Abstract
Background/Objectives
To date, data are lacking on the proportion of residents, and employees who have actually been exposed to SARS-Cov-2 in nursing homes and geriatric healthcare institutions, as well as the evolution of their serological status and the recurrence of Covid-19. The primary objective was to determine the prevalence of COVID-19 using NG Biotech rapid serological tests among caregivers and residents. The secondary objectives were to determine: prevalence according to RT PCR tests or clinical diagnosis; the risk factors (autonomy, arterial hypertension, diabetes mellitus) and clinical presentation (e.g. respiratory, abdominal or cutaneous symptoms, asthenia, fever) among residents; the risk factors (age, sex, profession, family situation) among caregivers; the evolution of the serological status at 1, 3 and 6 months using NG Biotech rapid serological tests; the symptomatic recurrence of Covid 19 at 1, 3 and 6 months.
Design
Multicentric prospective observational.
Setting
Study location: 27 nursing homes and 3 multilevel geriatric hospitals belonging to the UNIVI Group in France.
Participants
1334 professionals: 692 among multilevel geriatric hospitals (mean age: 43.6+/−11.8; 441 (82.4%) female) and 642 among nursing homes (mean age: 43.5+/−12.4; 685 (85.9%) female), and 1145 residents (mean age: 89+/−7.5; 898 (78.7%) female).
Measurements
Prevalence using NG Biotech rapid serological tests, medical diagnosis, RT-PCR tests. Risk factors among residents using the medical file and among caregivers using questionnaires. Clinical presentation in residents using the medical file.
Results
The prevalence using NG Biotech rapid serological test in residents was 14.4 % (168 of 1142 available diagnostics), the global prevalence (positive RT-PCR or positive serological test) was 22.7% (203 of 895 available diagnostics). The prevalence using NG Biotech rapid serological test in professionals was 12.8% (164 of 1315 available diagnostics), the global prevalence (positive RT-PCR test or positive serological test) was 23.8% (222 of 933 available diagnostics). The risk factors among residents were: living in an Alzheimer unit, and being a contact case. Being independent for activities of daily living was protective. The risk factor among caregivers was being a contact case. Another risk factor was the job; nurse assistants, nurses, and physicians were the most exposed. Residents had atypical clinical presentations including frequent geriatric syndromes (falls, delirium). 68.3% (71 of 104) of the initially positive residents still had a positive rapid serological test at 1 month follow up and 74 % (54 of 73) at 3 months follow up. 77.9% (88 of 113) of the initially positive employees still had a positive rapid serological test at 1 month follow up. Symptomatic reinfection was exceptional in caregivers or in residents during follow up.
Conclusion
COVID 19 prevalence among caregivers and residents in nursing homes and geriatric health Institutions is underestimated when using only one method for diagnosis. Geriatric syndromes such as falls and delirium in residents should trigger further investigations on a COVID-19 cause. Immunity was persistent in ¾ of caregivers and residents during the 3 months follow up. The high prevalence of COVID 19 in geriatric institutions pleads in favor of the French vaccination policy, initially targeting as a priority the most vulnerable and dependent people, followed by staff members in healthcare institutions and nursing homes. More studies on the persistence of immunity and the perspective of Covid 19 mutations will help determine the long-term vaccine booster policy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) was first reported in December 2019 in China. In February 2020, the Word Health Organization (WHO) named the disease caused by SARS-CoV-2 the 2019 Coronavirus disease (COVID-19) (1, 2).
In March 2020 the WHO declared the outbreak of a pandemic. COVID-19 rapidly spread in France, and was associated with high death rates, especially in older people (3, 4).
In May 2020, The Epidemiology and Living conditions linked to COVID-19 study (EpiCov) was carried out in France. It included 370,000 randomly selected people. According to this study, 4.5% of the French population had a SARS-CoV-2-positive serology. One of the risk factors of contamination was being a caregiver (5).
After the first COVID outbreak, the situation of the COVID 19 epidemic in geriatric healthcare institutions showed that both residents and caregivers had paid a heavy tribute and focused interventions were needed.
ELISA rapid serological tests can provide an assessment of immunological status (detection of IgG antibodies) in 15 minutes on a finger-prick blood sample. The French health authorities (Haute Autorité de Santé, HAS) (6) and the WHO(7) have validated use of these tests, notably for investigating on-going outbreaks, and for identifying previously infected individuals.
