Abstract
The low uptake of maternal healthcare services (MHS) in Nigeria is implicated in the country’s poor maternal health outcomes. In northern Nigeria where these outcomes are poorest, not much is known about the contribution of violence within unions on married women’s uptake of MHS. Using data on antenatal care (ANC) utilisation and place of delivery, and their sociodemographic confounders from the Nigerian Demographic and Health Survey, this study investigates this relationship. Results of univariate, bivariate and multivariate analyses show that 46.4% and 22.1% of the women had at least four ANC sessions and had health facility delivery respectively. At the subregional level however, the North-Central zone had the highest utilisation rates while the North-West zone had the lowest. The prevalence of intimate partner violence (IPV) ranged from 8.2% (sexual violence) to 16.7% (physical violence) and 35.8% (emotional violence). Subregional analysis of IPV shows that the North-West zone had the lowest prevalence rates. Contrary to some literature evidence, women who experienced IPV in the study area had higher odds of utilising MHS (P < 0.001). When the sociodemographic characteristics of the women were adjusted for, the relationship became statistically insignificant however. The association between the women’s socioeconomic characteristics and their MHS uptake suggests that attention be paid to the wealth and educational status of the population because of their propensity for sustaining the higher uptake recorded. The role of religion in the outcomes further suggests that it be used as a tool to promote the uptake of MHS in the region.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
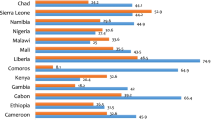
The uptake of maternal healthcare services in Africa’s most populous country, Nigeria, is among the poorest in the world. According to 2020 United Nations data, antenatal care (ANC) utilisation in Nigeria declined from 52% in 1990 to an all time low of 45% in 2008 and had only risen to 57% in 2018 (UNICEF, 2020). The data further shows that the percentage of women aged 15 to 49 in Nigeria who utilised health facilities for delivery oscillated between 31 and 39% between 1990 and 2018, except for 2011 when it was 45%. The percentage of deliveries attended to by skilled health personnel was as low as 30.8% in 1990 and had only risen to 43% in 2018. Postnatal care (PNC) utilisation in the country was 40% in 2013 and had risen marginally to 42% in 2018 (UNICEF, 2020). These figures show that except for ANC utilisation, maternal healthcare utilisation in Nigeria is worse than the continental average of 60.2% for health facility delivery and 63.9% for delivery by skilled health personnel (UNICEF, 2020). In Eastern Asia and the Pacific, the prevalence of health facility delivery and delivery by skilled personnel was 91.9% and 95.6% respectively. Both indicators were as high as 98.1% and 99.1% in Eastern Europe and much higher in Western Europe and North America. Even in Latin America with an almost similar fertility pattern with Sub-Saharan Africa, ANC utilisation was 90.6%, health facility delivery was 93.7% and delivery by skilled personnel was 93.5% in 2018. The poor uptake of these services is implicated in Nigeria’s maternal mortality ratio of 917 deaths per 100,000 live births – the fourth highest in the world after Sierra Leone (1120), South Sudan (1150) and Chad (1140) (WHO, 2019).
Within Nigeria, the level of utilisation is much lower in the three geopolitical zones of northern Nigeria. Data from the 2013 Nigerian Demographic and Health Survey (NDHS) shows that the percentage of women with a live birth in the five years preceding the survey who received ANC services in the north ranged from 41 to 67% as against 73% to 91% in the south. Only 11.5% of the women in the North-West region had a health facility delivery in 2013, compared to 80.2% in the South-East region (National Population Commission (NPC) [Nigeria] and ICF, 2014). In the 2018 survey, the pattern of utilisation was similar with only 15.7% of women in the North-West having a hospital delivery as against 79.8% in the South-East region (National Population Commission (NPC) [Nigeria] and ICF, 2019). The pattern is also reflected in the north–south variation in maternal mortality rates in Nigeria (Agan et al, 2018; Akinlo et al, 2016; Haruna-Ogun, 2018; Meh et al, 2019) and in the largely poor health outcomes in northern Nigeria (Alabi et al, 2014).
While studies have shown that the low level of uptake of maternal healthcare services in Nigeria is due to factors such as age, marital status, place of residence, number of children previously born, literacy, socioeconomic status, employment status, physical accessibility to the services, quality of services, culture and religion, media access, gender relations, and having someone to accompany the pregnant woman (Ononokpono et al, 2013; Adedini et al, 2014; Fapohunda & Orobaton, 2014; Dahiru & Oche, 2015; McNabb et al, 2015; Solanke et al, 2015; Abimbola et al, 2016; Adebowale & Akinyemi, 2016; Abubakar et al, 2017; Umar, 2017; Adewuyi et al, 2018; Haruna-Ogun, 2018; Barman et al, 2018; Adewoyin, 2021; Adewoyin et al., 2022a, 2022b), the role of intimate partner violence (IPV) in the low uptake has received little attention in Nigerian studies. IPV matters for maternal healthcare for several reasons. Firstly, IPV is the most common type of violence against women across the world (United Nations Women, 2019; WHO, 2016). One consequence of this is the likelihood that women may choose not to engage in outdoor activities like seeking healthcare that may expose them to being questioned about their psychological/emotional and physical wellbeing after suffering abuse. The mental and physical health of women who undergo IPV may therefore make maternal healthcare seeking less of a priority after being abused.
