Abstract
Considering food insecurity is a problem, even in developed countries, and the evidence gap regarding this issue in Italy, we aimed to assess the prevalence of food insecurity in a sample of Italian children and examine socio-economic and health correlates. This cross-sectional study was conducted in paediatric practices. Parents answered to the 18-items of the Household Food Security Module, 8 of which concern children. Paediatricians answered a questionnaire on children’s health. Socio-economic and health correlates of food insecurity in children were assessed using univariable and multivariable logistic regression. Among 573 households with children, 15·4% were food insecure, while 9·1% of children were food insecure. Socio-economic factors associated to food insecurity were living in south Italy, households with three or more children, lower household yearly income, worse economic situation description and younger parents. Food insecure children were less likely to have a normal relational [ aOR 0.31 (CI 0.11-0.85)] and physical development [aOR 0.32(CI 0.15-0.65) and had more school difficulties [aOR 3.1(CI 1.33-7.24)] compared to their food secure peers. Food insecure children had higher odds of a deterioration in their health since birth and of a worse perceived health status, as reported by their parents. Considering the results in this sample and the lack of research regarding this issues in Italy and Europe more broadly, we call for consistent, national monitoring to determine the magnitude of the problem of food insecurity in households with children in Italy and to examine the socio-economic variables and health implications in different contexts.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Food insecurity (FI) is an increasing public health issue even in developed countries. The sharp 2008–2009 global economic downturn had a great impact on that (Gundersen 2013; Loopstra et al. 2015) and since then there has been an uneven pace of recovery in many countries, while the global economic outlook is darkening again (FAO et al. 2019). According to Food and Agriculture Organization (FAO), FI is on the rise since 2014, with 2 billion people who do not have regular access to safe, nutritious and sufficient food, including 8 percent of the population in Northern America and Europe, in 2018. (FAO et al. 2019). That is more worrying in children, who, if affected, may be in danger for present and future adverse health effects, since their developing brains and bodies can suffer long-term negative consequences (Whitsett et al. 2019; Rocha et al. 2016).
FI-as assessed by United States Department of Agriculture (USDA) through the Household Food Security Survey Module (HFSSM)—is an economic and social condition, at an individual and household-level, of limited or uncertain access to adequate food due to income limitations (Coleman-Jensen et al. 2019). Household Food Insecurity (HFI) has been defined as lack of access by all people of the household, at all times to enough food for an active, healthy life (Bickel et al. 2000). The food security (FS) status of each household is determined by the responses to the 18 food security questions of the HFSSM, 8 of which concern households with children (United States Department of Agriculture 2012). Children Food Insecurity (CFI) is studied through dedicated questions, since FI is believed to affect all household members, although not necessarily in the same way, especially with reference to children (Fram et al. 2012).
As reported by a systematic review concerning high-income European countries, socio-economic correlates of food insecurity in children include low income, households with single parents, with a higher number of children, household’s structure, parents’ occupation and education level, household head’s age, depressive symptoms in parents and ethnicity (Zaçe et al. 2020). However, it is important to highlight that these correlates of FI are context-specific, being linked to country-level policies (i.e., social protection programs), demographics, and macroeconomic conditions that differ even between (and within) European/ high-income countries. For example, Loopstra et al. found that during the Great Recession in Europe, in countries where there were low levels of per capita investment in social protection spending, increasing unemployment and declining wages were associated with rising food insecurity, whereas this was not the case where social protection spending was high (Loopstra et al., 2016). FI is associated to income, wealth, gender and geographic inequalities, as well as accessing basic services and assets, which increase the likelihood of severe FI, taking it to three times higher in countries with high rather than those with low inequalities (FAO et al. 2019).
