Abstract
Background
Congenital heart disease (CHD) is one of the main supportive diseases of extracorporeal membrane oxygenation in children. The management of extracorporeal membrane oxygenation (ECMO) for pediatric CHD faces more severe challenges due to the complex anatomical structure of the heart, special pathophysiology, perioperative complications and various concomitant malformations. The survival rate of ECMO for CHD was significantly lower than other classifications of diseases according to the Extracorporeal Life Support Organization database. This expert consensus aims to improve the survival rate and reduce the morbidity of this patient population by standardizing the clinical strategy.
Methods
The editing group of this consensus gathered 11 well-known experts in pediatric cardiac surgery and ECMO field in China to develop clinical recommendations formulated on the basis of existing evidences and expert opinions.
Results
The primary concern of ECMO management in the perioperative period of CHD are patient selection, cannulation strategy, pump flow/ventilator parameters/vasoactive drug dosage setting, anticoagulation management, residual lesion screening, fluid and wound management and weaning or transition strategy. Prevention and treatment of complications of bleeding, thromboembolism and brain injury are emphatically discussed here. Special conditions of ECMO management related to the cardiovascular anatomy, haemodynamics and the surgical procedures of common complex CHD should be considered.
Conclusions
The consensus could provide a reference for patient selection, management and risk identification of perioperative ECMO in children with CHD.
Video abstract (MP4 104726 kb)
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Until the 1970s, extracorporeal membrane oxygenation (ECMO) was reported to be successfully used in a neonate with acute respiratory failure [1]. Since the 1980s, the number of cardiac ECMO cases has increased dramatically, though neonatal respiratory failure remains to be the most common indication for ECMO support [2]. ECMO is used for respiratory support, circulatory support and cardiopulmonary resuscitation (CPR) in pediatrics. The most common neonatal diagnosis requiring respiratory ECLS (extracorporeal life support) was congenital diaphragmatic hernia (32%), followed by meconium aspiration syndrome (24%) and persistent pulmonary hypertension (21%) [3]. The most common disease requiring circulatory ECLS is congenital heart disease (CHD), 80% in newborns and 52% in children [3].
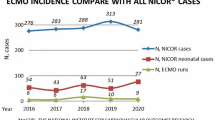
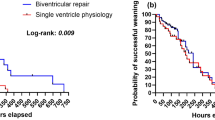
Veno-arterial ECMO (VA ECMO) is the main support mode for CHD. According to the data from Extracorporeal Life Support Organization (ELSO) registry, a total of 19,629 cases with CHD from 350 international centers worldwide from 1990 to 2019 have been supported by ECMO [4]. Among them, the most common condition was hypoplastic left heart syndrome (HLHS) in neonates, whereas in children conditions requiring complex biventricular repair (such as tetralogy of Fallot, double outlet of right ventricle, Ebstein's anomaly of the tricuspid valve) were the most common [4]. The median ECMO running duration for of pediatric cardiac diseases was 6–7 days, and the survival rate was 46%–55%, which was significantly lower than other classifications of diseases [4].
In China, ECMO was reported to be successfully used in a neonate with CHD in 2008 [5]. A total of 10,946 patients with CHD underwent cardiopumonary bypass from January 2017 to June 2020, ECMO cases accounted for 1.21% and a survival rate was 47% [6]. In 2021, ECMO was used for respiratory support in 126 children and for circulatory support in 422 children with a survival rate of 59.5% [7]. A total of 127 children underwent external cardiopulmonary resuscitation (ECRP) support with a survival rate 39.4%, and among them 10 were newborns with a survival rate of 8.3%. A total of 65 newborns with CHD underwent ECMO with a survival rate of 43.1% [7].
ECMO support after arterial switch operations (ASOs) accounted for 21.2% of total ECMO cases with CHD [8]. Children with CHD have more challenges due to complex heart anatomical structure, special pathophysiology, perioperative complications and various concomitant malformations. This consensus focused on the technical approach of ECMO support in pediatric CHD. Recommendations on patient selection, management and risk identification of perioperative ECMO support in pediatric CHD were provided.
Patient selection criteria
Indications
Most neonatal cardiac ECMO occurs during the perioperative period and particularly the post-procedure period [9]. Perioperative ECMO in children with CHD is used to stabilize and recover the respiratory and circulatory function. ECMO may also be used for recovery from the primary disease and providing time for follow-up diagnosis and treatment and for awaiting other therapeutic modalities, such as ventricular-assist device (VAD) or transplantation in the following situations: (1) pre-procedural patients with severe hypoxemia and low cardiac output syndrome (LCOS): patients with total anomalous pulmonary venous connection and transposition of the great arteries (TGA) may present with severe hypoxia, acidosis and LCOS due to insufficient oxygenation of blood and persistent pulmonary hypertension; (2) failure to wean off cardiopulmonary bypass (CPB): ECMO support may be required for patients who fail to wean off CPB after cardiac surgery for improper myocardial protection, myocardial ischemia injury or residual anatomical deformity; (3) severe postoperative LCOS: LCOS occurs due to myocardial damage or stunning, coronary ischemia, malignant arrhythmia, residual lesions and sudden obstruction of the postoperative systemic-pulmonary shunt; (4) cardiac arrest due to a variant of causes.
ECMO should be initiated as early as possible if with the following indications [10,11,12,13,14,15,16]: (1) cardiac index < 2 L/m2/minute; (2) persistent tissue hypoperfusion: blood pH < 7.15, BE < -5 mmol/L, lactate > 7.3 mmol/L, urine output < 1 mL/kg/hour, capillary refill time > 3 seconds, central venous oxygen saturation (SVO2) < 60% or arteriovenous oxygen saturation difference (AVO2) > 30% for cyanotic CHDs; (3) persistent hypotension: the blood pressure is two standard deviations lower than that of normal blood pressure at the same age, such as for systolic blood pressure < 50 mmHg (neonates), < 60 mmHg (infants) and < 70 mmHg (children); (4) patients presenting with low blood pressure under two or more high-dose inotropes and/or vasopressors, such as epinephrine > 0.3 µg/kg/minute, dopamine > 10 µg/kg/minute, etc., or vasoactive–inotropic score is over 20 for two or more times and keeps increasing; (5) severe respiratory failure: severe hypoxia or respiratory acidosis persists even after conventional aggressive treatment, such as pH < 7.1, partial pressure of oxygen/fraction of inspired oxygen (PaO2/FiO2) < 60–80 mmHg or oxygenation index > 40, lasting 3–6 hours; (6) malignant arrhythmias: ECMO should be considered when severe arrhythmias, such as ventricular fibrillation, cardiac arrest or pulseless electrical activity and short bursts of ventricular tachycardia occur repeatedly and cannot be terminated by antiarrhythmic drugs, inotropes or temporary cardiac pacemakers. Consideration for early initiation of ECMO is important as delayed initiation (beyond 6 hours of cardiogenic shock state) is associated with worse outcomes.
Contraindications
ECMO should not be used under the following conditions [10]: (1) prolonged cardiogenic shock state (more than 6 hours) complicated with irreversible multiple organ failure; (2) premature or low birth weight neonates (< 34 weeks of gestational age or weight < 2.0 kg); (3) severe chromosomal abnormalities; (4) irreversible brain injury or intracranial hemorrhage (grade III or IV intraventricular hemorrhage); (5) uncontrolled bleeding (unless ECMO cannulation can help to control bleeding).
