Abstract
As life expectancy continues to increase, there is a growing concern that the same pace of health improvement may not follow. An ageing population spending more years in disability and long-term sickness can place a significant financial burden on society. It is therefore crucial for governments to accurately forecast not just life expectancy but also healthy life expectancy. In particular, examining the highest healthy life expectancy can provide valuable information, as it represents the current best experience worldwide. Although there have been numerous studies on forecasting life expectancy, relatively few authors have investigated the forecasting of healthy life expectancy, often due to health data limitations. In this paper, we propose a Bayesian approach to co-model the highest healthy life expectancy and the highest life expectancy. The resulting forecasts would offer useful insights for governments in shaping healthcare and social policies to improve the wellbeing of seniors and retirees.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Introduction
Life expectancy has been rising globally for more than a century. For example, female (period) life expectancies at birth in the UK and US have climbed from 72.1 and 72.0 in 1951–1955 to 82.9 and 81.0 in 2016–2020, respectively. Traditionally, this indicator has been used to estimate how long people are expected to live and assess the overall wellbeing of a population. However, recent attention has gradually shifted to the quality of life, not just the quantity of life. Higher life expectancy does not necessarily mean more years of good health. To evaluate the situation, we have to delve deeper into the health states beyond the mortality patterns (e.g. Majer et al., 2013). But while mortality data are widely available, health data are usually scarcer and need to be collected from multiple sources.
Despite the challenges in data availability, healthy life expectancy serves as a valuable alternative indicator to life expectancy. In the broad sense, it represents the expected number of years of healthy life remaining for a person from a hypothetical cohort in a calendar year, and it includes a range of population health measures that incorporate both mortality and morbidity information and can be used to estimate both the length of life and the years spent in good health. Health expectancy (Nusselder & Looman, 2004), health-adjusted life expectancy (Australian Institute of Health & Welfare, 2017), disability-free life expectancy (Jagger et al., 2016), and healthy working life expectancy (Lynch et al., 2022) are some examples of this approach. It is essential to consider healthy life expectancy alongside life expectancy to gain a more comprehensive understanding of the health status of a population. Examining the gap between life expectancy and healthy life expectancy can provide insights into the financial burden of disability and morbidity, which can be used to inform policy decisions and health interventions.
As noted in Jivraj et al. (2020), there are three possible scenarios that describe the relationship between life expectancy and healthy life expectancy. The first scenario is called “expansion of morbidity”, which occurs when life expectancy increases faster than healthy life expectancy due to no or slow delay in morbidity or poor health recovery (Fries, 1980). By contrast, the second scenario is called “compression of morbidity”, which occurs when the onset of morbidity is delayed to older ages at a faster rate than the improvement in life expectancy, leading to a shorter duration in morbidity (Olshansky et al., 1991). The third scenario is a “dynamic equilibrium”, which combines the previous two scenarios (Manton, 1982). It is characterised by a higher prevalence rate of mild or moderate disability but a shorter duration of severe disability. The expected gap between life expectancy and healthy life expectancy in the future has important implications for government planning on health and retirement policies.
When planning for health and social services, it is crucial to consider the future trends in population health carefully. Many policy or institution decisions, such as investment in medical training, research and development, or health infrastructure, can take years to yield results and would have consequences that last for decades. To make informed decisions, policymakers and healthcare professionals need to make accurate forecasts, which can help them allocate resources more effectively and prioritise health initiatives based on their potential impact. Moreover, generating alternative scenarios is an essential tool for identifying areas of uncertainty and mitigating potential risks. By developing the ability to adapt to changing conditions and more robust contingency plans, decision-makers can enhance the resilience and stability of health systems and social services.
Although forecasting life expectancy has been extensively covered in previous studies, few have examined the forecasting and simulation of healthy life expectancy. The challenge arises from less available health data in general and the more complex modelling required for multiple health states. Recently, Cao et al. (2020) applied the multiple linear regression and the autoregressive integrated moving average (ARIMA) model to project healthy life expectancy. Lynch et al. (2022) adopted a three-state model and the Lee and Carter (1992) approach to project healthy working life expectancy. In this paper, we take a different perspective and consider the highest level of healthy life expectancy observed in a calendar year (Permanyer et al., 2021) amongst about 200 countries. Specifically, we establish a Bayesian framework to jointly model the highest healthy life expectancy and the highest life expectancy. By utilising the historical patterns between these two measures, we can forecast and simulate future outcomes and scenarios. This extrapolation approach is trend-based and primarily uses time as the only covariate. It offers the advantage of not having to forecast any social or economic indicators, which can be cumbersome and unreliable. Moreover, as the highest healthy life expectancy represents the best experience worldwide, examining its trend can provide valuable information for policymakers and demographers. There are already a number of previous studies on the highest life expectancy (Canudas-Romo et al., 2019; Li & Liu, 2020; Liu & Li, 2019; Medford, 2017, 2021; Oeppen & Vaupel, 2002; Pascariu et al., 2018; Shkolnikov et al., 2011; Torri & Vaupel, 2012; Vallin & Meslé, 2009). It would be insightful to do a parallel investigation on the highest healthy life expectancy to fill the knowledge gap. Furthermore, there are several advantages in taking a Bayesian modelling approach here, including a coherent incorporation of multiple model structures, estimation of missing data, and the ability to simulate future paths of healthy life expectancies. We implement the proposed approach on data covering multiple countries and showcase its ability to produce reasonable modelling and forecasting results, along with probability intervals that effectively capture the uncertainty in future outcomes.
The rest of the paper is structured as follows. In the next section, we inspect the highest life expectancy and healthy life expectancy trends and examine their historical patterns. Then we introduce the proposed Bayesian approach for modelling the highest life expectancy and healthy life expectancy jointly and illustrate its application to the data collected. Afterwards, we extend the approach to forecast healthy life expectancy for individual countries. Lastly, we present the concluding remarks. The “Appendix” gives more details about the Bayesian simulation process.
