Abstract
Purpose
To determine the 90% effective dose (ED90) of intrathecal hyperbaric bupivacaine for Cesarean delivery under combined spinal–epidural anesthesia (CSE) in parturients with super obesity (body mass index [BMI] ≥ 50 kg·m−2).
Methods
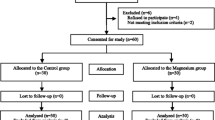
We enrolled parturients with BMI ≥ 50 kg·m−2 with term, singleton vertex pregnancies undergoing elective Cesarean delivery under CSE. An independent statistician generated the 0.75% hyperbaric bupivacaine dosing regimen in increments of 0.75 mg using a biased-coin up-down sequential allocation technique. This was combined with 15 μg fentanyl, 150 μg morphine, and normal saline to a volume of 2.05 mL. The initial and maximum doses were 9.75 mg and 12 mg, respectively. Participants, clinical team, and outcome assessors were blinded to the dose. The primary outcome was block success, defined as T6 block to pinprick within ten minutes and no intraoperative analgesic supplementation within 90 min of spinal injection. We determined the ED90 using logistic regression.
Results
We enrolled 45 parturients and included 42 in the analysis. All doses achieved a T6 level within ten minutes, and the primary outcome occurred in 0/1 (0%) of the 9.75-mg doses, 2/3 (67%) of the 10.5-mg doses, 21/27 (78%) of the 11.25-mg doses, and 11/11 (100%) of the 12-mg doses. The ED90 of hyperbaric bupivacaine was 11.56 mg (95% confidence interval, 11.16 to 11.99). Four parturients (9.5%) had sensory level higher than T2, but none was symptomatic or required general anesthesia.
Conclusion
The estimated ED90 of hyperbaric bupivacaine with fentanyl and morphine in parturients with super obesity undergoing Cesarean delivery under CSE was approximately 11.5 mg.
Study registration
ClinicalTrials.gov (NCT03781388); first submitted 18 December 2018.
Résumé
Objectif
Notre objectif était de déterminer la dose efficace à 90 % (DE90) de bupivacaïne hyperbare intrathécale pour l’accouchement par césarienne sous péri-rachianesthésie combinée (PRC) chez les personnes parturientes atteintes de super obésité (indice de masse corporelle [IMC] ≥ 50 kg·m−2).
Méthode
Nous avons recruté des personnes parturientes ayant un IMC ≥ 50 kg·m−2 présentant des grossesses uniques à terme, en présentation céphalique et bénéficiant d’un accouchement par césarienne programmée sous PRC. Un·e statisticien·ne indépendant·e a généré le schéma posologique de bupivacaïne hyperbare à 0,75 % par incréments de 0,75 mg à l’aide d’une technique d’allocation séquentielle en escalier. La bupivacaïne a été combinée à 15 μg de fentanyl, 150 μg de morphine et à une solution physiologique salée jusqu’à un volume de 2,05 mL. Les doses initiale et maximale étaient respectivement de 9,75 mg et 12 mg. Les participant·es, l’équipe clinique et les personnes évaluant les résultats n’avaient pas connaissance de la dose. Le critère d’évaluation principal était la réussite du bloc, définie comme un bloc à T6 à la piqûre dans les dix minutes et aucune supplémentation analgésique peropératoire dans les 90 minutes suivant l’injection rachidienne. Nous avons déterminé la DE90 à l’aide d’une méthode de régression logistique.
Résultats
Nous avons recruté 45 personnes parturientes et en avons inclus 42 dans l’analyse. Toutes les doses ont atteint le niveau T6 en dix minutes, et le critère d’évaluation principal a été obtenu pour 0/1 (0 %) des doses de 9,75 mg, 2/3 (67 %) des doses de 10,5 mg, 21/27 (78 %) des doses de 11,25 mg et 11/11 (100 %) des doses de 12 mg. La DE90 de bupivacaïne hyperbare était de 11,56 mg (intervalle de confiance à 95 %, 11,16 à 11,99). Quatre personnes parturientes (9,5 %) ont affiché un niveau sensoriel supérieur à T2, mais aucune n’était symptomatique ni n’a nécessité d’anesthésie générale.
Conclusion
La DE90 estimée de bupivacaïne hyperbare avec fentanyl et morphine chez les personnes parturientes hyperobèses bénéficiant d’une césarienne sous PRC était d’environ 11,5 mg.
