Abstract
This paper examines whether the combined participation in workfare and food grain subsidy programmes in India impacts the nutritional and health status of women and children, using body mass index (BMI) and short-term morbidity as indicators. Based on a nationally representative panel data survey conducted in 2005 and 2012, we estimate the participants’ average treatment effects by applying a semi-parametric differences-in-differences (DID) approach on the full sample and a regression-based DID approach on a matched sample. We find that simultaneous participation in these programmes lowers women’s morbidity by at least 25%, but women’s BMI increases only in states implementing those programmes well. For children, there is no robust evidence of impacts. Our results suggest that various social protection programmes can operate synergistically and deliver positive impacts on children and women’s nutrition or health, even though this is not their main objective. However, the effects are heterogeneous and confirm that the nutrition and health benefits, reached through a combination of the two social protection programmes, are mediated by intrahousehold dynamics. Synergistic and mediating effects must be considered in future efforts to upscale social protection in the Global South in order to deliver simultaneous progress across the Sustainable Development Goals.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Ever since the adoption of the Sustainable Development Goals (SDGs) in 2015, there has been considerable attention devoted to conceptualizing and operationalizing interlinkages between the SDGs, so that social policy can operate in a more holistic or integrated way (UN, 2018). There is increasing recognition that large-scale social protection programmes can decrease risks associated with livelihoods of the poor (Kanbur, 2015) and evidence suggests that they can contribute to putting these synergies into practice, even if specific goals of the programmes are somewhat narrow (BMZ, 2017; Cluver et al., 2016). The role of social protection in resilience, cutting across SDGs (poverty, food and nutrition security, health, employment, gender, and more), has also been highlighted as the COVID-19 pandemic unfolded (ILO, 2020, Pérez-Escamilla et al., 2020).
Social policy in developing countries can have varying goals, target groups and can take different forms, for example, cash transfers (with or without conditionalities), insurance, workfare programmes, food aid and subsidies. While there is a rich body of evidence on whether these schemes effectively target the poor and whether they fulfil their stated objectives, there is comparatively less literature on the synergistic potential of these programmes to promote SDG goals more generally and their ability to impact goals that are not explicit goals of the programme. Many programmes are increasingly redesigned or bundled with other programmes to more explicitly address multiple goals (See Berhane et al., 2020, Shigute et al., 2020; Shigute et al., 2017; Soares et al., 2016; Pace et al., 2017; Jensen et al., 2017) for discussions on Ethiopia’s workfare program, in particular.). There is also a need to understand better whether the convergence of benefits from different programmes to a single household accrues equitably to all household members, especially to women and children (Berhane et al., 2020).
In this paper, we investigate whether large-scale social protection programmes that purportedly focus on alleviating poverty and hunger (SDGs 1 and 2, especially targets 1.1, 1.2, 1.3, and 2.1), can have synergistic impacts on nutrition (SDG 2, target 2.2) and health (SDG3) as well, and in ways that forward gender equality (SDG 5). To that effect, we analyze the nutrition and health impacts of two large-scale social safety nets in India: a workfare program, the Mahatma Gandhi National Rural Employment Guarantee Act (MGNREGA), and the in-kind distribution of subsidized foodgrain, the Public Distribution System (PDS), on selected aspects of nutrition and health: – BMI/Z scores and morbidity for women and children. Specifically, we ask: are these programmes also `nutrition sensitive’ even if nutrion is not an explicit focus of the programmes (Ruel et al., 2013), do they deliver synergistic benefits and, finally, do these household–focussed interventions have the ability to reach vulnerable members within the household, especially women and children?
The MGNREGA is among the largest public works programmes in the world. Rolled out in three phases over the years 2006 to 2008, it guarantees, in principle, each rural household a minimum of 100 days of manual, unskilled work on demand for wages established according to the task undertaken. Unlike the earlier programmes it replaced, namely the Food for Work (FFW) programmeand the Sampoorna Gramin Rozgar Yojana (SGRY), the MGNREGA has a high participation of women, and contains several elements that fosters such participation (see Holmes et al., 2011; Khera & Nayak, 2009; Narayanan & Das, 2014 for example). The PDS is the largest subsidized food grain distribution scheme in the world and has been operational since the 1960s, with some major changes in the 1990s that involved targeting the poor as opposed to universal coverage. The programmeinvolves entitlements of rice and wheat, with pulses, sugar and oil provided additionally in several states, at subsidized rates. In general, eligible households might choose to use the PDS or not and are constrained in part by the administrative quality of the distribution systems. Nationally representative data in India suggest that in 2011–12, around half of all rural households were buying some rice or wheat from the PDS and close to a quarter of all rural households had at least one member who had worked for at least one day on the MGNREGA during the year preceding the date of the survey (Narayanan & Gerber, 2017).
There are two potentially opposing pathways through which the MGNREGA and PDS might influence the nutritional and health status (Narayanan & Gerber, 2017). A household’s participation in the MGNREGA augments incomes through wages earned as long as it does not crowd out private employment; similarly, accessing food grains at subsidized prices from the PDS represents an implicit transfer that frees income that might have otherwise been directed to food grains. The income thus gained or saved could then be used for investments in improving children’s health such as child immunization, institutional delivery of mothers, their antenatal and postnatal care, etc. or to improve the household health and sanitary investments. The works created under the MGNREGA, such as toilets and drinking water sources, enabling cultivation, can also potentially serve to protect nutritional status and health.
On the other hand, to the extent that the MGNREGA attracts women’s work effort, it could crowd out time spent on providing care to their children, which can impact child nutrition in various ways, or on seeking healthcare for themselves or for their children. Further, since the MGNREGA work involves substantial physical effort, if it is not compensated with adequate intake of calories it could leave adults worse off, especially given the well-documented phenomenon of substantial delay in paying wages to the MGNREGA workers (Khera, 2011b) and the fairly low wages offered to programme participants. Similarly, if access to subsidized food grains through PDS crowds out, rather than crowds in, a diverse food basket, this would have negative consequences for some aspects of nutrition and health.Footnote 1 These pathways are further mediated by intrahousehold allocation of resources, given that both the MGNREGA and PDS are entitlements at the household level, even if the MGNREGA wages accrue to the individual worker.
