Abstract
Objectives
Interventions to increase fruit and vegetable intake among community-dwelling older people have shown mixed effects. We investigated whether an intervention based on an initial multidimensional health risk assessment and subsequent physician-lead nutrition counselling has favourable effects on dietary intake among community-dwelling older people.
Design
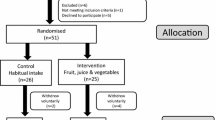
Randomised controlled trial comparing the intervention versus usual care.
Setting and participants
Non-disabled persons aged 65 years or older at an ambulatory geriatric clinic in Bucharest, Romania, allocated to intervention (n=100) and control (n=100) groups.
Intervention
Participants received a computer-generated health profile report based on answers to a health risk assessment questionnaire, followed by monthly individual counselling sessions with a geriatrician on topics related to health promotion and disease prevention, with a special focus on adequate fruit and vegetable consumption.
Measurements
Fruit and vegetable intake at baseline and at 6-month follow-up.
Results
At baseline, fruit and vegetable intake was below the recommended five portions per day in most study participants (85% in the intervention group, and 86% among controls, respectively). At six months, intake increased in the intervention group from a median of 3.8 to 4.6 portions per day, and decreased in the control group due to a seasonal effect from a median of 3.8 to 3.1 portions per day. At six months, fruit and vegetable consumption was significantly higher among persons in the intervention group as compared to controls (median difference 1.4 portions per day, 95% confidence interval 1.1–1.7, p<0.001).
Conclusion
Personalised food-based dietary guidance, delivered as part of multidimensional preventive health counselling during geriatric clinic visits, results in relevant improvement of fruit and vegetable intake in community-dwelling older adults.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
High fruit and vegetable intake is associated with favourable health-related outcomes in older people. It reduces mortality and morbidity related to cardiovascular disease, cancer, diabetes mellitus, and other conditions in adult persons, including in subsamples of older persons (1–4). Many health promotion programs include recommendations for increasing fruit and vegetable intake, or promote diets that include fruit and vegetable intake, such as the Mediterranean or DASH (Dietary Approaches to Stop Hypertension) diet (5–7). Recent research suggests benefits that are even more pronounced for older people given the impact of dietary intake on frailty (8–12), cognitive function (13–15), functional status (16), faecal continence (17), and other age-related health conditions (18–20).
Unfortunately, intake of fruit and vegetables continues to be below recommended levels in older people, and efforts for improvement have shown mixed results and demonstrated that it is challenging to change nutrition behaviour in older people (21–23). Nutrition counselling programs usually result in small effects, or effects may not be persistent because these programs are not integrated into usual care, resulting in organisational or financial barriers for widespread dissemination (24).
A promising approach might be the integration of specific health promotion and disease prevention topics into ambulatory clinical care, thereby giving the physician the opportunity to specifically address and emphasise nutrition counselling as part of usual care. In this approach, nutrition-counselling takes into account possible interactions of nutrition with health, physical activity, medication use or other factors in old age, potentially enhancing counselling effects. Previous studies of such multidimensional programs demonstrated that this is feasible, but it remains unclear to what extent this approach actually results in a relevant improvement in the dietary intake of older people (25–28). We evaluated the effects of a novel intervention based on multidimensional health risk assessment and subsequent physician-lead counselling on fruit and vegetable consumption in older community-dwelling persons. We hypothesised that this model of intensive, individualised intervention in a geriatric care setting might substantially improve fruit and vegetable consumption in people of advanced age.
Methods
Study organisation
This study is part of the RAHEO (Medical Risk Assessment and Health Education in Older People) trial examining the impact of health risk assessment (HRA) and specialised geriatric counselling on physical activity, nutrition, and preventive care uptake in community-dwelling older people. The methods and base-line results of this study have been previously published (29). The field phase of this study took place at the Ambulatory Clinic of the National Institute of Gerontology and Geriatrics “Ana Aslan,” Bucharest, Romania between May 2014 and February 2015.
Selection and randomisation of the participants
Consecutive patients 65 years of age and older, who were referred from general practitioners, were considered for study inclusion. Patients who met any of the following criteria were excluded from study participation: moderate to severe dementia, severe disability (needs help with one or more basic activities of daily living), terminal illness, major surgery within the last three months, not living in catchment area (Bucharest and within 2 to 4 hours travel time), living in nursing home, inability to speak/understand Romanian language, and inability or unwillingness to complete the pre-randomisation questionnaires. Persons who refused to give informed consent were also excluded.
