Abstract
Objectives
Frailty has become an independent risk factor for adverse outcomes in critically ill patients. This study aimed to explore the predictive ability of two electronic medical record-based frailty assessment tools, the Hospital Frailty Risk Score (HFRS) and Frailty Index based on physiological and laboratory tests (FI-lab), for long-term adverse prognosis in older critically ill survivors.
Design
Retrospective observational study.
Setting and Participants
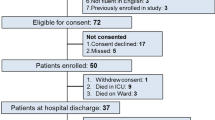
9,082 critically ill survivors aged ≥ 65 years.
Measurements
The HFRS and the 33-item FI-lab were constructed based on the published literature. Cox and logistic regression models assessed the association between frailty and 1-year mortality and post-discharge care needs.
Results
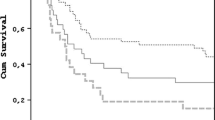
2,586 patients died within 1 year of follow-up. In fully adjusted models, frailty assessed using both the HFRS (per point, hazard ratio [HR] 1.06, 95% confidential interval [CI] 1.05–1.06; intermediate frailty risk, HR 2.00, 95% CI 1.78–2.25; high frailty risk, HR 3.06, 95% CI 2.68–3.50) and FI-lab (per 0.01 points, HR 1.03, 95% CI 1.03–1.03; intermediate frailty risk, HR 1.59, 95% CI 1.44–1.76; high frailty risk, HR 2.30, 95% CI 2.06–2.57) was associated with mortality. Addition of frailty indicators improved the predictive validity of the Sequential Organ Failure Assessment score for mortality (HFRS alone Δ C-index 0.034; FI-lab alone Δ C-index 0.016; HFRS and FI-lab combined Δ C-index 0.042). The HFRS but not the FI-lab was associated with higher probability of post-discharge care needs.
Conclusion
Both the HFRS and FI-lab could independently predict 1-year mortality in older critically ill survivors. Adding the HFRS to the SOFA score model improved it more than adding the FI-lab. The greatest improvement was achieved when both frailty indicators were used together. These findings suggest that electronic medical record-based frailty assessment methods can be useful tools for predicting long-term outcomes in older critically ill patients.


Similar content being viewed by others
Data availability statement: The MIMIC-IV database are available in PhysioNet (https://physionet.org).
References
Ihra GC, Lehberger J, Hochrieser H, et al. Development of demographics and outcome of very old critically ill patients admitted to intensive care units. Intensive Care Med. 2012;38(4):620–626.
Nguyen YL, Angus DC, Boumendil A, Guidet B. The challenge of admitting the very elderly to intensive care. Ann Intensive Care. 2011;1(1):29.
Bagshaw SM, Webb SA, Delaney A, et al. Very old patients admitted to intensive care in Australia and New Zealand: a multi-centre cohort analysis. Crit Care. 2009;13(2):R45.
Desai SV, Law TJ, Needham DM. Long-term complications of critical care. Crit Care Med. 2011;39(2):371–379.
Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13(10):818–829.
Vincent JL, Moreno R, Takala J, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22(7):707–710.
Hoogendijk EO, Afilalo J, Ensrud KE, Kowal P, Onder G, Fried LP. Frailty: implications for clinical practice and public health. Lancet. 2019;394(10206):1365–1375.
Xia F, Zhang J, Meng S, Qiu H, Guo F. Association of Frailty With the Risk of Mortality and Resource Utilization in Elderly Patients in Intensive Care Units: A Meta-Analysis. Front Med (Lausanne). 2021;8:637446.
Bagshaw SM, Stelfox HT, McDermid RC, et al. Association between frailty and short- and long-term outcomes among critically ill patients: a multicentre prospective cohort study. CMAJ. 2014;186(2):E95–102.
Brummel NE, Bell SP, Girard TD, et al. Frailty and Subsequent Disability and Mortality among Patients with Critical Illness. Am J Respir Crit Care Med. 2017;196(1):64–72.
McDermid RC, Stelfox HT, Bagshaw SM. Frailty in the critically ill: a novel concept. Crit Care. 2011;15(1):301.
Bertschi D, Waskowski J, Schilling M, Donatsch C, Schefold JC, Pfortmueller CA. Methods of Assessing Frailty in the Critically Ill: A Systematic Review of the Current Literature. Gerontology. 2022;68(12):1321–1349.
Rockwood K, Song X, MacKnight C, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173(5):489–495.
Pugh RJ, Battle CE, Thorpe C, et al. Reliability of frailty assessment in the critically ill: a multicentre prospective observational study. Anaesthesia. 2019;74(6):758–764.
Gilbert T, Neuburger J, Kraindler J, et al. Development and validation of a Hospital Frailty Risk Score focusing on older people in acute care settings using electronic hospital records: an observational study. Lancet. 2018;391(10132):1775–1782.
Subramaniam A, Ueno R, Tiruvoipati R, Srikanth V, Bailey M, Pilcher D. Comparison of the predictive ability of clinical frailty scale and hospital frailty risk score to determine long-term survival in critically ill patients: a multicentre retrospective cohort study. Crit Care. 2022;26(1):121.