Significant context-specific differences exist, also, concerning the impact of FI on children’s nutrition, health and well-being. FI may have negative effects through pathways such as compromised dietary intake, being a strong stressor, and indirectly through affecting their parents first (Coleman-Jensen et al. 2017; Huang et al. 2010). Although, FI has been associated with worse diet quality, reduced fruits and vegetables intake, increased consumption of carbohydrates and fats and micronutrient deficiency (Janice and Ford-Jones 2015), it is a different marker of nutritional vulnerability in different countries (Kirkpatrick et al. 2015). A systematic review including international samples from North America, Europe and Asia has reported that FI children have higher probability for presence of cardio-metabolic risk factors (Rocha et al. 2016) as well as chronic conditions, particularly asthma, depression and suicidal ideation (FAO et al. 2019). In addition, a study in USA has associated FI to higher odds of experiencing dental caries (Angelopoulou et al. 2019). Other studies have reported a correlation between FI and anemia, hypercholesteremia and hypertension (Bahadur et al. 2018; South et al. 2019). As for the relationship between FI and children’s BMI, while has been found a positive association between FI and obesity (Kral et al. 2017), in other studies it is concluded that this correlation does not exist (Trapp et al. 2015). Finally, Jyoti et al. suggest that children living in food insecure households have more emotional and behavioral problems and school difficulties (Jyoti et al. 2005).
USA (Gundersen 2013; Coleman-Jensen et al. 2017), Canada (Tarasuk et al. 2019) and United Kingdom (Loopstra et al. 2015) have reported rising of children living in FI, even in developed countries. But, despite FI rising and its burden on children’s health, there is a lack of evidence in many European countries, including Italy, regarding this issue (Zaçe et al. 2020), unlike USA and Canada where food security is routinely monitored. This gap in knowledge might be a missed opportunity for prevention in many European countries, as negative outcomes of FI are totally modifiable by assuring a situation of FS. To achieve this, there have been reported different interventions like social welfare policies, educational programs, food banks and community food programs. But, while there is a lack of evidence showing that the latter effectively reduce FI, social protection programs have proven to be successful, highlighting the crucial role of governmental investment in social protection, especially concerning children (Loopstra 2018).
The urge to have these data on FI emerges, also, by the socio-economic situation that many European countries, including Italy are going through. Socio-economic inequalities have increased, bringing to more unemployment and poverty, as well as less access to education and healthcare, all of which are correlated to FI. (Tarasuk et al. 2019; Miller et al. 2014).
In Italy, as reported by Istituto Nazionale di Statistica (ISTAT), there is an increase in absolute and relative poverty rates, with 12·1% of Italian children living in conditions of absolute poverty in 2017 (Istituto di Statistica 2018). Children in Italy live in a situation of high inequalities, which develop already in the first years of life (Ferro et al. 2007; Bonati and Campi 2005). Socio-economic inequalities are also a consequence of the fact that social spending for children is among the lowest in Europe, with important differences between the various regions in access to services for children and their families. Economic poverty is associated with educational and cultural poverty, access to sports and housing practices, factors that fall within the so-called “health determinants” (Save the Children 2019).
In this context, we conducted a study aiming to: (1) estimate the prevalence of household food insecurity (HFI) and child food insecurity (CFI) in a sample of Italian children; (2) examine the socio-economic factors associated to FI and (3) explore the association between HFI and CFI and children’s health correlates.
2 Methods
2.1 Study design and setting
This cross-sectional study was conducted from January 2017 to December 2018 in six Italian regions representative of all Italian geographical macro-areas; Lombardia (Milan), Lazio (Rome), Marche (Jesi), Campania (Caserta), Puglia (Brindisi, Lecce), Sicily (Palermo). Data collection was conducted in the offices of the paediatricians who adhered to the study.
2.2 Study sample and data collection
Only public practice paediatricians were enrolled in the study. Private paediatricians were not approached, so all the children participating in the study would have the same access to healthcare. Aiming to have a good national representativeness of paediatric practices throughout the Italian macro-areas, we randomly contacted 79 paediatricians via mail and 22 answered positively. The reasons for not participating were: (1) participating in other researches; (2) assisted population largely unmatching inclusion criteria; (3) not having time for the survey. Some paediatricians did not answer at all to our request for collaboration.
Subsequently, we asked all enrolled paediatricians to invite all children and their parents, who would present for a visit at the paediatrician’s office during the study period,to participate to the study. Children’s inclusion criteria were: (1) age 1–11 years old (2) born in Italy; (3) parents of Italian nationality;(4) regularly followed by a paediatrician. Children’s age range was selected for two reasons: (1) we wanted to take a snapshot of FI among children born after the last economic crisis in Italy (2007); (2) older children (adolescents) in the USA experience FI differently from younger ones (Coleman-Jensen et al. 2017). If more than one child from the same household would present for a visit, matching all the inclusion criteria, the paediatrician randomly chose one of them to participate in the study. We excluded children (1) whose mothers hadn’t lived in Italy five years before pregnancy; (2) with congenital malformations or genetic diseases; (3) with chronic neurological, behavioural or emotional diseases (4) undergoing adoption. This was justified by the specific nutritional, social or psychological needs they might have. Migrants were excluded since they may be more vulnerable, experiencing a series of FI determinants, like lower education level, lower income, unemployment, renting a house, social barriers (Perreira and Ornelas 2011).