Best-performance healthy life expectancy
Two sets of healthy life expectancy at birth data of both sexes are collected from the WHO (World Health Organization)Footnote 1 for four years 2000, 2010, 2015, and 2019, covering a total of 183 countries, and from the GBD (Global Burden of Disease Study)Footnote 2 for the period of 1990–2019 over 204 countries. The WHO data are not available for every calendar year, implying that there are many missing values in our Bayesian modelling process, and the GBD data are also unavailable for earlier periods. Life expectancy at birth data are obtained from the HMD (Human Mortality Database, 2022)Footnote 3 for the period of 1950–2020 for 41 populations. We follow Tuljapurkar et al. (2000) and Lee and Miller (2001) and choose the HMD data period from 1950 to exclude the structural changes or extreme volatilities in mortality levels that occurred in the first half of the twentieth century. Moreover, as noted in Liu and Li (2019), the highest life expectancy trend since 1751 can be split optimally into a few linear segments with different slopes. The most recent segment of 1960–2014 has a slope of 0.22, which is smaller than those of the previous two segments (~ 0.28) and is quite steady since then. We then record the highest life expectancies and the highest healthy life expectancies of females and males among all the populations in each year from 1950 to 2020, where data are available.
The GBD estimation strategy on mortality and morbidity is devised to work with the diversity of data sources and the potential biases in data. There are a number of major steps, including age-specific fertility estimation, under-5 mortality estimation, adult mortality estimation, age-specific mortality estimation (via a relational model life table system), allowance for fatal discontinuities (e.g. wars, natural disasters), and population estimation. For each step, it is required to consider the data availability, deal with the known biases, and perform the data synthesis, coping with the issues of missing records and differences in measurement methods.
The GBD study encountered various limitations caused by the availability of high-quality data or the use of low-quality data. For instance, the sparsity of census data in certain countries and the lag between censuses affected the completeness in estimation. The mortality estimation for the adult ages where there was no vital registration system depended heavily on estimates indirectly deduced from sibling survival data, household death recall from censuses and surveys, and covariates in data-sparse periods. Since the GBD and WHO data are the only two publicly available healthy life expectancy data sets covering numerous countries, despite their limitations, we investigate both data sets in parallel and compare their results in this paper. We note that the proposed model (in the next section) is based fundamentally on the best-performing countries, which are expected to have data of higher quality. As shown in the following sections, the model results and analysis are broadly consistent and can provide useful insights for public health policymakers, healthcare professionals, economists, actuaries, and demographers.
The Sullivan’s methodFootnote 4 is adopted by the WHO in computing healthy life expectancy and is the most widely used method in practice. It requires cross-sectional data only as it is prevalence-based. By contrast, if one wants to model the changes in health state across time, a multiple-state model has to be used, which requires more detailed longitudinal data. Both approaches would yield similar results when transition rates change smoothly and regularly over time. This method is also used in the GBD for estimating healthy life expectancy.Footnote 5
Oeppen and Vaupel (2002) illustrated that the highest female life expectancy at birth has increased steadily by 0.24 years per annum for 160 years since 1840. They called this measure “best-performance” or ‘best-practice’ life expectancy. Their discovery has far-reaching implications for demographic studies and forecasting (Li & Liu, 2020). Firstly, the persistent upward trend presents strong evidence against the argument that future life expectancy level has a limit (e.g. Dong et al., 2016). Secondly, the highest life expectancy can be used as an important reference for policymakers and demographers when evaluating the validity of country-specific forecasts. What’s more, it offers an alternative and insightful way of forecasting mortality by seeing global mortality improvements as the result of an implicit and continuing competition between populations, instead of the more isolated perspective (e.g. Lee & Carter, 1992) usually taken. In particular, individual countries would experience different rates of mortality improvements at different stages of economic and medical development.
Given the significance of the highest life expectancy, it would be interesting to explore this concept further and conduct a parallel study on the highest healthy life expectancy. We now refer to the former as the best-performance life expectancy (BPLE) and the latter as the best-performance healthy life expectancy (BPHALE), and we consider both sexes instead of just females. While Permanyer et al. (2021) briefly examined the “best-practice healthy life expectancy” concept for females, we provide a more formal mathematical definition below and define the BPHALE as
where \(hale_{i,j,t}\) is the (period) healthy life expectancy of country j of sex i in calendar year t, given that the total number of countries is adequately large. Similarly, the BPLE can be expressed as
where \(le_{i,j,t}\) is the (period) life expectancy of country j of sex i in year t.
Figure 1 plots the observed BPLEs and BPHALEs of females and males from 1970 to 2020. It can be seen that all the trends are upward and largely linear, suggesting that not only there is no sign of cessation in the overall increasing trend of human life expectancy, but also the human life can be expected to stay healthy for a longer duration in the future. Table 1 lists the top five performers in healthy life expectancy in 2000, 2010, 2015, and 2019 based on the WHO data. For females, the frequent winners include Japan, Singapore, South Korea, France, and Spain, and their rankings look quite stable over the last twenty years. For males, the top performers include Japan, Singapore, Iceland, and Israel, but the competition appears to be slightly more open and the frontrunners swap positions in different years. While it is not surprising to see that the female figures are higher than the male ones, it is remarkable to observe that the value at each rankFootnote 6 has been increasing continuously over the period. These observations strongly suggest that the BPHALE is likely to continue to reach even higher levels over time. Table 1 also provides the top performers based on the GBD data. Despite the small differences in the healthy life expectancy values, similar countries are identified for females (Japan, Singapore, and South Korea) and males (Japan, Singapore, Iceland, and Israel). Again, the observed value at each rank has been rising over time.
