Abstract
Purpose of Review
This abstract aims to examine the advancements in the utilization, indications, and implementation of ultrasound enhancing agents (UEAs) and their potential to enhance cost-effective diagnostics.
Recent Findings
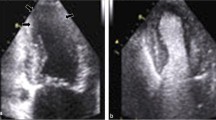
The review highlights significant progress in the application of UEAs, particularly in improving the delineation of endocardial borders, enhancing interpretation of wall motion, and increasing diagnostic accuracy. Moreover, UEAs contribute to streamlining workflows and help avoid more expensive procedures, especially in cases with technically challenging or suboptimal studies.
Summary
UEAs have shown great promise in various medical scenarios, such as enhancing the visualization of the cardiac blood pool and enabling better assessment of ventricular borders, ventricular function, masses, and other intracavitary or myocardial abnormalities. This abstract presents an overview of the recent findings that underscore the potential benefits of UEAs in optimizing cardiac diagnostics while considering cost-effectiveness.










Similar content being viewed by others
Data Availability
Not applicable.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Gramiak R, Shah PM. Echocardiography of the aortic root. Invest Radio. 1968;3:356–66.
Porter TR, Abdelmoneim S, Belcik JT, McCulloch ML, Mulvagh SL, Olson JJ, et al. Guidelines for the cardiac sonographer in the performance of contrast echocardiography: a focused update from the American Society of Echocardiography. J Am Soc Echocardiogr. 2014;27:797–810.
Wang S, et al. Targeting of microbubbles: contrast agents for ultrasound molecular imaging. J Drug Target. 2018;26(5–6):420–34.
Zullino S, et al. From micro- to nano-multifunctional theranostic platform: effective ultrasound imaging is not just a matter of scale. Mol Imaging. 2018;17:1536012118778216.
de Jong N, et al. Ultrasonic characterization of ultrasound contrast agents. Med Biol Eng Comput. 2009;47(8):861–73.
Omata D, et al. Lipid-based microbubbles and ultrasound for therapeutic application. Adv Drug Deliver Rev. 2020;154–155:236–44.
Chitnis PV, Koppolu S, Mamou J, et al. Influence of shell properties on high-frequency ultrasound imaging and drug delivery using polymer-shelled microbubbles. IEEE Trans Ultrason Ferroelectr Freq Control 2013; 60.
Chitnis PV, Lee P, Mamou J, et al. Rupture threshold characterization of polymer-shelled ultrasound contrast agents subjected to static overpressure. J Appl Phys. 2011;109:84906–8490610.
Sirsi S, Borden M. Microbubble compositions, properties and biomedical applications. Bubble Sci Eng Technol. 2009;1(1–2):3–17.
Feinstein SB, et al. Safety and efficacy of a new transpulmonary ultrasound contrast agent: initial multicenter clinical results. J Am College Cardiologyvol. 1990;16(2):316–24.
Mulvagh SL, et al. American Society of Echocardiography consensus statement on the clinical applications of ultrasonic contrast agents in echocardiography. J Am Soc Echocardiogr. 2008;21(11):1179–201 quiz 1281.
• Porter TR, Mulvagh SL, Abdelmoneim SS, Becher H, Belcik JT, Bierig M, et al. Clinical applications of ultrasonic enhancing agents in echocardiography: 2018 American Society of Echocardiography guidelines update. J Am Soc Echocardiogr. 2018;31:241–74.This paper updates the 2008 guidelines and replaces the term microbubbles with ultrasound enhancing agents. The paper also updates the new clinical evidence showing that UEAs are safe and efficacious for LV opacification in various clinical scenarios.
• Fraiche A, Strom J. Impact of ultrasound enhancing agents on clinical management. Curr Opin Cardiol. 2022;37(5):389–93.This paper updates the evidence that UEAs are cost effective in reducing downstream costs by improving endocardial border delineation. Improving workflows through enhanced reader confidence and study accuracy makes UEAs an asset in the echo lab despite its current laggard use.
• Ellenberger, Katherine et al. “The effect of obesity on echocardiographic image quality.” Heart Lung Circ 2022; 31(2): 207–215.This paper demonstrates that increasing BMI, a surrogate for obesity, necessitates increasing UEA use to reduce nondiagnostic studies.
Kooiman K, et al. Ultrasound-responsive cavitation nuclei for therapy and drug delivery. Ultrasound Med Biol. 2020;46(6):1296–325.
Wang M, et al. Sonoporation-induced cell membrane permeabilization and cytoskeleton disassembly at varied acoustic and microbubble-cell parameters. Sci Rep. 2018;8(1):3885.
Hu Y, et al. Membrane perforation and recovery dynamics in microbubble-mediated sonoporation. Ultrasound Med Biol. 2013;39(12):2393–405.
Man VH, et al. Molecular mechanism of the cell membrane pore formation induced by bubble stable cavitation. J Phys Chem B. 2019;123(1):71–8.