Recent literature documents wide-ranging impacts of these two programmes, notably on consumption expenditure, food intake, wages, etc., but few have focused on nutritional and health impacts (as noted in Bhatia et al., 2016; Sukhtankar, 2016; Narayanan & Gerber, 2017 and Pingali et al., 2017). Those that assess impacts on nutritional status do so for particular subpopulations (such as children) in specific geographies (Gaiha et al., 2010; Jha et al., (2011); Thampi, 2016; Dasgupta, 2017; Krishnamurthy et al., 2017; Kumar & Joshi, 2013; Bagavathinathan & Chaurey, 2020, Uppal, 2009). Using national data, others focus on a single programme and find that the PDS has limited or no impact on Body Mass Index (BMI) (Desai & Vanneman, 2015), or that the effects are apparent in some states but not in others (Thampi, 2016). Sharma (2015) finds that MGNREGA participation reduces children’s morbidity. This paper expands on this literature and is to our knowledge a first attempt at including both MGNREGA and PDS participation, potential synergies between them and the differential impacts on women and children.
We investigate whether women and children in households that utilize both the PDS and MGNREGA fare better in terms of nutritional and health status than if they had not. There is considerable evidence today suggesting that household benefits are not necessarily evenly distributed across household members and that norms and practices governing intra-household allocation could leave women in the household worse off (Brown et al., 2019a, b; Lentz et al, 2019). In the same vein, development literature identifies earnings accruing to women in the household as empowering and note that women often direct earnings from social safety nets to human capital investment (which would reflect in children’s well-being; Maity (2020) for example). This aspect is particularly interesting in the context of the MGNREGA where wages accrue to individuals.
In focussing on nutrition and health outcomes of women and children in participant households, we ignore spillover or general equilibrium impacts on non-participants as well. These could be positive (if for instance, the MGNREGA pushes up wage rates overall) or negative (if for instance, PDS increases food prices overall or promotes food grain, at the cost of dietary diversity). Nor are we able to comment on the direction of impacts for adult men, for whom we do not have comparable data. These remain limitations of the analysis.
The rest of this paper is organized into 4 sections. Following this introduction, in Section 2, we discuss the data, empirical strategy and broadly the methods. Section 3 presents the results. In Section 4, we present a set of robustness checks we implemented. The final Section 5 concludes the discussion.
2 Methods
The paper uses data from the Indian Human Development Survey (IHDS), a rich panel that captures anthropometric and morbidity indicators as well as PDS and MGNREGA participation, to understand the nature of the relationship between these safety nets and the nutrition and health of individuals. The IHDS provides household level PDS consumption, individual level participation in the MGNREGA, as well as nutritional and morbidity status of individuals at two points of time in 2005 and 2012. The first round provides a baseline because it preceded MGNREGA implementation; the PDS was however already in place at that time as were other workfare programmes such as the SGRY. There has been a substantial improvement in extending PDS coverage during the period 2005 and 2012 (Khera, 2011a; Rahman, 2014). We observe this in our sample as well. We attempt to estimate causal impacts of these programmes using semiparametric difference in differences (DID) and DID on matched subsamples to mitigate the selection bias.
2.1 The survey
The IHDS is a nationally representative, multi-topic survey of 41,554 households in 1503 villages and 971 urban neighborhoods across India. The first round of interviews, The India Human Development Survey-I (IHDS-I), was completed in 2004–5. In 2011–12, in the second round, IHDS-II, about 85 percent of the households covered in the 2004–05 round were reinterviewed. IHDS-II covered 42,152 households in 1,503 villages and 971 urban neighborhoods across India.Footnote 2
Both rounds of the IHDS survey capture household access to food grains distributed through the PDS while the 2011–12 round captures participation in the MGNREGA scheme at the individual level. The 2004–05 round captures an individual’s participation in the SGRY and Food-for-work programmes.Footnote 3 Based on this, we classify households as participating in the MGNREGA programme if at least one member of the household has worked in the programme for at least a day in the year preceding the date of the survey. Since it is unlikely that participation for just a few days has any meaningful impact, we also use models that account for the number of days of participation; these are described later in the paper. We define a household as utilizing PDS if it has purchased any quantity of rice, wheat, sugar or other cereals in the past 30 days prior to the date of the survey. As mentioned before, although the PDS was already in place during IHDS-I, its reach expanded considerably by 2012, when IHDS-II was undertaken. For example, the proportion of women who live in a household which utilized the PDS has increased from 36.16% in 2005 to 58.63% in 2012. In the children’s sample, this proportion increased from 27.21% in 2005 to 51.08% in 2012. We identify four categories of households – those that participated in or utilized both the MGNREGA and the PDS in 2012, those that access either programme (but not both) and those that access neither, so that we have four mutually exclusive categories of sample households. In our analysis we combine the latter three into one group, to be able to isolate the synergistic effect of participation in both programmes.
We conceptualize a treated household as one that accesses both programmes. Treatment is defined at the household level because of difficulties in apportioning the PDS entitlements to different members of the household. The comparison group pools households that use either of the two programmes but not both, and those that use neither program, to yield estimates of the combined impacts of PDS and the MGNREGA. Although it is well-established that those who don’t access either programmeare predominantly those that self-select out, we choose to retain them in the comparison group due to possible exclusion, elite capture and mistargeting, that exclude households that observationally resemble participant households. If on the other hand, better off participants select out so that this group is more likely to have better nutritional and health status to start with, any impact we might detect using this comparison group would likely be conservative estimates.
The outcomes of interest are BMI and morbidity for individuals. We use morbidity – number of days of short-term illness in the month preceding the date of the survey as a proxy of health status and the Body Mass Index (BMI) as a proxy for nutritional status, especially macronutrient adequacy and captures the whole spectrum of nutrition from thinness to obesity. Both measures are somewhat coarse indicators but are widely used in survey-based research. In developing countries such as India, there is substantial evidence that low BMI is correlated with low physical work capacity, higher mortality (Satyanarayana et al., 1989), higher morbidities, and a lower income (Deolalikar, 1988). Low BMI in women impacts reproductive outcomes. Women with a low BMI tend to give birth to a greater proportion of low birth weight babies compared with those of normal BMI (Kulkarni, et al., 2006, for example). Short-term morbidity involves subjective assessments of one’s own health. One concern is that this might be measured with error; however, the longitudinal nature of the dataset redresses to some extent the concern about systematic differences across individuals with respect to self-reported morbidity (e.g. using fixed effects in a panel framework).