Furthermore, the gap between the BPHALE and the BPLE (double arrows in Fig. 1) has also increased steadily during the period. Based on the WHO data, for females, this gap has risen from 11.0 years in 2000 to 12.6 years in 2019. For males, the gap has climbed from 8.4 years in 2000 to 9.5 years in 2019. (As a proportion of the BPLE, the BPHALE has declined from 87.0% in 2000 to 85.7% in 2019 for females, and from 89.2% to 88.4% for males.) These findings point to an overall expansion of morbidity, in which the average annual increase in the gap is 0.08 years for females and 0.06 years for males. Based on the GBD data, over a longer data period, the average annual increase in the gap is 0.06 years for females and 0.02 years for males. These statistics carry important implications for social welfare and healthcare policy planning, as people spending a longer time in morbidity can place a greater financial strain on governments and societies. It is also worth noting that although females live longer on average, they also experience a longer period of morbidity. This observation indicates that females would be more likely to suffer from financial stress after retirement and would need more healthcare and financial support and social services accordingly. For individual countries, Fig. 2 further illustrates that the difference between life expectancy and healthy life expectancy (i.e. duration in morbidity) has also increased over time. For the WHO data, almost all cases demonstrate an increase (those points above the diagonal line) over each period (from 2000 to 2010, 2010 to 2015, and 2015 to 2019). For the GBD data, despite the annual fluctuations (especially for males), the duration in morbidity has a broad increasing trend over the recent three decades. These observations provide more evidence for an expansion of morbidity in general for different countries.
Villavicencio et al. (2021) performed a simple Monte Carlo simulation and argued that the increasing gap between the BPHALE and the BPLE is not statistically significant in the GBD data, questioning about the data reliability. Basically, they assumed that the BPHALE values follow the normal distribution with their means equal to the point estimates and their standard deviations equal to one quarter of the corresponding 95% uncertainty intervals provided in the GBD data. They then simulated many scenarios, applied linear regression to each scenario, and calculated the sample means and 95% confidence intervals of the slope across all the simulated scenarios. As shown in Table 2 (first two columns), they noted that the 95% confidence intervals for the BPHALE and BPLE overlap and concluded that the differences in their trends (i.e. increasing gap between the BPHALE and BPLE) are insignificant. However, their approximation method is probably over-simplified—they just simulated each BPHALE value directly from a very simple normal distribution (noted as “Method 1” in Table 2), ignoring the fact that the underlying health data uncertainties of individual countries can potentially “offset” one another to some extent in the data estimation / synthesis. An alternative approximation approach is to simulate the healthy life expectancy value for each single country from a similar normal distribution and then collect the maximum value amongst these simulated values for different countries (noted as “Method 2”). We provide the resulting estimates in Table 2 (last column). For comparison purposes, we also repeat the approach in Villavicencio et al. (2021) and report our results in Table 2 (third column).
Using the initial approach (Method 1), we generate very similar estimates for females, while the estimates of the mean and 95% confidence interval are about 0.01 smaller for males. By contrast, under the alternative approach (Method 2), the 95% confidence intervals estimated are narrower for both sexes. For females, the differences in the BPHALE and BPLE trends can be treated marginally as insignificant at 5% significance level, but they become statistically significant at 10% level. For males, the differences in the BPHALE and BPLE trends are statistically significant at 5% level. These new results suggest that the widening gap between the BPHALE and BPLE as reflected in the GBD data is actually valid and clear.
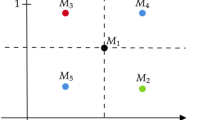
Figure 3 demonstrates the observed healthy life expectancy values of Australia, Brazil, India, and Japan from 1990 to 2019. They are plotted together with the BPHALE and the lowest healthy life expectancy,Footnote 7 which represent the best and worst experiences respectively and may be seen as some form of upper and lower bounds here. The four countries shown possess different levels of economic development and health systems, and their healthy life expectancies spread well across the range between the highest and lowest values in each year. While the lowest healthy life expectancy trend appears to be slightly more volatile, it can be observed that the low-income countries have improved at a faster pace than the high-income countries generally. For instance, healthy life expectancy has increased by about seven years from 2000 to 2019 for females in India, compared to an increase of only less than two years for females in Australia. It means that the health experiences of different countries are converging quite rapidly over time. This convergence appears to be driven by globalisation, enabling nations to become more connected and share their medical knowledge and healthcare experiences more effectively. For instance, Mukherjee and Krieckhaus (2012) analysed a pooled data set of 132 countries and found that on balance globalisation has a positive impact on human wellbeing. Welander et al. (2015) used panel data of 70 developing countries and concluded that globalisation and democracy are linked with better child health. This pattern is further illustrated in Fig. 4, in which there is clearly a negative relationship between the increase in healthy life expectancy (during the period of 1990–2019) and the GPD level per capita. There is a strong tendency for the low-income countries to catch up with the high-income countries.
Bayesian co-modelling approach
Bayesian joint model
As shown in Fig. 1, the momentum of the BPLE and BPHALE increases are strong, and the trends are quite stable during the period. Torri and Vaupel (2012) modelled this persistent (female) BPLE trend with the ARIMA(p, 1, 1) model. In order to cope with both sexes simultaneously, we incorporate the vector autoregressive integrated moving average, VARIMA(p, 1, 0) structure into the proposed Bayesian frameworkFootnote 8 and treat the female and male BPLEs as bivariate time series. We apply the standard Box-Jenkins method and examine the sample autocorrelations and partial autocorrelations and find that p = 1 is the optimal choice for the BPLE trends. Furthermore, as the gap between the BPHALE and the BPLE increases continuously and the progression is quite steady, we assume that the gaps of females and males follow the VARIMA(0, 1, 0) structure (i.e. bivariate random walk with drift) and integrate this structure within the Bayesian framework.