Cannulation strategy
VA ECMO was the most commonly used mode for most congenital heart diseases perioperatively. Cannulation site and strategy were determined by the patient’s body size, underlying cardiac anatomy and different surgical procedures for CHD. The commonly used cannulation strategy is listed in Table 1. Central cannulation is commonly used in failure to wean from CPB or in the presence of recent sternotomy (less than 10–14 days). The right neck or femoral vessels can be considered as the peripheral cannulation site. Most commonly, the right internal jugular vein and carotid artery configuration is used in younger patients (weight < 30 kg), while the femoral vein and femoral artery configuration is used in older patients (weight > 30 kg) [10]. Each ECMO center selects a peripheral cannulation site based on technique preference with reference to the patient’s weight range.
Peripheral vessel cannulation requires usually open surgical access [10]. The tip of the arterial cannula is located at the junction of the innominate artery and the aortic arch, preventing access to the ascending aorta. The tip of the venous cannula is located at the right atrium, preventing access to the right ventricle or hepatic vein. Single-ventricle patients with ductal- or shunt-dependent pulmonary blood flow may require excessive ECMO flow rates to accommodate the runoff into the pulmonary vascular bed and to provide adequate systemic tissue oxygen delivery. When a high volume of flow can be difficult to achieve from peripheral cannulation, central cannulation may be necessary [2]. When patients following the Glenn or Fontan procedure require VA ECMO, venous drainage cannulas may be possible in both the superior and inferior vena cava to achieve adequate vein drainage [17].
ECMO pump flow, ventilator parameters and vasoactive drug dosage setting
During ECMO, mixed venous oxygen saturation (SVO2) should be continuously monitored. The cardiac index should be maintained at 2.5–3 L/minute/m2 and the ratio of oxygen delivery (DO2) to oxygen consumption (VO2) should be set at least > 3:1 by adjusting pump flow and hemoglobin level [10]. Reasonable ventilator parameters and vasoactive drugs help to restore cardiac function and maintain perfusion of the organs and peripheral microcirculation (Table 2).
During the initial period, higher blood flow is required for early oxygen debt repayment, typically 100–150 mL/kg/minute in neonates and 80–120 mL/kg/minute in children [10, 18]. Pulmonary blood flow is reduced during VA ECMO, so the ventilation volume should be reduced proportionally [19]. Protective lung ventilation strategies with low parameter settings, including setting positive end-expiratory pressure (PEEP) 8–10 cm H2O and tidal volume < 6–8 mL/kg, peak inspiratory pressure < 18–20 cm H2O and frequency 10–15 times/minute can be utilized to reduce pulmonary complications [13, 19, 20]. High PEEP increases intra-thoracic pressure, pulmonary vascular resistance and right ventricular afterload, which adversely affect children with predominant right heart failure [21]. Conversely, children with predominant left heart failure often benefit from a high PEEP [19]. High pump flow will increase left ventricular afterload and myocardial performance after ECMO implantation; vasopressors should be reduced or discontinued as soon as possible and vasodilators administered to reduce afterload, to promote recovery of myocardium and microcirculation perfusion and to avoid important organ and extremity complications. Maintenance of normal rhythm with drugs or pacemakers improves ventricular emptying. In children with severe right heart failure and pulmonary hypertension, inhaled nitric oxide and/or targeted pulmonary arterial vasodilators can be used to reduce right heart afterload [13]. It is necessary to precisely regulate fluid balance, ventilator parameters and ECMO pump flow after ASO and anomalous left coronary artery origin from pulmonary artery (ALCAPA) repair. The regulation strategy should be tailored to improve the left ventricle adaptability to preload and afterload and avoid left ventricular distension. For children with HLHS, low pulmonary vascular resistance may lead to reduced systemic circulation and hypotension, whereas excessive pulmonary vascular resistance may lead to hypoxia. Children with B-T shunts or aortopulmonary collateral arteries require higher blood flow (150–200 mL/kg/minute) to accommodate the runoff into the pulmonary vascular bed [4, 22]. Additionally, when the flow of the shunt or the collateral artery is too great, the shunt or the collateral artery needs to be partially clamped or blocked.
Anticoagulation management
Bleeding is a common complication of ECMO for post-cardiac surgery patients, most frequently in central cannulation [23].The main causes of bleeding are the immature coagulation function of neonates and infants, the dilution of coagulation factors after connection to the ECMO circuit, the large open wound and the coagulopathy usually associated with a long duration of CPB. The main methods to reduce bleeding include reversing partial heparin with limited protamine administration [24], strict surgical hemostasis, and correcting coagulopathy and thrombocytopenia by infusing fibrinogen, fresh frozen plasma and platelets. If excessive bleeding occurs, particularly in post-cardiotomy patients, delayed infusion of unfractionated heparin (UFH) persistently for 4–6 hours is required. Under some circumstances where bleeding is difficult to control, UFH may be held up for 12 hours or longer until bleeding is controlled [25]. Delayed initiation of anticoagulation will increase the risk of circuit clots, which will increase the consumption of fibrinogen and platelet. UFH is currently the most commonly used anticoagulant for ECMO. The effectiveness of heparin can usually be monitored using activated clotting time (ACT) and activated partial thromboplastin time (APTT) combined with anti-Xa, thromboelastometry (ROTEM) and thromboelastography (TEG) [17]. ROTEM or TEG is currently recommended to guide the administration of blood products and coagulation factors in the presence of bleeding [26].
A bolus dose of UFH ranging from 50 to100 units/kg is given after the exposure of the vessels and before insertion of the cannulas for ECMO. Patients with severe coagulopathy, or active bleeding can receive a UFH bolus at the lower end of this range. Nevertheless, in the immediate postoperative transferring from CPB, bolus dosing of UFH may not be necessary [27]. UFH can be commenced when ACT reaches 300 seconds [18] and chest tube drainage is < 3 mL/kg/hour for 2 hours [28]. Some ECMO centers set maintenance dose of UFH infusion rate ranging from a minimum of 10–15 units/kg/hour to a maximum of 40–60 units/kg/hour [18]. The targeted ACT 180–220 seconds and APTT 1.5 and 2.5 times normal are needed. Targeted ACT value can be lowered to 160–180 seconds when there is a tendency to bleed. Blood production can be given to maintain platelet counts ≥ 100 × 109/L (bleeding patient) or ≥ 50–100 × 10 9/L (nonbleeding patient), fibrinogen > 1.5 g/L (bleeding patient or before surgical intervention) or > 1 g/L (nonbleeding patient). If a maximum dose of UFH cannot achieve the targeted ACT value, fresh frozen plasma could be infused to maintain antithrombin activity at > 50%–80% or 0.5–0.8 U/mL [25].
Direct thrombin inhibitors (DTIs) have been used in both adult and pediatric patients with heparin-induced thrombocytopenia (HIT), heparin resistance and non-HIT thrombocytopenia [29, 30]. The two DTIs most commonly used in ECMO are bivalirudin and argatroban. APTT is currently the standard test for monitoring DTIs (target 50–60 seconds), and the reported maintenance dose of bivalirudin and argatroban ranges from 0.045 to 0.48 mg/kg/hour and 0.1 to 0.7 μg/kg/minute, respectively [18]. Currently, experiences of using DTIs are lacking in pediatric ECMO in China, and clinicians should be aware of the safety and efficacy of DTIs.