Parents, once answered, returned the questionnaire in a closed envelope. Paediatrician filled the dedicated questionnaire for every child participating in the study, matching it with the parent’s questionnaire. Matched parent-paediatrician questionnaires were a requirement for inclusion in the final analysis.
2.3 Sample size
To calculate the needed sample, we considered a type 1 error of 5%, an absolute error (precision) of 2·5% and an expected prevalence of FI among households with children of 9·4% (primary outcome) (Coleman-Jensen et al. 2015). The obtained number was then corrected taking into consideration an expected response rate of 60%, establishing the need to recruit 872 children, to achieve a final sample of 523 children.
2.4 Questionnaires
A pilot study was conducted among 15 parent-paediatrician dyads at a paediatrician practice in Rome, assessing the reliability, validity and ease of understanding of the two questionnaires. The study used two questionnaires: paper-based for the parent and either paper-based or online for the paediatrician, both self-administered. Parents’ questionnaire was composed of 4 sections: socio-demographic information, economic information, child’s health, HFSSM. Paediatrician’s questionnaire was composed of 5 sections: child’s demographic and anthropometric information, physical health, psychomotor and relational health, dental health, other outcomes (school difficulties, physical activities). Paediatricians filled the questionnaire based on child’s last visit, but also on her/his records. Questionnaires are available on request.
2.5 Measures
2.5.1 HFI and CFI
HFSSM, reported by parents, was used to measure FI. It is a validated tool, composed by 18 questions, 8 of which specifically concern CFI and the rest HFI in the past 12 months. Because literature reports that adults tend to shield children from FI, it is probable that studies on children (especially younger ones) measuring only HFI may likely overestimate the prevalence of CFI, which has an even greater impact on children’s health, compared to HFI (Fram et al. 2012; Hanson and Connor 2014). Hence, we decided to report separately children experiencing HFI and CFI.
Households are classified as food secure if they report no food insecure conditions or only one or two food-insecure conditions. (Food-insecure conditions are indicated by responses of “often” or “sometimes” to questions 1–2 and 11–13; “almost every month” or “some months but not every month” to questions 5, 10, and 17; and “yes” to the other questions) (questions presented in supplementary Table 1). They are classified as food insecure if they report three or more food-insecure conditions. Households are classified as having food-insecure children if they report two or more food-insecure conditions among the children in response to questions 11–18 (Bickel et al. 2000; Coleman-Jensen et al. 2019).
Parents answered to the 8 children-related questions specifically for the child who was present for a visit at the paediatrician’s office.
2.5.2 Socio-economic factors
The collected variables included (1) household’s characteristics: region of residence, family structure, number of children in the household, household overall income in the last year, economic deterioration in the last 10 years, economic situation description; (2) parent’s characteristics: age at the moment the referred child was born, education, employment; (3) child’s characteristics: sex, age. Yearly income was collapsed and represented in two categories: <€20,000 and >€20,000 based on ISTAT data reporting that the poverty cut off for a family of two parents and two children is approximately €20,000/year (Istituto di Statistica 2018).
2.5.3 Children’s health correlates
Parents were asked: In the last year: (1) How many times did your child get sick?; (2) Did your child need a hospital admission?; (3) How would you describe your child’s health?. 4) Has your child’s health deteriorate since birth?
Paediatricians reported information on child’s physical examination, sight, hearing, psychomotor and relational development, dental health and interventions, blood pressure, school difficulties and physical activity. They also gave information on anthropometric measures (weight, weight by age percentile, height, height by age percentile, BMI).
2.6 Ethical considerations
Parents were handled two specific consent declarations for signature: the informed consent and data treatment. The study was approved by the Ethics Committee of Fondazione Policlinico Universitario “A. Gemelli”, on December 15th, 2016.