Further, the prevalence of IPV is rising and mostly under-reported, especially in sub-Saharan Africa (SSA). SSA is second in the prevalence of violence against women (21.5%) after Oceania’s 34.7% when Australia and New Zealand are excluded (United Nations Women, 2019). The World Health Organization puts the SSA prevalence at between 20 and 70% (WHO, 2013). In Nigeria, the prevalence ranges from 15.2 to 33.4% (Antai, 2011; Okemgbo et al., 2002; Onoh et al., 2013; Ononokpono & Azfredrick, 2014; Oyediran & Feyisetan, 2017). Study findings are also not uniform on the relationship between IPV and maternal healthcare seeking. For instance, while Leight and Wilson (2021), Idriss-Wheeler and Yaya (2021), Mai and Phyu (2020), Musa et al (2019), and Gashaw et al (2019) conclude that women who had experienced IPV were less likely to use maternal healthcare services, Kabiru (2018) and Maxwell et al (2018) did not find such an association. In the few Nigerian studies that investigated the association, the outcomes were similar. While Onoh et al (2013), Ononokpono and Azfredrick (2014), and Solanke (2014) report that IPV was associated with lower utilisation, Yaya et al (2019) did not find such association between physical and sexual violence and the uptake of maternal healthcare services. In northern Nigeria where maternal health outcomes are poorer and where the utilisation of maternal healthcare services are lower, such studies are much fewer.
In the context of the foregoing, this study investigates the association between IPV and the utilisation of maternal healthcare services among parous married women in northern Nigeria and hypothesises that married women who have experienced IPV are more likely to utilise maternal healthcare services. The choice of married women is predicated on the region’s religious and cultural beliefs about union formation and single motherhood. Most marriages in the region are strictly based on Islamic and cultural tenets that frown on all forms of pre-marital intimacy. Cohabitation in the region is therefore mostly after marriages have been formalised, unlike in other more liberal parts of the country. Consequently, intimate partner violence in northern Nigeria is mostly situated in a union (Solivetti, 1994). Further, and unlike in other regions, accessing reproductive health services in northern Nigeria is sometimes discriminatory. For instance, the utilisation of antenatal care (ANC) services in the region is usually within wedlock (Doctor, et al., 2012; Melah et al, 2003). Issues like single parenting and pregnancy outside wedlock among teenagers are largely unacceptable and stigmatised in the region (Anyebe et al., 2017; Adewoyin et al, 2020).
Methods
Study area and data source
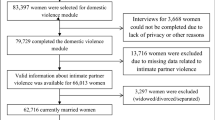
Nigeria is comprised of 36 States and a Federal Capital Territory (FCT). Based on geographical contiguity and cultural characteristics, the States and FCT are agglomerated as six geopolitical zones – North-East, North-West, North-Central, South-East, South-South and South-West. This study focused on the three geo-political zones in northern Nigeria. While the North-West and North-East zones are predominantly Hausa, Fulani, and Kanuri in ethnicity and are largely Islamic, the North-Central zone is a mix of several minority ethnic groups and has a slightly Christian majority. The 2018 Nigerian Demographic and Health Survey (NDHS) provided the data for this study. The NDHS is a nationally representative cross-sectional survey that draws samples from rural and urban areas of Nigeria based on the 2006 population and housing census frame (National Population Commission (NPC) and ICF International, 2014). A total of 41,821 women between the ages of 15 and 49 years were successfully interviewed in the 2018 NDHS. For this study, we restricted our analysis to a weighted sample size of 17,632 married women aged 15–49 years with at least one birth in the five years preceding the survey, and who by default, would require ANC and delivery care services, in the three northern geopolitical zones of Nigeria.
Variable measurement
Two outcome variables were employed as measures of maternal healthcare services in the study. These were Antenatal care (ANC) utilisation and place of delivery. In the women recode file of the NDHS, ANC utilisation was captured as ‘number of antenatal visits during pregnancy’ in variable (V) M14$1. Following the WHO recommendation of a minimum of four ANC visits (before it was revised to eight visits in late 2016), the numeric responses were recoded into a binary form of less than four (< 4) and at least four (4 +). Place of delivery (VM15$1) in the file had nine options for the respondents to choose from. The options were recoded to the binary form of health facility delivery and non-health facility delivery. Health facility delivery included either a public or private health facility.