Left ventricle decompression
When severe left ventricle (LV) dysfunction is supported with VA ECMO, continuous flow increases the pressure of the aortic root and LV afterload [31, 32]. Poor LV decompression may result in a persistently closed aortic valve, dilatation of the left heart, increased LV end-diastolic pressure, reduced sub-endothelial perfusion causing myocardial ischemia and poor LV function recovery, and a risk of LV stasis and consequent clot formation [33, 34]. It is important to recognize poor LV decompression early and to perform effective LV decompression.
After cardiac tamponade was excluded, the implications of poor LV decompression were reduced arterial pulse pressure (< 10 mmHg), increased pulmonary capillary wedge pressure (PCWP) or left atrium (LA) pressure (> 20 mmHg), pulmonary edema, closed aortic valve, increased LA or LV end-diastolic diameter and aggravated mitral valve regurgitation [35].
Conservative decompression was the first-line strategy: (1) titrate the ECMO flow [35] and use a vasodilator to decrease LV afterload; (2) increase inotrope to improve LV output; and (3) increase PEEP to decrease LV preload [35]. If conservative methods do not work effectively, invasive strategies can be utilized: (1) LA venting via the right-upper pulmonary vein or left atrial appendage (most commonly in post-cardiac surgery); (2) balloon atrial septostomy or blade atrial septostomy to allow left-to-right shunting [35, 36]; (3) a venting cannula via the LV apex or pulmonary artery [37, 38]; and (4) intra-aortic balloon pump or a percutaneous LV-to-aorta ventricular-assist device, such as impella, could be used in adolescents or young adults [2, 35, 39].
Residual lesions
Postoperative residual lesions of CHD can significantly increase the risk of postoperative complications and mortality rate [40]. Therefore, transesophageal echocardiography during the operation to detect residual lesions and timely intervention are conducive to the smooth withdrawal of CPB [41,42,43]. If there is no sign of myocardial function recovery after 48–72 hours of ECMO support, it is necessary to positively identify residual anatomical malformation. Identifying residual lesions and intervening during the first three days of ECMO support can significantly shorten support duration and improve the survival rate of patients [40, 41].
Common residual lesions include residual ventricular septal defects, stenosis and dysplasia of the pulmonary artery branch, stenosis of the left and right ventricular outflow tracts, pulmonary vein stenosis, B-T/Sano duct stenosis or too great, severe valvular regurgitation, bulky pulmonary collateral and coronary artery disease [41, 42]. In the early stage of support, residual lesion can present as ventricular dilatation and dyskinesia, insufficient systemic perfusion caused by excessive shunt, suboptimal blood lactate decrease, pulmonary hemorrhage, aberrant increase in mixed SvO2, etc. Children with a single ventricle may have insidious manifestations and may not present a significant increase in the left atrial or central venous pressure until the auxiliary flow is reduced to 30%–40%.
The first option for examination to identify residual anatomical malformation is ultrasound [41, 42]. When processing the examination, we can reduce the flow of ECMO or clamp the circuit temporarily to evaluate the cardiac function more accurately and identify residual lesions. Many factors, such as wound dressings, opened sternum, various cannulations and inappropriate size of ultrasound probe, can affect the acquisition of standard ultrasound views. If necessary, further examinations, such as cardiac catheterization or computed tomography angiography (CTA), can be recommended [43,44,45].
Fluid management and renal replacement therapy
Children with VA ECMO during the perioperative period of CHD need appropriate fluid to maintain cardiac output and ECMO flow. Dynamic monitoring of central venous pressure (CVP), PCWP, pre-pump pressure of circuit and other comprehensive evaluations of volume status are crucial. During the early period of ECMO support, bleeding, insensible fluid loss or capillary leakage syndrome may be attributed to insufficient ECMO flow. When the pre-pump pressure of ECMO becomes more negative (below -40 to -30 mmHg), the venous line vibrates or the inferior vena cava collapses [46] and colloids and low dose of vasoactive drugs can be given firstly to maintain the intravascular volume. Once the circulation of children is stable and capillary leakage is improved, fluid intake should be limited and negative fluid balance is warranted to avoid fluid overload. Renal replacement therapy should be actively applied in case of intravascular fluid overload, oliguria or refractory to diuretics and albumin, elevated creatinine and electrolyte disorder [10, 47].
About 49%–59% of children on ECMO with CHD developing acute kidney injury (AKI) and fluid overload require renal replacement therapy (RRT) [48, 49]. Low cardiac output, hypotension, venous congestion, non-pulsatile perfusion, inflammatory reaction and hemolysis may cause AKI [50] and fluid overload, prolonging ECMO supporting time and increasing mortality [51,52,53,54]. The commonly used RRT models in children are continuous renal replacement therapy (CRRT) [50] and peritoneal dialysis (PD). Although some researchers reported no improvements in the survival rate by utilizing ECMO with CRRT and no high-level evidence or guidelines support routine usage of CRRT during ECMO, some researchers discovered that the combination of ECMO and CRRT may be effective [51, 55, 56].
To avoid serious air embolism, we recommend the input and output interfaces of CRRT be connected to the post-pump part of the ECMO circuit (Fig. 1). Parallel connection with the CRRT circuit will increase the turbulence and coagulation risk of ECMO circuit interface, with the need for close monitoring for hemolysis, bleeding and coagulation [50]. If the patient has undergone CRRT before ECMO support, the original CRRT catheter is recommended to be continued. According to the KDIGO (Kidney Disease: Improving Global Outcomes) guidelines [57], for those who have already received systemic anticoagulation with UFH, other anticoagulants are generally not added. Some researchers [58] have proposed regional citrate anticoagulation to prolong the life span of the CRRT filter. Each center can make systematic assessment and decide the individual connection mode and anticoagulation schemes.
The safety and effect of peritoneal dialysis during ECMO in children with CHD should be affirmed [59,60,61,62,63]. Because anticoagulation increases the risk of bleeding during PD tube placement, the patient’s coagulation status should be evaluated before placement to prevent bleeding. Ultrasound guidance can avoid the risk of abdominal complications (such as intestinal perforation, parenchymal organ puncture injury).
Wound care
Central cannulation generally requires delayed sternal closure. The sternal skin should be sutured as much as possible or covered with sterile dressings [64]. Strict aseptic techniques, keeping the wound surface clean and dry, assessing the hemorrhage and exudation, routine cleaning and sterilizing the skin around the cannula and incision, and pericardial mediastinal irrigation are essential to prevent infections. Topical sealants, such as gelatin sponges or dry gauze strips, can be used to control oozing and bleeding [65]. When chest drainage increases or stops with increased tension of the dressing, accompanied by decreasing blood pressure and pulse pressure, lower cardiac sound and unstable pump flow [66], pericardial tamponade should be considered. Emergency thoracotomy to remove the accumulated blood is recommended.
Weaning and transition
When cardiac function recovers after 5–7 days of ECMO support, weaning can be considered. If there is no sign of improvement in cardiac function for longer than two weeks, transition to an intermediate- or long-term mechanical cardiac support device or heart transplant should be considered [67]. If irreversible multiple organ failure occurs, ECMO withdrawal should be considered. Before VA ECMO weaning, it is necessary to repeatedly evaluate cardiopulmonary function, residual lesions and adaptive changes in the cardiac structure. Reducing the pump flow and temporarily clamping the circuit are needed for further evaluation.