2.7 Statistical Analysis
Participants’ characteristics were summarized using frequencies and percentages (N, %) for categorical variables and means and standard deviations (M, SD) for continuous variables. All variables were described by household food security (HFS) (FS vs. FI households) and by child food security (CFS) (FS vs. FI children). Prevalence of HFS and CFS, with Confidence Intervals (CI), was reported for the categories FS, low FS and very low FS and for the two categories FS vs. FI. We performed univariable and multivariable logistic regression to assess the associations between both HFI and CFI, and the socio-economic correlates. We tested all univariable associations between socio-economic correlates and HFI and CFI, and included all variables that were statistically significant in the subsequent multivariable model. Based on the univariable models, the multivariable model included the following variables: region of residence, family structure, parent’s age, education and employment, number of children in the household, yearly household’s income, any economic deterioration in the last 10 years, economic situation description.
Univariable and multivariable logistic regression were also performed to test the associations between HFI and CFI and children’s health correlates. The multivariable model controlled for the variables that resulted significant in the final model assessing socio-economic correlates of food insecurity, and, as well as for child’s age and sex.
The strength of associations was estimated by adjusted odds ratios (aOR) with 95% confidence intervals (CI). All analyses were performed using STATA 15 and a p < 0·05 was considered statistically significant.
3 Results
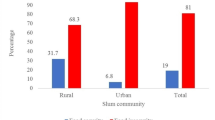
3.1 Prevalence of HFI and CFI
Out of 738 parents invited to participate in the study, 573 parent-pediatrician dyads were included in the analysis, counting for a response rate of 77·6%. Analysis revealed a 14·5% (CI 11.7–17.6) prevalence of HFI and 9·1% (CI 6.8–11.7) of CFI. The number of affirmative answers to the 18 and the 8 children-related questions of the HFSSM ranged from 0 to 13 and from 0 to 7, respectively (Table 1). Table 2 presents the characteristics of the study population, in relation to HFI and CFI status.
3.2 Socio-economic correlates of FI
As it is seen in Table 2, all households’ and parents’ characteristics that we included as variables resulted being significantly associated to HFI and CFI. However, after the multivariable logistic regression analysis only some of the variables remained significant (Table 2). This analysis showed that children living in households from the south of Italy, with three or more children, with less than €20,000/year incomes, that had felt an economic deterioration during the last 10 years and could not save any money monthly, had higher odds of experiencing HFI and CFI. Children with parents that belonged to the age category 30–49 years old had lower odds of experiencing HFI and CFI. Family structure, as well as parent’s characteristics such as employment and level of education lost the significant association after the multivariable logistic regression. Children’s age and sex were not significantly associated to HFI or CFI.
3.3 Health correlates of FI among children
Children living in FI households had higher odds of getting sick more often [(aOR) 3.75(CI 1.31–10.56)] and having worse perceived health [aOR 5.7 (CI 2.01–16.40)], as reported by parents, compared to their peers living in FS households, but there was not a significant association with hospitalization and health deterioration since birth (Table 3). Children who were FI had worse perceived health [aOR 11.1(CI 3.29–37.6) and a deterioration in health since birth [aOR 3.34(CI 1.14–9.77)] compared to children who were FS.
Based on pediatricians’ reports, children experiencing HFI were significantly less likely to have normal relational development [aOR 0.29(CI 0.11–0.77)], and more likely to have school difficulties [aOR 2.34(CI 1.34–6.02) and a weight-by-age percentile > 97 [aOR 3.46(CI 1.70–7.08)]. Children living in food insecure households were less likely to receive interventions to address dental issues [aOR 0.17(CI 0.05–0.54)] and to perform physical activity [aOR 0.51(CI 0.28–0.89)] as well as less likely to have a normal physical examination compared to FI children [aOR 0.32(CI 0.15–0.65)]. Likewise, CFI resulted being significantly associated to all the above health correlates, except physical activity (Table 3). On the contrary, there was not a significant association between the presence of caries or malocclusion as well as sight, hearing and psychomotor impairments and HFI or CFI.
A weight by age percentile higher than 97 was three times more frequently seen among children experiencing HFI and CFI compared to their food secure peers. Children experiencing HFI and CFI had a significant higher BMI compared to their FS peers (18.1 vs.16.8, p < 0.001).