Residents and healthcare professionals of 30 geriatric healthcare institutions belonging to the UNIVI Group were invited to undergo ELISA rapid serological tests to ascertain their COVID-19 serological profile.
The primary objective of this study was to determine the prevalence of COVID-19 using NG Biotech rapid serological tests among caregivers and residents
The secondary objectives were to determine prevalence according to RT PCR tests or clinical diagnosis; the risk factors (autonomy, arterial hypertension, diabetes mellitus) and clinical presentation (e.g. respiratory, abdominal or cutaneous symptoms, asthenia, fever) among residents; the risk factors (age, sex, profession, family situation) among caregivers; the evolution of the serological status at 1, 3 and 6 months using NG Biotech rapid serological tests; the symptomatic recurrence of Covid 19 at 1, 3 and 6 months
Methods
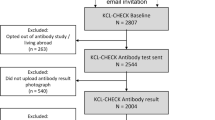
Design
This was a prospective observational multicentric study conducted between July 24th 2020 and October 16th 2020 during a Covid-19 testing campaign launched by the UNIVI Group, a network of 71 healthcare institutions in France specialized in care for disabled and older persons. Participants in this study were recruited in the 27 nursing homes (1926 residents and 1165 employees), and the three multilevel geriatric hospitals (1092 employees) that constitute the UNIVI Group’s geriatric institutions.
The Group decided to use an ELISA rapid serological test to ascertain the serological profile of the nursing home residents and caregivers and the multilevel geriatric hospital caregivers. NG Biotech finger-stick IgG-IgM combined antibody rapid tests were used (8, 9).
Residents and employees with a positive rapid serological test or a positive RT-PCR test were invited to attended follow-up visits at 1, 3 and 6 months for rapid serological tests.
Participants
-
All participants who had an ELISA rapid serological test were retained for analysis.
-
All residents of the 27 nursing homes, including those under legal guardianship, were invited to participate in the study.
-
All employees of the 30 healthcare institutions (27 nursing homes and 3 multilevel geriatric hospitals) were invited to participate in the study, irrespective of occupation.
-
As the objective of the study was to give an accurate as possible description of the population, no exclusion criteria were defined.
-
Results from vaccinated persons were not retained for analysis.
Data collection
Criteria for overall population
The results of three diagnostic strategies - clinical diagnosis, positive reverse transcriptase polymerase chain reaction (RT-PCR) results, serological tests - were collected. Positive diagnosis of infection since the beginning of the pandemic was recorded as follows:
-
probable SARS-CoV-2 infection based on symptoms and physical examination,
-
ongoing SARS-Cov-2 infection determined by a positive RT-PCR diagnostic test,
-
previous viral encounter determined by a positive NG Biotech rapid serological test.
The overall diagnosis of SARS-Cov-2 infection was considered positive if either the RT-PCR test or the rapid serological test was positive. Clinical assessment was not considered for determining the overall diagnosis. If the RT-PCR test data was unavailable and the rapid serological test negative, the overall diagnosis was not retained for analysis.
Criteria specific to residents
Symptoms associated with a clinical diagnosis of probable SARS-CoV-2 infection were recorded. Potential risk factors were also noted:
-
Autonomy measured by Iso-Ressource group (GIR) which is a national scale to evaluate the degree of autonomy in older persons (GIR 1/2: very dependent, GIR 3/4: moderately dependent, GIR 5/6: independent)
-
Arterial hypertension
-
Diabetes mellitus
-
Contact with an infected person
All information was gathered from the resident’s medical files.
Criteria specific to staff members
Various potential risk factors were collected:
-
Age and gender
-
Profession
-
Type of housing (house or apartment)
-
Family context (single, couple without or with children, single-parent)
-
Mode of transportation (car, public transportation, walk/bike)
-
Contact with an infected person.
Global data
The number of deaths among residents in each institution was collected from death certificate data for the period of March through May for the last three years (2018 to 2020).
Follow-up data
Results of rapid serological tests performed at follow-up visits one, three and six months after inclusion were recorded for employees and residents who had an initially positive diagnosis of infection (RT-PCR test and/or rapid serological test).
Data on any new infections clinically suspected and confirmed by RT PCR test, were also collected.
Ethics
The study protocol received approval before the beginning of the study from local authorities (Comité de Protection des Personnes Ile de France 1, N° IORG0009918). All participants (or the legal representative when appropriate) were informed about the study and those who declined to participate were not included.
The study was registered in clinicaltrials.gov (NCT04790994).
