Abstract
Background
The influence of new-onset atrial fibrillation (AF) on the long-term prognosis of nonagenarians who survive acute myocardial infarction (AMI) has not been demonstrated.
Objective
Our aim was to study the association between new-onset AF and long-term prognosis of nonagenarians who survive AMI.
Methods
From a total of 96 patients aged ≥89 years admitted during a 5-year period, 64 (67 %) were discharged alive and are the focus of this study.
Results
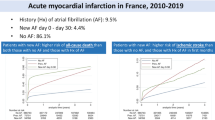
Mean age was 91.0 ± 2.0 years, and 39 patients (61 %) were women. During admission, 9 patients (14 %) presented new-onset AF, 51 (80 %) did not present AF, and 4 (6 %) had chronic AF. During follow-up (mean 2.3 ± 2.6 years; 6.6 ± 3.6 years in survivors), 58 patients (91 %) died, including the 9 patients with new-onset AF. Cumulative survival at 6, 12, 18, 24, and 30 months was 68.3 %, 57.2 %, 49.2 %, 47.6 %, and 31.8 %, respectively. The only two independent predictors of mortality in the multivariate analysis were age (hazard ratio [HR] 1.14; 95 % confidence interval [CI] 1.01–1.28; p = 0.04) and new-onset AF (HR 2.3; 95 % CI 1.1–4.8; p = 0.02).
Conclusion
New-onset AF is a marker of poor prognosis in nonagenarians who survive AMI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The incidence of acute myocardial infarction (AMI) in very elderly patients is increasing due to rapid ageing of the population, which is expected to be more noticeable in the coming years [1]. Atrial fibrillation (AF) is a common finding in patients who have AMI and becomes more frequent with age. AMI is associated with a sharp increase in the occurrence of AF. The incidence of AF among AMI patients ranges between 7 % and 22 % [2, 3] and has increased in recent years [4]. Although the influence of AF on AMI remains controversial in younger patients, the bulk of evidence suggests that AF has adverse prognostic implications after AMI [3, 5, 6]. In fact, a recent meta-analysis concluded that AF was associated with an increased risk of mortality in AMI patients with a mean age of 65 years [2]. The studies mentioned above demonstrated that new-onset AF at the time of AMI is associated with a higher risk of mortality than pre-existing AF, for which there is little or no risk of mortality [2, 5, 6].
Previous data on nonagenarians with AMI are scarce and are based mainly on studies comprising 100 or fewer patients with ST-segment elevation AMI (STEMI) [7–10]. In addition, these studies do not include data on long-term prognosis [7–9], are not focused on STEMI [10], or only include patients who have undergone primary percutaneous coronary intervention [8, 9]. In patients who survive AMI, mortality increases exponentially with age; in fact, age is the strongest predictor of short-term [11], medium-term [12], and long-term [13] mortality after discharge. As mortality is expected to be high during follow-up in nonagenarians who survive STEMI, the prognostic influence of new-onset AF should be easier to detect in these patients. We hypothesise that new-onset AF could be associated with higher all-cause mortality in nonagenarians who survive STEMI.
Methods
The Myocardial Infarction Management: Observation and Registry in Elderly patients aged 89 years or older (MIMORE 89) registry has been described previously [14, 15] and comprises 96 patients aged ≥89 years with STEMI or complete left bundle branch block AMI admitted to Hospital General Universitario ‘Gregorio Marañón’ (Madrid, Spain) from February 1998 to February 2004. A total of 64 patients (67 %) were discharged alive and are the focus of this study, with follow-up until December 2011.
Categorical variables were compared using the chi-square test (or Fisher’s exact test, when indicated); continuous variables were compared using the t test. We performed a backward stepwise Cox regression analysis with all relevant clinical variables to study independent predictors of long-term mortality. This Cox regression was repeated excluding patients with chronic AF. Results are expressed as the hazard ratio (HR) and 95 % confidence interval (CI). All analyses were performed with SPSS 11.0 (SPSS, Inc., Chicago, Illinois, USA).
The study complies with the Declaration of Helsinki and was approved by the Ethics Committee of Hospital General Universitario Gregorio Marañón, Madrid, Spain.
Results
Overall population
The independent predictors of in-hospital mortality have been published elsewhere [14] and did not include new-onset AF. At admission, 14 patients (14.6 %) presented new-onset AF, 73 (76.0 %) did not present AF, and 9 (9.4 %) had chronic AF. In-hospital mortality was similar in patients with and without new-onset AF (35.7 % vs. 32.9 %, respectively). A total of 64 patients (67 %) were discharged alive and are the focus of this study.