Mathematically, the proposed Bayesian joint model structure for the BPLEs and BPHALEs can be expressed as follows. The VARIMA(1, 1, 0) structure for the BPLEs is
in which \(\Delta\) is the first difference operator, \(bple_{i,t}\) is the BPLE value in year t (i = 1 for females and i = 2 for males), \(\theta_{i}\)’s are the intercept parameters, \(\varphi_{i,j}\)’s are the vector autoregressive parameters, and \(\varepsilon_{i,t}\)’s are bivariate normal error terms in year t. The VARIMA(0, 1, 0) structure for the BPHALEs is
in which \(gap_{i,t} = bple_{i,t} - bphale_{i,t}\) is the gap between the BPHALE and the BPLE in year t, \(\mu_{i}\)’s are the constant terms, and \(\epsilon_{i,t}\)’s are bivariate normal error terms in year t. The prior distribution for the unknown (intercept, autoregressive, constant) parameters θ is assumed as multivariate normal, where the hyperprior distribution for its mean vector M is taken as multivariate normal and the hyperprior distribution for its inverse covariance matrix Ω–1 as Wishart. The prior distributions for the inverse covariance matrices of the error terms, \(\Sigma_{\varepsilon }^{{{-}{1}}}\) and \(\Sigma_{\epsilon }^{{{-}{1}}}\), are set as Wishart.Footnote 9
We utilise WinBUGSFootnote 10 (Spiegelhalter et al., 2003) to conduct the Bayesian Markov chain Monte Carlo (MCMC) simulations for the proposed joint model structure. The purpose is to simulate samples from the posterior distribution of the unknown parameters and from the predictive distribution of future values. In theory, the posterior distribution is derived from the equation f (θ|D) ∝ f (D|θ) f (θ), and the predictive distribution is derived from the equation f (x|D) = ∫ f (x|θ) f (θ|D) dθ. For the proposed model here, these distributions are analytically intractable, and the MCMC simulation procedure is a practical alternative to provide a good approximation.
Li (2014) noted the benefits of incorporating different model structures in a Bayesian setting. For instance, the two model structures as described above are integrated coherently within the Bayesian framework. Estimating all their parameters in the same Bayesian process avoids the bias in estimation that would arise if the two model structures were fitted to the data separately. Moreover, the missing BPHALE data are automatically imputed or interpolated from the other values that are available during the simulation process. This ability to approximate the missing values is particularly useful for health data as they are often limited or incomplete. Furthermore, future paths or scenarios of the BPHALE are generated directly from the simulation process. The prediction intervals can be constructed based on the simulated values, allowing for the inherent uncertainty (via the error terms of the time series structures above) as well as the parameter uncertainty (as the model parameters are treated as random variables). Taking both of these into account can more adequately describe the overall uncertainty of the data, modelling process, and future outcomes.
Model results
Figure 5 (left column) shows the observed/imputed and the forecasted BPHALE and BPLE values for both sexes from 1970 to 2050, including the 95% prediction intervals. Based on the simulated results, the BPHALE and BPLE upward trends observed in 1970–2020 are expected to continue for the next thirty years. Back in 1960, 1970, 1980, and 1990 where the WHO data are unavailable, the imputed BPHALE values are 68.2, 68.8, 70.8, and 71.7 (66.4, 65.6, 66.2, and 68.2) years for females (males), respectively. The corresponding forecasted BPHALE values in 2030, 2040, and 2050 are 76.6, 77.7, and 78.9 (73.8, 75.0, and 76.1) years for females (males). It means that the gap between the BPHALE and the BPLE of females (males) is estimated to increase from 6.9 (5.5) years in 1951 to 12.7 (9.6) years in 2020, and further to 15.2 (11.3) years in 2050. In fact, based on the simulated posterior distribution, the 95% probability intervals of the slope difference between the BPHALE and BPLE upward trends are [0.04, 0.12] for females and [0.05, 0.07] for males during the data period. Both intervals do not cover 0, suggesting that the widening gap is statistically significant for both sexes. Moreover, using the GBD data, the imputed BPHALE values are 66.7, 67.5, and 69.7 years for females and are 64.7, 64.4, and 65.5 years for males in 1960, 1970, and 1980. The corresponding forecasted BPHALE values are 76.6, 78.0, and 79.4 years for females and are 75.4, 77.0, and 78.5 years for males in 2030, 2040, and 2050. The resulting gap increases from 12.9 (8.5) years in 2020 to 14.7 (8.8) years in 2050 for females (males). Compared to the estimates using the WHO data, the backcasted BPHALE values using the GBD data are about one year smaller for both sexes, while the forecasted values are around two years larger for males but are similar for females. Consequently, the gap is estimated to increase at a slower pace for both sexes (more so for males). These differences are in line with those reported earlier regarding Fig. 1. Figure 5 (right column) also shows the imputed BPHALE values from 1951, including the corresponding 95% probability intervals. First, the uncertainty of the imputed values is generally lower than the uncertainty of the forecasted values for a given time duration. Second, the uncertainty of the imputed values increases as one goes further back to the past.
In effect, this Bayesian joint model makes use of the annual BPLE data available and the historical relationships between the BPHALE and BPLE increases. It provides a reasonable backcastFootnote 11 of the BPHALE values before the starting year of the health data, which would be of interest to demographic researchers in studying healthy life expectancy in the more distant past, as well as a forecast for the next few decades, which would be useful for a range of applications in practice. However, we confine our forecasting analysis up to 2050 only—there are many challenges and uncertainties lying ahead, e.g. medical breakthroughs on ageing, cure for cancer, and behavioural and social changes (e.g. Christensen et al., 2009; Vaupel et al., 2021).
These results have some important implications for policymakers and healthcare professionals. First, as the duration in morbidity prolongs further, more resources need to be allocated to prepare for the higher medical and healthcare expenditure. Second, females continue to spend a longer time in morbidity, where its difference between both sexes is estimated to increase from 3.1 years in 2019 to 3.9 years in 2050 (based on the WHO data). Females then need comparatively more financial support, healthcare facilities, and social services, even more so in the foreseeable future. Therefore, more effective planning and allocation of resources are essential to deal with the aggravating financial burden on governments and societies as a whole.