Statistical analysis
Numeric data were described by mean and standard deviation (SD). Qualitative data were described by number and proportion of each modality.
The proportion of residents or employees with a positive test or diagnosis was computed.
To assess the impact of factors on the infection risk, mixed logistic models were used, including the factor as a fixed effect and the institution as a random effect. This was necessary because of considerable geographic differences in the pandemic situation.
A computing cross-table was used to search for a link between the clinical diagnosis and results of the RT-PCR or serological tests.
The number of deaths was compared between the years 2018, 2019 and 2020. A Poisson mixed model was used, with the period (COVID or not) added in fixed effect and the establishment in random effect.
At each visit, the proportion of positive rapid serologic test was computed, altogether with the number of new diagnostics of SARS-COV2 infections. The rates were compared according to the results of the initial test with Khi-2 tests or, in case of low numbers, with Fisher’s exact tests.
A 5% significance threshold is considered. Analyses were carried out with R software (version 3.6.1).
Results
Population
In this study, 1145 residents (mean age: 89+/−7.5; 898 (78.7%) female) were included and 1334 professionals: 692 among multilevel geriatric hospitals (mean age: 43.6+/−11.8; 441 (82.4%) female) and 642 among nursing homes (mean age: 43.5+/−12.4; 685 (85.9%) female).
For residents, the sex-ratio (male to female) was 1:3.7 and the mean age was 89.0±7.5 years, ranging from 58 to 106 years. For staff members (considering all institutions), the sex-ratio was 1:5.5 and the mean age was 43.6±12.2 years, ranging from 18 to 73 years.
Infection rate
The overall diagnosis was considered missing for 250 residents who had a negative rapid serological test and did not have an RT-PCR result due to unavailability (Table 1). Among the 895 residents with an overall diagnosis, 203 (22.7 %) were confirmed positive for SARS-CoV-2 infection either by a positive RT-PCR test or a positive rapid serological test. Taken separately, the RT-PCR test, the rapid serological test, and clinical assessment each produced a lower infection rate than the overall diagnosis.
The overall rate of SARS-Cov-2 infection in staff members was 23.8% (222/933); overall diagnosis data were missing for 401 (Table 1). This rate was significantly higher (108/276; 39.1%) among multilevel geriatric hospital staff members than among nursing home staff members (114/657; 17.4%) (OR = 3.06 [2.20; 4.24]; p <0001). The rate of infection among staff members based on either RT-PCR test, the medical diagnosis or the serological test alone was lower than for the overall diagnosis.
Geographical differences were manifest: by institution, infection rates ranged from 2.9% to 71.1% for residents and 0% to 66.7% for caregivers.
Risk factors
Residents
Institutional residents were more likely to be confirmed positive for SARS-CoV-2 than staff members (odd ratio 1.67[1.24; 2.23]; p = 0.001).
Prevalence among residents living in units designated as Alzheimer units was significantly higher than in conventional units (OR=1.85, p=0.048). The prevalence was significantly lower in residents who did not require assistance in activities of daily living (GIR 5–6) (p= 0.0024; GIR 1 or 2 vs GIR 5 or 6, OR= 0.22; GIR 3 or 4 vs GIR 5 or 6, OR= 0.21). Being a contact case was also a risk factor (p<0.0001) (Table 2).
Staff members
For staff members, having been in contact with a COVID-19 case was a highly significant risk factor. The only other statistically significant factor was the occupational category. Exposure was greatest among nurse assistants, nurses and physicians (Table 3).
Clinical presentation in residents
Clinically, residents presented with asthenia and respiratory symptoms, 54 and 50% respectively. Fever was observed in only 31%. Geriatric symptoms were frequent: abdominal symptoms (24.5%), delirium (17.3%), and falls (12%) (Table 4).
Lethality
The number of deaths for the period March to May was significantly higher in 2020 than in 2018 and 2019. The number of deaths increased 1.52-fold (p<0.0001), with 150 deaths in 2018 (data were not available for three institutions), 135 in 2019 and 230 in 2020.
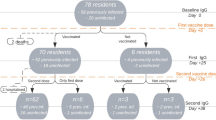
Follow-up visits
Follow-up visits were scheduled for 203 residents, of whom 137 (67.2%) attended the 1-month visit, 90 (44.1%) the 3-month visit and 12 (5.9%) the 6-month visit.