Subsequent allocation to study groups was carried out using a randomisation procedure designed by the independent study centre in Bern, Switzerland using a computer generated 1:1 ratio allocation sequence in a block randomisation process. Participants were allocated to study and control groups in equal numbers using sealed opaque envelopes supplied by the study centre.
Data collection
Prior to randomisation, a trained interviewer conducted face-to-face interviews with participants using a standardised pre-randomisation questionnaire that assessed self-perceived health status, self-reported health measurements, dependency in basic activities of daily living, and chronic conditions. Subsequently, participants were asked to complete a self-administered version of a Health Risk Appraisal (HRA) for Older Persons questionnaire. This questionnaire had originally been developed for use in multiple European countries in English and German languages (30). For the purpose of the present study, a Romanian version of this questionnaire was prepared, using translation, backward translation and cultural adaptation procedures. The HRA for Older Persons questionnaire consists of questions designed to identify potential health and disability risks, as well as lifestyle hazards (30). The questions are grouped into several domains evaluating functionality and mobility, medication use, sensory impairments, presence of pain, psychosocial health and well-being, social network, tobacco and alcohol consumption, level of physical activity, nutritional intake and preventive care.
Fruit and vegetable intake was measured by a six-item food-frequency questionnaire which is part of the self-administered HRA for Older Persons questionnaire (30). This dietary intake questionnaire is based on the validated rapid food screener to assess fat and fruit and vegetable intake based on dietary intake data from the Second U.S. National Health and Nutrition Examination Survey (31, 32). Specifically, the dietary intake questionnaire contains pictograms and text descriptions for defining the size of a portion in each of the six categories: fruit or vegetable juice: 200 ml of unsweetened juice; fruit and berries: one fruit weighing about 120 g or about one handful of berries; salad: one portion weighing about 120 g corresponding to a small plate or bowl; vegetables: about 120 g corresponding to half a cup; vegetable soup: one bowl; and tomato sauce: half a cup.
Consumption frequency in the last week was documented with six response categories: “none in the last week”, “once or twice in the last week”, “three to six times per week”, “once a day”, “twice a day”, or “three or more times a day”. Based on these answer categories, individual items were combined to calculate a composite score indicating the overall number of fruit and vegetable portions consumed per day per study participant.
At six month follow-up, participants were asked to complete the HRA for Older Persons questionnaire again, including the same six questions on fruit and vegetable intake. Participants completed the questionnaires by themselves on site, or with help from a research assistant, if requested. All research assistants were blinded to participants’ treatment allocation status. The completed questionnaires were scanned and sent to the study centre in Bern for double data entry.
Intervention
An individualised computer-generated feed-back report based on the participant’s answers to the baseline HRA for Older Persons questionnaire was provided to the geriatrician counsellor and the patient at the initial counselling session. For fruit and vegetable consumption, the algorithm determined whether the patient adhered to the five portions per day recommendation. If yes, the report encouraged the participant to continue with this healthy nutrition habit. If not, the report stated: “You reported that you eat less than 5 portions of fruit and vegetables a day. Watch out! Something can be done for your health here. Try to get more fruit and vegetables into your diet. Fruit and vegetables provide vitamins and support the gut.”
The initial counselling session with the geriatrician lasted approximately 30 minutes. Health counselling started with recommendations related to physical activity, followed by nutrition counselling, and advice on additional topics, such as preventive care. As part of nutrition counselling, the geriatrician explained changes in nutritional needs with advancing age, and emphasised health benefits of optimal nutrient intake. Participants with satisfactory fruit and vegetable consumption were encouraged to continue to follow their dietary habits. Specific recommendations to encourage balanced, healthy nutrition were provided. Examples of typical local nutrient rich, high-fibre foods were offered, and participant preferences, as well as level of income, were taken into account. Participants were asked about specific conditions that might require a modified diet (e.g., irritable bowel syndrome, constipation, diabetes, hyperuricemia, gastro-oesophageal reflux disease) and current medications that might require avoidance of particular foods (e.g., statins, antibiotics); nutritional recommendations were made accordingly. The geriatrician also made referrals for gastroenterological, diabetes and metabolic workups, or for stomatological assessment, as needed. Participants were actively involved in the process of learning and were encouraged to discuss their diet and the recommendations they received with family members and friends. They were also encouraged to ask questions and to discuss any concerns related to their dietary choices with the health specialist. Participants were advised to plan their meals for several days in advance, and to make shopping lists to facilitate allocation of financial resources and ensure consistency of healthy eating. At the end of the initial counselling session, participants received a written summary report with recommendations, key points of the discussion, and the date and time of the next appointment.