When the pump flow is gradually reduced to less than 30% of the full flow for 6–24 hours, weaning can be attempted if the following conditions are met [10, 68,69,70]: (1) with low levels of vasoactive drugs (epinephrine ≤ 0.02–0.05 μg/kg/minute, dopamine/dobutamine 3–5 μg/kg/minute), arterial pressure within the normal values and pulse pressure difference greater than 20 mmHg, CVP > 5 mmHg [10]; (2) left ventricular ejection fraction > 25%, left and right ventricular motion coordination and aortic valve velocity time integral ≥ 10 cm[69]; (3) with the ventilator parameters as follows: oxygen concentration ≤ 60%, tidal volume 6–8 mL/kg, peak inspiratory pressure < 30 cmH2O, PEEP 5–15 cmH2O and PaO2/FiO2 > 200 mmHg after biventricular correction, PCO2 ≤ 45 mmHg, pH > 7.3, SvO2 ≥ 65%, blood lactate, electrolyte and hematocrit (HCT) values within the normal range; (4) in patients with a single ventricle, it is necessary to adjust the balance of systemic/pulmonary blood flow according to the cardiac surgical procedures and the level of peripheral blood oxygen saturation (SpO2). The oxygenation index and mechanical ventilation parameters should meet the targets and all conditions remain stable.
First-aid medicines, equipment and blood availability should be accessible to address the possible risks during weaning. The trial off VA ECMO for CHD is similar to the ELSO guideline [10, 68, 71, 72]. The LV decompression cannula should be removed first. The sternal incision could be closed at the same time as decannulation if hemodynamics is stable. If the carotid artery is difficult to repair, ligation should be considered. It is still necessary to evaluate cardiopulmonary function after weaning off. If cardiopulmonary function is unstable, ECMO should be implanted once again.
Main complications
Bleeding and thromboembolism
Bleeding after cardiac surgery could be caused by surgical factors or coagulation disorder. The optimal treatment depends on the cause, amount and site of bleeding. For surgical bleeding, operative hemostasis should be performed. For light bleeding other than the brain, the anticoagulation level can be adjusted downward. In cases of intracranial hemorrhage and/or massive bleeding, anticoagulants should be suspended until the bleeding is controlled. Hemostatic and blood products should be given as needed. For refractory bleeding, anti-fibrinolytic therapy (e.g., tranexamic acid) should be initiated if necessary.
ECMO-associated thrombosis could occur both in the ECMO circuit and vessels. Coagulation disorders after prolonged CPB, high-dose vasopressor infusion, delayed initiation of heparin and excessive infusion of coagulation substrate increase the risk of thrombosis. An individual anticoagulation strategy, careful surgical hemostasis, stable internal environment, reasonable infusion of coagulation substrate, appropriate vasopressor usage, effective left heart decompression [73] and reduction of ventricular blood stasis could contribute to reduce the risk of thrombosis. Small thrombi in the ECMO circuit should be observed closely by improving the anticoagulation level. In case of life-threatening thrombotic events, emergency treatment of surgical thrombectomy [74] and ECMO circuit replacements should actively be taken into consideration.
Brain injury
The risk factors for ECMO-related brain injury include younger age (gestational age < 34 weeks), lower body weight (< 3 kg), exposure to CPR, acidosis, surgical factors, thromboembolism, systemic anticoagulation and cerebral hypoperfusion [76]. Routine neurological assessment and multimodal neurological function monitoring [76], such as transcranial ultrasound, continuous near-infrared spectral oxygen saturation, electroencephalography and bispectral index, should be performed to monitor possible cerebral dysfunction. A CT scan is recommended to evaluate the possibility of acute brain injury in cases with clinical signs. In cases with cerebral edema, slightly lowering the circuit temperature, local sub-hypothermia therapy, glucocorticoids and dehydrating agents should be used to control the intracranial pressure. It is necessary to monitor CO2 levels to avoid the effects of hyperventilation on cerebral vessels. In patients with mild intracranial hemorrhage, close monitoring of neurological function and optimization anticoagulant strategy are required. ECMO discontinuation should be considered in cases of severe intracranial hemorrhage with an expected poor prognosis.
Extracorporeal cardiopulmonary resuscitation
ECPR is the rapid deployment of VA ECMO to provide reperfusion with oxygenation and cardiac support when conventional cardiopulmonary resuscitation (CPR) fails to restore sustained spontaneous circulation [77]. Owing to the anatomical and physiological characteristics of CHD, low cardiac output, poor oxygenation and insufficient cerebral perfusion are prone to occur during chest compression. Therefore, when CPR fails to restore spontaneous circulation within 15 minutes, the ECPR procedure should be started immediately [70, 77]. Timely application of ECPR can reduce organ damage and improve the survival of children with CHD in the hospital [78,79,80,81].
According to the anatomical characteristics of CHD and the speed of rescue, the ECPR cannulation strategy is formulated, central cannulation can be performed in the early stage within the postoperative 14 days, and cervical or femoral arteriovenous cannulation can be performed in children before surgery or during the late postoperative period [70, 82].
One of the key factors for the success of ECPR is the full effectiveness of CRP and the rapid implementation of ECMO [83, 84]. After ECMO initiation, high pump flow is given to improve the perfusion, oxygenation and inner environment of organs as soon as possible to create the conditions for subsequent diagnosis and treatment. Although effects of mild hypothermia brain protection is controversial, targeted management of mild hypothermia (33–34 °C) for 24–48 hours may be considered in children at risk of serious neurological complications [85]. Carrying out imaging examinations, identifying the primary cause of cardiac arrest and implementing timely intervention or surgical re-intervention will help to improve the prognosis [82, 86, 87].
Special considerations for complicated CHD
Hypoplastic left heart syndrome
ECMO management differences after Norwood surgery for HLHS is related to the procedures of Sano or B-T shunt. After Sano shunt, pulmonary vessels only receive blood supply in ventricular systolic stage, whereas after B-T shunt, pulmonary vessels receive continuous blood supply in the systolic and diastolic stages, and the latter is prone to resulting in a greater risk of coronary insufficiency. To provide sufficient systemic and coronary perfusion during ECMO running, in addition to strengthening cardiac function and maintaining higher HCT level, excessive reduction in pulmonary vascular resistance should be avoided by adjustment of medicine and ventilator setting.
Single-ventricular, bidirectional Glenn and Fontan circulation
For uncorrected or stage 1 single ventricle, when patent ductus arteriosus (PDA) (or B-T shunt) closure and/or restricted atrial septal defect (ASD) occurs, insufficient pulmonary and systemic blood mixing leads to severe hypoxemia, elevated pulmonary arterial and venous pressure and finally to circulatory failure. Under these conditions, ECMO support should be considered. A high ECMO flow rate (150–200 mL/kg/minute) is usually required to compensate for the flow shunt into the pulmonary circulation [17]. Emergency atrial septostomy or corresponding surgery is required when hemodynamics is stable.
Bidirectional Glenn and Fontan circulations rely on passive low pulmonary resistance. When central cannulation is adopted after early surgery, superior vena cava cannulation should be established first to achieve venous drainage and reduced intracranial pressure to decrease intracranial bleeding risks. If venous drainage is insufficient, inferior vena cava cannulation should be added. Excessive ventilation causing low CO2 blood levels perhaps might lead to insufficient cerebral blood flow, further resulting in insufficient venous drainage [10, 17].