Follow-up visits were scheduled for 222 employees, of whom 147 (66.2%) attended the 1-month visit, 99 (44.6%) the 3-month visit and 28 (12.6%) the 6-month visit.
Due to the concomitant vaccination campaign that had started before the scheduled 6-month visit, few employees attended; thus, the 6-month results are not reported.
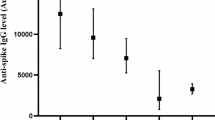
Time course of rapid serologic tests
There was a strong link between the initial rapid serologic test result and the presence of antibodies at each visit. Among residents with an initial positive test, 68% still had a positive test at 1 month, and 74% at 3 months. For employees with an initial positive test, 78% still have a positive test at 1 month and 54% at 3 months (Table 5).
Reinfection
At 1 month, the rate of clinically symptomatic reinfection was low: 1.5% suspected infection in residents (n=2) and 2.1% in employees (n=3); rate of RT-PCR confirmed infection = 2.1% in employees (n=3). At 3 months, the rate of suspected infection in residents was 1% (n=1) and 3.3% in employees (n=3); rate of RT-PCR confirmed infection = 3.1% in employees.
Discussion
The overall prevalence of COVID-19 infection among residents between the two waves of the pandemic in France (May to August 2020) was 22.7% while the seroprevalence was 14% and the RT-PCR prevalence 13%.
In a study determining COVID-19 prevalence by RT-PCR in 24 nursing homes in the Marseille area of France, the prevalence was 13.4% (10), a level similar to the 12.9% RT-PCR prevalence in our study. In our opinion, these data underestimate the global impact of COVID-19 that is better described taking into account both RT-PCR results and serology. We observed that clinical diagnosis of COVID-19 was poorly adapted to an estimation of overall prevalence, mainly because older people present with comorbidities and frequent cognitive impairment, which makes COVID-19 diagnosis quite challenging.
Our different estimations of COVID-19 prevalence among institutional residents are all higher than the 5.7% overall positivity rate among dependant residents of French institutions reported by a national survey (39,638 cases in nursing homes on July 31st 2020 among an estimated 695,060 elderly dependent residents of French nursing care institutions) (11). This may be because most of the UNIVI Group nursing homes are situated in high COVID-19-prevalence zones in France.
Regarding caregivers, the EpiCov study among people working in French healthcare institutions in May 2020 found that 4% were positive for SARS-Cov-2 (ELISA method). The prevalence in our staff members was higher (23.8 %). This may have been because the EpiCov study took into consideration staff less frequently in contact with patients positive for SARS-Cov-2 (laboratory technicians, ambulance personnel, etc). This may also be because we pooled RT-PCR test and rapid serological test results (5). The risk factor of a large number of people living together noted in the EpiCov as a risk factor of COVID-19 was not observed in this study. Statistical power may be an issue here.
Regarding prevalence in both staff members and residents, the NG Biotech rapid serological tests appeared to have sufficient sensitivity for identifying individuals with past SARS-CoV-2 infection. Nevertheless, some rapid serological tests may lack specificity, with a risk of false positivity mainly on the IgM band, which may lead to an overestimation of the seroprevalence (8, 9). Regarding the risk factors for infection, the prevalence in residents living in units designated as Alzheimer units was significantly higher. Moreover, COVID-19 prevalence was significantly lower in residents who did not require assistance in activities of daily living (GIR 5–6). This suggests a higher risk of COVID-19 infection in residents with severe cognitive impairment with behavioral disturbances, probably due to poorer compliance with barrier gestures and greater frequency of medical staff assistance.
It should also be noted that the COVID-19 symptomatology presented by the elderly residents was dominated by asthenia (53.6%) and respiratory symptoms (49.5%) with a non-negligible frequency of digestive symptoms (diarrhea, etc.). Geriatric syndromes (delirium, falls) have been described as a possible clinical presentation in older patients. Geriatric syndromes and fever were found in one-third of cases. Fever was less frequent than in other studies describing clinical characteristics of older patients (3, 4).
Follow-up was in a favor of a satisfactory rate of persistent immunity in three-quarters of the study population, both caregivers at one month and residents at 1 and 3 months according to the rapid serological test that does not take into account T cell-linked immunity.
Concerning reinfection, Firzan et al. (12) described a number of cases at an apparently higher rate than in our study, perhaps related to the fact that reinfection was only suspected in symptomatic caregivers and residents.