Participants attended monthly follow-up sessions with the geriatrician for six months. Each session lasted between 15 and 30 minutes. Participants were asked about their progress in following the nutritional recommendations and reasons for non-adherence were explored. The geriatrician reinforced the importance of following the nutritional recommendations and modified recommendations based on a participant’s progress. The last counselling session at six months included additional reinforcement to encourage continued adherence with the recommendations. Participants allocated to the intervention group received the intervention, plus usual care from their general practitioners during the entire study period.
Participants allocated to the control group received usual primary care, and did not receive the intervention.
Statistical analysis
The estimated sample size to detect a 20% increase in the proportion of persons adhering to recommended health behaviour was 200, based on an expected drop-out rate of 10%, a two-sided alpha of 0.05, a power of 0.8, and a control group prevalence of adherence to recommended health behaviour of 60% (based on a power analysis for two-sample proportions test). All analyses were conducted according to a detailed analysis plan (29).
For the purpose of this study, the primary outcomes at six-month follow-up were the proportion of persons adhering to the recommended ≥5 portions of fruit and vegetable intake per day, and the amount of fruit and vegetable intake at six-month follow-up. Secondary outcomes were defined as the number of portions reported for each of the six specific fruit and vegetable categories. In addition, we identified the proportion of persons increasing fruit and vegetable intake by comparing response categories between baseline and six-month follow-up for each of the six categories. Group differences were tested by a chi-squared test for binary variables, and by a Kruskal-Wallis test for continuous variables. For binary variables, we report odds ratios (OR) with 95% confidence intervals (CI) from logistic regression models as effect measure. If no effect measure was estimable due to no event outcome, we report a p-value from an exact Fisher test for group comparison. For continuous variables, we report median group differences from quantile regression models (33) with 95% CI. All p-values are two-sided. Possible selection bias was assessed by an inverse probability of censoring weighting approach (34, 35). Statistical analyses were performed in R V.3.1.1 (R Project, University of Vienna, Austria).
Exploratory subgroup analyses were also performed to investigate the effects of the intervention on specific subgroups of the study population. However, because of sample size limitation and the post hoc approach of these subgroup analyses, no measures of effect were attempted and only descriptive results are presented.
Results
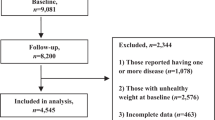
Figure 1 depicts the CONSORT flow diagram indicating the number of persons excluded due to non-eligibility. Overall, 200 persons were included in the study and allocated to intervention (n=100) and control groups (n=100). There were no notable differences in baseline characteristics between the two groups (Table 1). Study participants had a mean age of 75 years, and the majority were highly educated, non-disabled women. At baseline, self-reported fruit and vegetable intake was low in both intervention and control groups, with the vast majority of participants not adhering to the recommended intake of five or more portions per day (85% among persons in the intervention group, and 86% among controls). In both groups, participants reported consuming a median of 3.8 portions of fruits and vegetables per day, consisting mostly of fruits, berries, and vegetable soup. About one third of participants reported that they intended to increase their consumption of fruits and vegetables in the future.
Eighty-eight participants in the control group and 90 participants in the intervention group completed the six-month follow-up (Figure 1). Reasons for non-completion were loss to follow-up with unknown survival status (control group n=7, intervention group n=6), death (control group n=2, intervention group n=1), and withdrawal of informed consent (control group n=3, intervention group n=3).
At six-month follow-up, fruit and vegetable consumption was higher in the intervention group (4.6 portions per day) as compared to the control group (3.1 portions per day) (Table 2). The median difference between the two groups was 1.4 portions per day (p<0.001) and was due to two factors. First, fruit and vegetable intake increased among participants in the intervention group from 3.8 portions per day at baseline (Table 1) to 4.6 portions per day at six-month follow-up (Table 2). Second, fruit and vegetable intake decreased among participants in the control group from 3.8 at baseline (Table 1) to 3.1 portions per day at follow-up (Table 2). This decline is explained by a seasonal effect (baseline data were collected between May and July while six-month follow-up data were collected between November and February).