Further, although there is a large random element to short term illnesses, there is an established positive correlation, i.e. a systematic relationship, between socio-economic status and health as represented by morbidity (Glymour et al., 2014; Phelan et al., 2010). Socio-economic status has been identified as a “fundamental determinant of health”. That said, this study inherits limitations of data availability that pervades literature in this field, including seasonality effects within and across survey rounds. Our estimation therefore controls for the quarter of the calendar year in which the survey was conducted.
For the purpose of this study, we have considered those aged 15 and above as adults and those aged below 15 as children. Since we use two rounds of a longitudinal data that span across seven years, it is possibile that a few individuals who are aged below 15 in the first round are aged above this threshold in the second. To maintan the panel structure, we consider data only for those who are aged below15 years (15 and above) in both the rounds for the children (women) sample. The IHDS surveys collected anthropometric data for children. Using the WHO guidelines, we construct Z-scores for BMI-for-Age (BAZ) for these individuals,Footnote 4 excluding individuals whose BAZ is deemed implausible according to the WHO guidelines and those whose BAZ was missing for one or both the years. This left us with 15,408 observations (7,704 for each year) of children aged below 15 years in both the years. To maintain a consistent sample, we restrict our analysis of the morbidity outcome also to these 15,408 observations for whom the BAZ is also available.
The IHDS also captures the anthropometric data for ‘eligible’ women who are defined as those who were ever married and are in the age group of 15–49 years. Ever-married women who were interviewed in IHDS-I “but were no longer eligible i.e. older than 49 years of age” were interviewed as well.Footnote 5 We focus on women who were interviewed in both rounds, for whom BMI was recorded in both rounds. We dropped 160 women, whose BMI is implausible as per WHO norms. Consequently, the analysis was conducted on 32,964 observations for women (i.e. 16,482 individuals per year). As with the children’s sample, we restrict our analysis of the morbidity outcome to these 16,482 women for whom the BMI is also available.
2.2 Summary statistics
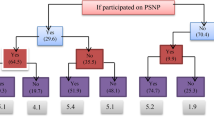
In the children’s sample in 2012, there are 1255 (16.29%) children who belong to households that use both PDS and MGNREGA, 2680 (34.79%) children belong to households use only the PDS, 674 (8.75%) belonging to those households who use only MGNREGA and 3095 (40.17%) children who use neither of these two programmes. In the women’s sample in 2012, there are 2764 individuals (16.77%) who belong to households accessing both PDS and MGNREGA, 6900 (41.86%) belonging to households who use only PDS, 996 (6.04%) belonging to those households who use only MGNREGA and 5822 (35.32%) who use neither of these two programmes. The distribution of household access is therefore broadly comparable across the two groups.
In general, those who use neither programme seem to have better indicators of BMI and less morbidity, especially among women (Table 1). This could be indicative of selection effects, such that those with worse indicators might select into the programmes with others self-selecting out. This is not surprising since the MGNREGA pays minimum wages for manual unskilled work and the PDS provides relatively poorer quality grain – both tend to select in the relatively poor (Liu & Barrett, 2013). To the extent that nutrition and health are correlated with economic status, this offers some suggestive evidence that despite recorded instance of elite capture and patronage in programme allocation, at the aggregate level, both programmes appear to be reasonably well targeted, mitigating the serious threat of possible selection bias on account of unobservable characteristics. To further examine the issue of who utilizes these programmes, we implement multinomial logit models for participation in the two programmes. We use “only PDS” as a base category, with the other three categories being “only MGNREGA”, neither programme and both programmes. These results are available in Annexure (Tables A1 and A2). Our findings confirm the pro-poor nature of both programmes. Relative to only PDS, those participating in neither programme tend to have more sendentary occupations, have an adult who has better education than the base group, belong to upper castes, are wealthier in terms of land holding. In contrast those participating in both programs tend to have less sedentary occupations relative to the “only PDS category”, have members whose highest education is less than for the base group, belong to the marginalized castes and are poorer in terms of land holding. In states that are known to have better implementation capacity (“Star” states, discussed later) households are less likely to belong to the “neither programme” category and more likely to use both programmes relative to the only PDS category. The relative odds of being in households that access only NREGA versus households that access only PDS are higher in ‘Star”; the relative odds reduce with an increase in most educated adult’s education level; the odds are higher for lower caste households; and reduce with household’s per-capita income but increase with land size. These results are similar for both the women’s sample as well as the kids’ sample. As such therefore, we would need to correct for such systematic patterns in selection into participation before we can uncover any synergistic impacts of the programmes.
2.3 Empirical strategy
We employ two different approaches to answer the set of questions at hand. Our preferred approach is a semi-parametric difference-in-differences approach (SDID) proposed by Abadie (2005) to identify Average Treatment Effect on the Treated (ATT). Given that those who use both the MGNREGA and PDS could be systematically different from those who use “neither or one” of the programmes based on observable characteristics, estimates that ignore this are likely to be biased. This approach addresses the imbalance in characteristics between the treated and comparison groups.
The additional advantage that this approach has over a traditional difference-in-differences (DID) approach is that it can address violations of the parallel trends assumption: that in the absence of treatment the outcome variable would have followed the same trend in the treated and untreated groups (Houngbedji, 2015). Accordingly, SDID is given by
where \(\Delta y\) is the change in outcome over the two periods, d is the treatments status, \({X}_{b}\) is the vector of baseline characteristics that drive selection into treatment, \(\pi \left({X}_{b}\right)\) is the propensity to get treated. The estimator is a weighted average of the difference of trend \((\Delta \mathrm{y}\)) across treatment groups. It reweights the trend for untreated participants based on their propensity score \(\frac{\uppi \left({\mathrm{X}}_{\mathrm{b}}\right)}{1-\uppi \left({\mathrm{X}}_{\mathrm{b}}\right)}\) that derives from baseline characteristics. The term (1) is an unbiased estimate of ATT if the following assumptions hold: (i) given the baseline characteristics, the treated and control units that share these characteristics would have the same treatment effects and (ii) the propensity score for the treated is a subset of the support of the propensity score for the untreated. We believe this approach is relevant given the limitation with our data that we cannot explicitly test for parallel trends. Further, in the case of the MGNREGA and PDS, both pro-poor programmes, selection characteristics could also affect the outcome differently for those with different characteristics and hence the SDID approach is more appropriate in this context.