Our study has some limitations. The population was not randomly and homogeneously recruited. The use of individual preventive measures by caregivers outside of work was not documented which may have caused bias. The residents tested had survived COVID-19 first wave and were therefore more robust than the usual nursing home population.
There also is a significant number of residents and staff members with missing RT-PCR results, eventually related to the fact that RT-PCR was scarcely available at the beginning of the COVID-19 pandemic. When a missing RT-PCR result was associated with a negative rapid serology result, the overall infection diagnosis was considered missing.
Missing data during follow-up was also noted, but probably occurred because vaccination policy was a priority, inducing many vaccinated residents to drop out of the study. For employees, who adhered less well to follow-up, the results are only statistically significant at 1 month.
Moreover, even though the UNIVI Group has a large number of nursing homes, they are not located in all regions of France, which limits geographical generalization.
Furthermore, limitations related to informing the most cognitively impaired may have created a selection bias. Nevertheless, we were able to include nursing home residents with different levels of autonomy.
Another limitation concerns the difficulty of diagnosing COVID-19 in older residents. In order to limit this bias, we chose to combine the RT-PCR results with the rapid serological test results in order to increase diagnostic sensitivity.
Finally, mortality rate could not be determined. We can nevertheless hypothesize that the higher mortality observed in 2020 was due to the COVID-19 pandemic.
Conclusion
This is the first epidemiological study carried out in residents and caregivers of 27 nursing homes and 3 French multilevel geriatric hospitals between the 2 epidemic waves of the SARS-COV-2 pandemic. The results provide an estimate of COVID-19 prevalence based on different diagnosis methods. The seroprevalence determined by rapid serological tests in institutional residents was 14%, an underestimation compared with the overall prevalence of 22.7%. In staff members, the seroprevalence determined by rapid serological tests was 12.8%, again underestimated compared with the overall 23.8% prevalence.
Geriatric syndromes such as falls and delirium were frequent and should be taken into account as a possible clinical presentation of COVID-19 in order to trigger further investigations. Clinicians should also be aware of such manifestations of COVID-19 in order to institute preventive measures.
For institutional residents, living in an Alzheimer unit was found to be a risk factor for COVID-19. Inversely, independence for activities of daily living was a protective factor. For caregivers, having been in contact with a COVID-19 infected person was the major risk factor.
Immunity seemed to be persistent in three-quarters of caregivers and residents during the 3-month follow-up.
The high prevalence of COVID-19 in geriatric institutions pleads in favor of the French vaccination policy, initially targeting as a priority the most vulnerable and dependent people, followed by staff members in healthcare institutions and nursing homes. More studies on the persistence of immunity and the perspective of COVID-19 mutations will help determine a long-term vaccine booster policy.
References
N. Zhu, D. Zhang, W. Wang, X. Li, B. Yang, J. Song, X. Zhao, B. Huang, W. Shi, R. Lu, P. Niu, F. Zhan, X. Ma, D. Wang, W. Xu, G. Wu, G. F. Gao and W. Tan, A Novel Coronavirus from Patients with Pneumonia in China, 2019, New England Journal of Medicine 2020;382; 727–733.; DOI:https://doi.org/10.1056/NEJMoa2001017
F. Wu, S. Zhao, B. Yu, Y.-M. Chen, W. Wang, Z.-G. Song, Y. Hu, Z.-W. Tao, J.-H. Tian, Y.-Y. Pei, M.-L. Yuan, Y.-L. Zhang, F.-H. Dai, Y. Liu, Q.-M. Wang, J.-J. Zheng, L. Xu, E. C. Holmes, et al., A new coronavirus associated with human respiratory disease in China, Nature 2020;579; 265–269.; DOI:https://doi.org/10.1038/s41586-020-2008-3
S. Niu, S. Tian, J. Lou, X. Kang, L. Zhang, H. Lian and J. Zhang, Clinical characteristics of older patients infected with COVID-19: A descriptive study, Archives of Gerontology and Geriatrics 2020;89; 104058.; DOI:https://doi.org/10.1016/j.archger.2020.104058
L. Wang, W. He, X. Yu, D. Hu, M. Bao, H. Liu, J. Zhou and H. Jiang, Coronavirus disease 2019 in elderly patients: Characteristics and prognostic factors based on 4-week follow-up, Journal of Infection 2020;80; 639–645.; DOI:https://doi.org/10.1016/j.jinf.2020.03.019
Drees, INSERM, EpiCOV: Connaître le statut immunitaire de la population pour guider la décision publique. Press release.; Retrieved October 20, 2021, from https://presse.inserm.fr/epicov-connaitre-le-statut-immunitaire-de-la-population-pour-guider-la-decision-publique/39141/
Patricia Minaya Flores, Andrea Lasserre, Nadia Zeghari-Squalli, Cédric Carbonneil, Michèle Morin-Surroca, and Suzie Dalour, Place des tests sérologiques rapides (TDR, TROD, autotests) dans la stratégie de prise en charge de la maladie COVID-19 (Rapport dévaluation). HAS.