In parallel, the proportion of participants who adhered to the recommended daily intake of five portions of fruit and vegetables increased among participants in the intervention group (from 15.0% at baseline to 38.9% at follow-up), and decreased among participants in the control group (from 14.0% at baseline to 1.1% at follow-up). Secondary detailed analyses revealed older people in the intervention group increased consumption of fruits, berries, and vegetables (Table 2). The intervention also resulted in a small increase in salad, tomato soup, and fruit juice consumption, but it had no effect on vegetable soup consumption. The sensitivity analyses conducted to assess possible selection bias due to missing six-month follow-up information (inverse probability of censoring weighting) revealed similar results for the primary outcome (median difference of number of portions of fruit/ vegetables per day 1.4 (1.1, 1.7; 95% CI, p<0.001). None of the study participants experienced any harm or other unintended effects related to the study.
Discussion
This innovative intervention of multidimensional HRA combined with geriatrician-lead counselling for physical activity, nutrition and preventive care resulted in a substantial increase in fruit and vegetable intake in a sample of Romanian community-dwelling older people. At baseline, the vast majority (over 80% of study participants) did not adhere to the recommended intake of five portions of fruit and vegetables per day. Following the intervention, participants in the intervention group consumed approximately 1.5 additional portions of fruits and vegetables per day, as compared to control group participants. This increase in fruit and vegetable intake was observed even for participants with low income, low initial intention to improve nutrition behaviour, and poor self-reported health.
The effect observed in our study corresponds to an increased intake of approximately 180 g of fruits and vegetables per day, and is likely clinically relevant. Based on estimates from the National Health and Nutrition Examination surveys an increase of 100 g of fruit and 100 g of vegetables per day reduces mortality risk from stroke by 10%, and 14% respectively (3). In comparison, other intervention models have shown no, or only modest, improvement in fruit and vegetable intake (21–28). It is likely that a combination of factors contributed to these positive findings. First, by having a geriatrician provide nutrition counselling, participants may have viewed the individualised recommendations as health-related prescriptions, and this may have encouraged adherence. Second, counselling was individualised, taking into account each person’s overall health status, coexisting factors, and preferences, and included specific recommendations tailored for the situation of each participant based on the HRA approach. Third, counselling was repeated at monthly intervals, thereby providing an opportunity for the participant and geriatrician to discuss progress with implementation of recommendations, problem-solve barriers, and revise recommendations, if needed. Finally, the intervention was highly structured, including written material that was provided to the participant. We previously demonstrated that this intervention approach is highly successful for increasing physical activity among older persons (29). Our current findings indicate that this approach is also highly effective for improving nutrition intake among older people.
We found strong seasonal variations in nutritional intake over the course of the study. Previous studies have also demonstrated that nutrition intake might vary by season, most likely in regions with relevant differences between summer and winter weather (37–39). In earlier times, fruit and vegetable products were not easily available in the Bucharest area during the winter. Although many products are now available all year round, older persons are apparently still less likely to buy fruit and vegetable products in the winter.
The present study has several limitations. First, generalisability is limited in a single-site study with a study population consisting of patients referred to a geriatric clinic, although this study provides evidence that older persons with different characteristics might benefit from such an intervention. Second, outcome data are based on self-report, and no observational or weekly diary data were collected. We tried to minimise bias by blinding outcome assessors to treatment allocation status of study participants and by using a validated food frequency questionnaire. Third, an overall measure of fruit and vegetable intake has limitations, since it derives one composite score based on six selected fruit and vegetable items with approximate numbers of portions per day. Fourth, our study examines fruit and vegetable intake, and does not address other relevant aspects of nutrition, such as fat or protein intake. Finally, the present study had no follow-up beyond six-months. Consequently, we do not know whether these intervention effects persisted over time.
