Abstract
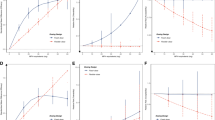
The objectives of this study are: (1) to estimate the expected health outcomes of atypical antipsychotics (AAPs) and other non-stimulant attention-deficit/hyperactivity disorder (ADHD) medications and (2) to evaluate the cost-effectiveness of AAPs compared to other non-stimulant ADHD medications. We used decision analysis to compare three alternatives for treating children and adolescents with ADHD who failed initial stimulant treatment: (1) AAPs, (2) a selective norepinephrine reuptake inhibitor (atomoxetine), and (3) selective α2-adrenergic agonists (clonidine and guanfacine). Probability estimates and quality-adjusted life year (QALY) weights were derived from a literature review. Cost-effectiveness was estimated using the expected health outcomes derived from the decision analysis and expected costs from the literature. The study was conducted from the third-party payer perspective, and the study period was 1 year. One-way deterministic sensitivity analysis and a Monte Carlo simulation were performed. Over the course of 1 year of ADHD pharmacotherapy, the highest QALY was for clonidine/guanfacine (expected QALY = 0.95) followed by atomoxetine (expected QALY = 0.94). Atypical antipsychotics yielded the lowest health outcome with an expected QALY of 0.84. In the cost-effectiveness analysis, the AAP strategy was dominated as it was less effective and more costly than other two strategies. Compared to clonidine/guanfacine, AAPs provided lower QALYs (0.11 QALY lost) at an additional cost of $2186 on average. Compared to atomoxetine, AAPs resulted in 0.10 QALYs lost at an additional cost of $2186. In this decision analysis model, AAPs provide lower expected health outcomes than other ADHD medications in children and adolescents who failed prior stimulant therapy. Furthermore, AAPs were not a cost-effective option.




Similar content being viewed by others
References
Aman MG, Binder C, Turgay A (2004) Risperidone effects in the presence/absence of psychostimulant medicine in children with ADHD, other disruptive behavior disorders, and subaverage IQ. J Child Adolesc Psychopharmacol 14(2):243–254
Andrade SE, Lo JC, Roblin D et al (2011) Antipsychotic medication use among children and risk of diabetes mellitus. Pediatrics 128(6):1135–1141
Armenteros JL, Lewis JE, Davalos M (2007) Risperidone augmentation for treatment-resistant aggression in attention-deficit/hyperactivity disorder: a placebo-controlled pilot study. J Am Acad Child Adolesc Psychiatry 46(5):558–565
Bangs ME, Tauscher-Wisniewski S, Polzer J et al (2008) Meta-analysis of suicide-related behavior events in patients treated with atomoxetine. J Am Acad Child Adolesc Psychiatry 47(2):209–218
Barbaresi WJ, Katusic SK, Colligan RC, Weaver AL, Jacobsen SJ (2007) Modifiers of long-term school outcomes for children with attention-deficit/hyperactivity disorder: does treatment with stimulant medication make a difference? Results from a population-based study. J Dev Behav Pediatr 28(4):274–287
Biederman J, Melmed RD, Patel A et al (2008) A randomized, double-blind, placebo-controlled study of guanfacine extended release in children and adolescents with attention-deficit/hyperactivity disorder. Pediatrics 121(1):e73–e84
Bobo WV, Cooper WO, Stein CM et al (2013) Antipsychotics and the risk of type 2 diabetes mellitus in children and youth. JAMA Psychiatry 70(10):1067–1075
Buse JB, Cavazzoni P, Hornbuckle K, Hutchins D, Breier A, Jovanovic L (2003) A retrospective cohort study of diabetes mellitus and antipsychotic treatment in the United States. J Clin Epidemiol 56(2):164–170
Chinn S (2000) A simple method for converting an odds ratio to effect size for use in meta-analysis. Stat Med 19:3127–3131
Consumer reports best buy drugs (2012) Evaluating prescription drug used to treat: attention deficit hyperactivity disorder (ADHD). http://www.CRBestBuyDrugs.org
Cooper WO, Arbogast PG, Ding H, Hickson GB, Fuchs DC, Ray WA (2006) Trends in prescribing of antipsychotic medications for US children. Ambul Pediatr 6(2):79–83
Correll CU, Manu P, Olshanskiy V, Napolitano B, Kane JM, Malhotra AK (2009) Cardiometabolic risk of second-generation antipsychotic medications during first-time use in children and adolescents. JAMA J Am Med Assoc 302(16):1765–1773
Correll CU, Harris J, Figen V, Kane JM, Manu P (2011) Antipsychotic drug administration does not correlate with prolonged rate-corrected QT interval in children and adolescents: results from a nested case-control study. J Child Adolesc Psychopharmacol 21(4):365–368
Daviss WB, Patel NC, Robb AS et al (2008) Clonidine for attention-deficit/hyperactivity disorder: II. ECG changes and adverse events analysis. J Am Acad Child Adolesc Psychiatry 47(2):189–198
Gau SS, Huang YS, Soong WT et al (2007) A randomized, double-blind, placebo-controlled clinical trial on once-daily atomoxetine in Taiwanese children and adolescents with attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol 17(4):447–460
Goldney RD, Fisher LJ, Wilson DH, Cheok F (2001) Suicidal ideation and health-related quality of life in the community. Med J Aust 175(10):546–549
Hough DW, Natarajan J, Vandebosch A, Rossenu S, Kramer M, Eerdekens M (2011) Evaluation of the effect of paliperidone extended release and quetiapine on corrected QT intervals: a randomized, double-blind, placebo-controlled study. Int Clin Psychopharmacol 26(1):25–34