When higher pump flow is provided, maintaining pulsatile blood flow by a certain degree of ventricle filling and output is needed to avoid blood stasis in Fontan graft [17]. In patients with chronic cardiac insufficiency, increased afterload induced by higher pump flow may not be conducive to myocardial recovery and ECMO withdrawal [17]. Due to the lack of a sub-pulmonic pumping/capacitance chamber, compressions and recoil by chest outside massage often result in blood moving back through the venous chamber rather than antegrade through the lungs and into the systemic ventricle for coronary artery and cerebral perfusion. Once cardiac arrest happens in patients after Fontan procedure, ECMO should be established as soon as possible [17].
Various causes of bidirectional Glenn and Fontan circulation failure should be investigated, such as arrhythmia, anatomic obstruction to flow, pulmonary vascular remodeling, atrioventricular valve dysfunction, univentricular diastolic dysfunction and chronic under filling and/or univentricular systolic dysfunction. As one might imagine, the outcome of extracorporeal support largely depends upon the underlying physiology and mechanism for “Fontan failure” [17].
ECMO is effective for early postoperative support of Fontan circulation failure. However, patients with late-phase failure usually present with extreme end-organ failure, such as protein losing enteropathy, plastic bronchitis, cirrhosis, or renal failure. The middle-to-late phase failure patients are appropriate transplant candidates and are better suited for transitioning to more durable mechanical support (ventricular-assist device) via ECMO [17].
Transposition of the great arteries with intact ventricular septum
Pulmonary hypertension is uncommon in patients with TGA/IVS). The incidence of TGA/IVS with pulmonary hypertension was 1%–12% [88, 89]. Increased pulmonary vascular resistance leads to reduced pulmonary blood flow and atrial blood does not mix effectively. Coupled with PDA right-to-left shunt, effective pulmonary blood flow is further lost. The VV or VA ECMO mode can be adopted. The time of ECMO supporting should not be too long and both pulmonary hypertension and left ventricular “deconditioning” resulting from preoperative use of ECMO are responsible for left ventricular mass decaying and functional degeneration [89, 90]. ASO should be performed as soon as possible when the condition is stable. When the uncorrected TGA/IVS with restricted ASD and without pulmonary hypertension develops severe hypoxemia, it is not suitable to establish the ECMO, but emergency ASO or atrial septostomy should be given priority because the risk of pulmonary hemorrhage and left heart dramatic expansion owing to restricted ASD and excessive pulmonary blood coming from PDA is dramatically increased.
Other conditions
Aortic regurgitation
VA ECMO blood flow may aggravate aortic regurgitation and increase the risk of left ventricular afterload and left ventricular dramatic expansion, so aortic regurgitation should be assessed carefully before ECMO implantation. If it is found after ECMO implantation, early left ventricular decompression or surgical correction is required [10].
Aortic arch separation
Careful attention to the anatomy of the head and neck vessels (i.e., location of interruption of arch) is required before ECMO cannulation to ensure brain perfusion with oxygenated ECMO flow [10].
Anomalous left coronary artery origin from pulmonary artery
Due to secondary severe myocardial ischemia, most of the ALCAPA patients had severe cardiac insufficiency, with high incidence of perioperative adverse events [91, 92]. Planned application of ECMO could be carried out for children with severe LV insufficiency. If cardiac function cannot be improved within a short period postoperation, central cannulation can be changed to peripheral cannulation or converted to VAD, which could be beneficial for chest closure, prolonging ventricularassisting time and reducing infection risks.
Conclusions
This consensus provided a comprehensive clinical and technical approach for ECMO support in CHD in children. Indications and contraindications should be evaluated carefully before ECMO application. The cannulation strategy is determined based on the patient’s body size, cardiac anatomy and different surgical procedures of CHD. ECMO pump flow, ventilator parameters and vasoactive drugs should be adjusted according to different ECMO support stages and goals as well as special characteristics of cardiac function, procedures and hemodynamics, to maintain the balance of DO2 and VO2 and to promote the recovery of cardiac function and organ protection. The anticoagulation strategy should be tailored by considering the unique bleeding and clotting risks. Left ventricular decompression and pericardial tamponade should be monitored carefully in the early stage of ECMO. Residual lesions, volume overload, bleeding and brain complication should be identified and intervened as soon as possible. Special considerations for complicated CHD should be considered during ECMO management.
References
Bartlett RH, Gazzaniga AB, Jefferies MR, Huxtable RF, Haiduc NJ, Fong SW. Extracorporealmembrane oxygenation (ECMO) cardiopulmonary supportininfancy. Trans Am Soc Artif Intern Organs. 1976;1976:80–93.
Allen KY, Allan CK, Su L, McBride ME. Extracorporeal membrane oxygenation in congenital heart disease. Semin Perinatol. 2018;42:104–10.
Barbaro RP, Paden ML, Guner YS, Raman L, Ryerson LM, Alexander P, et al. Pediatric extracorporeal life support organization registry international report 2016. ASAIO J. 2017;63:456–63.
Lorusso R, Raffa GM, Kowalewski M, Alenizy K, Sluijpers N, Makhoul M, et al. Structured review of post-cardiotomy extracorporeal membrane oxygenation: part 2-pediatric patients. J Heart Lung Transplant. 2019;38:1144–61.
Lin R, Tan LH, Zhang ZW, Sun MY. Du LZ. Extracorporeal membrane oxygenation treatment of a neonate with severe low cardiac output syndrome following open heart surgery. Zhonghua Er Ke Za Zhi. 2008;46:26–9 (in Chinese).
Liu ML, Yang YY, Zhang W, Jiang L, Shen J, Guo Z, et al. ECMO in patients with residual lesions after cardiac surgery. J Clin Pediatr Surg. 2021;20:518–24 (in Chinese).
Chinese Society of Extra Corporeal Life Support. 2022.
Jin Y, Feng Z, Zhao J, Hu J, Tong Y, Guo S, et al. Outcomes and factors associated with early mortality in pediatric postcardiotomy veno-arterial extracorporeal membrane oxygenation. Artif Organs. 2021;45:6–14.
Ford MA, Gauvreau K, McMullan DM, Almodovar MC, Cooper DS, Rycus PT, et al. Factors associated with mortality in neonates requiring extracorporeal membrane oxygenation for cardiac indications: analysis of the extracorporeal life support organization registry data. Pediatr Crit Care Med. 2016;17:860–70.
Brown G, Moynihan KM, Deatrick KB, Hoskote A, Sandhu HS, Aganga D, et al. Extracorporeal life support organization (ELSO): guidelines for pediatric cardiac failure. ASAIO J. 2021;67:463–75.
Valencia E, Staffa SJ, Nathan M, Smith-Parrish M, Kaza AK, DiNardo JA, et al. Hyperlactataemia as a predictor of adverse outcomes post-cardiac surgery in neonates with congenital heart disease. Cardiol Young. 2021;31:1401–6.
Gaies MG, Gurney JG, Yen AH, Napoli ML, Gajarski RJ, Ohye RG, et al. Vasoactive–inotropic score as a predictor of morbidity and mortality in infants after cardiopulmonary bypass. Pediatr Crit Care Med. 2010;11:234–8.