The main explanatory variable of the study, IPV, was derived from questions in the NDHS that measured whether respondents had ever been emotionally abused, humiliated, insulted, pushed, slapped, kicked, dragged, tried to be strangled or forced into having sex etc., by their spouses. These were classified as emotional, physical and sexual violence in the NDHS. An experience of any of these was recoded as Yes to IPV while non-experience was recoded as No. Other explanatory variables employed in the study were age, level of education, husband’s education, place of residence, religion, wealth status, number of children ever born, family composition and media exposure. While family composition was derived from number of sons and daughters a woman has, media exposure was derived from the respondent’s access to radio and TV. The variables have all been found to have implications for the utilisation of maternal health care services, as highlighted in the introductory section.
Data analysis
Simple frequency analysis was used at the descriptive level to show the sociodemographic characteristics of the study population, their experience of IPV and their level of utilisation of maternal healthcare services. Chi Square test statistics were employed to show the association between experience of marital violence and the uptake of the selected maternal healthcare services, while binary logistic regression analysis was used to predict the relationship. At the descriptive level, each form of IPV was shown separately while the composite IPV variable, showing an experience of any of the forms, was used for the bivariate and multivariate analyses. The regression analysis was carried out at the unadjusted level and with the sociodemographic confounders of utilisation at the adjusted level. All analyses were carried out at the regional level (northern Nigeria) and across the zonal components (North-Central, North-East and North-West zones) to account for spatial variations in the relationships.
Results
Sociodemographic characteristics of study population
Of the 17,632 respondents, 28.0% were from the North-Central zone while 29.8% and 42.2% were from the North-East and North-West zones respectively. Respondents aged 25–39 (55.7%), who had no formal education (62.9%), whose husbands had no formal education (49.2%), who resided in rural areas (74.6%), practiced Islamic religion (78.2%), were from poor households (59.0%), had between one and four children (53.2%), had more sons (41.5%) and had media exposure (69.3%) constituted the majority in the sample. At the subregional level, they also constituted the majority except with respect to husband’s educational level and religion. More husbands (39.3%) in the North-Central zone had secondary education, while there were slightly more Christians (including Catholics) (50.5%) than adherents of Islam (49.1%) as shown in Table 1.
Emotional violence in the study area was more prevalent (35.8%) than physical violence (16.7%) and sexual violence (8.2%). The prevalence of emotional and physical violence was however higher than the regional average in both the North-Central and North-East zones. The North-West had the least prevalence of all forms of IPV as shown in Table 1. Slightly over 46% of the study population utilised ANC services at least four times whereas the utilisation of health facility for delivery was a mere 22.1% among the respondents. ANC utilisation (58.0%) and health facility delivery (38.0%) were however higher in the North-Central zone while they were lowest in the North-West geopolitical zone of northern Nigeria at 41.0% and 12.7% respectively.
Association between respondents’ sociodemographic characteristics and maternal healthcare services utilisation
The utilisation of ANC services, at least four times for their most recent birth preceding the survey, was more prevalent among respondents aged 25–39 (47.9%), urban residents (63.5%), with higher education (87.0%) and whose husbands had higher education (74.3%), Christians other than Catholics (66.0%), from rich households (72.4%), had between one and four children (49.6%) and had media exposure (47.9%) as shown in Table 2. The prevalence was uniform at around 46% among women with more sons, more daughters and those who had equal number of sons and daughters. The spatial comparison of the utilisation pattern among the zones shows that the patterns were similar across all the sociodemographic groups except for age. In the North-West zone, utilisation was highest among women aged 15–24 (42.1%). Among the total population and in the zones, health facility delivery also had a similar prevalence pattern as ANC utilisation except with age, religion and media exposure.
Across the different spatial units, respondents aged 15–24 had more health facility deliveries. While hospital delivery was more prevalent among Catholics in the general population (42.4%), in the North-Central (45.5%) and North-West (34.9%), it was highest among other Christians in the North-East (33.2%) as shown in Table 2. Hospital delivery was more prevalent among women with media exposure except in the North-West zone where the prevalence was 12.5% as against 13.1% among those who had no radio or TV. In the general population, women who had experienced IPV had a higher utilisation rate of ANC (49.2%) and health facility delivery (27.7%). In the zones, ANC utilisation was higher among women who had not experienced IPV only in the North-Central zone (58.7%). Health facility delivery was higher among women who experienced IPV in all the zones. With the exception of family composition across all spatial units, number of children and ANC in North-East, media exposure in North-Central, and media and place of delivery in North-West, all the associations were significant at P < 0.001.