Conclusion
This study provides evidence that HRA combined with a geriatrician-lead nutrition intervention can improve nutrition intake in older persons. The study also demonstrates the feasibility of implementing a multidimensional health promotion approach with a focus on multiple aspects of health behaviours and preventive care within a geriatric outpatient clinic. Given the limitation of a single-site study using self-reported outcome data, additional research is warranted to confirm our findings. We believe that this nutrition-based intervention is a promising approach for addressing the nutritional needs of older persons and dissemination of this approach could have positive impacts on cardiovascular disease burden, functional status, cognition, frailty, and other health-related outcomes in old age.
Abbreviations
- CI:
-
confidence interval
- IADL:
-
IQR, interquartile range
- HRA:
-
health risk assessment
- OR:
-
odds ratio
References
Hajishafiee M, Saneei P, Benisi-Kohansal S, Esmaillzadeh A. Cereal fibre intake and risk of mortality from all causes, CVD, cancer and inflammatory diseases: a systematic review and meta-analysis of prospective cohort studies. Br J Nutr. 2016;116:343–52. doi:https://doi.org/10.1017/S0007114516001938
Kiefte-de Jong JC, Mathers JC, Franco OH. Nutrition and healthy ageing: the key ingredients. Proc Nutr Soc. 2014;73:249–59. doi: https://doi.org/10.1017/S0029665113003881
Micha R; Peñalvo JL, Cudhea F, Imamura F, Rehm CD, Mozaffarian D. Association between dietary factors and mortality from heart disease, stroke, and type 2 diabetes in the United States. JAMA. 2017;317:912–24. doi:https://doi.org/10.1001/jama.2017.0947
Rivlin RS. Keeping the young-elderly healthy: is it too late to improve our health through nutrition? Am J Clin Nutr. 2007;86(suppl): 1572S–6S. doi: https://doi.org/10.1093/ajcn/86.5.1572S
Badia T, Formiga F, Ferrer A, Sanz H, Hurtos L, Pujol R. Multifactorial assessment and targeted intervention in nutritional status among the older adults: a randomized controlled trial: the Octabaix study. BMC Geriatr. 2015;15:45. doi: https://doi.org/10.1186/s12877-015-0033-0
Hersey JC, Cates SC, Blitstein JL, Kosa KM, Santiago Rivera OJ, Contreras DA, et al. Eat Smart, Live Strong intervention increases fruit and vegetable consumption among low-income older adults. Nutr Gerontol Geriatr. 2015;34:66–80. doi:https://doi.org/10.1080/21551197.2015.1007199
Saneei P, Salehi-Abargouei A, Esmaillzadeh A, Azadbakht L. Influence of Dietary Approaches to Stop Hypertension (DASH) diet on blood pressure: a systematic review and meta-analysis on randomized controlled trials. Nutr Metabol Cardiovasc Dis. 2014;24:1253–61. doi:https://doi.org/10.1016/j.numecd.2014.06.008
Bonnefoy M, Berrut G, Lesourd B, Ferry M, Gilbert T, Guerin O, et al. Frailty and nutrition: searching for evidence. J Nutr Health Aging. 2015;19:250–7. doi:https://doi.org/10.1007/s12603-014-0568-3
Gao J, Jia Y, Dai J, Fu H, Wang Y, Yan H, et al. Association of fruit and vegetable intake and frailty among Chinese elders: a cross-sectional study in three cities. J Nutr Health Aging. 2019;23:890–5. doi:https://doi.org/10.1007/s12603-019-1236-4.