SDID estimates are however sensitive to the type of approximation used for the propensity score and we therefore use both the simple linear probability model and a series logit estimator (Hirano et al., 2003) to estimate propensity scores rather than a simple polynomial series or orders of polynomial approximation. In all the models, we estimate propensity scores using the same set of covariates relating to the individual’s baseline (2004–05) characteristics.
This approach identifies the combined impact of participation in both programmes. However, to isolate the additional impact (or synergy) from participating in both programmes vis-à-vis participation in either program, we implement a Difference-in-Differences on a matched subsample using the propensity score (PSM). We perform the PSM analysis using the 2005 sample and keep only the matched individuals from 2005 and merge them with the panel so that the DID analysis is done only for the matched individuals.Footnote 6 In these models, while exposure to both programmes is the causal variable of interest, we present the version that controls for programme participation in MGNREGA and PDS. This enables us to isolate the synergistic impact, if any, over and above the independent association of the PDS and the MGNREGA with individual nutrition and health.Footnote 7
In these models, we cluster errors at the household level, given that programme participation is at the household level and given that our sample comprises multiple respondents from the same household.
3 Results and discussion
3.1 SDID analysis
For the SDID analysis, we use the following variables from the baseline survey for the estimation of the propensity scores: income per-capita (excluding the income received from SGRY/FFW) and its square, land size, education of the household head (for children sample)/occupation (for women), adult sex ratio, number of married females in the household (proxy for family structure), social group, household’s participation in SGRY in 2005, household’s participation in PDS in 2005; age of household head, years of education (for women), an index for assets for measuring household possessions and housing quality (constructed by the IHDS), nearest town distance (categorical variable).Footnote 8 While the MGNREGA was first implemented in 2007, it subsumed two other predecessors – the Sampoorna Grameen Rozgar Yojana (SGRY) and the Food for Work programme (FFW). We consider households’ participation in these programmes from the IHDS data from 2005 as a predictor for whether they are likely to participate in the MGNREGA and hence influence their propensity to be a treated household in 2011–12.Footnote 9 This is a reliable proxy not only for observable characteristics that drive selection but also of unobservable characteristics such as elite networks and political or social connections that might drive access to workfare.
We recognize that the quality of implementation varies widely across states, influencing participation and likely also the benefits accruing from the program. In states where the MGNREGA was implemented well, it is likely that households residing in these states are more likely to participate, relative to observationally similar households in other states. Following Imbert and Papp’s (2015) classification of states performing well on the implementation of MGNREGA,Footnote 10 we include a variable on whether the individual resides in one of these seven ‘star states’ or in West Bengal, which, the IHDS data show, has also been performing well on the implementation of MGNREGA. Henceforth, these eight states are referred to as “star-states + ”. About 37 percent of the women’s sample and 39 percent of the children’s sample reside in these eight states. Moreover, there are a few states where the access to PDS is universal or near universal and not limited to the poor. Residing in these states could increase the propensity of a household to participate in PDS. Based on Khera (2011a) there are four states where PDS is universal or near universal.Footnote 11 It turns out these states are a subset of the ‘star states’. Hence, by controling for whether the individual resides in one of these ‘star states’, we are inherently accounting for the state-specific effects of residing either in those states with universal/near-universal PDS or in those that implement the MGNREGA well.
We present SDID estimates of Average Treatment Effect among the Treated (ATT) in Table 2, where the propensity score is based on a Linear Probability Model (LPM) and then a Series Logit Estimator (SLE). The number of observations used in the estimation with LPM is smaller than the full sample since observations with propensity score greater than 1 or less than zero are dropped while estimating ATT using the LPM method. On the other hand, the advantage with the Series Logit Estimator (SLE) is that it uses a logistic function to estimate the propensity score and hence all the observations in the sample can be used for the analysis.
For women, participation in the MGNREGA and PDS leads to lower short-term morbidity by 0.26 to 0.28 days, relative to not participating in both programmes. This effect is equal to 25% of the comparison group average during the baseline. There is however no impact on women’s BMI. For children, while there is no evidence for any impact of the participation in the MGNREGA and PDS on children’s morbidity, children from the participating households experience an increase in their BMI-for-Age Z-scores (BAZ) as per both the LPM and SLE estimations, by 0.13 to 0.16 points, although the LPM results are statistically weaker. Considering that the baseline BAZ for children in the comparison group is -0.16, this suggests that children’s BMI deficits are virtually fully erased.Footnote 12 When we run these models for younger and older children separately, we find that in some models, positive effects are evident for BAZ younger children – i.e., those who were under the age of 5 years in 2005. While this is plausible since that is the window where children tend to falter and are able to catch up, we do not find this to be robust across models.
3.1.1 What drives the treatment effects?
The SDID approach allows us to assess whether the treatment effect varies with baseline characteristics associated with the individual (Abadie, 2005). Here, the baseline covariate is used as a modifier in the ATT estimation that operates just like an interaction term with the treatment variable (See Houngbedji, 2015 for details).
We examine this with respect to the following: income per-capita (excluding income from SGRY), whether the individual is resident in either one of the states with well-performing MGNREGA or in states with (near-) universal PDS, distance of the village from the nearest town (categorical variable), whether the individual’s village has health facilities; in addition, for the the analysis of children, we also consider the gender of the child and the distance of the village from the nearest anganwadi (government-run childcare) centre (Table 3).
Women residing in states with well-performing MGNREGA or with (near-) universal PDS have ATT for BMI that is higher by between 0.67 and 0.77 as compared to the ATT on women participants from other states. This represents a 3.77% increase relative to the baseline BMI for women in the comparison group in these well-performing states. There is a legitimate concern that increases in BMI are not necessarily a good thing if those experiencing these increases are already those with high BMI, in the overweight/obesity spectrum. We examine this issue in Section 4.