Patients discharged alive
Mean age was 91.0 ± 2.0 years, and 39 patients (61 %) were women. During the index AMI admission, 9 patients (14 %) presented new-onset AF, 51 (80 %) did not present AF, and 4 (6 %) had chronic AF. The CHA2DS2 VASc score [16] was similar in patients with new-onset AF and in those with chronic AF (5.0 ± 1.4 and 5.3 ± 1.5, respectively), and only 3 patients (4.7 %) received warfarin at discharge. The clinical characteristics and discharge treatment (Table 1) of patients with or without new-onset AF were similar. During long-term follow-up (mean 2.3 ± 2.6 years; 6.6 ± 3.6 years in survivors), 58 patients died (91 %), including the 9 patients with new-onset AF (Fig. 1). We were able to identify the cause of death in 16 patients (29 %); the most frequent causes were heart failure (5 patients), stroke (3 patients), and a new AMI (2 patients). A total of 6 patients died from non-cardiac causes (2 hip fractures, 2 respiratory infections, 1 pulmonary embolism, and 1 head injury). Cumulative survival at 6, 12, 18, 24, and 30 months was 68.3 %, 57.2 %, 49.2 %, 47.6 %, and 31.8 %, respectively. The only two independent predictors of mortality in the multivariate analysis were age (HR 1.16; 95 % CI 1.02–1.31; p = 0.03) and new-onset AF (HR 2.3; 95 % CI 1.1–4.7; p = 0.01). The results excluding 4 patients with chronic AF were similar, as follows: age (HR 1.14; 95 % CI 1.01–1.28; p = 0.04) and new-onset AF (HR 2.3; 95 % CI 1.1–4.8; p = 0.02).
Discussion
Long-term follow-up of the MIMORE 89 registry shows that new-onset AF in nonagenarians who survive AMI has serious adverse implications for long-term mortality. In this high-risk population, new AF was a strong predictor of all-cause mortality.
As expected, the incidence of AF in our population (15 % new-onset, 9 % previous) was higher than previously described in younger populations [2–4] and similar to the incidence found in a population of nonagenarians with AMI [10]. Data on nonagenarians with STEMI are scarce and do not cover long-term prognosis [7–10]; therefore, there is no previous evidence for the influence of new-onset AF on long-term prognosis of very elderly patients who survive AMI. All of the 9 patients with new-onset AF who were discharged died during follow-up. Interestingly, 6 of these patients died in the first 4 months after discharge, suggesting that new-onset AF affects the short-term prognosis of nonagenarians who survive AMI. Moreover, the clinical characteristics of patients with new-onset AF were similar to those of patients who did not present this condition during admission; this could imply that new-onset AF is more than a marker of advanced disease.
There are several potential explanations for the observed association between increased all-cause mortality and AF in elderly patients with AMI. The morphofunctional characteristics of the heart in the very elderly [17], including increased left ventricular thickness, suggest a high susceptibility to new-onset AF that could lead to adverse outcome through haemodynamic effects such as loss of atrial contraction, rapid ventricular rates, loss of atrioventricular synchrony, and irregular RR interval, all of which lead to a decrease in cardiac output [18]. AF can also predispose to ventricular arrhythmia after AMI [19]. Finally, new-onset AF in patients with AMI carries a substantial future risk for stroke [4, 6, 20], which is particularly high in nonagenarians. Interestingly, of the 16 patients with a known cause of death during follow-up, 3 died from stroke. Despite a high CHA2DS2 VASc score, oral anticoagulants were very rarely prescribed to these patients, and even clopidogrel was rarely used.
Age is the strongest predictor of mortality after discharge [11–13]; therefore, the high mortality we found (51 % at 18 months) was expected. Interestingly, even in this very elderly population, age was still an important predictor of prognosis, suggesting that the previously described deleterious effect of age on the prognosis of elderly patients with AMI persists in nonagenarians. Most patients had multivessel coronary artery disease, and severe left ventricular dysfunction was common; both factors probably contributed to the poor prognosis of our cohort. In addition, most nonagenarians in our study were women, a finding that is consistent with the generally longer life expectancy of women, although the association between female sex and prognosis is probably dependent on comorbid conditions and age. Comorbid conditions were very common in our population and mainly included diabetes, chronic obstructive pulmonary disease, renal disease, and stroke. The importance of these conditions is reflected in the high frequency of non-cardiac deaths in our registry.
Limitations and strengths
As this is a relatively small single-centre study, our findings may not be generalisable to other populations, and confirmation in larger and more diverse series is desirable. In addition, we were unable to assess other relevant outcomes, such as re-hospitalisation and quality of life. Caution must be exercised when evaluating all-cause mortality and differences between the two groups, given the relatively small number of patients studied. However, the long follow-up and high mortality overcome this limitation. Although our data show a strong association between AF and poor prognosis, it is still unclear whether AF per se is a complication of AMI or merely demarcates the severity of AMI.
One of the strengths of our study is that the cohort comprised a relatively contemporary and consecutive series of well-characterised patients ≥89 years of age with documented STEMI. We also had complete follow-up information with respect to vital status over a mean duration of 5 years after hospital admission. The high mortality rate afforded excellent statistical power, which made it possible to identify independent predictors of decreased survival.