4 Discussion
The present study aimed at estimating the prevalence and explore the predictors and health correlates of FI in a sample of Italian children aged 1–11 years old. Results show that 14·5% of children experience HFI and 9·1% experience CFI. These numbers are worrying, considering that the study was not conducted in necessarily low-income households or neighborhoods. As it is seen, there is a difference between children who live in food insecure households and those who are actually food insecure, which confirms results from other studies that adults try to shield children – especially younger ones – from experiencing FI (Pereira et al. 2017; Fram et al. 2012). This prevalence is higher than that of UNICEF report, which, based on data collected in 2015–2016, showed how almost 10·0% of Italian children lived in food insecure households (Pereira et al. 2017). Unlike Europe, where not many countries have conducted research to assess the situation of FI among children (Zaçe et al. 2020), in Canada and USA there are yearly nationwide Government measurements of FI. In USA, according to USDA, 15·7% of households with children were food insecure and 7·7% of children were food insecure in 2017 (Coleman-Jensen et al. 2017).
Our multivariable logistic regression analysis showed that region of residence, number of children in the household, household’s yearly income, economic situation description and presence of economic deterioration in the last 10 years were significantly associated to both HFI and CFI, which is in line with other studies (Tarasuk et al. 2019; Miller et al. 2014). Among the strongest variables associated with HFI and CFI there were the economic ones (household’s overall yearly income, economic deterioration during the last 10 years and the inability to save money monthly) as well as, having three or more children in a household (2·38 times higher odds compared to having 1 or 2 children).
Among parents’ characteristics, age resulted being associated to both, HFI and CFI. A study in Portugal has also reported that households with younger parents experience more often FI (Maia et al. 2019).
Employment status and education level lost significance in the regression analysis, which does not correspond to the studies published so far, that affirm employment and education are important determinants of FI (Martin-Fernandez et al. 2013; Petralias et al. 2016 ). Probably our result is explained by the fact that we only asked for the employment status and education level of the parent answering the questionnaire and not that of the partner. Also, sometimes, the origin family (parents, siblings) plays an important role in sustaining economically young families in Italy, which could shield them from FI even in the case of unemployment.
As for children’s characteristics, nor age, neither gender resulted being associated to FI, even if there are some studies that report differences in FI based on gender and age (Molcho et al. 2007, Niclasen et al. 2013). Probably this lack of association with age is explained by the fact that the higher differences are seen between children of a very young age and teenagers (who were not our target population) (Petralias et al. 2016).
Children in our sample living in a condition of food insecurity got sick more frequently and had a worse health status, as reported by parents, than their food secure peers. These results are in line with other publications (Ashbrook et al. 2017), but unlike them, we did not find a significant association between children’s hospitalization and FI. The presence of an abnormal physical examination was twice more frequent among children in HFI and almost three times more frequent in children in CFI. The presence of a relational impairment was associated to HFI and CFI. Results from other studies report a delay in every aspect of development among these children (Ashbrook et al. 2017).
There was not a significant association with dental malocclusion or caries. However, we found that among those who had dental problems, the frequency of those who did not have any intervention to correct the condition was higher among children experiencing HFI and CFI. This could mean that these children may have less access to healthcare facilities and interventions. Future research should explore this possible association.
High blood pressure has been associated to FI in a sample of children and adolescents in the USA (South et al. 2019) but the fact that only four children in our sample resulted having this condition didn’t allow us to better explore the possible association and to include this variable in the model.
We saw that a weight by age percentile > 97 (indicative of obesity) was more frequent among children experiencing HFI and CFI. Also, these children had a significantly higher mean BMI compared to their food secure peers. Some studies have, also, found a positive association between BMI and FI (Kral et al. 2017), even if others have failed to do so (Trapp et al. 2015).
It is worth highlighting that all the aforementioned negative health correlates were more frequently noticed among children experiencing CFI (a more severe situation of FI) compared to HFI. This means that children experiencing a more severe condition of FI are more frequently faced with the negative health outcomes of it.
The lack of physical activity was twice more frequent among children experiencing HFI and CFI compared to their food secure peers, as highlighted, also by other studies (Fram et al. 2015) Also, school difficulties were almost three times more frequent among children experiencing HFI. A study in Canada affirms that children who come from food insecure households have lower odds of meeting reading or mathematics expectations and have poor academic achievements (Fought et al. 2017).