Determinants of maternal healthcare services utilisation
In the unadjusted regression model, summarised in Table 3, women who experienced IPV were more likely to utilise ANC services at least four times (OR: 1.135, P < 0.05) and equally more likely to deliver in a health facility (OR: 1.407, P < 0.05). In the zones, the outcomes are different. In the North-Central zone, women who experienced IPV were less likely to have four ANC services, while in the North-East and North-West, they were more likely to use the services. In all the zones, women who experienced IPV were more likely to have hospital delivery, although the relationship was only statistically significant in the North-East (OR: 1.260, P < 0.05). When other sociodemographic confounders were controlled for in the regression model, only the relationship between women who experienced IPV and the use of a health facility for delivery remained statistically significant among the general population (OR: 1.212, P < 0.05). In the zones, and except for ANC utilisation in the North-Central, which had negative odds, the relationships were positive, albeit statistically insignificant.
In the general population, urban residence, education, religion, wealth status, and media exposure were statistically significant in predicting the utilisation of ANC services while age, number of children and family composition were not. Regarding hospital delivery however, all the predictors were statistically significant in their relationship with health facility delivery except family composition. In the North-Central zone, women aged 15–24 were less likely to use ANC services but were seven times more likely to have hospital delivery when compared with women aged 40–49. In the North-East and North-West zones, the likelihood of having hospital delivery was also higher among the 15–24 age group. Across the zones, urban residents were more likely to have hospital delivery when compared with rural women. The same pattern applied to ANC utilisation except in the North-East zone.
In the three zones, and relative to women who had higher education and whose husbands had higher education, women with no education, primary education and secondary education were less likely to use the two maternal healthcare services, the same as for women from poor and middle wealth classes relative to women from rich households. While media exposure, number of children and religion presented varying outcomes on their relationship with maternal healthcare services utilisation in the three zones, the most varied of the three was religion. Number of children was only significant (negative odds) in the North-East and North-West with respect to hospital delivery, while media exposure was associated with an increased likelihood of hospital delivery in the North-East and ANC utilisation in the North-West. Relative to Catholics, other Christians and Islamic faithful were less likely to have hospital delivery in the North-Central and North-West whereas other Christians were more likely to have hospital delivery in the North-East. They were also more likely to have the recommended ANC services only in the North-West.
Discussion
The paper analyses the determinants of maternal healthcare services utilisation in northern Nigeria with a focus on how this is impacted by the experience of intimate partner violence among parous married women in the region. Results show that ANC utilisation among the study population was more prevalent (46.4%) than the use of health facilities for delivery (22.1%). At the subregional level, ANC utilisation was highest in the North-Central zone (58.0%) and lowest in the North-West (41.0%). Women in the North-Central zone also had more health facility deliveries (38.0%) while the prevalence was lowest in the North-West zone (12.7%). When the utilisation rates are contextualised within the religious composition of the zones, the predominantly Islamic North-East and North-West had lower utilisation rates. Similarly, women in the North-East and North-West zones, and their husbands, were less educated and wealthy when compared with those in the North-Central zone. The women shared similar characteristics on other sociodemographic attributes across the region.
The experience of IPV was almost at par both in the North-Central and North-East zones. When this was decomposed into emotional, sexual and physical violence, the prevalence of sexual violence in the North-East zone was three and five times higher than in North-Central and North-West zones respectively. The North-West zone had the lowest prevalence of all forms of IPV. Overall, the prevalence of emotional violence was higher in all the zones, than physical and sexual violence. The findings on the prevalence of the three forms of IPV are similar with those from studies by Karakurt and Silver (2013) in America, and Sorbo et al (2013) in Norway. In their study of 36 countries, Leight and Wilson (2021) also found the prevalence of emotional violence higher than physical and sexual violence in Comoros, Cambodia, and most of the Latin America and West African countries studied.
Findings on the association between the uptake of maternal healthcare services and experience of IPV show that women who had experienced violence had higher utilisation rates of the services. At the bivariate level, the utilisation of ANC and health facility delivery services was higher among women who had experienced IPV at the regional and subregional levels. The only exception being ANC utilisation in the North-Central zone. At the unadjusted level of the regression models, women who experienced IPV were also more likely to use ANC and health facility delivery services in northern Nigeria. This result is in contrast with findings from previous studies that did not take the sociodemographic and cultural diversity of northern and southern Nigeria into consideration. Ononokpono and Azfredrick (2014), for instance, analysed the NDHS 2008 data for the whole of Nigeria and found that physical intimate partner violence (IPV) was associated with low antenatal care service utilisation. The authors also found that emotionally abused women were less likely to use health facility delivery services. In the same vein, and without disaggregating the Nigerian dataset into geographic regions, Onoh et al (2013) and Solanke (2014) found significantly less likelihood of utilisation of maternal health care services among women who experienced one form of IPV or the other.