In addition, there is a small but statistically significant “penalty” on the ATT on BMI for participants from richer households relative to the ATT for relatively poorer households, indicating a pro-poor bias in the effect. To the extent that overweight and obesity in the sample is higher among the richer/non-poor households, the “penalty” here might be desirable, indicating that the impacts of these programmes are more muted for those who are more likely to be overweight or obese.Footnote 13
On the other hand, there is some evidence suggesting that both women and children (Table 3) who are accessing these programmes and are living in villages which are sufficiently farther away from towns (more than 30 kms.) are more vulnerable to short-term morbidity than participants residing in villages that are closer to a town (less than 5 kms.). This is unsurprising since benefits to nutrition and health are predicated on the availability of basic, if not good quality, healthcare.Footnote 14
3.2 DID on matched sample
As an alternative to the SDID, we estimate a traditional regression-based difference-in-difference (DID) model using a sample matched on the propensity scores. We estimate the propensity score using characteristics from the baseline data similar to those we used for the SDID. These include non-SGRY income per-capita and its square, occupation, adult sex ratio, number of married females in the household (proxy for household structure), whether the individual lives in a ‘star state + ’ or a (near-) universal PDS state (as defined earlier). In addition to these, we also use the variables of land size and social group for estimating the propensity score for the children’s sample. Only those individuals that are matched from the PSM analysis are then merged with the panel so that the DID is conducted only on matched individuals.Footnote 15
We estimate the following DID model, where we evaluate the combined total effect of participation in the two programmes (as with the SDID) after isolating the synergistic effect of the two programmes beyond what they individually deliver. We estimate two models, with and without fixed effects (Eqs. (2) and (3) respectively).
where ‘i’, ‘h’, ‘v’ and ‘t’ denote the individual, household, village and time respectively; ROUND refers to the survey round. The variable ‘\({T}_{h}\)’ denotes the treatment dummy of whether the household accessed PDS and MGNREGA in 2012 such that \({T}_{h}\) = 1 for households that accessed both these programmes and \({T}_{h}\) = 0 for other households; X denotes a set of controls, which include the following:
Age, social group (i.e. caste and religion), occupation, individual’s education (for the women’s sample) / household head’s education (for the children’s sample), household size, dependency ratio, age of household head, adult sex ratio, female-headed households, number of married females in the household, non-NREGA/SGRY income per-capita, assets, land size, access to health facilities, access to toilet, piped water, income from other government programmes, access to other food-based welfare schemes like Annapurna, and whether the household belongs to ‘star states + ’. In addition, we have village-level control variables such as village’s distance from surfaced road, nearest town, number of health facilities in the village. Since the outcome variables exhibit strong seasonality, we also control for the quarter of the year in which the interview was administered. In Eq. 2, the independent effects of individual programmes are represented by the inclusion of two binary variables for household participation in PDS and MGNREGA respectively.
Since the treatment is at the level of the household, the standard errors have been clustered at the household level. We estimate both an Ordinary Least Squares (OLS) estimation as well as an individual fixed effects (FE) estimation, using the panel structure of the data.Footnote 16 Table 4 contains the results for women and Table 5 for children; detailed results of this and of the model without individual programmecontrols are available from the authors. With individual specific fixed effects, the DID estimate suggests that participation in both programmes lowers short-term morbidity among women in participant households, similar to the semiparametric DID, but larger in magniture (0.49–0.58 days). We interpret only the coefficient on participation in both programmes as causal, but observe that household participation in MGNREGA is associated with lower BMI among women in participant households (column 2 of Table 4). This is not surprising, given the physical hardship involved in working as part of the MGNREGA and delays in wage payments, as well as intra-household distribution issues. If the physical effort of MGNREGA work is the channel through which BMI is impacted adversely, then that effect should only come about if the woman herself is participating in the programme (as opposed to only other household members’ participation). In order to verify this,, we control for a woman’s own participation in workfare programmes and conduct the matched DID analysis for both the outcomes, BMI and short-term morbidity.Footnote 17 Table 4 shows that the DID coefficient for BMI continues to be insignificant, while the dummy for household participation in MGNREGA is now insignificant, whereas the individual worfare participation dummy is negative and significant. This supports our hypothesis: women who participate in workfare programmes might be worse off for it. This points to the need for wages to compensate work effort adequately, timely payments of these wages and effort-saving implements for work.
For children, participation in both programmes impacts neither the children’s BAZ nor their short-term morbidity consistently across model specifications (see Table 5 below). To the extent that the SDID analysis showed that children’s BAZ is improving from belonging to a treated household at least for some specifications, it is of interest to know if the gender of their household’s adult participant in the treatment matters in impacting children’s health. While it is not possible to assess the intra-household distribution of grains from the PDS, we can look at instances where either only males or only females from the household have participated in MGNREGA and assess the differential impact on children’s health. This addresses an established view that benefits accruing to women are more likely to be channeled to food consumption and health, especially for children (Alderman et al., 1997; Thomas, 1990, for example).
To ascertain this, we analyze subsamples separately, restricting the treatment group to children in households where only women participate in workfare programmes, then to children in households where only the men participate in workfare programmes and then those in households where both men and women participate. Out of 15,086 observations for children that matched, gender-wise household participation in workfare programmes was available for 15,044 observations and we use these for the subsample analysis. For this set of regressions we also control for the intensity of participation, so that we partial out the effect of working more versus less, focusing instead on the channel through which the incomes accrue to the household. Table 5 indicates that only when both men and women work, children in treated households experience an improvement in their BAZ though statistically weak. In contrast when only men work, there is evidence that their morbidity increases. Households with only women participation in workfare do not seem to have either adverse or beneficial impacts. This is perhaps indicative of interesting intra-household effects, spurred for example by gender differences in the way the negative impacts of workfare on the participants’ BMI is compensated for (or not) and transferred to their children (or not). Data limitations prevent us from exploring this further.