In conclusion, in our sample food insecurity was an issue and was significantly associated to different negative health outcomes. Knowing the prevalence of FI and the groups at risk for experiencing it is important, in order to proactively identify those who are more likely to be food insecure and reach out to them with interventions such as education, services, and connections to internal and external resources. Based on our results these interventions should pay special attention to children who live in households coming from the south, with three or more children in them, with lower income, that have felt an economic deterioration during the last years and cannot save any money monthly. Also, special attention must be paid to households with younger parents. In the light of these results and the lack of research regarding this issue in Italy and Europe, we believe this study may act as a foundation for future longitudinal research that investigate FI and its impact on children’s health and behavior and that advocate for higher food security. If our results were to be confirmed by longitudinal future studies with more representative and larger sample sizes, this would be a strong call for increasing governmental efforts in Italy and other high- income countries to expand investment in social protection, which could likely tackle FI and may have long-term benefits by improving health and reducing healthcare and other spending resulting from the harms of food insecurity.
4.1 Strengths and limitations
The current study has several strengths. To the best of our knowledge, it is the first to explore prevalence, associated factors, and outcomes of FI among Italian children. It is novel insofar as little is known about the experience of household food insecurity in Italy. The sample size was calculated for the study to have the appropriate statistical power. A widely used, validated scale to assess FI was used and the information on children’s health and other outcomes were reported by paediatricians, based on their records, to increase the accuracy and reliability of data and reduce the risk of reporting bias. FI was measured at the household and individual level, hence, along with data of children experiencing HFI, we also reported the exact prevalence of children experiencing CFI. There is a lack of evidence regarding this issue in Europe so this study would contribute to start filling this gap and could act as an impetus for future research in other countries.
Nevertheless, the results of this study need to be interpreted in the light of some limitations. The sample does not include all Italian households, but only those with children aged 1–11 years old. The cross-sectional design of the study allowed us only to examine associations, not assessing causality or the long-term health implications of FI, which may not appear until after multiple years of exposure. We did not ask about school meals among children, hence could not explore the potential role of the school canteen as a strategy to reduce FI.
Also, some studies have reported that parents may be ashamed of their inability to feed their family and their children, which could result in under-reporting of the prevalence given in this study. So, social desirability may have biased the parents’ responses (Fram et al. 2012). Because all measures regarding socio economic determinants and FS status were self-reported, it is possible that there was a response bias.
5 Conclusions
Food security is a human right, involving social justice, public health and policies. Children in our sample were experiencing high levels of HFI and CFI, which are associated to a series of health impairments, modifiable by assuring a situation of FS. Economic conditions are of utmost importance in this regard and a particular attention must be posed on food security during economic downturns.
Considering the results in this sample and the lack of research regarding this issues in Italy and Europe more broadly, future studies would benefit from longitudinal data exploring the situation of FI over time, socio-economic variables associated to it and the health implications in different contexts. Increased efforts in Italy and other high- income countries to expand investment in social protection, especially with regard to children, would likely tackle FI, an issue that is threatening our present and future.
Change history
05 November 2020
Springer Nature’s version of this paper was updated to present the Abstract and Keywords.
05 February 2021
A Correction to this paper has been published: https://doi.org/10.1007/s12571-020-01122-y
References
Angelopoulou, M. V., Shanti, S. D., Gonzalez, C. D., Love, A., & Chaffin, J. (2019). Association of food insecurity with early childhood caries. Journal of Public Health Dentistry, 79, 102–108.
Ashbrook, A., Hartline-Grafton, H., Dolins, J., Davis, J., & Watson, C. (2017). Addressing food insecurity; a toolkit for pediatricians. Washington, DC: American Academy of Pediatrics and the Food Research and Action Center. Available at: http://www.frac.org/wp-content/uploads/frac-aap-toolkit.pdf. Accessed Feb 2019.
Bahadur, K., Pai, S. H., Thoby, E., & Petrova, A. (2018). Frequency of food insecurity and associated health outcomes in pediatric patients at a federally qualified health center. Journal of Community Health, 43, 896–900.
Bickel, G., Nord, M., Price, C., Hamilton, W. L., & Cook, J. T. (2000). Guide to Measuring Household Food Security (Revised 2000). USDA, Food and Nutrition Service. Available at: https://fns-prod.azureedge.net/sites/default/files/FSGuide.pdf. Accessed Mar 2019.
Bonati, M., & Campi, R. (2005). What can we do to improve child health in Southern Italy? PLos Medicine, 2(9), e250.