The north–south diversity in Nigeria is exemplified in the level of education of the women, their wealth status, religion, and number of children ever born. From the 2018 NDHS, while Christianity was the dominant religion in the south, Islam was the dominant religion in the north. Women with no formal education in the three zones in southern Nigeria were less than 10%, whereas they constituted an average of 58% in the north. Women in the south were also richer than their counterparts from the north. All these are masked in pan-Nigerian studies and may have accounted for the different outcomes on the association between the uptake of maternal healthcare services and IPV. The results from this study also differ from the findings in most studies on the subject outside Nigeria, like those of Leight and Wilson (2021), Idriss-Wheeler and Yaya (2021), Mai and Phyu (2020), Musa et al (2019), Gashaw et al (2019), Maxwell et al (2018) who found that women who had experienced IPV were less likely to use maternal healthcare services.
Although, when the regression models were adjusted to confound for the sociodemographic characteristics of the women, the relationship became statistically insignificant with ANC utilisation but women who had experienced IPV still had higher odds of using health facilities for delivery. The departure from the general pattern as found in this study could be attributed to the socioeconomic profiles of the study population and, perhaps, the need for self-preservation by the abused women. In the former case, relative to women who had higher education, whose husbands had higher education, and from rich households, the respondents (in the respective sociodemographic categories) were less likely to use maternal healthcare services. This suggests that being educated and wealthy provide opportunities for knowledge, exposure and affordability of maternal healthcare services. Fapohunda and Orobaton (2014), Dahiru and Oche (2015), Kifle et al (2018), Yahya and Pumpaibool (2019) and Okedo-Alex et al (2019) have also shown how these factors were positively linked with higher odds of maternal healthcare services utilisation.
In the latter case of self-preservation, the higher odds of utilisation among women who had experienced IPV might be as a result of the women taking precautions to safeguard theirs and their unborn babies’ health as a result of the violence they were exposed to. Women who experienced violence while pregnant might resort to visiting health facilities to check on their status and, in the process, become more committed to their physicians’ recommendations to safeguard their pregnancies and health as described in the theories of obedience (Milgram, 1963; Stimson, 1967). At the subregional level, education, wealth, place of residence, as well as religion may have also accounted for the variation in the relationship between IPV and the uptake of maternal healthcare services.
In the unadjusted model, women who experienced IPV in the North-Central were less likely to use ANC services whereas those in the North-West were more likely to use them. While the relationship between the experience of IPV and the use of heath facility for delivery was not significant in both the North-Central and North-West zones, women in the North-East who experienced IPV were more likely to use health facilities for delivery. More women in the North-West (75.2%) had no formal education when compared with other zones, just as the North-East had the highest proportion of poor women (68.7%). The North-East also had the highest proportion of rural dwellers in the study area. As shown by Adewoyin (2021), the utilisation of healthcare facilities is higher in rural areas of Africa despite the low provision of healthcare facilities in the area. This implies that, although urban centres have more facilities, utilisation (relative to availability) is higher in rural areas where the facilities are fewer. Rural dwellers, particularly those with access to radio, take government broadcast (on health) more seriously than urban dwellers who have various other forms of socialisation and are exposed to myriad media information that is sometimes conflicting (Adewoyin, 2021; Adewoyin et al., 2022a, 2002b). In the prevailing context, nearly 80% of the North-East sample lived in rural areas and had media access.
Islam was the dominant religion in the North-East and North-West, while it was Christianity in the North-Central zone. In the regression model, relative to Catholics, women who practiced Islam and other Christian denominations were less likely to use ANC and health facility delivery services in the North-Central zone, whereas being other Christian increased the odds in the predominantly Islamic North-West and North-East. Islamic religion was associated with lower odds in both zones. In other words, Islamic religion was largely associated with lower odds of maternal healthcare services utilisation in the region. The findings are similar to those from Solanke et al (2015), Umar (2017), Ene et al (2019) and Odimegwu and Adewoyin (2020) on the place of religion in the utilisation of maternal healthcare and reproductive healthcare services. In Northern Nigeria, religion is a very sensitive topic. Most government programmes or policies for health improvement are usually resisted on the premise that such policies are for population control and are therefore against Islamic religious teachings (Adegbola, 2008; Ghinai et al., 2013; Olufowote, 2011; Yahya, 2007.).
Expectedly, and as established in most studies (Adewoyin, 2021; Dahiru & Oche, 2015; Leight & Wilson, 2021; Okedo-Alex et al, 2019; Ononokpono et al, 2013), media exposure was also found to be associated with increased odds of using maternal healthcare services in this study. Having access to radio and television broadcasts on health promotes informed health choices, including seeking healthcare services.