4 Further results
As further analysis, we performed all of the above analysis on two subsamples of women to see if the results hold (Table 6). They are: (1) the subsample residing in the eight well-performing states, constituting about 37 percent of the entire sample; the subsample allows us to investigate any heterogeneity across states based on state implementation capacity;and (2) the subsample with their BMI values less than 25 in both the years (the threshold for being classified as overweight), constituting about 77 percent of the entire sample.
For the subsample residing in the eight well-performing states, the results for women show that the impact of treatment on lowering morbidity continues to hold weakly, with a magnitude in the range of 0.29 to 0.48 days, suggesting that women in these ‘star states + ’ do better than those in other states. With respect to the BMI, we find treatment to improve it by around 0.16 points in the LPM specification of SDID analysis but only at 10 percent significance. It is evident that these are the effects of participation in the programmes and not the synergistic impact since the effect dissipates when PDS and MGNREGA participation is controlled for.
For the sample of women with BMI values less than 25, morbidity is lower by about 0.5 days at 5% level of significance as per the matched DID analysis. Moreover, when we consider the covariate-specific ATT for this subsample, we see that the ATT on BMI for those residing in the eight well-performing states is highly significant and is higher by about 0.48 to 0.53 points than the ATT for those outside these states, echoing the results we found for the entire sample. This suggests that those who are undernourished as per the BMI stand to gain from participation. Due to the limited number of observations of women who are overweight or obese we are unable to estimate the impacts for this sub-group.
With respect to the children’s sample, we similarly check for robustness focussing on the sub-sample of those residing in the eight well-performing states, constituting about 39 percent of the entire sample. However, we do not find statistically significant results for any of the models with either of the two outcome variables.Footnote 18
5 Concluding remarks
To summarize our results, we find that consistently across methods the synergistic effect of participation in both the MGNREGA and PDS reduces women’s morbidity by 0.26 to 0.58 days – this constitutes at least 24.5% reduction relative to the baseline average for women in the comparison group. Some specifications suggest that perhaps women who themselves work in the MGNREGA in treated households have worse BMI, likely due to the physically demanding nature of the MGNREGA. For children, we find no consistent impacts, barring weak evidence for BMI-for-age scores (by 0.13 to 0.16 standard deviations) especially in households where both women and men work on the MGNREGA. We find likewise weak indications of worsening of morbidity when only men in the household work on the MGNREGA. We also find suggestive evidence that synergistic benefits accrue disproportionately to those located closer to health facilities.
We started out asking if social protection programmes can effectively take advantage of the interlinkages between the various SDGs and put these synergies into practice. Our paper offers evidence from India that this faith is not misplaced: progammes aimed at reducing poverty and hunger can deliver nutrition and health impacts. At the same time these synergies are currently weak and there might be scope to consider strengthening the nutrition sensitivity of these programmes. The study also highlights that programmes targeting households can have complex and heterogeneous impacts on individuals within the household, suggesting that for social protection programmes to be effective in addressing multiple SDGs, we would need the programmes to be nutrition, gender and generation sensitive.
Notes
In the literature on the PDS, the dominant view is that the PDS represents both a price and income effect. The in-kind transfer represented by the PDS frees up income of the household that would have been directed to essential and price inelastic commodities and therefore is akin to an income transfer. Thus, the price subsidy itself embodies both an income and substitution effect. Thus although the MGNREGA mainly operates via income and the PDS via prices, in reality, we are constrained by our inability to neatly separate out income from price effects.
http://www.ihds.umd.edu/. Accessed October 20, 2016.
Very few households have participated in SGRY/ Food for work. For the women sample this accounts for 0.38% of all observations in 2005 and for the children’s sample, this accounts for 0.52% of all observations in 2005.
We use the STATA igrowup package for calculating the BAZ scores for those aged 0- less than 5 years; and WHO Reference 2007 package for the BAZ scores for those aged 5 or above.
IHDS 2011–12 User Guide, pg. 8.
This is different from a DID model that weights the observations using propensity score. A recent example of the latter approach in the context of India is Unnikrishnan and Imai (2020).
We also implemented models that distinguish households in this pooled comparison group by controlling for those households that participate exclusively in the PDS and MGNREGA. The results are available on request.
The rationale for including income, land size and assets, is to account for the potentially different sources of inequality in rural India, that may not be correlated.. While the correlation coefficient between income and its square is expectedly high at around 0.7, the coefficient for all the other variables are relatively low, less than 0.33 in most cases.
There are only 7 observations in the children sample and 18 observations in the women sample whose households have participated in SGRY and PDS in 2004–05.
These are Andhra Pradesh, Chhattisgarh, Himachal Pradesh, Madhya Pradesh, Rajasthan, Uttarakhand, and Tamil Nadu.
These are Tamil Nadu, Himachal Pradesh, Andhra Pradesh, and Chhattisgarh.
The SDID estimates in Table 2 were obtained using the polynomial order 1. Our results remain when we estimate the ATT with polynomial orders 2, 3, and 4. Results are available on request.
The correlation between BMI and income is positive although small, 0.1624.
We note that morbidity is a self-reported variable in our data, and thus could be higher among more educated households (or located in richer states) due to greater awareness. However, we find no such correlation in our data (using state of residence as a proxy).
About 45 observations from the women sample and 161 observations from the children’s sample were dropped from the baseline data as a result of the PSM exercise. Given that the trimming only drops a few observations we estimate a version without trimming. This alternative approach without the trimming does not change the results much and they are available on request to the authors.
For the OLS estimation, the model we estimate is without the individual-specific fixed effects, \({\alpha }_{i}\).
By ‘workfare’ programmes, we imply participation in SGRY in 2005 / NREGA participation in 2012. Bahal (2021) shows that ignoring SGRY underestimates the impact of NREGA. Only 19 women out of 16,437 in 2005 have participated in SGRY.
The detailed results of these robustness exercises for both the women and children’s analysis are available on request. Similarly, estimations resulting from robustness checks (three scenarios) addressing potential measurement errors in the age of the individuals were performed. Results are similar to those presented here and are available on request.
References
Abadie, A. (2005). Semiparametric difference-in-differences estimators. The Review of Economic Studies, 72(1), 1–19. https://doi.org/10.1111/0034-6527.00321
Alderman, H., Haddad, L., & Hoddinott, J. (1997). Intrahousehold Resource Allocation in Developing Countries. Johns Hopkins University Press.