Coleman-Jensen, A., Rabbitt, M. P., Nord, M., & Singh, A. (2015). Household food security in the United States in 2014. USDA Economic Research Report No 194. Washington, DC. Available at: https://www.ers.usda.gov/publications/pub-details/?pubid=45428. Accessed Mar 2019.
Coleman-Jensen, A., Rabbit, M. P., Gregory, C. A., & Singh, A. (2017). Household food security in the United States in 2017; U.S Department of Agriculture Economic Research Service. Available at: https://www.ers.usda.gov/publications/pub-details/?pubid=90022. Accessed May 2019.
Coleman-Jensen, A., Rabbitt, M. P., Gregory, C. A., & Singh, A. (2019). Household food security in the United States in 2018, ERR-270, U.S. Department of Agriculture, Economic Research Service. Available at: https://www.ers.usda.gov/publications/pub-details/?pubid=94848. Accessed 15 Jan 2020.
FAO, IFAD, UNICEF, WFP and WHO. (2019). The State of food security and nutrition in the world 2019. Safeguarding against economic slowdowns and downturns. Rome: FAO. Available at: http://www.fao.org/3/ca5162en/ca5162en.pdf. Accessed Nov 2019.
Ferro, R., Besostri, A., Meneghetti, B., Olivieri, A., Benacchio, L., Tabaccanti, S., et al. (2007). Oral health inequalities in preschool children in North-Eastern Italy as reflected by caries prevalence. European Journal of Paediatric Dentistry, 8(1), 13–8.
Fought, E. L., Williams, P. L., Willows, N. D., Asbridge, M., & Veugelers, P. J. (2017). The association between food insecurity and academic achievement in Canadian school-aged children. Public Health Nutrition, 20, 2778–2785.
Fram, M. S., Frongillo, E. A., Draper, C. L., & Fishbein, E. (2012). Development and validation of a child report assessment of child food insecurity and comparison to parent report assessment. Journal of Hunger & Environmental Nutrition, 8(2), 128–145.
Fram, M. S., Ritchie, L. D., Rosen, N., & Frongillo, E. A. (2015). Child experience of food insecurity is associated with child diet and physical activity. Journal of Nutrition, 145, 499–504.
Gundersen, C. (2013). Food insecurity is an ongoing national concern. Advances in Nutrition, 4, 36–41.
Hanson, K. L., & Connor, L. M. (2014). Food insecurity and dietary quality in US adults and children: a systematic review. American Journal of Clinical Nutrition, 100(2), 684–692.
Huang, J., Oshima, K. M. M., & Kim, Y. (2010). Does food insecurity affect parental characteristics and child behavior? Testing mediation effects. Social Service Review , 84, 381–401.
Istituto di Statistica. Povertà in Italia, Anno. (2017). Available at: https://www.istat.it/it/files/2018/06/La-povert%C3%A0-in-Italia-2017.pdf. Accessed Feb 2019.
Janice, K. E., & Ford-Jones, E. L. (2015). Food insecurity and hunger: A review of the effects on children’s health and behavior. Paediatrics & Child Health, 20, 89–91.
Jyoti, D. Frongillo, E., & Jones, S. (2005). Food insecurity affects school children’s academic performance, weight gain, and social skills. Journal of Nutrition, 135(12), 2831–2839.
Kirkpatrick, Sh., Dodd, K. W., Parsons, R., Ng, C., Garriguet, D., & Tarasuk, V. (2015). Household food insecurity is a stronger marker of adequacy of nutrient Intakes among Canadian compared to American youth and adults. Journal of Nutrition, 145(7), 1596–1603.
Kral, T. V. E., Chittams, J., & Moore, R. H. (2017). Relationship between Food Insecurity, Child Weight Status, and Parent-Reported Child Eating and Snacking Behaviors. Journal for Specialists in Pediatric Nursing, 22(2).
Loopstra, R. (2018). Interventions to address household food insecurity in high-income countries. Proceedings of the Nutrition Society, 77, 270–281.
Loopstra, R., Reeves, A., McKee, M., et al. (2016). Food insecurity and social protection in Europe: quasi-natural experiment of Europe’s great recessions 2004–2012. Preventive Medicine, 89, 44–50.
Loopstra, R., Reeves, A., & Stuckler, D. (2015). Rising food insecurity in Europe. The Lancet, 385, 2041.