Conclusions
The uptake of maternal healthcare services is poor in northern Nigeria. As shown in this study however, the low uptake is not as a result of the prevalence of marital violence. Rather, and contrary to the overarching hypothesis of this study, this study has shown that women who experienced any of physical, sexual or emotional violence in their union had a higher uptake of maternal healthcare services in the study area. This finding and the association between the socioeconomic characteristics of the study population and their uptake of maternal healthcare services suggest that attention be paid to the educational and wealth statuses of the population because of their positive contribution to the higher uptake of MHS recorded. The role of religion as a major driver of the low uptake of maternal healthcare services should also constitute policy issues for improving maternal health services utilisation in northern Nigeria.
Data availability
The study utilized secondary data in the public domain.
References
Abimbola, J. M., Makanjuola, A. T., Ganiyu, S. A., Babatunde, U. M. M., Adekunle, D. K., & Olatayo, A. A. (2016). Pattern of utilisation of ante-natal and delivery services in a semi-urban community of North-Central Nigeria. African Health Sciences, 16(4), 962–971.
Abubakar, S., Adamu, D., Hamza, R., & Galadima, J. B. (2017). Determinants of home delivery among women attending antenatal care in Bagwai Town, Kano Nigeria. African Journal of Reproductive Health, 21(4), 73–79.
Adebowale, A. S., & Akinyemi, O. J. (2016). Determinants of maternal utilisation of health services and nutritional status in a rural community in SW Nigeria. African Journal of Reproductive Health, 20(2), 72–85.
Adedini, S. A., Somefun, O. D., & Odimegwu, C. (2014). Gender inequality and maternal and child healthcare utilisation in sub-Saharan Africa. Gender and Behaviour, 12(4), 6050–6070.
Adegbola, O. (2008). Population Policy Implementation in Nigeria, 1988–2003. Population Review, 47(1), 56–110.
Adewoyin, Y. (2021). Maternal Healthcare, Place Differentials and Regional Planning in Africa. In Adewoyin, Y., Adeagbo, A., Ogunkan, D. and Chakwizira, J. (eds). Contemporary Issues in Urban and Regional Planning and Development in Africa: A Festschrift in Honour of Professor Aina Thompson Adeboyejo. Ibadan: Ladoke Akintola University of Technology. ISBN: 978–978–31064 2 7
Adewoyin, Y., Awelewa, O. F., Uzoma, I. E., & Anazonwu, N. P. (2020). Prevalence pattern and sociodemographic correlates of single motherhood in Nigeria. Sexuality Research and Social Policy. https://doi.org/10.1007/s13178-020-00523-0
Adewoyin, Y., Nwosu, I. J., Ossai, O. G., & Onuh, J. C. (2022). Rural-Urban Differentials in Levels and Determinants of Financial Inclusion among Nigerian Women. Journal of Population and Social Studies, 30(2022), 448–462. https://doi.org/10.25133/JPSSv302022.026
Adewoyin, Y., Odimegwu, C. O., Bassey, T. I., Awelewa, O. F., & Akintan, O. (2022). National and Subnational Variations in Gender Relations and the Utilisation of Maternal Healthcare Services in Nigeria. Pan African Medical Journal, 42, 28. https://doi.org/10.11604/pamj.2022.42.28.25689
Adewuyi, E. O., Auta, A., Khanal, V., Bamidele, O. D., Akuoko, C. P., Adefemi, K., Tapshak, S. J., & Zhao, Y. (2018). Prevalence and factors associated with underutilisation of antenatal care services in Nigeria: A comparative study of rural and urban residences based on 2013 Nigeria demographic and health survey. PLoS ONE, 13(5), e0197324.
Agan, T. U., Monjok, E., Akpan, U. B., Omoronyia, O. E., & Ekabua, J. E. (2018). Trend and causes of maternal mortality in a Nigerian Tertiary Hospital: A 5-year retrospective study (2010–2014) at the University of Calabar Teaching Hospital, Calabar, Nigeria. Open Access Macedonian Journal of Medical Sciences, 6(6), 1153–1158.
Akinlo, A., Idemusia, E. S., Ogunjuyigbe, P. O., & Solanke, P. S. (2016). Women’s empowerment status and exposure to maternal mortality risks in Nigeria. Gender and Behaviour, 14(1), 7085–7099.
Alabi, O., Doctor, H. V., Afenyadu, G. Y., & Findley, S. E. (2014). Lessons learned from setting up the Nahuche Health and Demographic Surveillance System in the resource-constrained context of northern Nigeria. Global Health Action, 7(1), 23368.
Antai, D. (2011). Traumatic physical health consequences of intimate partner violence against women: What is the role of community-level factors? BMC Women’s Health, 11, 56.
Anyebe, E., Lawal, H., Dodo, R., & Adeniyi, B. (2017). Community Perception of Single Parenting in Zaria, Northern Nigeria. Journal of Nursing Care, 6(411).
Barman, B., Saha, J., & Chouhan, P. (2018). Impact of education on the utilisation of maternal health care services: An investigation from National Family Health Survey (2015–16). Children and Youth Services Review, 2020, 1018.