Maratta C, Potera RM, van Leeuwen G, Castillo Moya A, Raman L, Annich GM. Extracorporeal life support organization (ELSO): 2020 pediatric respiratory ELSO guideline. ASAIO J. 2020;66:975–9.
Rais-Bahrami K, Van Meurs KP. Venoarterial versus venovenous ECMO for neonatal respiratory failure. Semin Perinatol. 2014;38:71–7.
Zhao J, Jin ZX. ECMO speciallist training manual. Beijing: People's Medical Publishing House; 2015.
Pediatrics Group of Extracorporeal Life Support Professional Committee of Chinese Medical Doctor Association, Emergency Treatment Group of Pediatric Society of Chinese Medical Association, Extracorporeal Life Support Society of Chinese Society of Cardiovascular Anesthesia, Cardiothoracic Surgery Group of Pediatric Surgery Society of Chinese Medical Association. Expert consensus of extracorporeal membrane oxygenation supports in pediatric fulminant myocarditis. Chin J Emerg Med. 2020;29:36–42.
Bacon MK, Gray SB, Schwartz SM, Cooper DS. Extracorporeal membrane oxygenation (ECMO) support in special patient populations-the bidirectional glenn and fontan circulations. Front Pediatr. 2018;6:299.
Brogan TV, Lequier L, Lorusso R, MacLaren G, Peek G. Extracorporeal life support: the ELSO red book. 5th ed. Ann Arbor, MI: Extracorporeal Life Support Organization; 2017.
Schmidt M, Pellegrino V, Combes A, Scheinkestel C, Cooper DJ, Hodgson C. Mechanical ventilation during extracorporeal membrane oxygenation. Crit Care. 2014;18:203.
Alapati D, Aghai ZH, Hossain MJ, Dirnberger DR, Ogino MT, Shaffer TH, et al. Lung rest during extracorporeal membrane oxygenation for neonatal respiratory failure-practice variations and outcomes. Pediatr Crit Care Med. 2017;18:667–74.
Jardin F, Vieillard-Baron A. Monitoring of right-sided heart function. Curr Opin Crit Care. 2005;11:271–9.
Sherwin ED, Gauvreau K, Scheurer MA, Rycus PT, Salvin JW, Almodovar MC, et al. Extracorporeal membrane oxygenation after stage 1 palliation for hypoplastic left heart syndrome. J Thorac Cardiovasc Surg. 2012;144:1337–43.
Sy E, Sklar MC, Lequier L, Fan E, Kanji HD. Anti-coagulation practices and the prevalence of major bleeding, thromboembolic events, and mortality in venoarterial extracorporeal membrane oxygenation: a systematic review and meta-analysis. Crit Care. 2017;39:87–96.
Beckmann E, Ismail I, Cebotari S, Busse A, Martens A, Shrestha M, et al. Right-sided heart failure and extracorporeal life support in patients undergoing pericardiectomy for constrictive pericarditis: a risk factor analysis for adverse outcome. Thorac Cardiovasc Surg. 2017;65:662–70.
McMichael ABV, Ryerson LM, Ratano D, Fan E, Faraoni D, Annich GM. 2021 ELSO adult and pediatric anticoagulation guidelines. ASAIO J. 2022;68:303–10.
Task Force on Patient Blood Management for Adult Cardiac Surgery of the European Association for Cardio-Thoracic Surgery (EACTS) and the European Association of Cardiothoracic Anaesthesiology (EACTA), Boer C, Meesters MI, Milojevic M, Benedetto U, Bolliger D, et al. 2017 EACTS/EACTA Guidelines on patient blood management for adult cardiac surgery. J Cardiothorac Vasc Anesth. 2018;32:88–120.
Lorusso R, Whitman G, Milojevic M, Raffa G, McMullan DM, Boeken U, et al. 2020 EACTS/ELSO/STS/AATS expert consensus on post-cardiotomy extracorporeal life support in adult patients. Ann Thorac Surg. 2021;111:327–69.
Sorabella RA, Padilla L, Byrnes JW, Timpa J, O’Meara C, Buckman JR, et al. Outcomes in pediatric post-cardiotomy ecmo support with modification of systematic support strategy. World J Pediatr Congenit Heart Surg. 2022;13:46–52.
Neunert C, Chitlur M, van Ommen CH. The changing landscape of anticoagulation in pediatric extracorporeal membrane oxygenation: use of the direct thrombin inhibitors. Front Med (Lausanne). 2022;9:887199.
Zhang ZR, Zhou XQ, Fan ZK, Shi Y, Shen YY, Zhu C, et al. Extracorporeal membrane oxygenation treatment for high-risk pulmonary embolism with cardiac arrest in a young adult male. World J Emerg Med. 2021;12:324–6.
Burkhoff D, Sayer G, Doshi D, Uriel N. Hemodynamics of mechanical circulatory support. J Am Coll Cardiol. 2015;66:2663–74.
Ostadal P, Mlcek M, Kruger A, Hala P, Lacko S, Mates M, et al. Increasing venoarterial extracorporeal membrane oxygenation flow negatively affects left ventricular performance in a porcine model of cardiogenic shock. J Transl Med. 2015;13:266.
Hireche-Chikaoui H, Grubler MR, Bloch A, Windecker S, Bloechlinger S, Hunziker L. Nonejecting hearts on femoral veno-arterial extracorporeal membrane oxygenation: aortic root blood stasis and thrombus formation-a case series and review of the literature. Crit Care Med. 2018;46:e459–64.
Williams B, Bernstein W. Review of venoarterial extracorporeal membrane oxygenation and development of intracardiac thrombosis in adult cardiothoracic patients. J Extra Corpor Technol. 2016;48:162–7.
Cevasco M, Takayama H, Ando M, Garan AR, Naka Y, Takeda K. Left ventricular distension and venting strategies for patients on venoarterial extracorporeal membrane oxygenation. J Thorac Dis. 2019;11:1676–83.
Donker DW, Brodie D, Henriques JPS, Broome M. Left ventricular unloading during veno-arterial ECMO: a simulation study. ASAIO J. 2019;65:11–20.
Hacking DF, Best D, d’Udekem Y, Brizard CP, Konstantinov IE, Millar J, et al. Elective decompression of the left ventricle in pediatric patients may reduce the duration of venoarterial extracorporeal membrane oxygenation. Artif Organs. 2015;39:319–26.
Kimura M, Kinoshita O, Fujimoto Y, Murakami A, Shindo T, Kashiwa K, et al. Central extracorporeal membrane oxygenation requiring pulmonary arterial venting after near-drowning. Am J Emerg Med. 2014;32:e1–2.
Fiedler AG, Dalia A, Axtell AL, Ortoleva J, Thomas SM, Roy N, et al. Impella placement guided by echocardiography can be used as a strategy to unload the left ventricle during peripheral venoarterial extracorporeal membrane oxygenation. J Cardiothorac Vasc Anesth. 2018;32:2585–91.
Agarwal HS, Hardison DC, Saville BR, Donahue BS, Lamb FS, Bichell DP, et al. Residual lesions in postoperative pediatric cardiac surgery patients receiving extracorporeal membrane oxygenation support. J Thorac Cardiovasc Surg. 2014;147:434–41.
Howard TS, Kalish BT, Wigmore D, Nathan M, Kulik TJ, Kaza AK, et al. Association of extracorporeal membrane oxygenation support adequacy and residual lesions with outcomes in neonates supported after cardiac surgery. Pediatr Crit Care Med. 2016;17:1045–54.