Yong Y, Wu D, Fernandes V, Kopelen HA, Shimoni S, Nagueh SF, Callahan JD, Bruns DE, Shaw LJ, Quinones MA, Zoghbi WA. Diagnostic accuracy and cost-effectiveness of contrast echocardiography on evaluation of cardiac function in technically very difficult patients in the intensive care unit. Am J Cardiol. 2002;89(6):711–8.
Hughes RK, et al. Apical hypertrophic cardiomyopathy: the variant less known. J Am Heart Assoc. 2020;9(5):e015294.
• Nagueh, Sherif F et al. “Recommendations for multimodality cardiovascular imaging of patients with hypertrophic cardiomyopathy: an update from the American Society of Echocardiography, in Collaboration with the American Society of Nuclear Cardiology, the Society for Cardiovascular Magnetic Resonance, and the Society of Cardiovascular Computed Tomography.” J Am Soc Echocardiogr 2022; 35(6): 533–569. This paper provides the latest ASE guidelines on how to image in HCM patients and excellent examples of multimodality imaging incorporating UEAs.
Urbano-Moral JA, et al. Contrast-enhanced echocardiographic measurement of left ventricular wall thickness in hypertrophic cardiomyopathy: comparison with standard echocardiography and cardiac magnetic resonance. J Am Soc Echocardiogr. 2020;33(9):1106–15.
Phelan D, et al. Comparison of ventricular septal measurements in hypertrophic cardiomyopathy patients who underwent surgical myectomy using multimodality imaging and implications for diagnosis and management. Am J Cardiol. 2017;119(10):1656–62.
Lang RM, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Euro Heart J Cardiovasc Imaging. 2015;16(3):233–70.
Aggarwal S, et al. Masking and unmasking of isolated noncompaction of the left ventricle with real-time contrast echocardiography. Circ Cardiovasc Imaging. 2017;10(11):e006999.
Gin KG, et al. Femoral vein delivery of contrast medium enhances transthoracic echocardiographic detection of patent foramen ovale. J Am Coll Cardiol. 1993;22(7):1994–2000.
Goyal SK, Punnam SR, Verma G, Ruberg FL. Persistent left superior vena cava: a case report and review of literature. Cardiovasc Ultrasound. 2008;10(6):50.
Bagur R, et al. A novel application of contrast echocardiography to exclude active coronary perforation bleeding in patients with pericardial effusion. Catheter Cardiovasc Interv: official journal of the Society for Cardiac Angiography & Interventions. 2013;82(2):221–9.
Weinsaft JW, et al. Echocardiographic algorithm for post-myocardial infarction LV thrombus: a gatekeeper for thrombus evaluation by delayed enhancement CMR. JACC Cardiovasc imaging. 2016;9(5):505–15.
Camaj A, et al. Left ventricular thrombus following acute myocardial infarction: JACC state-of-the-art review. J Am College Cardiol. 2022;79(10):1010–22. https://doi.org/10.1016/j.jacc.2022.01.011.
Janardhanan R, et al. Usefulness of myocardial contrast echocardiography using low-power continuous imaging early after acute myocardial infarction to predict late functional left ventricular recovery. Am J Cardiol. 2003;92(5):493–7.
Kurt M, et al. Impact of contrast echocardiography on evaluation of ventricular function and clinical management in a large prospective cohort. J Am College Cardiol. 2009;53(9):802–10.
Senior R, et al. Clinical practice of contrast echocardiography: recommendation by the European Association of Cardiovascular Imaging (EACVI) 2017. Euro Heart J Cardiovasc Imaging. 2017;18(11):1205–1205af.
Plana JC, Mikati IA, Dokainish H, et al. A randomized cross-over study for evaluation of the effect of image optimization with contrast on the diagnostic accuracy of dobutamine echocardiography in coronary artery disease: the OPTIMIZE trial. J Am Coll Cardiol Img. 2008;1:145.
Woodward W, et al. Real-world performance and accuracy of stress echocardiography: the EVAREST observational multi-centre study. Euro Heart J Cardiovasc Imaging. 2022;23(5):689–98.
Becher H, von Bibra H. “Verstärkung von Doppler-Signalen bei Aorten- und Mitralvitien” [Enhancement of Doppler signals in aortic and mitral valve diseases]. Zeitschrift fur Kardiologie. 1997;86(12):1033–9.
Smith LA, et al. Contrast agent increases Doppler velocities and improves reproducibility of aortic valve area measurements in patients with aortic stenosis. J Am Soc Echocardiogr. 2004;17(3):247–52.
Dwivedi G, Hickman M, Senior R. Accurate assessment of aortic stenosis with intravenous contrast. Eur J Echocardiogr. 2006;7(2):165–7.
Byrd BF 3rd, et al. Contrast echocardiography enhances tricuspid but not mitral regurgitation. Clin Cardiol. 1991;14(11 Suppl 5):V10–4.
Sorrell, Vincent, Kumar, Sachin. "Doppler contrast echocardiography". Establishing better standards of care in doppler echocardiography, computed tomography and nuclear cardiology, edited by Richard Fleming, IntechOpen 2011; https://doi.org/10.5772/25152.