Dahiru, T. & Oche, O.M. (2015). Determinants of antenatal care, institutional delivery and postnatal care services utilisation in Nigeria. Pan African Medical Journal, 21(321).
Doctor, H. V., Findley, S. E., & Afenyadu, G. Y. (2012). Estimating maternal mortality level in rural northern Nigeria by the sisterhood method. International Journal of Population Research, 2012, 5.
Ene, J. C., Adewoyin, Y., & Chukwu, N. A. (2019). Patterns and Determinants of Contraceptives Utilisation in a Religiously Homogeneous Settlement: A Nigerian Case Study. Research Journal of Health Sciences, 7(3), 217–226.
Fapohunda, B., & Orobaton, N. (2014). Factors influencing the selection of delivery with no one present in Northern Nigeria. Implications for policy and programs. International Journal of Women’s Health., 6, 171–183.
Gashaw, B. T., Magnus, J. H., & Schei, B. (2019). Intimate partner violence and late entry into antenatal care in Ethiopia. Women and Birth, 2019, e530–e537.
Ghinai, I., Willott, C., Dadari, I., & Larson, H. J. (2013). Listening to the Rumours: What the Northern Nigeria Polio Vaccine Boycott Can Tell Us Ten Years On. Global Public Health, 8(10), 1138–1150.
Haruna-Ogun, O. A. (2018). Geographical differentials in uptake of antenatal care services in Nigeria. Health Care for Women International, 39(1), 34–49.
Idriss-Wheeler, D. and Yaya, S. (2021). Exploring antenatal care utilization and intimate partner violence in Benin - are lives at stake? BMC Public Health 21, 830. https://doi.org/10.1186/s12889-021-10884-9
Kabir, R. (2018). Impact of intimate partner violence on ever-married women and utilisation of antenatal care services in Tanzania. Revue D’epidemiologie Et De Sante Publique, 66, S376. https://doi.org/10.1016/j.respe.2018.05.377
Karakurt, G., & Silver, K. E. (2013). Emotional abuse in intimate relationships: The role of gender and age. Violence and Victims, 28(5), 804.
Kifle, M. M., Kesete, H. F., Gaim, H. T., Angosom, G. S., & Araya, M. B. (2018). Health Facility or home delivery? Factors influencing the choice of delivery place among mothers living in rural communities in Eritrea. Journal of Health, Population and Nutrition, 37, 22.
Leight, J., & Wilson, N. (2021). Intimate partner violence and maternal health services utilisation: Evidence from 36 National Household Surveys. BMC Public Health, 21, 405. https://doi.org/10.1186/s12889-021-10447-y
Mai, V., & Phyu, W. E. (2020). Intimate partner violence and utilisation of reproductive and maternal health services in Cambodia. Journal of Health Research, 34(2), 100–111.
Maxwell, L., Brahmbhatt, H., Ndyanabo, A., Wagman, J., Gertrude, N., Jay, S. K., Fred, N., David, S., & Arijit, N. (2018). The impact of intimate partner violence on women’s contraceptive use: evidence from the Rakai community cohort study in Rakai, Uganda. Social Science & Medicine, 209, 25–32.
McNabb, M., Chukwu, E., Ojo, O., Shekhar, N., Gill, C. J., Salami, H., & Jega, F. (2015). Assessment of the quality of antenatal care services provided by health workers using a mobile phone decision support application in Northern Nigeria: A pre/post-intervention study. PLoS, 10(5), e0123940.
Meh, C., Thind, A., Ryan, B., & Terry, A. (2019). Levels and determinants of maternal mortality in northern and southern Nigeria. BMC Pregnancy and Childbirth, 19(417).
Melah, G., El-Nafaty, A., Massa, A., & Audu, B. (2003). Obstructed labour: A public health problem in Gombe, Gombe State, Nigeria. Journal of Obstetrics and Gynaecology, 23(4), 369–373.
Milgram, S. (1963). Behavioural study of obedience. The Journal of Abnormal and Social Psychology, 67(4), 371–378.
Musa, A., Chojenta, C., Geleto, A., & Loxton, D. (2019). The associations between intimate partner violence and maternal health care service utilization: A systematic review and meta-analysis. BMC Women’s Health, 19(1), 1–14.
National Population Commission (NPC) [Nigeria] and ICF International (2014). Nigeria Demographic and Health Survey 2013. Abuja, Nigeria, and Rockville, Maryland, USA: NPC and ICF International.
National Population Commission (NPC) [Nigeria] and ICF (2019). Nigeria Demographic and Health Survey 2018. Abuja, Nigeria, and Rockville, Maryland, USA: NPC and ICF.