Conclusion
New-onset AF is common in nonagenarians who survive AMI and is a strong marker of poor prognosis.
References
Christensen K, Doblhammer G, Rau R, et al. Ageing populations: the challenges ahead. Lancet. 2009;374:1196–208.
Jabre P, Roger VL, Murad MH, et al. Mortality associated with atrial fibrillation in patients with myocardial infarction: a systematic review and meta-analysis. Circulation. 2011;123:1587–93.
Schmitt J, Duray G, Gersh BJ, et al. Atrial fibrillation in acute myocardial infarction: a systematic review of the incidence, clinical features and prognostic implications. Eur Heart J. 2009;30:1038–45.
Saczynski JS, McManus D, Zhou Z, et al. Trends in atrial fibrillation complicating acute myocardial infarction. Am J Cardiol. 2009;104:169–74.
Mehta RH, Dabbous OH, Granger CB, et al. Comparison of outcomes of patients with acute coronary syndromes with and without atrial fibrillation. Am J Cardiol. 2003;92:1031–6.
Zusman O, Amit G, Gilutz H, et al. The significance of new onset atrial fibrillation complicating acute myocardial infarction. Clin Res Cardiol. 2012;101:17–22.
Ionescu CN, Amuchastegui M, Ionescu S, et al. Treatment and outcomes of nonagenarians with ST-elevation myocardial infarction. J Invasive Cardiol. 2010;22:474–8.
Danzi GB, Centola M, Pomidossi GA, et al. Usefulness of primary angioplasty in nonagenarians with acute myocardial infarction. Am J Cardiol. 2010;106:770–3.
Salinas P, Galeote G, Martin-Reyes R, et al. Primary percutaneous coronary intervention for ST-segment elevation acute myocardial infarction in nonagenarian patients: results from a Spanish multicentre registry. EuroIntervention. 2011;6:1080–4.
Hovanesyan A, Rich MW. Outcomes of acute myocardial infarction in nonagenarians. Am J Cardiol. 2008;101:1379–83.
Gharacholou SM, Lopes RD, Alexander KP, et al. Age and outcomes in ST-segment elevation myocardial infarction treated with primary percutaneous coronary intervention: findings from the APEX-AMI trial. Arch Intern Med. 2011;171:559–67.
Maggioni AP, Maseri A, Fresco C, et al. Age-related increase in mortality among patients with first myocardial infarctions treated with thrombolysis. The Investigators of the Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto Miocardico (GISSI-2). N Engl J Med. 1993;329:1442–8.
Juliard JM, Charlier P, Golmard JL, et al. Age and lack of beta-blocker therapy are associated with increased long-term mortality after primary coronary angioplasty for acute myocardial infarction. Int J Cardiol. 2003;88:63–8.
Martínez-Sellés M, Datino T, Bueno H. Influence of reperfusion therapy on prognosis in patients aged >or=89 years with acute myocardial infarction. Am J Cardiol. 2005;95:1232–4.
Martínez-Sellés M, Datino T, Bueno H. Coronary care unit admission of very old patients with acute myocardial infarction. Heart. 2006;92:549–50.
Lip GY, Nieuwlaat R, Pisters R, et al. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010;137:263–72.
Fleg JL, Strait J. Age-associated changes in cardiovascular structure and function: a fertile milieu for future disease. Heart Fail Rev. 2012;17:545–54.
Clark DM, Plumb VJ, Epstein AE, et al. Hemodynamic effects of an irregular sequence of ventricular cycle lengths during atrial fibrillation. J Am Coll Cardiol. 1997;30:1039–45.
Sankaranarayanan R, James MA, Nuta B, et al. Does atrial fibrillation beget ventricular fibrillation in patients with acute myocardial infarction? Pacing Clin Electrophysiol. 2008;31:1612–9.
Bishara R, Telman G, Bahouth F, et al. Transient atrial fibrillation and risk of stroke after acute myocardial infarction. Thromb Haemost. 2011;106:877–84.
Disclosures
This study was presented, in part, as an oral communication at the Congress of the European Society of Cardiology, Paris, France, September 2011.
The Myocardial Infarction Management: Observation and Registry in Elderly patients aged 89 years or older (MIMORE 89) registry was supported by a grant from the Mapfre-Medicina Foundation, Madrid, Spain.
The present analysis was partly financed by the Red Temática de Investigación Cooperativa en Enfermedades Cardiovasculares (RECAVA) Cardiovascular Research Network of the Spanish Ministry of Health.
Conflict of interest
None declared
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Martínez-Sellés, M., Datino, T., Figueiras-Graillet, L.M. et al. New-onset atrial fibrillation and prognosis in nonagenarians after acute myocardial infarction. Neth Heart J 21, 499–503 (2013). https://doi.org/10.1007/s12471-013-0439-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12471-013-0439-2