Kobayashi S, Asakura K, Suga H, Sasaki S. Inverse association between dietary habits with high total antioxidant capacity and prevalence of frailty among elderly Japanese women: A multicenter cross-sectional study. J Nutr Health Aging. 2015;18:827–36. doi:https://doi.org/10.1007/s12603-014-0478-4
Kojima G, Avgerinou C, Iliffe S, Jivraj S, Sekiguchi K, Walters K. Fruit and vegetable consumption and frailty: a systematic review. J Nutr Health Aging. 2018;22:1010–7. doi:https://doi.org/10.1007/s12603-018-1069-6
Rahi B, Ajana S, Tabue-Teguo M, Dartigues JF, Peres K, Feart C. High adherence to a Mediterranean diet and lower risk of frailty among French older adults community-dwellers: Results from the Three-City-Bordeaux Study. Clin Nutr. 2018;37:1293–8. doi:https://doi.org/10.1016/j.clnu.2017.05.020
Wu L, Sun D. Adherence to Mediterranean diet and risk of developing cognitive disorders: An updated systematic review and meta-analysis of prospective cohort. Scientific Reports. 2017;7:41317.∣ doi:https://doi.org/10.1038/srep41317
Loughrey DG, Lavecchia S, Brennan S, Lawlor BA, Kelly ME. The impact of the Mediterranean diet on the cognitive functioning of healthy older adults: A systematic review and meta-analysis. Adv Nutr. 2017;8:571–86. doi:https://doi.org/10.3945/an.117.015495
Masana MF, Koyanagi A, Haro JM, Tyrovolas S. n-3 fatty acids, Mediterranean diet and cognitive function in normal aging: a systematic review. Exper Geron. 2017,91:39–50. doi:https://doi.org/10.1016/j.exger.2017.02.008
van Doorn-van Atten MN, Haveman-Nies A, van Bakel MM, Ferry M, Franco M, LCPGM de Groot L, de Vries JHM. Effects of a multi-component nutritional telemonitoring intervention on nutritional status, diet quality, physical functioning and quality of life of community-dwelling older adults. Br J Nutr. 2018;119:1185–94. doi:https://doi.org/10.1017/S0007114518000843
Staller K, Song M, Grodstein F, Whitehead WE, Matthews CA, Kuo B, Chan AT. Increased long-term dietary fiber intake is associated with a decreased risk of fecal incontinence in older women. Gastroenterol. 2018;155:661–7. doi:https://doi.org/10.1053/j.gastro.2018.05.021
Schwingshackl L, Missbach B, Jürgen König J, Hoffmann G. Adherence to a Mediterranean diet and risk of diabetes: a systematic review and meta-analysis. Public Health Nutr. 2015;18:1292–9. doi:https://doi.org/10.1017/S1368980014001542
Haveman-Nies A, de Groot L, Burema J, Cruz JA, Osler M, van Staveren WA, and the SENECA Investigators. Dietary quality and lifestyle factors in relation to 10-year mortality in older Europeans: the SENECA study. Am J Epidemiol. 2002;156:962–68. doi: https://doi.org/10.1093/aje/kwf144
Prince MJ, Wu F, Guo Y, Gutierrez Robledo LM, O’Donnell M, Sullivan R, Yusuf S. The burden of disease in older people and implications for health policy and practice. Lancet. 2015;385:549–62. doi:https://doi.org/10.1016/S0140-6736(14)61347-7.
Jepson RG, Harris FM, Platt S, Tannahill C. The effectiveness of interventions to change six health behaviours: a review of reviews. BMC Public Health. 2010;10:538. doi:https://doi.org/10.1186/1471-2458-10-538
Hazavehei SMM, Afshari M. The role of nutritional interventions in increasing fruit and vegetable intake in the elderlies: a systematic review. Aging Clin Exp Res. 2016;28:583–98. doi:https://doi.org/10.1007/s40520-015-0454-9
Maderuelo-Fernandez JA, Recio-Rodríguez JI, Patino-Alonso MC, Pérez-Arechaederra D, Rodriguez-Sanchez E, Gomez-Marcos MA, García-Ortiz L. Effectiveness of interventions applicable to primary health care settings to promote Mediterranean diet or healthy eating adherence in adults: a systematic review. Prev Med. 2015;76: S39–55. doi:https://doi.org/10.1016/j.ypmed.2014.12.011
Elder JP, Williams SJ, Drew JA, Wright BL, Boulan TE. Longitudinal effects of preventive services on health behaviors among an elderly cohort. Am J Prev Med. 1995;11:354–9.