Nevertheless, producing a point forecast only is inadequate as there is always uncertainty in future outcomes. The analysis should be accompanied with alternative scenarios that encompass a broader spectrum of possible outcomes. This additional information can prove invaluable in long-term planning and investments in health-related matters, when comparing multiple options and assessing their potential effects under different circumstances in the future. Based on the 5,000 simulated samples, using the WHO data, the 95% prediction intervals for the future BPHALE values in 2030, 2040, and 2050 are [74.5, 78.7], [74.7, 80.8], and [74.9, 82.9] for females, and are [72.0, 75.7], [72.3, 77.6], and [72.7, 79.5] for males. Figure 6 provides a density plot of the simulated values in 2050, having roughly the shape of a normal distribution. The range between the 2.5th and 97.5th percentiles can provide some indication on the scope for policy change. In particular, if we consider the 2.5th percentile as the worst-case scenario in practice,Footnote 12 the mean forecasts may potentially underestimate the overall duration in morbidity in the next few decades by up to about two years. Without proper planning and preparation, such a shortfall can create a substantial financial strain on retirement systems and funding. Comparatively, using the GBD data, the 95% prediction intervals are [74.6, 78.7], [74.9, 81.1], and [75.6, 83.5] for females, and are [72.2, 78.6], [72.4, 81.9], and [72.4, 84.8] for males, in 2030, 2040, and 2050. As noted earlier, the gap between the BPHALE and the BPLE is estimated to increase at a slower pace with the GBD data. However, all the 2.5th percentile estimates from the GBD data are more or less the same as those based on the WHO data, which means that there could also be a larger extent of underestimation in the mean forecasts of the gap.
Forecasting for individual countries
Extended Bayesian joint model
We can further extend the earlier Bayesian joint model structure to forecast healthy life expectancy for individual countries. As discussed previously (regarding Fig. 3 and its discussion), healthy life expectancies of different countries have been converging during the last thirty years. Considering the reducing differences between countries and also the data limitations, we assume that the difference between a country’s healthy life expectancy and the BPHALE of females and that of males follow another VARIMA(0, 1, 0) structure, which is specified as
where \(\partial hale_{i,t}\) is the difference between a country’s healthy life expectancy and the BPHALE in year t, \(\alpha_{i}\)’s are the constant terms, and \(\omega_{i,t}\)’s are bivariate normally distributed error terms in year t. The prior distributions for the unknown parameters can be set similarly as before. Note that all the three model structures (BPLE, BPHALE, individual healthy life expectancy) are integrated and estimated within the same Bayesian framework.
Model results
As an example, Fig. 7 illustrates the observed/imputed and the resulting forecasted healthy life expectancy values of Australia, Brazil, Hungary, India, Indonesia, Nigeria, and Spain for both sexes from 2000 to 2040. The seven countries shown represent different stages of economic development, education levels, and health systems. Their healthy life expectancies range from the highest in Spain to the lowest in Nigeria. It shows that the upward healthy life expectancy trends occurred during 2000–2019 would remain strong in the coming two decades. Moreover, the low-income countries are expected to catch up with the leading countries gradually. For instance, it can be seen that the healthy life expectancy values of India and Nigeria are forecasted to improve at a faster pace than the others. These implications appear reasonable and realistic, considering the effects of globalisation, and the high GDP growth rates and recent economic development of the two countries over the last two decades. In line with our earlier discussion about Fig. 4, there is generally a negative relationship between the forecasted increase in healthy life expectancy (from 2019 to 2040) and the income level. Based on the WHO data, from the lowest income quartile to the highest, the forecasted increases in healthy life expectancy are 9.5, 5.0, 3.6, and 2.9 years (7.8, 3.4, 2.9, and 2.9 years) on average for females (males), respectively. Based on the GBD data, the corresponding figures are 5.5, 3.2, 2.2, and 2.4 years (5.3, 2.9, 2.2, and 2.9 years). Broadly speaking, healthy life expectancy of a country with lower GDP per capita tends to increase faster, and vice versa, leading to gradual convergence of health outcomes across countries with varying income levels.
Next, we attempt to assess the forecasting performance further by applying the extended Bayesian joint model to the GBD and HMD data of 1950–2009, forecasting the healthy life expectancy values in 2010–2019, and comparing the forecasted and actual values of the 204 countries. We split the countries into four quartile groups based on the observed healthy life expectancy values in 2019 and calculate the mean absolute error (MAE) and the mean square error (MSE)Footnote 13 for each group. As a comparison, we also use the ARIMA(0, 1, 0) model (i.e. random walk with drift) on the healthy life expectancy data (only) of 1990–2009 and extrapolate the 2010–2019 values correspondingly. Table 3 presents the numerical results of this out-of-sample analysis. First, the forecasting errors for females are smaller than the errors for males, except for the lowest quartile group of healthy life expectancy. This result is broadly in line with the earlier findings on the higher volatility and the wider prediction intervals for males. Second, the forecasting errors tend to increase from the highest quartile group to the lowest. This observation can be explained by the fact that the low-income countries with poorer health outcomes often have more volatile healthy life expectancy trends (probably due to unstable conditions and data inadequacy), and so it is more difficult to make accurate forecasts. Moreover, it is interesting to see that the extended Bayesian joint model outperforms the ARIMA(0, 1, 0) model for the two highest quartile groups, but the situation is reversed for the remaining two groups. It appears that the extended Bayesian joint model, which exploits the BPHALE trend, works better with the high-income countries, capturing their more stable relationships with the best performing countries in health outcomes. Besides the mean forecasts, Table 3 also provides the proportion of the observed values falling outside the 95% prediction interval. Under the extended Bayesian joint model, the proportions are largely around 5% or lower (except for the lowest quartile group), indicating that the level of uncertainty allowed is adequate and reasonable. By contrast, under the ARIMA(0, 1, 0) approach, the proportions of outliers are all around 20% or higher. It means that the estimated prediction intervals fail to capture the actual observations adequately and the implied level of uncertainty is too low.