Enregistrement de l'étude
ClinicalTrials.gov (NCT03781388); soumis pour la première fois le 18 décembre 2018.


Similar content being viewed by others
References
American College of Obstetricians and Gynecologists. Obesity in pregnancy: ACOG Practice Bulletin, Number 230. Obstet Gynecol 2021; 137: e128–44. https://doi.org/10.1097/aog.0000000000004395
Tonidandel A, Booth J, D’Angelo R, Harris L, Tonidandel S. Anesthetic and obstetric outcomes in morbidly obese parturients: a 20-year follow-up retrospective cohort study. Int J Obstet Anesth 2014; 23: 357–64. https://doi.org/10.1016/j.ijoa.2014.05.004
Tan HS, Habib AS. Obesity in women: anaesthetic implications for peri‐operative and peripartum management. Anaesthesia 2021; 76: 108–17. https://doi.org/10.1111/anae.15403
Betran AP, Ye J, Moller AB, Souza JP, Zhang J. Trends and projections of Caesarean section rates: global and regional estimates. BMJ Glob Health 2021; 6: e005671. https://doi.org/10.1136/bmjgh-2021-005671
Saucedo M, Esteves-Pereira AP, Pencolé L, et al. Understanding maternal mortality in women with obesity and the role of care they receive: a national case-control study. Int J Obes (Lond) 2021; 45: 258–65. https://doi.org/10.1038/s41366-020-00691-4
Onishi E, Murakami M, Hashimoto K, Kaneko M. Optimal intrathecal hyperbaric bupivacaine dose with opioids for Cesarean delivery: a prospective double-blinded randomized trial. Int J Obstet Anesth 2017; 31: 68–73. https://doi.org/10.1016/j.ijoa.2017.04.001
Ginosar Y, Mirikatani E, Drover DR, Cohen SE, Riley ET. ED50 and ED95 of intrathecal hyperbaric bupivacaine coadministered with opioids for cesarean delivery. Anesthesiology 2004; 100: 676–82. https://doi.org/10.1097/00000542-200403000-00031
Lee Y, Balki M, Parkes R, Carvalho JC. Dose requirement of intrathecal bupivacaine for Cesarean delivery is similar in obese and normal weight women. Rev Bras Anestesiol 2009; 59: 674–83. https://doi.org/10.1016/s0034-7094(09)70092-3
Tubog TD, Ramsey VL, Filler L, Bramble RS. Minimum effective dose (ED50 and ED95) of intrathecal hyperbaric bupivacaine for Cesarean delivery: a systematic review. AANA J 2018; 86: 348–60.
Hogan QH, Prost R, Kulier A, Taylor ML, Liu S, Mark L. Magnetic resonance imaging of cerebrospinal fluid volume and the influence of body habitus and abdominal pressure. Anesthesiology 1996; 84: 1341–9. https://doi.org/10.1097/00000542-199606000-00010
Carpenter RL, Hogan QH, Liu SS, Crane B, Moore J. Lumbosacral cerebrospinal fluid volume is the primary determinant of sensory block extent and duration during spinal anesthesia. Anesthesiology 1998; 89: 24–9. https://doi.org/10.1097/00000542-199807000-00007
Brodsky JB, Lemmens HJ. Regional anesthesia and obesity. Obes Surg 2007; 17: 1146–9. https://doi.org/10.1007/s11695-007-9207-y
Soens MA, Birnbach DJ, Ranasinghe JS, van Zundert A. Obstetric anesthesia for the obese and morbidly obese patient: an ounce of prevention is worth more than a pound of treatment. Acta Anaesthesiol Scand 2008; 52: 6–19. https://doi.org/10.1111/j.1399-6576.2007.01483.x
Patel SD, Habib AS. Anaesthesia for the parturient with obesity. BJA Educ 2021; 21: 180–6. https://doi.org/10.1016/j.bjae.2020.12.007
Hartwell BL, Datta S, Aglio LS, Hauch MA. Vertebral column length and spread of hyperbaric subarachnoid bupivacaine in the term parturient. Reg Anesth Pain Med 1991; 16: 17–9.
Norris MC. Height, weight, and the spread of subarachnoid hyperbaric bupivacaine in the term parturient. Anesth Analg 1988; 67: 555–8.