Soynov IA, Kornilov IA, Kulyabin YY, Zubritskiy AV, Ponomarev DN, Nichay NR, et al. Residual lesion diagnostics in pediatric postcardiotomy extracorporeal membrane oxygenation and its outcomes. World J Pediatr Congenit Heart Surg. 2021;12:605–13.
Hull NC, Schooler GR, Binkovitz LA, Williamson EE, Araoz PA, Yu L, et al. Chest computed tomography angiography in children on extracorporeal membrane oxygenation (ECMO). Pediatr Radiol. 2018;48:1021–30.
Boscamp NS, Turner ME, Crystal M, Anderson B, Vincent JA, Torres AJ. Cardiac catheterization in pediatric patients supported by extracorporeal membrane oxygenation: a 15-year experience. Pediatr Cardiol. 2017;38:332–7.
Booth KL, Roth SJ, Perry SB, del Nido PJ, Wessel DL, Laussen PC. Cardiac catheterization of patients supported by extracorporeal membrane oxygenation. J Am Coll Cardiol. 2002;40:1681–6.
Krishnan S, Schmidt GA. Hemodynamic monitoring in the extracorporeal membrane oxygenation patient. Curr Opin Crit Care. 2019;25:285–91.
Siddall E, Khatri M, Radhakrishnan J. Capillary leak syndrome: etiologies, pathophysiology, and management. Kidney Int. 2017;92:37–46.
Smith AH, Hardison DC, Worden CR, Fleming GM, Taylor MB. Acute renal failure during extracorporeal support in the pediatric cardiac patient. ASAIO J. 2009;55:412–6.
Elella RA, Habib E, Mokrusova P, Joseph P, Aldalaty H, Ahmadi MA, et al. Incidence and outcome of acute kidney injury by the pRIFLE criteria for children receiving extracorporeal membrane oxygenation after heart surgery. Ann Saudi Med. 2017;37:201–6.
Joannidis M, Forni LG, Klein SJ, Honore PM, Kashani K, Ostermann M, et al. Lung-kidney interactions in critically ill patients: consensus report of the acute disease quality initiative (ADQI) 21 workgroup. Intensive Care Med. 2020;46:654–72.
Gorga SM, Sahay RD, Askenazi DJ, Bridges BC, Cooper DS, Paden ML, et al. Fluid overload and fluid removal in pediatric patients on extracorporeal membrane oxygenation requiring continuous renal replacement therapy: a multicenter retrospective cohort study. Pediatr Nephrol. 2020;35:871–82.
Selewski DT, Askenazi DJ, Bridges BC, Cooper DS, Fleming GM, Paden ML, et al. The impact of fluid overload on outcomes in children treated with extracorporeal membrane oxygenation: a multicenter retrospective cohort study. Pediatr Crit Care Med. 2017;18:1126–35.
Blijdorp K, Cransberg K, Wildschut ED, Gischler SJ, Jan Houmes R, Wolff ED, et al. Haemofiltration in newborns treated with extracorporeal membrane oxygenation: a case-comparison study. Crit Care. 2009;13:R48.
Schmidt M, Bailey M, Kelly J, Hodgson C, Cooper DJ, Scheinkestel C, et al. Impact of fluid balance on outcome of adult patients treated with extracorporeal membrane oxygenation. Intensive Care Med. 2014;40:1256–66.
Zarbock A, Kellum JA, Schmidt C, Van Aken H, Wempe C, Pavenstadt H, et al. Effect of early vs delayed initiation of renal replacement therapy on mortality in critically ill patients with acute kidney injury: the ELAIN randomized clinical trial. JAMA. 2016;315:2190–9.
Tan BK, Liew ZH, Kaushik M, Cheah AKW, Tan HK. Early initiation of renal replacement therapy among burned patients with acute kidney injury. Ann Plast Surg. 2020;84:375–8.
Section 5: Dialysis Interventions for Treatment of AKI. Kidney Int Suppl (2011). 2012;2:89–115.
Giani M, Scaravilli V, Stefanini F, Valsecchi G, Rona R, Grasselli G, et al. Continuous renal replacement therapy in venovenous extracorporeal membrane oxygenation: a retrospective study on regional citrate anticoagulation. ASAIO J. 2020;66:332–8.
Sasser WC, Robert SM, Askenazi DJ, O’Meara LC, Borasino S, Alten JA. Peritoneal dialysis: an alternative modality of fluid removal in neonates requiring extracorporeal membrane oxygenation after cardiac surgery. J Extra Corpor Technol. 2014;46:157–61.
Golej J, Boigner H, Burda G, Hermon M, Kitzmueller E, Trittenwein G. Peritoneal dialysis for continuing renal support after cardiac ECMO and hemofiltration. Wien Klin Wochenschr. 2002;114:733–8.
Li G, Zhang L, Sun Y, Chen J, Zhou C. Co-initiation of continuous renal replacement therapy, peritoneal dialysis, and extracorporeal membrane oxygenation in neonatal life-threatening hyaline membrane disease: a case report. Medicine (Baltimore). 2019;98:e14194.
Bao Q, Hong XY, Liu YY, Zhang XJ, Gao HT, Feng ZC. Outcome of pediatric extracorporeal membrane oxygenation in a single center. Zhonghua Er Ke Za Zhi. 2018;56:122–7 (in Chinese).
Nourse P, Cullis B, Finkelstein F, Numanoglu A, Warady B, Antwi S, et al. ISPD guidelines for peritoneal dialysis in acute kidney injury: 2020 update (paediatrics). Perit Dial Int. 2021;41:139–57.
Li XF, Luo DD, Zhu WZ. Application of delayed sternal closure after neonatal cardiac surgery. Chin J Thorac Cardiovasc Surg. 2016;32:257–60 (in Chinese).
Lorusso R, Whitman G, Milojevic M, Raffa G, McMullan DM, Boeken U, et al. 2020 EACTS/ELSO/STS/AATS expert consensus on post-cardiotomy extracorporeal life support in adult patients. Eur J Cardiothorac Surg. 2021;59:12–53.
Basilio C, Fontoura A, Fernandes J, Roncon-Albuquerque R Jr, Paiva JA. Cardiac tamponade complicating extracorporeal membrane oxygenation: a single-centre experience. Heart Lung Circ. 2021;30:1540–4.
Lorusso R, Whitman G, Milojevic M, Raffa G, McMullan DM, Boeken U, et al. 2020 EACTS/ELSO/STS/AATS expert consensus on post-cardiotomy extracorporeal life support in adult patients. J Thorac Cardiovasc Surg. 2021;161:1287–331.
Extracorporeal Life Support Organization. ELSO guidelines for cardiopulmonary extracorporeal life support. Version 14. 2017. http://www.elso.org/resources/guidelines.aspx. Accessed 1 Jul 2022.
Keebler ME, Haddad EV, Choi CW, McGrane S, Zalawadiya S, Schlendorf KH, et al. Venoarterial extracorporeal membrane oxygenation in cardiogenic shock. JACC Heart Fail. 2018;6:503–16.
Perry T, Brown T, Misfeldt A, Lehenbauer D, Cooper DS. Extracorporeal membrane oxygenation in congenital heart disease. Children (Basel). 2022. https://doi.org/10.3390/children9030380.