Bruno RR, Wernly B, Flaatten H, Scholzel F, Kelm M, Jung C. The hospital frailty risk score is of limited value in intensive care unit patients. Crit Care. 2019;23(1):239.
Redfern OC, Harford M, Gerry S, Prytherch D, Watkinson PJ. Frailty and unplanned admissions to the intensive care unit: a retrospective cohort study in the UK. Intensive Care Med. 2020;46(7):1512–1513.
Blodgett JM, Theou O, Howlett SE, Wu FC, Rockwood K. A frailty index based on laboratory deficits in community-dwelling men predicted their risk of adverse health outcomes. Age Ageing. 2016;45(4):463–468.
Howlett SE, Rockwood MR, Mitnitski A, Rockwood K. Standard laboratory tests to identify older adults at increased risk of death. BMC Med. 2014;12:171.
Bai W, Hao B, Xu L, Qin J, Xu W, Qin L. Frailty index based on laboratory tests improves prediction of short-and long-term mortality in patients with critical acute myocardial infarction. Front Med (Lausanne). 2022;9:1070951.
Goldberger AL, Amaral LA, Glass L, et al. PhysioBank, PhysioToolkit, and PhysioNet: components of a new research resource for complex physiologic signals. Circulation. 2000;101(23):E215–220.
Johnson A, Bulgarelli L, Pollard T, Celi LA, Mark R, Horng S. MIMIC-IV (version 2.0). PhysioNet. 2022; Available from: https://doi.org/10.13026/as7t-c445.
Zampieri FG, Iwashyna TJ, Viglianti EM, et al. Association of frailty with short-term outcomes, organ support and resource use in critically ill patients. Intensive Care Med. 2018;44(9):1512–1520.
Le Gall JR, Lemeshow S, Saulnier F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA. 1993;270(24):2957–2963.
Nishimura S, Kumamaru H, Shoji S, et al. Assessment of coding-based frailty algorithms for long-term outcome prediction among older people in community settings: a cohort study from the Shizuoka Kokuho Database. Age Ageing. 2022;51(3).
McAlister F, van Walraven C. External validation of the Hospital Frailty Risk Score and comparison with the Hospital-patient One-year Mortality Risk Score to predict outcomes in elderly hospitalised patients: a retrospective cohort study. BMJ Qual Saf. 2019;28(4):284–288.
Gilbert T, Cordier Q, Polazzi S, et al. External validation of the Hospital Frailty Risk Score in France. Age Ageing. 2022;51(1).
Eckart A, Hauser SI, Haubitz S, et al. Validation of the hospital frailty risk score in a tertiary care hospital in Switzerland: results of a prospective, observational study. BMJ Open. 2019;9(1):e026923.
Ladha KS, Zhao K, Quraishi SA, et al. The Deyo-Charlson and Elixhauser-van Walraven Comorbidity Indices as predictors of mortality in critically ill patients. BMJ Open. 2015;5(9):e008990.
Gu JJ, Liu Q, Zheng LJ. A Frailty Assessment Tool to Predict In-Hospital Mortality in Patients with Acute Exacerbations of Chronic Obstructive Pulmonary Disease. Int J Chron Obstruct Pulmon Dis. 2021;16:1093–1100.
Montgomery CL, Rolfson DB, Bagshaw SM. Frailty and the Association Between Long-Term Recovery After Intensive Care Unit Admission. Crit Care Clin. 2018;34(4):527–547.
Acknowledgement: We acknowledge the Laboratory for Computational Physiology team from the Massachusetts Institute of Technology (LCP-MIT) who establish and maintain the MIMIC-IV databases.
Funding
Funding: Not available.
Author information
Authors and Affiliations
Contributions
Author contributions: Study concept and design: H-BL, LS and B-CH. Acquisition of data: B-CH, W-HX, W-YG, JQ and T-KH. Analysis and interpretation of data: D-YL, H-NX, H-YL and LL. Drafting of the manuscript: B-CH, W-HX and W-YG. Critical revision of the manuscript for important intellectual content: H-BL, LS, B-CH, W-HX, W-YG, T-KH, LL, D-YL, H-NX, H-YL and JQ.
Corresponding authors
Ethics declarations
Conflicts of interest: The authors declare that they have no Conflicts of interest.
Ethics approval and consent to participate: The establishment of this de-identified database was approved by the Institutional Review Board at the Beth Israel Deaconess Medical Center. Written informed consent for participation was not required for this project in accordance with the national legislation and the institutional requirements.
Electronic Supplementary Material
12603_2023_1961_MOESM1_ESM.docx
Association between frailty assessed using two electronic medical record-based frailty assessment tools and long-term adverse prognosis in older critically ill survivor
Rights and permissions
About this article
Cite this article
Hao, B., Xu, W., Gao, W. et al. Association between Frailty Assessed Using Two Electronic Medical Record-Based Frailty Assessment Tools and Long-Term Adverse Prognosis in Older Critically Ill Survivors. J Nutr Health Aging 27, 649–655 (2023). https://doi.org/10.1007/s12603-023-1961-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-023-1961-6