Odimegwu, C. O., & Adewoyin, Y. (2020). Latent and under-explored determinants of contraceptive use in Nigeria. Sexuality Research and Social Policy. https://doi.org/10.1007/s13178-020-00495-1
Okedo-Alex, I. N., Akamike, I. C., Ezeanosike, O. B., et al. (2019). Determinants of antenatal care utilisation in sub-Saharan Africa: A systematic review. British Medical Journal Open, 2019(9), e031890. https://doi.org/10.1136/bmjopen-2019-031890
Okemgbo, C. N., Omideyi, A. K., & Odimegwu, C. O. (2002). Prevalence, patterns and correlates of domestic violence in selected Igbo communities of Imo State, Nigeria. African Journal of Reproductive Health, 6(2), 101–114.
Olufowote, J. O. (2011). Local resistance to the global eradication of polio: newspaper coverage of the 2003–2004 vaccination stoppage in northern Nigeria. Health Communication, 26(8), 743–753.
Onoh, R., Umeora, O., Ezeonu, P., Onyebuchi, A., Lawani, O., & Agwu, U. (2013). Prevalence, pattern and consequences of intimate partner violence during pregnancy at Abakaliki southeast Nigeria. Annals of Medical and Health Sciences Research, 3(4), 484–491.
Ononokpono, D. N., & Azfredrick, E. C. (2014). Intimate partner violence and the utilisation of maternal health care services in Nigeria. Health Care for Women International, 35(7–9), 973–989.
Ononokpono, D. N., Odimegwu, C. O., Imasiku, E. N. S., & Adedini, S. A. (2013). Contextual determinants of maternal health care service utilisation in Nigeria. Women and Health, 53(7), 647–668.
Oyediran, K. A. & Feyisetan, B. (2017). Prevalence and contextual determinants of intimate partner violence in Nigeria. African Population Studies, 31(1).
Solanke, B. L. (2014). Association between intimate partner violence and utilisation of maternal health services in Nigeria. Etude De La Population Africaine, 28(2), 933.
Solanke, B. L., Oladosu, O. A., Akinto, A., & Olanisebe, S. O. (2015). Religion as a social determinant of maternal health care service utilisation in Nigeria. African population Studies, 29(2)
Solivetti, L. M. (1994). Family, marriage and divorce in a Hausa community: a sociological model. Africa: Journal of the International Institute of African Languages and Cultures, 64(2), 252–271.
Sorbo, M. F., Grimstad, H., Bjørngaard, J. H., Schei, B., & Lukasse, M. (2013). Prevalence of sexual, physical and emotional abuse in the Norwegian mother and child cohort study. BMC Public Health, 13(1), 186.
Stimson, G. V. (1967). Obeying doctor’s orders: A view from the other side. Social Science and Medicine, 8(2), 97–104.
Umar, A. S. (2017). The use of maternal health services in Nigeria: Does ethnic and religious beliefs matter? MOJ Public Health, 6(6), 442–447.
United Nations Women (2019). Progress of the world’s women 2019-2020 – Families in a Changing World. New York, United Nations
UNICEF (2020). Maternal and Newborn Health Coverage Database, August 2020.
World Health Organization (2016). Violence against Women: Intimate Partner and Sexual Violence against Women. Fact sheet 2016.
World Health Organization (2013). Global and regional estimates of violence against women: prevalence and health effects of intimate partner violence and non-partner sexual violence. Geneva: World Health Organization
World Health Organization (2019). Newborns: Reducing Mortality. Available from: www.who.int/news-room/fact-sheets/detail/newborns-reducing-mortality
Yahya, M. (2007). Polio vaccines – ‘No Thank You!’ barriers to polio eradication in northern Nigeria. African Affairs, 106(423), 185–204.
Yahya, M. B., & Pumpaibool, T. (2019). Factors influencing the decision to choose a birth centre by pregnant women in Gombe State, Nigeria: Baseline survey. Journal of Health Research, 33(3), 228–237.
Yaya, S., Gunawardena, N., & Bishwaji, G. (2019). Association between intimate partner violence and utilisation of facility delivery services in Nigeria: A propensity score matching analysis. BMC Public Health, 2019(19), 1131. https://doi.org/10.1186/s12889-019-7470-1
Acknowledgements
The authors appreciate the DHS program and the National Population Commission of Nigeria for granting access to the Nigeria DHS data.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors declare that they have no conflict of interests.
Ethical approval
Relevant ethical clearance for the survey was sought and obtained by the DHS project from the National Health Research Ethics Committee (NHREC) in Nigeria before the surveys were conducted.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Adewoyin, Y., Odimegwu, C.O., Alabi, O. et al. Intimate partner violence and the spatial pattern of maternal healthcare services utilization among parous married women in northern Nigeria. J Pop Research 39, 617–636 (2022). https://doi.org/10.1007/s12546-022-09293-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12546-022-09293-5