Holgren SE, Frede RT, Crumley JP, Patel SS, Moore EA, Turek JW. Novel utilization of the bridge during weaning off venoarterial ECMO: the Hoffman clamp method. Innovations (Phila). 2016;11:229–31.
Westrope C, Harvey C, Robinson S, Speggiorin S, Faulkner G, Peek GJ. Pump controlled retrograde trial off from VA-ECMO. ASAIO J. 2013;59:517–9.
Kumar SR, Scott N, Wells WJ, Starnes VA. Liberal use of delayed sternal closure in children is not associated with increased morbidity. Ann Thorac Surg. 2018;106:581–6.
Said AS, Guilliams KP, Bembea MM. Neurological monitoring and complications of pediatric extracorporeal membrane oxygenation support. Pediatr Neurol. 2020;108:31–9.
Brogan TV. ECMO specialist training manual. Michigan: Extracorporeal Life Support Organization; 2018.
Cerebral Protection In Cardiac Intensive Care Group Neural Regeneration And Repair Committee Chinese Research Hospital Association. Chinese consensus guideline for cerebral protection in the perioperative period of cardiac surgery (2019). Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2019;31:129–34 (in Chinese).
Guerguerian AM, Sano M, Todd M, Honjo O, Alexander P, Raman L. Pediatric extracorporeal cardiopulmonary resuscitation ELSO guidelines. ASAIO J. 2021;67:229–37.
Raymond TT, Cunnyngham CB, Thompson MT, Thomas JA, Dalton HJ, Nadkarni VM, et al. Outcomes among neonates, infants, and children after extracorporeal cardiopulmonary resuscitation for refractory in hospital pediatric cardiac arrest: a report from the National Registry of Cardiopulmonary Resuscitation. Pediatr Crit Care Med. 2010;11:362–71.
Ortmann L, Prodhan P, Gossett J, Schexnayder S, Berg R, Nadkarni V, et al. Outcomes after in-hospital cardiac arrest in children with cardiac disease: a report from get with the guidelines-resuscitation. Circulation. 2011;124:2329–37.
Matos RI, Watson RS, Nadkarni VM, Huang HH, Berg RA, Meaney PA, et al. Duration of cardiopulmonary resuscitation and illness category impact survival and neurologic outcomes for in-hospital pediatric cardiac arrests. Circulation. 2013;127:442–51.
Alsoufi B, Awan A, Manlhiot C, Guechef A, Al-Halees Z, Al-Ahmadi M, et al. Results of rapid-response extracorporeal cardiopulmonary resuscitation in children with refractory cardiac arrest following cardiac surgery. Eur J Cardiothorac Surg. 2014;45:268–75.
Ergun S, Yildiz O, Gunes M, Akdeniz HS, Ozturk E, Onan IS, et al. Use of extracorporeal membrane oxygenation in postcardiotomy pediatric patients: parameters affecting survival. Perfusion. 2020;35:608–20.
Alsoufi B, Awan A, Manlhiot C, Al-Halees Z, Al-Ahmadi M, McCrindle BW, et al. Does single ventricle physiology affect survival of children requiring extracorporeal membrane oxygenation support following cardiac surgery? World J Pediatr Congenit Heart Surg. 2014;5:7–15.
Kane DA, Thiagarajan RR, Wypij D, Scheurer MA, Fynn-Thompson F, Emani S, et al. Rapid-response extracorporeal membrane oxygenation to support cardiopulmonary resuscitation in children with cardiac disease. Circulation. 2010;122:S241–8.
Cerebral Protection In Cardiac Intensive Care Group Neural Regeneration And Repair Committee Chinese Research Hospital Association, Neural Intensive Nursing And Rehabilitation Group Neural Regeneration And Repair Committee Chinese Research Hospital Association. Chinese consensus for mild hypothermia brain protection. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2020;32:385–91 (in Chinese).
Guo Z, Yang Y, Zhang W, Shen J, Jiang L, Yu X, et al. Extracorporeal cardiopulmonary resuscitation in children after open heart surgery. Artif Organs. 2019;43:633–40.
Farhat A, Ling RR, Jenks CL, Poon WH, Yang IX, Li X, et al. Outcomes of pediatric extracorporeal cardiopulmonary resuscitation: a systematic review and meta-analysis. Crit Care Med. 2021;49:682–92.
Yam N, Chen RH, Rocha BA, Lun KS, Yung TC, Au TW. Preoperative venovenous extracorporal membrane oxygenation for transposition of great arteries with severe pulmonary hypertension in a newborn. Ann Thorac Surg. 2020;109:e329–30.
Jaillard S, Belli E, Rakza T, Larrue B, Magnenant E, Rey C, et al. Preoperative ECMO in transposition of the great arteries with persistent pulmonary hypertension. Ann Thorac Surg. 2005;79:2155–8.
Sarris GECG, Balmer CS, Bonou PG, Comas JVS, da Cruz EU, Chiara LDI, et al. Clinical guidelines for the management of patients with transposition of the great arteries with intact ventricular septum. Eur J Cardiothorac Surg. 2017;51:e1–32.
Fudulu DP, Dorobantu DM, Azar Sharabiani MT, Angelini GD, Caputo M, Parry AJ, et al. Outcomes following repair of anomalous coronary artery from the pulmonary artery in infants: results from a procedure-based national database. Open Heart. 2015;2:e000277.
Cashen K, Kwiatkowski DM, Riley CM, Buckley J, Sassalos P, Gowda KN, et al. Anomalous origin of the left coronary artery from the pulmonary artery: a retrospective multicenter study. Pediatr Crit Care Med. 2021;22:e626–35.
Funding
This study was supported by “the Fundamental Research Funds for the Central Universities” (No. 226–2022-00060) and National Key R&D Program of China (No. 2021YFC2701700).
Author information
Authors and Affiliations
Contributions
LR, WW, WX, XZM, LJP, ZCB, HXY, MXM, SSS and YLF contributed equally to this paper. LR contributed to conceptualization, data curation, formal analysis, investigation, methodology, project administration, writing of the original draft, reviewing and editing. WW contributed to data curation, investigation, supervision, validation, writing of the original draft, reviewing and editing. WX contributed to formal analysis, investigation, validation and writing of the original draft. XZM contributed to formal analysis, investigation, supervision, validation and writing of the original draft. LJP contributed to formal analysis, investigation, supervision, validation, writing of the original draft, reviewing and editing. ZCB contributed to formal analysis, investigation, supervision, validation, writing of the original draft, reviewing and editing. HXY contributed to investigation, writing of the original draft, reviewing and editing. MXM contributed to investigation, supervision, validation, reviewing and editing. SSS contributed to investigation, writing of the original draft, reviewing and editing. YLF contributed to conceptualization, data curation, formal analysis, investigation, methodology, writing of the original draft, reviewing and editing. SQ contributed to investigation, supervision, validation, reviewing and editing. All the authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
Not applicable.
Conflict of interest
No financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article. The authors have no conflict of interest to declare. Author Qiang Shu is the Chief Editor of World Journal of Pediatrics. The paper was handled by the other editors and has undergone a rigorous peer-review process. Author Qiang Shu was not involved in the journal's review or decision making of this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lin, R., Wang, W., Wang, X. et al. Perioperative extracorporeal membrane oxygenation in pediatric congenital heart disease: Chinese expert consensus. World J Pediatr 19, 7–19 (2023). https://doi.org/10.1007/s12519-022-00636-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-022-00636-z