Note that this extended Bayesian joint model for individual countries is a “top-down” approach, where the consideration starts from the record level of life expectancy and the record level of healthy life expectancy to a country’s own healthy life expectancy. It follows the spirit of Pascariu et al. (2018), in which the structuring starts from the record level of life expectancy to a country’s life expectancy. This approach exploits the consistent BPLE and BPHALE trends and their steady relationships observed over time, resulting from ongoing competition and interactions between a large number of countries. Alternatively, one can take a “bottom-up” approach, where each country’s healthy life expectancy is modelled and forecasted and then the BPHALE is computed as the maximum value across different countries. While forecasting each country on its own may be beneficial for the low-income countries as discussed above, putting together the individual forecasts for different countries and then calculating the maximum value would have a number of potential issues. First, if each country is forecasted separately, the results would be affected by the higher volatility at the individual level. The trend of a single country is often less stable, especially for those that have high mortality or a small population size. One would also lose the opportunity to “borrow” information from the other countries for the modelling process. Second, if different countries are forecasted jointly instead, the dimension of the problem becomes very high. It involves multivariate time series, the dimension of which is equal to the number of countries included in the study. Some methods for dealing with this problem are the dimension reduction techniques and sparse vector autoregressive models. Regardless of the method used, however, there is no guarantee that the resulting forecasts would be reasonable, due to the sophistication of these methods and the arbitrariness of the required assumptions. We deem that the extended Bayesian joint model is a natural way to extrapolate the best-performance trends and provides a useful and practical alternative for modelling healthy life expectancy for individual countries (e.g. Li, 2023).
As a final check, we compare the forecasted BPHALE values in Fig. 5 with the maximum values amongst the forecasted healthy life expectancy values of all the individual countries in this section. For females (males), the previously forecasted values are 75.86, 76.58, 77.28, and 77.97 (74.57, 75.38, 76.19, and 76.99) in 2025, 2030, 2035, and 2040. The corresponding maximum values from the extended Bayesian joint model are 75.76, 76.46, 77.15, and 78.11 (73.16, 74.12, 75.65, and 77.18), respectively. The two sets of results are very close, suggesting that the overall Bayesian framework is reasonably coherent and consistent.
Concluding remarks
We present a novel approach of examining the highest level of healthy life expectancy and develop a Bayesian joint model for co-modelling the BPHALE and the BPLE. The proposed modelling approach is extrapolative by nature—it exploits the historical relationships between the highest levels of life expectancy and healthy life expectancy and does not require the forecasting of any social or economic indicator variables. The Bayesian process allows one to integrate multiple model structures coherently, approximate the missing values, and simulate future paths and scenarios, incorporating both the inherent uncertainty and parameter uncertainty. The BPHALE reflects the best global performance and provides useful information for policymakers in designing retirement and healthcare policies and for demographers in studying the long-term trend of health.
There are a number of major results in this study. First, based on the WHO and HMD data, the BPHALE and BPLE have increased annually by about 0.1 and 0.2 years over the last few decades. Their upward trends are persistent and approximately linear and are forecasted to continue under our Bayesian model. Second, the gap between the two measures has also increased annually by about 0.07 years during the period. These results suggest that while the human life is expected to live longer in the future, more years will also be spent in morbidity. Accordingly, more effective planning and distribution of resources are needed to address the mounting medical and healthcare needs and costs, particularly for females. Moreover, the simulation of alternative scenarios provides a robust assessment of future uncertainty, and the width of the 95% prediction interval indicates the potential scope for policy adjustments. Considering the worst-case scenario thoroughly can help prepare for the possibility of a longer-than-anticipated duration in morbidity. Furthermore, we extend the Bayesian model for forecasting healthy life expectancy for a single country. We find that the low-income countries would continue to improve at a faster speed than the leading countries. Finally, the Bayesian modelling process also offers a statistically sound way to backcast the past BPHALE values, which would be of interest to those demographers studying longer-term health trends.
One limitation of this study is the nature of the healthy life expectancy data. As noted in Villavicencio et al. (2021), the definitions of healthy life expectancy can vary significantly between different studies and databases. We attempt to deal with this problem (partially) by investigating two data sets from different sources at the same time for comparison, where both results show a rising BPHALE trend and an increasing gap between the BPHALE and the BPLE. However, the underlying methods for producing those data are rather opaque, and their estimations have been performed for a large number of countries with very different situations. Furthermore, the definition of healthy life expectancy can also change over time. As diagnostic methods improve with medical advances and the awareness of health maintenance (including mental health) rises with higher education and economic development, it may be more likely for some people to appear as unhealthier than otherwise. Further research with more detailed health data is called for.
Another limitation of this research is that the extrapolation approach adopted is arguably not as interpretable as the expectation approach and the explanation approach (Booth, 2006). The expectation approach makes use of individuals’ expectations and experts’ opinions. The explanation approach uses theories to describe the underlying relationships between demographic variables and the relevant social, economic, and environmental factors. However, experts’ opinions are often limited by the present knowledge which may not reflect possible future developments adequately. Moreover, it is difficult to build such explanation theories due to the intricacy of the problem and the general lack of detailed data covering a sufficiently long period of time, leading to a high risk of model misspecification. Despite its limitations, the extrapolation approach remains the most common approach in practice and can help one exploit the remarkable regularity in certain demographic trends over a sustained period of time.
The improvement in mortality and morbidity rates is a complex outcome of advances in various factors such as income, education, nutrition, and medicine. These factors differ between ages, time periods, birth cohorts, sexes, populations, and types of diseases. The aggregate result is a consistent and mostly linear increase in the BPLE and BPHALE, which suggests that these improvements are not isolated events but instead a continuous and regular stream of progresses. These trends have significant socioeconomic implications and point to the need for reforming retirement systems and revising the pension age. Social welfare and pension policies for seniors can remain solvent only when there is a large proportion of people being active in the workforce. When society is ageing rapidly, however, the sustainability of the current policies and systems would become highly questionable. It is vital for government officials to make more accurate forecasts and allow for different scenarios, where an underestimation of just a few years could lead to significant shortfall and financial strain. An inability to do so would mislead people’s life cycle decisions and give politicians an excuse to delay making painful but unavoidable changes to the current welfare and healthcare systems. The interaction between policy decisions, innovation in technologies, and growing social, environmental, and geopolitical risks need to be investigated carefully and extensively to provide a sustainable and healthy environment for the current and the next generations.
The extent that a country’s healthy life expectancy is below the BPHALE can be a useful measure of the potential for further improvement under the existing knowledge, technology, and practices. After rapid improvements when catching up with the leaders, progress would eventually slow down. But it does not mean that the healthy life expectancy level of the country will reach a maximum any time soon. As more health data becomes available, future research can explore in more detail how the rates of increase of different countries converge in the long term. In this regard, an autoregressive kind of model would be more suitable than the random walk with drift for making longer-term forecasts.