World Health Organization, Laboratory testing for coronavirus disease 2019 (COVID-19) in suspected human cases: interim guidance, 2 March 2020 (Technical documents) (p. 10 p.). World Health Organization.
T. Nicol, C. Lefeuvre, O. Serri, A. Pivert, F. Joubaud, V. Dubée, A. Kouatchet, A. Ducancelle, F. Lunel-Fabiani and H. Le Guillou-Guillemette, Assessment of SARS-CoV-2 serological tests for the diagnosis of COVID-19 through the evaluation of three immunoassays: Two automated immunoassays (Euroimmun and Abbott) and one rapid lateral flow immunoassay (NG Biotech), Journal of Clinical Virology 2020;129; 104511.; DOI:https://doi.org/10.1016/j.jcv.2020.104511
H. Péré, R.-S. Mboumba Bouassa, S. Tonen-Wolyec, I. Podglajen, D. Veyer and L. Bélec, Analytical performances of five SARS-CoV-2 whole-blood finger-stick IgG-IgM combined antibody rapid tests, J Virol Methods 2021;290; 114067.; DOI:https://doi.org/10.1016/j.jviromet.2021.114067
T. D. A. Ly, D. Zanini, V. Laforge, S. Arlotto, S. Gentile, H. Mendizabal, M. Finaud, D. Morel, O. Quenette, P. Malfuson-Clot-Faybesse, A. Midejean, P. Le-Dinh, G. Daher, B. Labarriere, A.-M. Morel-Roux, A. Coquet, P. Augier, P. Parola, et al., Pattern of SARS-CoV-2 infection among dependant elderly residents living in long-term care facilities in Marseille, France, March-June 2020, International Journal of Antimicrobial Agents 2020;56; 106219.; DOI:https://doi.org/10.1016/j.ijantimicag.2020.106219
Tableau de bord COVID-19.; Retrieved February 2, 2021, from https://www.gouvernement.fr/info-coronavirus/carte-et-donnees
F. Nainu, R. S. Abidin, Muh. A. Bahar, A. Frediansyah, T. B. Emran, A. A. Rabaan, K. Dhama and H. Harapan, SARS-CoV-2 reinfection and implications for vaccine development, Human Vaccines & Immunotherapeutics 2020;16; 3061–3073.; DOI:https://doi.org/10.1080/21645515.2020.1830683
Author information
Authors and Affiliations
Contributions
A. de Malherbe participated in the study concept and design acquisition of subjects and data, interpretation of data and preparation of the manuscript; S. Verdun participated in the study concept and design, analysis and interpretation of data, and preparation of the manuscript; V. Brenière participated in the acquisition of subjects and data, interpretation of data and preparation of the manuscript; M. Jourdan participated in the acquisition of subjects and data and preparation of the manuscript; L. Luquel participated in the acquisition of subjects and data and preparation of the manuscript; M. Harboun participated in the study concept and design acquisition of subjects and data, interpretation of data and preparation of the manuscript.
Corresponding author
Additional information
Conflict of interest
The authors have no conflict of interest.
Sponsor’s Role
UNIVI financed the exploitation of the eCRF, the recruitment of two nurses who contributed in collecting data in nursing homes. UNIVI also financed the rapid serological tests.
Impact Statement
We certify that this work is novel. This work identifies the prevalence of COVID 19 among caregivers and residents in French geriatric institutions and the evolution of serological status as well as symptomatic recurrence of Covid-19.
Rights and permissions
About this article
Cite this article
de Malherbe, A., Verdun, S., Brenière, V. et al. COVID-19 Prevalence in UNIVI Group Nursing Homes and Multilevel Geriatric Hospitals: Epidemiological Study of Immunological Status with Rapid Serological Tests for Diagnostic Guidance and Follow Up. J Nutr Health Aging 26, 477–484 (2022). https://doi.org/10.1007/s12603-022-1780-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-022-1780-1