Pérez LM, Enfedaque-Montes MB, Cesari M, Soto-Bagaria L, Gual N, et al. A community program of integrated care for frail older adults: +AGIL Barcelona. J Nutr Health Aging. 2019;23:710–6. doi:https://doi.org/10.1007/s12603-019-1244-4
Harari D, Iliffe S, Kharicha K, Egger M, Gillmann G, von Renteln-Kruse W et al. Promotion of health in older people: a randomised controlled trial of health risk appraisal in British general practice. Age Ageing. 2008;37:565–71. doi: https://doi.org/10.1093/ageing/afn150
Dapp U, Anders JA, von Renteln-Kruse W, Minder CE, Meier-Baumgartner HP, Swift CG et al. PRO-AGE Study Group. A randomized trial of effects of health risk appraisal combined with group sessions or home visits on preventive behaviors in older adults. J Gerontol A Biol Sci Med Sci. 2011;66:591–8. doi: https://doi.org/10.1093/gerona/glr021
Stuck AE, Moser A, Morf U, Wirz U, Wyser J, Gillmann G et al. Effect of health risk assessment and counselling on health behaviour and survival in older people: a pragmatic randomised trial. PLoS Med. 2015;12:e1001889. doi: https://doi.org/10.1371/journal.pmed.1001889
Herghelegiu AM, Moser A, Prada GI, Born S, Wilhelm M, Stuck AE. Effects of health risk assessment and counselling on physical activity in older people: A pragmatic randomised trial. PLoS ONE. 2017;12(7):e0181371. doi:https://doi.org/10.1371/journal.pone.0181371
Stuck AE, Kharicha K, Dapp U, Anders J, von Renteln-Kruse W, Meier-Baumgartner HP et al. Development, feasibility and performance of a health risk appraisal questionnaire for older persons. BMC Med Res Methodol. 2007;7:1. doi:https://doi.org/10.1186/1471-2288-7-1
Block G, Hartman AM, Dresser CM, Carroll MD, Gannon J, Gardner L. A data-based approach to diet questionnaire design and testing. Am J Epidemiol. 1986;124: 453–69.
Block G, Gillespie C, Rosenbaum EH, Jenson C. A rapid food screener to assess fat and fruit and vegetable intake. Am J Prev Med. 2000;18:284–8. doi: https://doi.org/10.1016/S0749-3797(00)00119-7
Koenker R and Bassett G. Regression Quantiles. Econometrica. 1978;46:33–50.
Robins JM, Hernán MA, Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology. 2000;11:550–560.
Weuve J, Tchetgen Tchetgen EJ, Glymour MM, Beck TL, Aggarwal NT, et al. Accounting for bias due to selective attrition: the example of smoking and cognitive decline. Epidemiol. 2012;23:119–28. doi:https://doi.org/10.1097/EDE.0b013e318230e861
National Institute of Statistics. Press Release No. 225 Sept. 2014. Number of pensioners and medium monthly pension in second trimester 2014. http://www.insse.ro/cms/ro/content/numarul-de-pensionari-si-pensia-medie-lunara
Stelmach-Mardas M, Kleiser C, Uzhova I, Penalvo JL, La Torre G, Palys W, et al. Seasonality of food groups and total energy intake: a systematic review and metaanalysis. Eur J Clin Nutr. 2016;70:700–8. doi:https://doi.org/10.1038/ejcn.2015.224
Fowke JH, Schlundt D, Gong Y, Jin F, Shu XO, Wen W, et al. Impact of season of food frequency questionnaire administration on dietary reporting. Ann Epidemiol. 2004;14:778–85. doi:https://doi.org/10.1016/j.annepidem.2004.02.002
Bernstein S, Zambell K, Amar MJ, Arango C, Kelley RC, Miszewski SG, et al. Dietary intake patterns are consistent across seasons in a cohort of healthy adults in a metropolitan population. J Acad Nutr Diet. 2016;116:38–45. doi:https://doi.org/10.1016/j.jand.2015.08.008
Acknowledgments
We are grateful to all the participants for their valuable contribution to this study. We thank Karen R. Josephson for helpful review and editing of the manuscript.
Funding
Funding: This work was supported by the Forschungsfonds Geriatrie, Bernische Stiftung für die Regionalen Spitalzentren, Bern, Switzerland. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest: The authors have no financial or personal conflicts to disclose.
Ethical Standards: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study received approval from the Ethics Committee of the National Institute of Gerontology and Geriatrics “Ana Aslan,” Bucharest (972/2014). Written informed consent was obtained from all participants.
Additional information
Trial Registration: International Standard Randomized Controlled Trial Number: ISRCTN11166046
Electronic supplementary material
Rights and permissions
Open Access: This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, duplication, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
About this article
Cite this article
Herghelegiu, A.M., Wenzel, K.M., Moser, A. et al. Effects of Health Risk Assessment and Counselling on Fruit and Vegetable Intake in Older People: A Pragmatic Randomised Controlled Trial. J Nutr Health Aging 24, 591–597 (2020). https://doi.org/10.1007/s12603-020-1373-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-020-1373-9