Carvalho B, Collins J, Drover DR, Atkinson Ralls L, Riley ET. ED(50) and ED(95) of intrathecal bupivacaine in morbidly obese patients undergoing Cesarean delivery. Anesthesiology 2011; 114: 529–35. https://doi.org/10.1097/aln.0b013e318209a92d
Ngaka TC, Coetzee JF, Dyer RA. The influence of body mass index on sensorimotor block and vasopressor requirement during spinal anesthesia for elective Cesarean delivery. Anesth Analg 2016; 123: 1527–34. https://doi.org/10.1213/ane.0000000000001568
Lamon AM, Einhorn LM, Cooter M, Habib AS. The impact of body mass index on the risk of high spinal block in parturients undergoing Cesarean delivery: a retrospective cohort study. J Anesth 2017; 31: 552–8. https://doi.org/10.1007/s00540-017-2352-0
Ivanova A, Montazer-Haghighi A, Mohanty SG, Durham SD. Improved up-and-down designs for phase I trials. Stat Med 2003; 22: 69–82. https://doi.org/10.1002/sim.1336
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009; 42: 377–81. https://doi.org/10.1016/j.jbi.2008.08.010
Ross VH, Dean LS, Thomas JA, Harris LC, Pan PH. A randomized controlled comparison between combined spinal-epidural and single-shot spinal techniques in morbidly obese parturients undergoing Cesarean delivery: time for initiation of anesthesia. Anesth Analg 2014; 118: 168–72. https://doi.org/10.1213/ane.0000000000000022
Butwick A, Carvalho B, Danial C, Riley E. Retrospective analysis of anesthetic interventions for obese patients undergoing elective Cesarean delivery. J Clin Anesth 2010; 22: 519–26. https://doi.org/10.1016/j.jclinane.2010.01.005
Katz D, Hamburger J, Gutman D, et al. The effect of adding subarachnoid epinephrine to hyperbaric bupivacaine and morphine for repeat cesarean delivery: a double-blind prospective randomized control trial. Anesth Analg 2018; 127: 171–8. https://doi.org/10.1213/ane.0000000000002542
She YJ, Liu WX, Wang LY, Ou XX, Liang HH, Lei DX. The impact of height on the spread of spinal anesthesia and stress response in parturients undergoing Caesarean section: a prospective observational study. BMC Anesthesiol 2021; 21: 298. https://doi.org/10.1186/s12871-021-01523-2
Plaat F, Stanford SE, Lucas DN, et al. Prevention and management of intra‐operative pain during caesarean section under neuraxial anaesthesia: a technical and interpersonal approach. Anaesthesia 2022; 77: 588–97. https://doi.org/10.1111/anae.15717
Klimek M, Rossaint R, van de Velde M, Heesen M. Combined spinal-epidural vs. spinal anaesthesia for Caesarean section: meta-analysis and trial-sequential analysis. Anaesthesia 2018; 73: 875–88. https://doi.org/10.1111/anae.14210
Author contributions
Ashraf S. Habib contributed to all aspects of this manuscript, including conception and design; acquisition, analysis, and interpretation of data; and drafting the article and revising it critically for intellectual content. Matthew Fuller contributed to the analysis of the data. Hon Sen Tan, Emily Barney, Olga Diomede, Riley Landreth, Trung Pham, Samantha Rubright, and Liliane Ernst contributed to the acquisition and interpretation of data and drafting of the article.
Acknowledgements
The authors acknowledge the contribution of the members of the Division of Women’s Anesthesia at Duke University Medical Center for their assistance with this study.
Disclosures
None.
Funding statement
Ashraf Habib has received research support from Pacira Biosciences, Haisco USA and Heron Therapeutics. He has also served on the Advisory Board for MDoloris, Vertex Pharmaceuticals, Merck and Heron Therapeutics.
Prior conference presentations
This study was presented in part at the 2023 Annual Meeting of the Society for Obstetric Anesthesia and Perinatology (3–7 May, New Orleans, LA, USA).
Editorial responsibility
This submission was handled by Dr. Ronald B. George, Associate Editor, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tan, H.S., Fuller, M.E., Barney, E.Z. et al. The 90% effective dose of intrathecal hyperbaric bupivacaine for Cesarean delivery under combined spinal–epidural anesthesia in parturients with super obesity: an up-down sequential allocation study. Can J Anesth/J Can Anesth 71, 570–578 (2024). https://doi.org/10.1007/s12630-024-02705-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-024-02705-5