Notes
In practice, the computation of healthy life expectancy is usually based on data from several sources, due to health data limitations. Moreover, we need the annually available HMD data for our Bayesian modelling process. While the number of countries is different between the WHO, GBD, and HMD data, we focus on the highest expectancies, and the missing data of high-mortality countries are very unlikely to have any impact on the highest expectancies even if they were available.
This method uses the “equivalent lost healthy year fraction (adjusted for comorbidity) at each age in the current population (for a given year)” to divide the “hypothetical years of life lived by a period life table cohort at different ages” into “years of equivalent full health and equivalent lost healthy years”. The equivalent lost healthy year fractions are calculated as the “all-cause years lost due to disability rate per capita, adjusted for independent comorbidity, by age, sex, and country”.
If the healthy life expectancy values of different countries in year t (i.e. halei,1,t, halei,2,t, …, halei,n,t) are treated approximately as independent and identically distributed random variables, the top five performers can be seen as the nth, (n − 1)th, (n − 2)th, (n − 3)th, and (n − 4)th order statistics, in which the sample size (total number of countries) is n. As noted in Li and Liu (2020), the general trend of converging mortality, particularly between high-income countries, provides some support to the working assumption of identical distribution. In this aspect, Liu and Li (2019) applied the maxima and minima generalised extreme value distributions to the highest and lowest life expectancies (i.e. nth order and 1st order statistics), respectively. Li and Liu (2020) applied the generalised extreme value theorem with Archimedean copulas to the BPLE (i.e. nth order statistic).
Liu and Li (2019) utilised both the highest and lowest life expectancies to develop approximate upper and lower bounds as a supplementary tool for forecasting life expectancy. We have excluded the data of Rwanda in 1994 and Haiti in 2010 when constructing the lower bound here, in order to remove the extreme outliers caused by historical events. The lower bound is slightly more volatile than the upper bound, probably due to the unstable conditions and the inadequacy in data collection in those countries with the lowest incomes.
Rosenberg and Young (1999) noted that it is more computationally efficient to use the AR models (instead of the MA models) in Bayesian modelling. In principle, if the selected AR order p is high enough, the model results are comparable to those under a fully specified ARIMA model. As such, we set the MA order as zero here.
\(\uptheta \sim {\text{MVN}}\left( {{\text{M}},{\Omega }} \right)\), \({\text{M}}\sim {\text{MVN}}\left( {{\Psi },{\Gamma }} \right)\), \(\Omega^{ - 1} \sim {\text{W}}\left( {{\text{R}}_{\Omega } ,10} \right)\), \(\Sigma_{\varepsilon }^{ - 1} \sim {\text{W}}\left( {{\text{R}}_{\varepsilon } ,4} \right)\), and \(\Sigma_{\epsilon }^{ - 1} \sim {\text{W}}\left( {{\text{R}}_{\epsilon } ,4} \right)\).
The WinBUGS code is available upon request.
Wang and Chan (2022) modified the Lee–Carter method to backcast the England and Wales mortality rates in the seventeenth and eighteenth centuries.
Examining the 2.5th percentile (which corresponds to approximately two standard deviations below the mean) is a commonly used but somewhat arbitrary approach. Alternatively, a less severe worst-case scenario could be defined using the 5th, 10th, or even 15th percentile.
The MAE and MSE are computed as the sample means of \(\left|\widehat{x}-x\right|\) and \({\left(\widehat{x}-x\right)}^{2}\) over time and the countries in the same quartile group, respectively, where \(\widehat{x}\) and \(x\) are the forecasted and observed values in 2010–2019.
References
Australian Institute of Health and Welfare. (2017). Health-Adjusted Life Expectancy in Australia: Expected Years Lived in Full Health 2011. https://www.aihw.gov.au/reports/burden-of-disease/health-adjusted-life-expectancy-australia
Booth, H. (2006). Demographic forecasting: 1980 to 2005 in review. International Journal of Forecasting, 22(2006), 547–581.
Cao, X., Hou, Y., Zhang, X., Xu, C., Jia, P., Sun, X., Sun, L., Gao, Y., Yang, H., Cui, Z., Wang, Y., & Wang, Y. (2020). A comparative, correlate analysis and projection of global and regional life expectancy, healthy life expectancy, and their GAP: 1995–2025. Journal of Global Health, 10(2), 020407.
Canudas-Romo, V., Booth, H., & Bergeron-Boucher, M. (2019). Minimum death rates and maximum life expectancy: The role of concordant ages. North American Actuarial Journal, 23(3), 322–334.
Christensen, K., Doblhammer, G., & Rau, R. (2009). Ageing populations: The challenges ahead. Lancet, 374(9696), 1196–1208.
Dong, X., Milholland, B., & Vijg, J. (2016). Evidence for a limit to human lifespan. Nature, 538(7624), 257–259.
Fries, J. F. (1980). Aging, natural death, and the compression of morbidity. New England Journal of Medicine, 303(3), 130–135.
Human Mortality Database. (2022). University of California, Berkeley (USA) and Max Planck Institute for Demographic Research (Germany). www.mortality.org
Jagger, C., Matthews, F. E., Wohland, P., Fouweather, T., Stephan, B. C. M., Robinson, L., Arthur, A., & Brayne, C. (2016). A comparison of health expectancies over two decades in England: Results of the cognitive function and ageing study I and II. Lancet, 387(10020), 779–786.
Jivraj, S., Goodman, A., Pongiglione, B., & Ploubidis, G. B. (2020). Living longer but not necessarily healthier: The joint progress of health and mortality in the working-age population of England. Population Studies, 74(3), 399–414.
Lee, R., & Miller, T. (2001). Evaluating the performance of the Lee–Carter method for forecasting mortality. Demography, 38(4), 537–549.
Lee, R. D., & Carter, L. R. (1992). Modeling and forecasting US mortality. Journal of the American Statistical Association, 87(419), 659–671.