Jain R, Segal S, Kollins SH, Khayrallah M (2011) Clonidine extended-release tablets for pediatric patients with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 50(2):171–179
Jensen PS, Garcia JA, Glied S et al (2005) Cost-effectiveness of ADHD treatments: findings from the multimodal treatment study of children with ADHD. Am J Psychiatry 162(9):1628–1636
Kelly DL, Conley RR, Love RC, Horn DS, Ushchak CM (1998) Weight gain in adolescents treated with risperidone and conventional antipsychotics over six months. J Child Adolesc Psychopharmacol 8(3):151–159
Kelsey DK, Sumner CR, Casat CD et al (2004) Once-daily atomoxetine treatment for children with attention-deficit/hyperactivity disorder, including an assessment of evening and morning behavior: a double-blind, placebo-controlled trial. Pediatrics 114(1):e1–e8
Koller E, Malozowski S, Doraiswamy PM (2001) Atypical antipsychotic drugs and hyperglycemia in adolescents. JAMA J Am Med Assoc 286(20):2547–2548
Koller EA, Cross JT, Schneider B (2004) Risperidone-associated diabetes mellitus in children. Pediatrics 113(2):421–422
Kratochvil CJ, Vaughan BS, Stoner JA et al (2011) A double-blind, placebo-controlled study of atomoxetine in young children with ADHD. Pediatrics 127(4):e862–e868
Martenyi F, Zavadenko NN, Jarkova NB et al (2010) Atomoxetine in children and adolescents with attention-deficit/hyperactivity disorder: a 6-week, randomized, placebo-controlled, double-blind trial in Russia. Eur Child Adolesc Psychiatry 19(1):57–66
Martin A, Landau J, Leebens P et al (2000) Risperidone-associated weight gain in children and adolescents: a retrospective chart review. J Child Adolesc Psychopharmacol 10(4):259–268
Naglie G, Krahn MD, Naimark D, Redelmeier DA, Detsky AS (1997) Primer on medical decision analysis: part 3–estimating probabilities and utilities. Med Decis Making 17(2):136–141
Olfson M (2004) New options in the pharmacological management of attention-deficit/hyperactivity disorder. Am J Managed Care 10(4 Suppl):S117–S124
Pathak P, West D, Martin BC, Helm ME, Henderson C (2010) Evidence-based use of second-generation antipsychotics in a state medicaid pediatric population, 2001–2005. Psychiatr Serv 61(2):123–129
Remkova A, Kratochvil’ova H (2002) Effect of the new centrally acting antihypertensive agent rilmenidine on endothelial and platelet function in essential hypertension. J Hum Hypertens 16(8):549–555
Sallee FR, Kollins SH, Wigal TL (2012) Efficacy of guanfacine extended release in the treatment of combined and inattentive only subtypes of attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol 22(3):206–214
Sikirica V, Pliszka SR, Betts KA et al (2012) Comparative treatment patterns, resource utilization, and costs in stimulant-treated children with ADHD who require subsequent pharmacotherapy with atypical antipsychotics versus non-antipsychotics. J Managed Care Pharm JMCP 18(9):676–689
Sohn M, Talbert J, Blumenschein K, Moga DC (2015) Atypical antipsychotic initiation and the risk of type II diabetes in children and adolescents. Pharmacoepidemiol Drug Saf 24(6):583–591
Subcommittee on Attention-Deficit/Hyperactivity D, Steering Committee on Quality I, Management et al (2011) ADHD: clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics 128(5):1007–1022
Takahashi M, Takita Y, Yamazaki K et al (2009) A randomized, double-blind, placebo-controlled study of atomoxetine in Japanese children and adolescents with attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol 19(4):341–350
Tickle-Degnen L (2001) From the general to the specific. Using meta-analytic reports in clinical decision making. Eval Health Prof 24:308–326
Tramontina S, Zeni CP, Ketzer CR, Pheula GF, Narvaez J, Rohde LA (2009) Aripiprazole in children and adolescents with bipolar disorder comorbid with attention-deficit/hyperactivity disorder: a pilot randomized clinical trial. J Clin Psychiatry 70(5):756–764
Uzark K, Jones K, Slusher J, Limbers CA, Burwinkle TM, Varni JW (2008) Quality of life in children with heart disease as perceived by children and parents. Pediatrics 121(5):e1060–e1067
Varni JW, Burwinkle TM (2006) The PedsQL as a patient-reported outcome in children and adolescents with attention-deficit/hyperactivity disorder: a population-based study. Health Qual Life Outcomes 4:26
Varni JW, Burwinkle TM, Jacobs JR, Gottschalk M, Kaufman F, Jones KL (2003) The PedsQL in type 1 and type 2 diabetes: reliability and validity of the pediatric quality of life inventory generic core scales and type 1 diabetes module. Diabetes Care 26(3):631–637
Weiss M, Panagiotopoulos C, Giles L et al (2009) A naturalistic study of predictors and risks of atypical antipsychotic use in an attention-deficit/hyperactivity disorder clinic. J Child Adolesc Psychopharmacol 19(5):575–582
Wernicke JF, Faries D, Girod D et al (2003) Cardiovascular effects of atomoxetine in children, adolescents, and adults. Drug Saf 26(10):729–740
Williams J, Wake M, Hesketh K, Maher E, Waters E (2005) Health-related quality of life of overweight and obese children. JAMA J Am Med Assoc 293(1):70–76
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human and animals rights
Our study uses publicly available aggregate data drawn from published journal articles. Our study does not meet the definition of human subjects’ research and therefore does not require IRB review.