Wei K, et al. Quantification of myocardial blood flow with ultrasound-induced destruction of microbubbles administered as a constant venous infusion. Circulation. 1998;97(5):473–83.
Abdelmoneim SS, et al. Microvascular function in Takotsubo cardiomyopathy with contrast echocardiography: prospective evaluation and review of literature. J Am Soc Echocardiogr. 2009;22(11):1249–55.
Lashin H, et al. Contrast-enhanced echocardiography application in patients supported by extracorporeal membrane oxygenation (ECMO): a narrative review. J Cardiothorac Vasc Anesth. 2022;36(7):2080–9.
Pereira JB, et al. The feasibility of contrast echocardiography in the assessment of right ventricular size and function. Echocardiography. 2019;36(11):1979–88.
Argulian E, et al. Safety of ultrasonic enhancing agents in patients with COVID-19. J Am Soc Echocardiogr : official publication of the American Society of Echocardiography. 2020;33(7):906–8. https://doi.org/10.1016/j.echo.2020.04.022.
Johri AM, et al. ASE statement on point-of-care ultrasound during the 2019 novel coronavirus pandemic. J Am Soc Echocardiogr. 2020;33(6):670–3.
Porter TR, Mulvagh SL, Abdelmoneim SS, Becher H, Belcik JT, Bierig M, et al. Clinical applications of ultrasonic enhancing agents in echocardiography: 2018 American Society of Echocardiography guidelines update. J Am Soc Echocardiogr. 2018;31:241–74.
Hoffmann R, et al. Assessment of systolic left ventricular function: a multi-centre comparison of cineventriculography, cardiac magnetic resonance imaging, unenhanced and contrast-enhanced echocardiography. Euro Heart J. 2005;26(6):607–16.
Lindner JR, Wei K. Contrast echocardiography. Curr Problems Cardiol. 2002;27(11):454–519.
• Cosyns B, Helfen A, Leong-Poi H, Senior R. How to perform an ultrasound contrast myocardial perfusion examination? Euro Heart J Cardiovasc Imaging. 2022;23(6):727–9.This paper shows how to give UEAs step by step and tips and tricks on how to enhance the images.
Gavan, Kane [@gavankane] “Really useful echo contrast (UEA) trouble shooting tips by @ceb_cardsdoc at #MayoEchoBR @JaeKOh2 @MayoClinicCV” Twitter, April 24,2021. https://twitter.com/garvankane/status/1385986960087470080
D’Amico A, et al. Definity, an affinity for painful crisis: a case series describing vaso-occlusive pain crises in sickle cell patients undergoing echocardiogram with Definity contrast. Euro Heart J Case Rep. 2020;5(2):ytaa555.
Lindner JR, et al. Expert consensus statement from the American Society of Echocardiography on hypersensitivity reactions to ultrasound enhancing agents in patients with allergy to polyethylene glycol. J Am Soc Echocardiogr. 2021;34(7):707–8.
Desai AK, et al. Hypersensitivity cross-reactivity for ultrasound-enhancing agents and COVID-19 vaccines. J Am Soc Echocardiogr. 2022;35(5):523–5.
• Lindner JR. Contrast echocardiography: current status and future directions. Heart (British Cardiac Society). 2021;107(1):18–24.This paper reviews the latest clinical indications, current and emerging, for UEAs.
Kopechek JA, McTiernan CF, Chen X, et al. Ultrasound and microbubble-targeted delivery of a microRNA inhibitor to the heart suppresses cardiac hypertrophy and preserves cardiac function. Theranostics. 2019;9:7088–98.
Pacella JJ, Brands J, Schnatz FG, Black JJ, Chen X, Villanueva FS. Treatment of microvascular micro-embolization using microbubbles and long-tone-burst ultrasound: an in vivo study. Ultrasound Med Biol. 2015;41:456–64.
Roos ST, Juffermans LJM, Slikkerveer J, Unger EC, Porter TR, Kamp O. Sonothrombolysis in acute stroke and myocardial infarction: a systematic review. IJC Heart Vess. 2014;4:1–6.
• Mathias W., Tsutsui J.M., Tavares B.G., et al."Sonothrombolysis in ST-segment elevation myocardial infarction treated with primary percutaneous coronary intervention". J Am Coll Cardiol 2019;73:2832–2842.This paper shows the first cardiology benefit of UEAs in myocardial infarction.
Mason OR, Davidson BP, Sheeran P, et al. Augmentation of tissue perfusion in patients with peripheral artery disease using microbubble cavitation. J Am Coll Cardiol Img. 2020;13:641–51.
Author information
Authors and Affiliations
Contributions
R.T. and R.J. wrote the main manuscript text and prepared the figures. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Ethical Approval
Not applicable
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Thamman, R., Janardhanan, R. Review of Ultrasound Enhancing Agents in Echocardiography for Better Diagnostic Accuracy. Curr Cardiovasc Imaging Rep 17, 33–42 (2024). https://doi.org/10.1007/s12410-024-09589-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12410-024-09589-5