Bagavathinathan, K. S., & Chaurey, R. (2020). Workfare programmes and children’s meals intake: Evidence from India. Food Policy. https://doi.org/10.1016/j.foodpol.2020.101942
Bahal, G. (2021). A Tale of Two Programmes: Assessing Treatment and Control in NREGA Studies. The World Bank Economic Review. https://doi.org/10.1093/wber/lhab019
Berhane, G., Golan, .J, Hirvonen, K., Hoddinott, J. F., Kim, S. S., Taffesse, A. S., Abay, K., Assefa, T. W., Habte, Y., Abay, M. H., Koru, B., Tadesse, F., Tesfaye, H., Wolle, A., & Yimer, F. (2020). Evaluation of the nutrition-sensitive features of the fourth phase of Ethiopia's Productive Safety Net Programme (Vol. 140). International Food Policy Research Institute, Washington, D.C.
Bhatia, R., Chinoy, S. L., Kaushish, B., Puri, J., Chahar, V. S., & Waddington, H. (2016). Examining the evidence on the effectiveness of India’s rural employment guarantee act, 3ie Working Paper 27. New Delhi: International Initiative for Impact Evaluation (3ie).
BMZ. (2017). Social protection for equitable development. BMZ position paper 09/2017, Federal Ministry for Economic Cooperation and Development (BMZ). Bonn and Berlin, Germany.
Brown, C., Rossella, C., & Jacob, P. (2019a). Sharing the Pie: Undernutrition, Intra-household Allocation, and Poverty. Working Paper, Central European University, School of Public Policy. https://drive.google.com/file/d/1dwiC1ZshZ71IT2A7wAOtmUCZEWT2J7ca/view
Brown, C., Ravallion, M., & van de Walle, D. (2019b). Most of Africa’s nutritionally-deprived women and children are not found in poor households. The Review of Economics and Statistics, 101(4), 631–644. https://doi.org/10.1162/rest_a_00800
Cluver, L. D., Orkin, F. M., Meinck, F., Boyes, M. E., Yakubovich, A. R., & Sherr, L. (2016). Can social protection improve sustainable development goals for adolescent health?. PLoS One, 11(10). https://doi.org/10.1371/journal.pone.0164808
Dasgupta, A. (2017). Can Major Public Works Policy Buffer Negative Shocks in Early Childhood? Evidence from Andhra Pradesh, India. Economic Development and Cultural Change, 65(4), 767–804. https://doi.org/10.1086/691992
Deolalikar, A. (1988). Nutrition and labor productivity in agriculture: Estimates for rural south India. Review of Economics and Statistics., 70, 406–413. https://doi.org/10.2307/1926778
Desai, S., & Vanneman, R. (2015). Enhancing Nutrition Security via India's National Food Security Act: Using an Axe instead of a Scalpel? In India Policy Forum:[papers]. India Policy Forum. Conference (Vol. 11, p. 67). NIH Public Access.
Gaiha, R., Kulkarni. V. S., Pandey, M. K., & Imai, K. S. (2010). National Rural Employment Guarantee Scheme, poverty and prices in rural India. Journal of Asian and African Studies, 45, 645–69. https://doi.org/10.1177/2F0021909610383365
Glymour, M. M., Mauricio, A., & Ichiro, K. (2014). Socioeconomic status and health. Social Epidemiology, 2, 17–63. https://doi.org/10.1093/MED%2F9780195377903.003.0002
Hirano, K., Imbens, G. W., & Ridder, G. (2003). Efficient estimation of average treatment effects using the estimated propensity score. Econometrica, 71(4), 1161–1189.
Holmes, R., Rath, S., & Sadana, N. (2011). An Opportunity for Change? Gender Analysis of the Mahatma Gandhi National Rural Employment Guarantee Act. Project Briefing 53, Overseas Development Institute.
Houngbedji, K. (2015). Abadie’s Semiparametric Difference-in-Difference Estimator. The Stata Journal, 16(2), 482–490. https://doi.org/10.1177/2F1536867X1601600213
ILO (International Labor Organisatuion). (2020). Social protection responses to the COVID-19 pandemic in developing countries: Strengthening resilience by building universal social protection. https://www.ilo.org/wcmsp5/groups/public/---ed_protect/---soc_sec/documents/publication/wcms_744612.pdf
Imbert, C., & Papp, J. (2015). Labor market effects of social programmes: Evidence from india’s employment guarantee. American Economic Journal: Applied Economics, 7(2), 233–263. https://doi.org/10.1257/app.20130401
Jensen, et al. (2017). Cash transfers and index insurance: A comparative impact analysis from Northern Kenya. Journal of Development Economics, 129, 14–28. https://doi.org/10.1016/j.jdeveco.2017.08.002
Jha, R., Bhattacharyya, S., & Gaiha, R. (2011). Social safety nets and nutrient deprivation: An analysis of the National Rural Employment Guarantee Programme and the Public Distribution System in India. Journal of Asian Economics, 22, 189–201. https://doi.org/10.1016/j.asieco.2010.11.004
Kanbur, R. (2015). Mitigating risk: Social protection and the rural poor. In 2014–2015 Global Food Policy Report, International Food Policy Research Institute (IFPRI), Washington.
Khera, R. (2011a). Revival of the public distribution system: Evidence and explanations. Economic and Political Weekly, 46(44 & 45), 36–50.
Khera, R. (ed.). (2011b). Battle for Employment Guarantee, Oxford University Press.
Khera, R., & Nayak, N. (2009). Women Workers and perceptions of the National rural employment Guarantee act. Economic and Political Weekly, 49–57.
Krishnamurthy, P., Pathania, V., & Tandon, S. (2017). Food price subsidies and nutrition: Evidence from state reforms to India’s public distribution system. Economic Development and Cultural Change, 66(1), 55–90. https://doi.org/10.1086/694033
Kulkarni, B., Shatrugna, V., & Balakrishna, N. (2006). Maternal lean body mass may be the major determinant of birth weight: A study from India. European Journal of Clinical Nutrition, 60(11), 1341. https://doi.org/10.1038/sj.ejcn.1602461
Kumar, P., & Joshi, P. K. (2013). Household Consumption Pattern and Nutritional Security among Poor Rural Households: Impact of the MGNREGA. Agricultural Economics Research Review, 26(1), 73–82.
