; a randomized trial. Can J Anesth 2011; 58: 1083-9.
Pace NL, Stylianou MP. Advances in and limitations of up-and-down methodology: a précis of clinical use, study design, and dose estimation in anesthesia research. Anesthesiology 2007; 107: 144-52.
Stylianou M, Flournoy N. Dose finding using the biased coin up-and-down design and isotonic regression. Biometrics 2002; 58: 171-7.
Stylianou M, Proschan M, Flournoy N. Estimating the probability of toxicity at the target dose following an up-and-down design. Stat Med 2003; 22: 535-43.
Maayan-Metzger A, Schushan-Eisen I, Todris L, Etchin A, Kuint J. Maternal hypotension during elective cesarean section and short-term neonatal outcome. Am J Obstet Gynecol 2010; 202: 56e1-5.
Van de Velde M, Van Schoubroeck D, Jani J, Teunkens A, Missant C, Deprest J. Combined spinal-epidural anesthesia for cesarean delivery: dose-dependent effects of hyperbaric bupivacaine on maternal hemodynamics. Anesth Analg 2006; 103: 187-90.
Dahl JB, Jeppesen IS, Jorgensen H, Wetterslev J, Moiniche S. Intraoperative and postoperative analgesic efficacy and adverse effects of intrathecal opioids in patients undergoing cesarean section with spinal anesthesia: a qualitative and quantitative systematic review of randomized controlled trials. Anesthesiology 1999; 91: 1919-27.
Brenck F, Hartmann B, Katzer C, et al. Hypotension after spinal anesthesia for cesarean section: identification of risk factors using an anesthesia information management system. J Clin Monit Comput 2009; 23: 85-92.
Carpenter RL, Caplan RA, Brown DL, Stephenson C, Wu R. Incidence and risk factors for side effects of spinal anesthesia. Anesthesiology 1992; 76: 906-16.
Klasen J, Junger A, Hartmann B, et al. Differing incidences of relevant hypotension with combined spinal-epidural anesthesia and spinal anesthesia. Anesth Analg 2003; 96: 1491-5.
Conflicts of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author contributions
Albert Moore, Samuel Bourassa-Blanchette, Aly el-Bahrawy, William Li-Pi-Shan, and Roupen Hatzakorzian participated in the design of the study. Albert Moore, Samuel Bourassa-Blanchette, Eva el-Mouallem, Ian Kaufman, and Aly el-Bahrawy participated in the performance of the study. Albert Moore, Samuel Bourassa-Blanchette, Ian Kaufman, and Aly el-Bahrawy participated in the data analysis. Albert Moore, Samuel Bourassa-Blanchette, Eva el-Mouallem, Ian Kaufman, Aly el-Bahrawy, William Li-Pi-Shan, and Roupen Hatzakorzian participated in the preparation of the manuscript.
Rights and permissions
About this article
Cite this article
Moore, A., Bourrassa-Blanchette, S., El Mouallem, E. et al. The median effective seated time for hypotension induced by spinal anesthesia at Cesarean delivery with two doses of hyperbaric bupivacaine: a randomized up-down sequential allocation study. Can J Anesth/J Can Anesth 61, 916–921 (2014). https://doi.org/10.1007/s12630-014-0208-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-014-0208-8