Maia, I., Monjardino, T., Lucas, R., Ramos, E., & Santos, A. C. (2019). Household food insecurity and socio-demographic determinants in young adults: findings from a Portuguese population-based sample. International Journal of Public Health, 64(6), 887–895.
Martin-Fernandez, J., Grillo, F., Parizot, I., Caillavet, F., & Chauvin, P. (2013). Prevalence and socioeconomic and geograph-ical inequalities of household food insecurity in the Paris Region, France, 2010. BMC Public Health, 13, 486. https://doi.org/10.1186/1471-2458-13-48626
Miller, D. P., Nepomnyaschy, L., Ibarra, G. L., & Garasky, S. (2014). Family structure and child food insecurity. American Journal of Public Health, 104, 70–76.
Molcho, M., Gabhainn, S., Kelly, C., Friel, S., & Kelleher, C. (2007). Food poverty and health among schoolchildren in Ireland: Findings from the Health Behaviour in School-aged Children (HBSC) study. Public Health Nutrition, 10, 364–370.
Niclasen, B., Petzold, M., & Schnohr, C. W. (2013). Adverse health effects of experiencing food insecurity among Greenlandic school children. International Journal of Circumpolar Health, 72, 20849. https://doi.org/10.3402/ijch.v72i0.20849
Pereira, A. L., Handa, S., & Holmqvist, G. (2017). Prevalence and correlates of food insecurity among children across the globe. Available at https://www.unicefirc.org/publications/pdf/IWP_2017_09.pdf. Accessed Mar 2019.
Perreira, K. M., & Ornelas, I. J. (2011). The physical and psychological well-being of immigrant children. The Future of Children, 21, 195–218.
Petralias, A., Papadimitriou, E., Riza, E., et al. (2016). The impact of a school food aid program on household food insecurity. European Journal of Public Health, 26, 290–296. https://doi.org/10.1093/eurpub/ckv223
Rocha, N. P., Milagres, L. C., De Novaes, J. F., & Franceschini, S. C. (2016). Association between food and nutrition insecurity with cardiometabolic risk factors in childhood and adolescence: a systematic review. Revista Paulista de Pediatria, 34, 225–233.
Save the Children. (2019). Il miglior inizio. Disugualianze e opportunità nei primi anni di vita. Report 2019. Available at: https://s3.savethechildren.it/public/files/uploads/pubblicazioni/il-miglior-inizio-disuguaglianze-e-opportunita-nei-primi-anni-di-vita.pdf. Accessed Oct 2019.
South, A. M., Palakshappa, D., & Brown, C. L. (2019). Relationship between food insecurity and high blood pressure in a national sample of children and adolescents. Pediatric Nephrology, 34(9), 1583–1590.
Tarasuk, V., Fafard, St-Germain, A. A., & Mitchell, A. (2019). Geographic and socio-demographic predictors of household food insecurity in Canada, 2011–12. BMC Public Health, 19, 12.
Trapp, C. M., Burke, G., Gorin, A. A., Wiley, J., Hernandez, D., Crowell, R., et al. (2015). The relationship between dietary patterns, body mass index percentile, and household food security in young urban children. Childhood Obesity, 11, 148–155.
United States Department of Agriculture, Economic Research Service. (2012). U.S. household food security survey module: Three-stage design, with screeners. Available at: https://www.ers.usda.gov/media/8271/hh2012.pdf. Accessed Nov 2016.
Whitsett, D., Sherman, M. F., & Kotchick, B. A. (2019). Household food insecurity in early adolescence and risk of subsequent behavior problems: Does a connection persist over time? Journal of Pediatric Psychology, 44, 478–489.
Zaçe, D., Di Pietro, M. L., Caprini, F., de Waure, C., & Ricciardi, W. (2020). Prevalence and correlates of food insecurity among children in high-income European countries. A systematic review. Annali dell’Istituto Superiore di Sanità, 56(1), 90–98.
Funding
Open access funding provided by Università Cattolica del Sacro Cuore within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors declare no conflict of interests.
Additional information
The original online version of this article was revised: Abstract and Keywords have been added in the paper.
Supplementary Information
ESM 1
(DOCX 17.2 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zaҫe, D., Di Pietro, M.L., Reali, L. et al. Prevalence, socio-economic predictors and health correlates of food insecurity among Italian children- findings from a cross-sectional study. Food Sec. 13, 13–24 (2021). https://doi.org/10.1007/s12571-020-01111-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12571-020-01111-1