Lentz, E. C., Narayanan, S., & Anuradha, D. (2019). Last and least: Findings on intrahousehold undernutrition from participatory research in South Asia. Social Science and Medicine, 232, 316–323. https://doi.org/10.1016/j.socscimed.2019.05.024
Liu, Y., & Barrett, C. B. (2013). Heterogeneous Pro- Poor Targeting in India’s Mahatma Gandhi National Rural Employment Guarantee Scheme. Economic and Political Weekly, 48(9&10), 46–53.
Maity, B. (2020). Consumption and Time-Use Effects of India's Employment Guarantee and Women's Participation. Economic Development and Cultural Change, 68(4). https://doi.org/10.1086/702789
Narayanan, S., & Gerber, N. (2017). Safety Nets for Food and Nutritional Security in India. Global Food Security, 15, 65–76. https://doi.org/10.1016/j.gfs.2017.05.001
Narayanan, S., & Das, U. (2014). Women participation and rationing in the employment guarantee scheme. Economic and Political Weekly, 49(46), 46–53.
Pace, et al. (2017). One plus one can be greater than two: Evaluating synergies of development programmes in Malawi. The Journal of Development Studies, 54(11), 2023–2060. https://doi.org/10.1080/00220388.2017.1380794
Pérez-Escamilla, R., Cunningham, K., & Moran, V. H. (2020). COVID-19 and maternal and child food and nutrition insecurity: A complex syndemic. Maternal & Child Nutrition, 16(3), e13036.
Phelan, J. C., Bruce G. L., & Parisa, T. (2010). Social conditions as fundamental causes of health inequalities: theory, evidence, and policy implications. Journal of Health and Social Behavior, 51(1_suppl ), S28–S40. https://doi.org/10.1177/0022146510383498
Pingali, P., Mittra, B., & Rahman, A. (2017). The bumpy road from food to nutrition security–Slow evolution of India’s food policy. Global Food Security, 15, 77–84. https://doi.org/10.1016/j.gfs.2017.05.002
Rahman, A. (2014). Revival of rural public distribution system. Economic and Political Weekly, 49(20), 62–68.
Ruel, M., H. Alderman and the Maternal and Child Nutrition Study Group. (2013). Nutrition-sensitive interventions and programmes: How can they help to accelerate progress in improving maternal and child nutrition? The Lancet, 383, 536–551. https://doi.org/10.1016/S0140-6736(13)60843-0
Satyanarayana, K., Venkataramana, Y., & Rao, S. M. (1989). Nutrition and work performance: studies carried out in India. In Proceedings of XIVth International Congress of Nutrition. Seoul, Korea: Korean Nutrition Society (pp. 98–99).
Sharma, A. (2015). Employment Guarantee Scheme and Child Health Outcome: Evidence from MGNREGA Using Propensity Score Matching Analysis. Available at SSRN 2708549.
Shigute, Z., Strupat, C., Burchi, F., Alemu, G., & Bedi, A. S. (2017), The Joint Effects of a Health Insurance and a Public Works Scheme in Rural Ethiopia. IZA Discussion Paper No. 10939. Available at SSRN: https://ssrn.com/abstract=3029810
Shigute, et al. (2020). Linking Social Protection Schemes: The Joint Effects of a Public Works and a Health Insurance Programme in Ethiopia. The Journal of Development Studies, 56(2), 431–448. https://doi.org/10.1080/00220388.2018.1563682
Soares et al. (2016). Combined effects and synergies between agricultural and social protection interventions: What is the evidence so far. Rome: Food and Agriculture Organization. http://www.fao.org/3/a-i6589e.pdf
Sukhtankar, S. (2016). India’s National Rural Employment Guarantee Scheme: What Do We Really Know about the World’s Largest Workfare Program? In India Policy Forum (Vol. 13, pp. 2009–10).
Thampi, A. (2016). The Impact of the Public Distribution System in India. Indian Journal of Human Development, 10(3), 353–365. https://doi.org/10.1177/2F0973703016685792
Thomas, D. (1990). Intra-household resource allocation: An inferential approach. Journal of Human Resources, 25(4), 635–664. https://doi.org/10.2307/145670
United Nations. (2018). Advancing the 2030 Agenda: Interlinkages and Common Themes at the HLPF 2018 A UN-DESA Report of the Meeting,of experts in preparation fo the HLPF 2018: Transformation towards sustainable United Nations Headquarters, New York, 25–26 January 2018.
Uppal, V. (2009). Is the NREGS a Safety Net for Children: Studying the access to the National Rural Employment Guarantee Scheme for the Young Lives families and its impact on child outcomes in Andhra Pradesh. MSc Thesis- Young Lives student paper, University of Oxford. Available at: http://knowledge.nrega.net/859/1/Is_the_NREGS_a_Safety_Net_for_Children.pdf
Unnikrishnan, V., & Imai, K. S. (2020). Does the old-age pension scheme improve household welfare? Evidence from India. World Development, 134. https://doi.org/10.1016/j.worlddev.2020.105017
Acknowledgements
We thank the editor and two anonymous referees of this journal for their valuable inputs that helped improve the paper. We thank without implicating S. Mahendra Dev and participants at seminars in Bonn, Mumbai and Montreal for comments and suggestions. We also thank Priya Rampal and Sanchita Roychowdhury for valuable research assistance.
Funding
Open Access funding enabled and organized by Projekt DEAL. The research leading to this paper has received funding from the European Union's Seventh Framework Programmes FP7/2007-2011 under Grant Agreement n° 290693 FOODSECURE. Neither the FOODSECURE project, its partner organizations, nor any organization of the European Union or European Commission are accountable for the content of papers in this series.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Narayanan, S., Naraparaju, K. & Gerber, N. An assessment of India's multiple national social protection schemes in improving nutrition and health. Food Sec. 15, 1215–1229 (2023). https://doi.org/10.1007/s12571-023-01376-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12571-023-01376-2