Li, J. (2014). A quantitative comparison of simulation strategies for mortality projection. Annals of Actuarial Science, 8(2), 281–297.
Li, J. (2023). Bayesian joint modelling of life expectancy and healthy life expectancy and valuation of retirement village. Scandinavian Actuarial Journal. https://doi.org/10.1080/03461238.2023.2232816
Li, J., & Liu, J. (2020). A modified extreme value perspective on best-performance life expectancy. Journal of Population Research, 37(4), 345–375.
Liu, J., & Li, J. (2019). Beyond the highest life expectancy: Construction of proxy upper and lower life expectancy bounds. Journal of Population Research, 36(2), 159–181.
Lynch, M., Bucknall, M., Jagger, C., & Wilkie, R. (2022). Projections of healthy working life expectancy in England to the year 2035. Nature Aging, 2, 13–18.
Majer, I. M., Stevens, R., Nusselder, W. J., Mackenbach, J. P., & van Baal, P. H. M. (2013). Modeling and forecasting health expectancy: Theoretical framework and application. Demography, 50(2), 673–697.
Manton, K. G. (1982). Changing concepts of morbidity and mortality in the elderly population. The Milbank Memorial Fund Quarterly. Health and Society, 60(2), 183–244.
Medford, A. (2017). Best-practice life expectancy: An extreme value approach. Demographic Research, 36(34), 989–1014.
Medford, A. (2021). Modeling best practice life expectancy using Gumbel autoregressive models. Risks (Special Issue: Mortality Forecasting and Applications, edited by Jackie Li), 9, 51.
Mukherjee, N., & Krieckhaus, J. (2012). Globalization and human well-being. International Political Science Review, 33(2), 150–170.
Nusselder, W. J., & Looman, C. W. N. (2004). Decomposition of differences in health expectancy by cause. Demography, 41(2), 315–334.
Oeppen, J., & Vaupel, J. W. (2002). Broken limits to life expectancy. Science, 296(10), 1029–1031.
Olshansky, S. J., Rudberg, M. A., Carnes, B. A., Cassel, C. K., & Brody, J. A. (1991). Trading off longer life for worsening health: The expansion of morbidity hypothesis. Journal of Aging and Health, 3(2), 194–216.
Pascariu, M. D., Canudas-Romo, V., & Vaupel, J. W. (2018). The double-gap life expectancy forecasting model. Insurance: Mathematics and Economics, 78(C), 339–350.
Permanyer, I., Trias-Llimos, S., & Spijker, J. J. A. (2021). Best practice healthy life expectancy vs. life expectancy: Catching up or lagging behind? PNAS, 118(46), e2115273118.
Rosenberg, M. A., & Young, V. R. (1999). A Bayesian approach to understanding time series data. North American Actuarial Journal, 3(2), 130–143.
Shkolnikov, V. M., Jdanov, D. A., Andreev, E. M., & Vaupel, J. W. (2011). Steep increase in best-practice cohort life expectancy. Population and Development Review, 37(3), 419–434.
Spiegelhalter, D., Thomas, A., Best, N., & Lunn, D. (2003). WinBUGS User Manual. https://www.mrc-bsu.cam.ac.uk/wp-content/uploads/manual14.pdf
Torri, T., & Vaupel, J. W. (2012). Forecasting life expectancy in an international context. International Journal of Forecasting, 28(2), 519–531.
Tuljapurkar, S., Li, N., & Boe, C. (2000). A universal pattern of mortality decline in the G7 countries. Nature, 405(6788), 789–792.
Vallin, J., & Meslé, F. (2009). The segmented trend line of highest life expectancies. Population and Development Review, 35(1), 159–187.
Vaupel, J. W., Villavicencio, F., & Bergeron-Boucher, M. P. (2021). Demographic perspectives on the rise of longevity. PNAS, 118(9), e2019536118.
Villavicencio, F., Bergeron-Boucher, M. P., & Vaupel, J. W. (2021). The uncertainty surrounding healthy life expectancy indicators. PNAS, 118(46), e2115544118.
Wang, D., & Chan, W. S. (2022). Backcasting mortality in England and Wales, 1600–1840. North American Actuarial Journal, 26(1), 102–122.
Welander, A., Lyttkens, C. H., & Nilsson, T. (2015). Globalization, democracy, and child health in developing countries. Social Science & Medicine, 136–137, 52–63.
Acknowledgements
We thank the editor and referees for their very valuable comments and suggestions, which greatly enhance the presentation of this paper.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author has no relevant financial or non-financial interests and no competing interests to disclose.
Ethical approval
We declare that there are no potential conflicts of interest associated with this research. Furthermore, this study did not involve human participants or animals, and therefore, no informed consent was required for this project.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Regarding the Bayesian MCMC simulation process, we first generate 1000 simulated samples and discard them to remove the effects of the initial values. We then produce another 5000 simulated samples, using a thinning of 100, i.e., collecting the samples from every 100th iteration. Table
4 reports the Monte Carlo errors and the sample standard deviations of the simulated BPHALE and BPLE values in 2030, 2040, and 2050 using the WHO and HMD data. All the Monte Carlo errors turn out to be smaller than 1.5% of the sample standard deviations, suggesting that the level of convergence of the MCMC simulation is acceptable. As a rule of thumb, the Monte Carlo error for each variable of interest should be less than 5% of the sample standard deviation (Spiegelhalter et al., 2003). Figure
8 displays some autocorrelation plots over successive iterations (after thinning). The sample autocorrelations are all immaterial, which provide further indication that the level of convergence is adequate here, since high sample autocorrelations over successive samples and high Monte Carlo errors are often associated with poor convergence (Spiegelhalter et al., 2003). Moreover, Fig.
9 shows that there are no particular trends in the simulated values across iterations. The extent of convergence hence looks reasonable.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, J. Bayesian modelling of best-performance healthy life expectancy. J Pop Research 41, 8 (2024). https://doi.org/10.1007/s12546-024-09330-5
Accepted:
Published:
DOI: https://doi.org/10.1007/s12546-024-09330-5