Informed consent
For this type of study, formal consent is not required.
Supplementary appendix
Supplementary appendix
This section provides supplementary material for the primary paper, including a more detailed presentation of several methodological points. They should be read in conjunction with the primary paper.
Standardizing probabilities from different forms presented in literature
Probabilities of events in our decision tree were obtained in various forms from the literature. One of the typical ways of presenting the effectiveness/safety of a drug in a randomized control trial (RCT) is to use a two-by-two table. Also, many RCTs report effect size, which is calculated as the difference between the treatment group mean and the control group mean divided by pooled standard deviation [i.e., effect size = (treatment mean—control mean)/pooled SD]. However, these are rarely used in observational studies. For example, studies that assessed antipsychotic agent-associated weight gain reported the average change in body weights with standard deviation. In order to convert the different forms of probabilities into a standardized probability that takes 0 as the lowest possible value and 1 as the highest possible value, we used following methods.
-
1.
Calculating the standardized probability from two-by-two table (ADHD 2012).
The effectiveness/safety of a drug can be expressed using two-by-two table in a RCT. For example, following table is based on the result of RCT conducted by Daviss et al. (2008).
Bradycardia | No Bradycardia | |
|---|---|---|
Clonidine-treated (n = 31) | 7 | 24 |
Placebo (n = 30) | 1 | 29 |
They reported that the probability of having bradycardia in clonidine-treated children was 22.6 % (7/31 × 100 = 22.6 %), and the probability of having bradycardia in placebo group was 3.3 % (1/30 × 100 = 3.3 %). The probability of clonidine-associated bradycardia is calculated as the proportionate increase in the probability of bradycardia resulting from clonidine treatment, which is equal to 0.854 = (0.226 − 0.033)/0.226.
-
2.
Calculating the standardized probability from effect size (Tickle-Degnen 2001).
The effect size is defined as the difference between the mean outcomes for treatment and control groups in standard deviation units. Tickle-Degnen (2001) argues that because the effect size is a standard normal deviate, we can assume a normal distribution to describe the variation of individuals’ responses around the average outcomes (Tickle-Degnen 2001). For example, if the effect size is 0.65 as shown in the guanfacine RCT study conducted by Sallee et al. (2012), the probability of effectiveness is simply the area under the standard normal curve at 0.65, which is equal to 0.627.
-
3.
Calculating the standardized probability from the change in body weight.
The effect size of a drug with respect to weight gain is calculated based on the reported body weight changes of the treatment and control groups. Once the effect size is estimated, the standardized probability is obtained using the standard normal table (Tickle-Degnen 2001).
-
4.
Calculating the standardized probability from hazard ratio (Chinn 2000).
The hazard ratio is equivalent to the odds that a patient in the treatment group reaches the endpoint first (Chinn 2000). For example, the probability of developing type II diabetes first can be derived from the odds of developing type II diabetes first, which is the probability of developing type II diabetes first divided by the probability of not developing first:
$${\text{Hazard ratio }}\left( {\text{HR}} \right) \, = {\text{ odds }} = \, P/\left( {1 \, - \, P} \right);$$$$P \, = {\text{ HR}}/\left( {1 \, + {\text{ HR}}} \right)$$
Rights and permissions
About this article
Cite this article
Sohn, M., Talbert, J., Moga, D.C. et al. A cost-effectiveness analysis of off-label atypical antipsychotic treatment in children and adolescents with ADHD who have failed stimulant therapy. ADHD Atten Def Hyp Disord 8, 149–158 (2016). https://doi.org/10.1007/s12402-016-0198-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12402-016-0198-1